Abstract
Background
Acute kidney injury (AKI) is a serious health problem in critically ill children. It is associated with poor treatment outcomes and high morbidity and mortality rates. Globally, one in three critically ill children suffers from acute kidney injury. However, limited data are available in Africa, particularly Ethiopia, which highlighting the risk factors related to acute kidney injury. Therefore, this study aimed to identify the risk factors associated with acute kidney injury among critically ill children admitted to the pediatric intensive care unit (PICU) at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia.
Methods
A facility-based unmatched case-control study was carried out on 253 (85 cases and 168 controls) critically ill children admitted to the pediatric intensive care unit from January 2011 to December 2021. Participants were selected using a systematic random sampling technique for the control group and all cases consecutively. Data were collected using a structured checklist. Data were entered using Epi data version 4.6 and analyzed using SPSS version 25. Multivariable analysis was carried out using the adjusted odds ratio (aOR) with a 95% confidence interval (CI) to identify associated factors with acute kidney injury. Statistical significance was set at P < 0.05.
Results
The median age of the participants was two years. Approximately 55.6% of cases and 53.1% of controls were females. The diagnosis of hypertension (aOR = 5.36; 95% CI: 2.06–13.93), shock (aOR = 3.88, 95% CI: 1.85–8.12), exposure to nephrotoxic drugs (aOR = 4.09; 95% CI: 1. 45- 11.59), sepsis or infection aOR = 3.36; 95% CI: 1.42–7.99), nephritic syndrome (aOR = 2.97; 95% CI:1.19, 7.43), and use of mechanical ventilation aOR = 2.25, 95% CI: 1.12, 4.51) were significantly associated factors with acute kidney injury.
Conclusion
The diagnosis of sepsis or infection, hypertension, shock, nephrotoxic drugs, demand for mechanical ventilation support, and nephritic syndrome increased the risk of AKI among critically ill children. Multiple risk factors for AKI are associated with illness and severity. All measures that ensure adequate renal perfusion must be taken in critically ill children with identified risk factors to prevent the development of AKI.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) refers to any sudden decline in kidney function that can be reversible with timely detection and interventions. It is a common complication in children admitted to (PICU) [1,2,3,4]. Kidney disease and improving global outcomes (KDIGO) have been established to provide a standardized definition for AKI in children by harmonizing the risk, injury, failure, loss, end-stage (RIFLE), and acute kidney injury network (AKIN) criteria [1, 5]. Staging is based on changes in serum creatinine from baseline or urine output as stages I, II, III, and severe AKI [6]. AKI is one of the most serious global public health problems in the pediatric population [6, 7]. It is highly associated with mortality risk in children worldwide. In children, one-third of the AKI survivors carry the risk of future progression to chronic kidney diseases such as proteinuria, hypertension, and reduced glomerular filtration rate (GFR) may persist in up to 60% of the survivors [1, 3, 8,9,10,11,12].
The International Society of Nephrology revealed that 13.3 million patients develop AKI per year worldwide, and of these, 85% live in low- and middle-income countries (LMICs) [3, 13]. Moreover, KDIGO reported, one in three children experienced AKI during hospital admission, with 30% of incidence among critically ill children [14]. The Assessment of Worldwide AKI Renal Angina and Epidemiology (AWARE) study indicated that 15% of children had AKI on the first day of admission to the PICU, 26.9% had developed AKI within the first seven days of admission, and 11.6% had severe AKI [5, 10, 15, 16].
The risk factors for AKI are not well investigated especially in LMICs [13]. The possible causes of AKI are multidimensional and widely vary from individual to individual and geographical location [1]. The burden of AKI is associated with poor awareness of the public about the possible causes of kidney disease. Some studies indicated that prolonged hospital stay, need for mechanical ventilation, infection, and volume depletion are factors associated with AKI [1, 13]. Children often present to the hospital late, which suggests more severe AKI at admission and an increased risk of death in LMICs [14]. The disease imposes a severe burden of morbidity and mortality, with a major economic effect on healthcare expenditure worldwide, especially in low-resource settings [4, 14, 17,18,19,20]. Studies by the International Society of Nephrology imply that wide gaps remain regarding the determinant factors that affect AKI and its poor outcomes [13]. Children with AKI who progress to the stage at which renal replacement therapy would be indicated die because dialysis is simply not available or affordable in this setting [14]. Higher mortality is likely caused by lack of awareness, delayed recognition and diagnosis of AKI, late hospital presentation, and limited dialysis resources [14, 17].
Moreover, data regarding the risk of AKI in LMICs are limited. Understanding the factors associated with AKI and its early diagnosis is very important for the development of preventive and therapeutic strategies. Therefore the objective of this study was to assess the risk factors for AKI among critically ill children admitted to the PICU at the Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia.
Methods
Study setting and design
This retrospective, facility-based, unmatched case-control study was conducted at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. All children aged one month to 18 years admitted to the PICU at the Tikur Anbessa Specialized Hospital between January 2011 and December 2021 were included in this study.
Population
Children with confirmed AKI cases and unmatched non-AKI children admitted to the PICU at Tikur Anbessa Specialized Hospital during the study period were included. However, we excluded children with short intensive care unit stays (< 24 h) and those who had no laboratory investigation of serum creatinine or urine output measurements during their PICU admission. Moreover, we excluded children with known chronic renal diseases and those who had undergone renal transplantation.
Sample size and procedure
The sample size was computed using Statcalc software. The software application EPI-Info version 7.2.5.0. with the following assumptions: the proportion of mortality among controls was 8.7% and 26.5% of the cases [21], 95% confidence interval, 90% power of the study, control to case ratio of 2:1, and odds ratio of 3.78. We added a 10% non-response rate. Thus, the required sample size was 253 (85 cases and 168 controls).
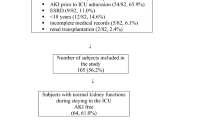
The study was conducted at the Tikur Anbessa specialized hospital in Addis Ababa, Ethiopia, and the data were collected from the PICU. All the patients (cases) were critically ill children with confirmed AKI who were admitted to the PICU between January 2011 and December 2021. For each case, two controls were selected using systematic random sampling. According to data obtained from the PICU of the Tikur Anbessa specialized hospital, 2468 were admitted, of which 2374 children did not have AKI and 94 had AKI. Of these, 85 cases and 168 controls were selected.
Data collection
Data were collected through a review of medical records using a pre-tested structured data abstraction checklist developed and validated by experts. The review checklist contained sociodemographic and morbidity mortality-related factors. It also included mechanical ventilation, radiologic contrast, and length of hospital stay. Case: Children with ≥ 0.3 mg/dL or ≥ 26.5 mmol/L serum creatinine level increase from the baseline within 48 h, or 1.5 to 1.9 times increment in serum creatinine from the baseline within 7 days, or urine output < 0.5 ml/kg/h for 6-12 h [2]. Control: Children who had no increment in serum creatinine level or urine output and did not fulfill for AKI using kidney disease improving global outcome criteria. Baseline creatinine: Take as normal serum creatinine of children to the age; 0.2–0.4 mg/dL for infants; 0.3–0.7 mg/dL for 1–12 years; 0.5- 1.0 mg/dL for 13–18 years [22, 23].
Critically ill child
Child with two or more of the following signs and symptoms such as; impaired consciousness, shock, severe respiratory distress; (severe lower chest wall in drawing, cyanosis, grunting, stridor/wheezes, hypoxemia of SPO2 < 88% or those in gasping or apneic state) severe dehydration, generalized edema, acute bleeding, severe burn, severe pallor with signs of heart failure, severe malaria, anemia < 5 g/dl, and history of two or more episodes of convulsions [24].
Sepsis
two or more of the following systemic inflammatory response syndrome criteria; ( fever of more than 38 °C or less than 36 °C, heart rate > 2SD per age group, respiratory > 2SD breaths per minute, abnormal white blood cell count (> 12,000/µL or < 4,000/µL), an increase in C Reactive protein (CRP), or confirmed by blood culture).
Nephron toxic drugs
Drugs and agents considered to cause nephrotoxicity include non-steroidal anti-inflammatory drugs, antibiotics, amphotericin-B, antiviral agents, angiotensin-converting enzyme inhibitors, calcineurin inhibitors, radiocontrast media, and cytostatic agents.
Hypertension
Children’s blood pressure above the 95th percentile for the same age, sex, and height.
Data quality control
Data quality was ensured using a wise and carefully designed standardized checklist. A pretest was carried out on 12 (5%) medical charts at St. Paul’s Hospital, Millennium Medical College, before actual data collection. The content validity index was calculated by seven experts, the result was 0.93. Two days of training were provided to all data collectors and supervisors. The data collection process was closely supervised and the completeness of each questionnaire was checked daily by supervisors and the principal investigator. During data cleaning, a logical checking technique was employed to identify errors. Finally, double data entry was performed to verify the data consistency.
Data processing and analysis
Data were entered using Epi data 3.1 version and analyzed using SPSS software 25.0 version. Cross-tabulation was performed to determine the sample characteristics. Descriptive statistics were used to describe the characteristics using tables, figures, and text. AKI was labeled as yes (coded as 1) for cases and no for controls (coded as 0). Factors associated with AKI were analyzed using a binary logistic regression model. All variables with a p-value < 0.25 in the bi-variable regression were added to the multivariable analysis after checking for multicollinearity. Associations were described using an adjusted odds ratios (aOR) and with a 95% confidence interval (CI). Multi-collinearity was checked using a variance inflation factor (> 10) and a standard error (> 2). Goodness-of-fit was checked using the Hosmer-Lemeshow test (> 0.05). Finally, statistical significance was set at a p-value < 0.05.
Results
Socio-demographic characteristics
A total of 241 (81 cases and 160 controls) medical charts of critically ill children were completed and reviewed for this study. The remaining records were excluded from the analysis due to incomplete data and unknown clinical measurements. Of the participants; 54 (66.7%) of the cases and 100 (62.5%) of the controls were between the age of one month and five years old, with a median age of two years. Forty-five (55.6%) cases and 75(53.1%) controls were females. Twenty-five (30.9%) cases were from the Oromia region and 45 (28.1%) of the controls were from the Addis Ababa administration. Regarding the length of hospital stay of critically ill children, Fifty-three (65.4%) of cases and 116 (72.5%) controls stayed for less than 14 days in PICU, with a median length of eight days (Table 1).
Diagnosis at admission
The most common diagnoses of cases at admission were shock 52 (63%), sepsis or infection 26 (32.1%), hypertension 25 (30.9%), and nephritic syndrome 23(28.4%. Whereas 48 (30%) of children were diagnosed with shocks and 39 (24.4%) with surgery-related diseases were among the controls group (Table 2).
Stage of acute kidney injury and treatment outcome
Of the total cases, 72 (88.9%) had stage III AKI. Only 6 (7.4%) had a full renal recovery, and 66 (81.5%) children suffered from no renal recovery (Table 3).
Risk factors associated with acute kidney injury
Multivariable logistic regression showed that AKI was associated with sepsis or infection, shock, hypertension, nephrotoxic drugs, mechanical ventilation, and nephritic syndrome. Critically ill children diagnosed with hypertension were five times (aOR = 5.36, 95% CI: 2.06–13.93) more likely to develop AKI than their counterparts. Children who suffered from shock were four times (aOR = 3.88, 95% CI: 1.85–8.12) more likely to develop AKI compared with their counterparts. Moreover, critically ill children exposed to nephrotoxic drugs were four times (aOR = 4.09, 95% CI: 1.45–11.59) more likely to suffer from AKI than those who didn’t have exposure to nephrotoxic drugs. Furthermore, children admitted with sepsis or infections were three times (aOR = 3.36, 95% CI: 1. 42-7.99) more likely to develop AKI than their counterparts. Children diagnosed with the nephritic syndrome were three times (aOR = 2.97, 95% CI: 1.19,-7.43) more likely to have AKI compared to their counterparts. In addition, children who received mechanical ventilation intervention were two times (aOR = 2.25, 95% CI: 1.12–4.51) more likely to develop AKI compared with those who did not receive mechanical ventilation intervention (Table 4).
Discussion
AKI is a serious public health problem, especially in children, and a common cause of morbidity and mortality [11, 25, 26]. There is evidence that AKI is often underdiagnosed; delays in recognition and treatment can lead to death before diagnosis [27]. This study was conducted to assess the risk factors associated with AKI among critically ill children admitted to the PICU at the Tikur Anbessa Specialized Hospital in Addis Ababa, Ethiopia. We found the risk of AKI was higher among critically ill children admitted with hypertension, hypovolemic shock, nephrotoxic drug exposure, sepsis or infection, nephritic syndrome, and mechanical ventilation.
In this study, critically ill children diagnosed with hypertension were five times more likely to develop AKI than their counterparts. This is consistent with the results of a study conducted in Montreal, Canada [28]. This could be related to high blood pressure, which causes narrowing, weakening, or hardening of arteries around the kidney. Moreover, damaged arteries cannot deliver sufficient blood to the kidney tissue which resulting in a decline in renal function [29, 30].
Similarly, critically ill children admitted with hypovolemic shock were four times more likely to develop AKI than critically ill children admitted without hypovolemic shock. This study was supported by previous studies conducted in China and other countries [31,32,33]. This is because shock causes circulatory compromise; consequently, kidney injury develops because of ineffective renal blood flow and renal vascular ischemia, and kidney function declines as urine flow decreases and execration is completely suppressed.
Moreover, the present findings indicate that critically ill children diagnosed with sepsis or infection are three times more likely to develop AKI than their counterparts. This finding is in agreement with those of studies in China [31], Addis Ababa, Ethiopia [21], Pennsylvania, the USA, and Taiwan [34, 35]. Sepsis causes profound alteration of circulation and is characterized by impaired distribution of blood flow, decreased peripheral vascular resistance, and derangement of microcirculatory perfusions, such as the renal vasculature [36, 37]. Moreover, some evidence suggests that the inflammatory response that occurs during sepsis causes an adaptive response of the tubular epithelial cell, which is to ensure cell survival by decreasing the cellular function to reduce energy use. Therefore, the occurrence of renal inflammation and abnormal microvascular function, exacerbates the adaptive response of tubular epithelial cells to injury, and consequently declines renal function [36, 38].
Furthermore, critically ill children who had nephritic syndrome were three times more likely to develop AKI than those who didn’t have nephritic syndrome. This study is in line with the result of a previous study conducted in China [32]. Nephritic syndrome is an immunological complication of infection with group A β-hemolytic streptococcus, the immunological complex where deposited in the membranous of glomeruli it results in damaging the underlying tissue and impaired glomerular filtration, it is characterized by microscopic or gross hematuria, hypertension, edema, oliguria, and AKI occurs as a complication of post-streptococcal glomerular nephritis [39].
In addition, the current findings showed that exposure to nephrotoxic drugs such as aminoglycosides, vancomycin, non-steroidal anti-inflammatory drugs, and radiologic contrast were four times greater risk to develop AKI than their counterparts. This finding was supported by studies conducted in India, Toronto Canada, Ethiopia, and Italy [28, 40, 41]. This is because of the decline in detoxification and excretion of kidney function as a result of kidney injury caused by endogenous or exogenous toxicants [42]. Another justification indicated that the exposure of nephrons to drugs often results in alteration of the regulatory mechanism, including impaired glomerular filtration rate, and induces inflammation surrounding the glomerulus, proximal tubules, and cellular matrix [43].
According to the present findings, critically ill children who received mechanical ventilation intervention were twice as likely to develop AKI compared to those who did not receive mechanical ventilation. This finding is in line with studies conducted in Canada and Taiwan [11, 35]. Mechanical ventilation-induced AKI resulting from renal tissue perfusion is impaired due to changes in hemodynamics [44]. Another explanation is that the chemical is released from neurohumoral-mediated changes in intrarenal blood flow [42]. In addition, some studies have shown that systemic inflammatory mediators produced by ventilator-induced lung injury damage kidney tissue through systemic circulation [45]. Moreover, critically ill children who are on mechanical ventilation may experience prolonged hospital stays, which is indeed associated with AKI [46].
We believe that the evidence generated from this study has implications for local policymakers, researchers, and clinicians to give special attention to reducing preventable AKI-associated deaths through the betterment of infrastructure and more prospective research is needed in LMICs for the prevention and early treatment of AKI to save more lives.
Limitations
Our study has some limitations. First, the findings are based on a retrospective review of medical records; therefore, some important variables may be missed. Second, this is an institutional study focusing on patients with AKI admitted to the PICU and may not be generalizable to other populations. Third, the availability of baseline creatinine data was challenging. We calculated the baseline based on the assumption of normal renal function which has been used in different studies.
Conclusion
In conclusion, the diagnosis of sepsis or infection, hypertension, shock, exposure to nephrotoxic drugs, demand for mechanical ventilation support, and nephritic syndrome were factors that increased the risk of AKI in critically ill children. Multiple risk factors for AKI are associated with illness and its severity. All measures that ensure adequate renal perfusion must be taken in children with identified risk factors to prevent the development of AKI. Further studies with larger sample sizes and high-level study designs are recommended to better understand the risk factors.
Data Availability
All data of this study are available from the corresponding author upon reasonable request.
Abbreviations
- AKI:
-
Acute Kidney Injury
- AOR:
-
adjusted Odd Ratio
- AWARE:
-
Assessment of Worldwide Acute Kidney Injury Renal Angina Epidemiology
- COR:
-
Crude Odd Ratio
- CRP:
-
C-reactive protein
- KDIGO:
-
Kidney Disease Improving Global Outcome
- LMICs:
-
Low-middle-income countries
- PICU:
-
Pediatric Intensive Care Unit
- SPSS:
-
Statistical Package for Social Sciences
- TASH:
-
Tikur Anbessa Specialized Hospital
References
Kellum JA, Lameire N, Aki K, Work G, KDIGO, AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary. Crit Care [Internet].2013;17(Part 1):1–15. Available from: https://pubmed.ncbi.nlm.nih.gov/23394211/.
Kellum JA, Lameire N, Aspelin P, Barsoum RS, Burdmann EA, Goldstein SL et al. Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group. Vol. 2, KDIGO clinical practice guideline for acute kidney injury. 2012. p. 1–138.
Olowu WA, Niang A, Osafo C, Ashuntantang G, Arogundade FA, Porter J et al. Outcomes of acute kidney injury in children and adults in sub-saharan Africa: a systematic review. Vol. 4, The Lancet Global Health. 2016. p. e242–50.
Chawla LS, Bellomo R, Bihorac A, Goldstein SL, Siew ED, Bagshaw SM, et al. Acute kidney disease and renal recovery: Consensus report of the Acute Disease Quality Initiative (ADQI) 16 workgroup. Nat Rev Nephrol. 2017;13:241–57.
Sutherland SM, Byrnes JJ, Kothari M, Longhurst CA, Dutta S, Garcia P et al. AKI in hospitalized children: Comparing the pRIFLE, AKIN, and KDIGO definitions. Vol. 10, Clinical Journal of the American Society of Nephrology. 2015. p. 554–61.
Ciccia E, Devarajan P. Pediatric acute kidney injury: prevalence, impact and management challenges. Int J Nephrol Renovascular Disease. 2017;10:77–84.
Kellum JA, Romagnani P, Ashuntantang G, Ronco C, Zarbock A, Anders HJ. Acute kidney injury. Nat Rev Dis Prim [Internet]. 2021;7(1). https://doi.org/10.1038/s41572-021-00284-z.
Bjornstad EC, Smith ZH, Muronya W, Munthali CK, Mottl AK, Marshall SW, et al. High risk of acute kidney injury in malawian trauma patients: a prospective observational cohort study. BMC Nephrol. 2021;22(1):1–12.
Lameire NH, Bagga A, Cruz D, De Maeseneer J, Endre Z, Kellum JA et al. Acute kidney injury: An increasing global concern. Vol. 382, The Lancet. 2013. p. 170–9.
Kataria Y. Epidemiology of acute kidney injury in critically ill children and young adults. Ann Clin Biochem. 2017;54:416.
Alkandari O, Eddington KA, Hyder A, Gauvin F, Ducruet T, Gottesman R et al. Acute kidney injury is an independent risk factor for pediatric intensive care unit mortality, the longer length of stay and prolonged mechanical ventilation in critically ill children: a two-center retrospective cohort study. Vol. 15, Crit Care. 2011.
Sutherland SM, Ji J, Sheikhi FH, Widen E, Tian L, Alexander SR et al. AKI in hospitalized children: Epidemiology and clinical associations in a national cohort. Vol. 8, Clinical Journal of the American Society of Nephrology. 2013. p. 1661–9.
Mehta RL, Cerdá J, Burdmann EA, Tonelli M, García-García G, Jha V et al. International Society of Nephrology’s 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Vol. 385, The Lancet. 2015. p. 2616–43.
Perico N, Remuzzi G. Acute kidney injury in low-income and middle-income countries: No longer a death sentence. Lancet Glob Heal [Internet]. 2016;4(4):e216–7. https://doi.org/10.1016/S2214-109X(16)00065-6.
Fleming GM, Sahay R, Zappitelli M, King E, Askenazi DJ, Bridges BC et al. The incidence of Acute kidney Injury and its effect on neonatal and Pediatric extracorporeal membrane oxygenation outcomes: a Multicenter Report from the kidney intervention during extracorporeal membrane oxygenation Study Group. Vol. 17, Pediatric Critical Care Medicine. 2016. p. 1157–69.
Selewski DT, Askenazi DJ, Kashani K, Basu RK, Gist KM, Harer MW et al. Quality improvement goals for pediatric acute kidney injury: pediatric applications of the 22nd Acute Disease Quality Initiative (ADQI) conference. Vol. 36, Pediatric Nephrology. 2021. p. 733–46.
De Zan F, Amigoni A, Pozzato R, Pettenazzo A, Murer L, Vidal E. Acute kidney Injury in critically Ill Children: a retrospective analysis of risk factors. Vol. 49, Blood Purification. 2020. p. 1–7.
Kasililika AG. Prevalence, risk factors, and immediate outcome of acute kidney injury in critically ill children admitted at Benjamin Mkapa (BMH) and Dodoma regional referral hospitals (DRRH). Unpubl Diss. 2020.
Gordillo R, Ahluwalia T, Woroniecki R. Hyperglycemia and acute kidney injury in critically ill children. Int J Nephrol Renovascular Disease. 2016;9:201–4.
Markos F, Argaw R, Bekele BA. Profile, Risk factors and outcome of Acute kidney Injury in critically Ill Pediatric Patients in Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Vol. 22, Pediatric Critical Care Medicine. 2021. p. 149–9.
Shimelis D, Abebe B, Deyessa N. Incidence of Acute kidney Injury and determinant factors in children admitted to a Tertiary Hospital. IOSR J Dent Med Sci. 2018;17(3):48–53.
Roufosse F, Klion AD, Weller PF, Connor RF. Acute kidney injury in children: clinical features, etiology, evaluation, and diagnosis. UpToDate. 2016. p. 1–21.
Hughes HK, Kahl LK. A Manual for Pediatric House Officers The Harriet Lane Handbook. 2018. 653–659 p.
World Health Organization. Updated guideline: Paediatric Emergency Triage, Assessment, and treatment: care of critically-ill children. World Heal Organ. 2016;7.
Rewa O, Bagshaw SM. Acute kidney injury-epidemiology, outcomes and economics. Nat Rev Nephrol. 2014;10(4):193–207.
Sethi SK, Bunchman T, Chakraborty R, Raina R. Pediatric acute kidney injury: new advances in the last decade. Kidney Res Clin Pract. 2021;41(1):40–51.
Emily L, Joyce SL, Kane-Gill, Dana Y, Fuhrman JAK. Drug-associated acute kidney injury_ who’s at risk_ - PubMed. Pediatr Nephrol. 2017;32(1):39–69.
Hessey E, Perreault S, Roy L, Dorais M, Samuel S, Phan V, et al. Acute kidney injury in critically ill children and 5-year hypertension. Pediatr Nephrol. 2020;35:1097–107.
Czarniak P, Zurowska A. Treatment strategies to prevent renal damage in hypertensive children. Vol. 16, Curr Hypertens Rep. 2014.
Greenberg JH, Coca S, Parikh CR. Long-term risk of chronic kidney disease and mortality in children after acute kidney injury: a systematic review. Vol. 15, BMC Nephrol. 2014.
Xu X, Nie S, Zhang A, Mao J, Liu HP, Xia H et al. Acute kidney injury among hospitalized children in China. Vol. 13, Clinical Journal of the American Society of Nephrology. 2018. p. 1791–800.
Suarez J, Busse LW. New strategies to optimize renal hemodynamics. Vol. 26, Current opinion in critical care. 2020. p. 536–42.
Makris K, Spanou L. Acute Kidney Injury: Definition, Pathophysiology and Clinical Phenotypes. [Internet]. Vol. 37, The Clinical biochemist. Reviews. 2016. p. 85–98.
Formeck CL, Joyce EL, Fuhrman DY, Kellum JA. Association of Acute kidney Injury with subsequent Sepsis in critically Ill Children. Pediatr Crit Care Med. 2021. p. E58–66.
Chang JW, Jeng MJ, Yang LY, Chen TJ, Chiang SC, Soong WJ et al. The epidemiology and prognostic factors of mortality in critically ill children with acute kidney injury in Taiwan. Vol. 87, Kidney International. 2015. p. 632–9.
Zarbock A, Gomez H, Kellum JA. Sepsis-induced acute kidney injury revisited: pathophysiology, prevention and future therapies. Vol. 20, Current Opinion in Critical Care. 2014. p. 588–95.
Bagshaw SM, Bellomo R, Devarajan P, Johnson C, Karvellas CJ, Kutsiogiannis DJ, et al. Review article: Acute kidney injury in critical illness. Can J Anesth. 2010;57:985–98.
Peerapornratana S, Manrique-Caballero CL, Gómez H, Kellum JA. Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention, and treatment. Vol. 96, Kidney International. 2019. p. 1083–99.
Skrzypczyk P, Ofiara A, Zacharzewska A, Panczyk-Tomaszewsk M. Acute post-streptococcal glomerulonephritis - immune-mediated acute kidney injury - case report and literature review. Cent Eur J Immunol. 2021;46:516–23.
Tadesse AME, MMA. and Y. Nephrology in Ethiopia _ Semantic Scholar. Nephrol Worldwide 2021. 2021;35–40.
Gupta S, Sengar G, Meti P, Lahoti A, Beniwal M, Kumawat M. Acute kidney injury in pediatric intensive care unit: incidence, risk factors, and outcome. Indian J Crit Care Med. 2016;20:526–9.
Kim SY, Moon A. Drug-induced nephrotoxicity and its biomarkers. Vol. 20, Biomolecules and Therapeutics. 2012. p. 268–72.
Rodríguez-Iturbe B, García García G. The role of tubulointerstitial inflammation in the progression of chronic renal failure. Vol. 116, Nephron - Clinical Practice. 2010.
Hepokoski ML, Malhotra A, Singh P, Crotty Alexander LE. Ventilator-induced kidney injury: Are novel biomarkers the key to prevention? Vol. 140, Nephron. 2018. p. 90–3.
Hepokoski M, Englert JA, Baron RM, Crotty-Alexander LE, Fuster MM, Beitler JR et al. Ventilator-induced lung injury increases expression of endothelial inflammatory mediators in the kidney. Vol. 312, American Journal of Physiology - Renal Physiology. 2017. p. F654–60.
Aoun B, Daher GA, Daou KN, Sanjad S, Tamim H, El Rassi I, et al. Acute kidney Injury Post-cardiac surgery in infants and children: a single-center experience in a developing country. Front Pediatr. 2021;9(July):1–6.
Acknowledgements
We thank Addis Ababa and Haramaya University for their financial and technical support. We also extend our gratitude to the hospital heads, study participants, data collectors, and supervisors for their collaboration.
Funding
This work was financially supported by Addis Ababa and Haramaya University, Ethiopia. The funder had no role in the study selection, data collection, analysis, conclusion, and interpretation.
Author information
Authors and Affiliations
Contributions
MK, RM, AD, and KB conceived, designed anaysied and interpreted this study. MK and AD drafted the manuscript. AD, TA, ST, and GT reviewed the manuscript and incorporated their intellectual input. All authors read, provided feedback, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was conducted in accordance with the declaration of Helsinki. The study was ethically cleared and approved by the Ethical Review Committee of the Addis Ababa University College of Health Science, School of Nursing and Midwifery (Ref. No: AAUMF03-008). Following approval, an official written letter of cooperation was given to the administrative health bureau and facilities. Written informed consent was obtained from the head of hospital administration. Confidentiality was ensured throughout the process.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Keneni, M., Murugan, R., Bizuwork, K. et al. Risk factors associated with acute kidney injury in a pediatric intensive care unit in Addis Ababa Ethiopia: case-control study. BMC Nephrol 24, 279 (2023). https://doi.org/10.1186/s12882-023-03322-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-023-03322-y