Abstract
Background
This study aimed to investigate the effect of a family-centered empowerment program on hyperphosphatemia management.
Method
This experimental study was performed on 80 randomly selected eligible patients with hyperphosphatemia undergoing hemodialysis. Patients were assigned randomly to two groups of family-centered empowerment program (FCEPG) and control group (CG) by coin toss (40 people per group). Data collection tools were the researcher-made Phosphate Control Knowledge Scale, the researcher-made Adherence to Dietary Restriction of Phosphorus Intake Scale, the eight-item Morisky Medication Adherence Scale, and serum phosphorus measurements. Data were collected before the intervention, one month, and three months after the intervention. Patients in FCEPG participated in a family-centered empowerment program. The statistical significance level was considered to be 0.05.
Results
Inter-group comparisons showed no significant difference between FCEPG and CG in terms of the mean score of knowledge of phosphate control, adherence to dietary restriction of phosphorus intake, adherence to medication, and the mean serum phosphorus level before the empowerment program, but showed significant differences between them in these respects at one month after the program and three months after the program (p < 0.05). Intra-group comparisons showed a significant difference in FCEPG between the mean and standard deviation of all four variables before the empowerment program and the corresponding values one month and three months after the program (P < 0.05).
Conclusion
The findings of this study can be used in various fields of healthcare in the hospital and community.
Similar content being viewed by others
Introduction
Maintenance hemodialysis is a commonly used treatment for end-stage renal disease. In this condition, phosphate becomes easily retained in the body due to decreased renal function, leading to hyperphosphatemia, a common complication in these patients [1]. For adults, hyperphosphatemia has been defined as an abnormal increase in serum phosphate level to concentrations above 5.5 mg/dl [2]. Hyperphosphatemia has a variety of consequences including the modification of vascular smooth muscle cells, which leads to vascular calcifications, hyperparathyroidism, and alterations in bone metabolism. Hyperphosphatemia has been shown to be an independent risk factor associated with increased mortality [3].
Primary interventions for hyperphosphatemia management include the dietary restriction of phosphorus intake (DRPI) and the use of phosphate binders [4, 5]. However, dialysis patients tend to have a poor understanding of DRPI [6] and find it difficult to adhere to DRPI because it requires lifestyle modification [7]. It has been estimated that roughly 43% of dialysis patients do not adhere to the prescribed dietary regimens [5]. The rate of non-adherence to phosphate binders is also quite high, as some estimates suggest that over half of dialysis patients do not follow the prescribed medication regimens [8].
There are a variety of strategies, including educational and behavioral interventions, to improve the phosphorus control of hemodialysis patients (HPs) by improving their adherence to treatment regimens and helping them engage in healthy behaviors [5, 9]. Patient empowerment interventions can potentially improve the motivation, lifestyle control, and self-confidence of HPs [10]. While healthcare workers are responsible for caring for HPs in medical settings, they need to be cared for at home by family caregivers (FCGs) and also need to take care of themselves. Thus, HPs need adequate support from FCGs who are directly involved in their care [11]. However, most FCGs have poor knowledge of the disease, symptom management solutions, and home care practices. Thus, providing education and support in the framework of family empowerment can help HPs and their FCGs take charge in managing the disease and treatment-related problems, which can reduce the complications of hemodialysis [12]. Family empowerment can help families change for the better. Family-centered empowerment makes the patients and their families more involved in health-related decision-making, thereby enabling the patients to control their health and take necessary actions to improve their health on their own [13].
Considering the importance of empowering HPs with hyperphosphatemia and their FCGs in relation to adherence to dietary and medication regimens for the purpose of controlling serum phosphorus levels, this study investigated the effect of a family-centered empowerment program (FCEP) on hyperphosphatemia management and specifically the subjects’ knowledge of phosphate control, adherence to DRPI, adherence to medication, and serum phosphorus level.
Literature review
The effects of education programs on knowledge, adherence to dietary and medication regimens, and serum phosphorus levels of HPs with hyperphosphatemia have been the subject of several studies. In a study by Yin et al., the results showed an improvement in the HPs’ phosphate control rate, their knowledge of phosphate control, and their adherence to phosphate binder regimens after the intervention [1]. A study by Chan et al. on the effectiveness of a multidisciplinary program in controlling the hyperphosphatemia of HPs in Kuala Lumpur, Malaysia, also reported a decrease in the percentage of patients with uncontrolled phosphorus levels and an increase in the percentage of patients adhering to phosphate binder regimens [14]. In another study on the effects of a comprehensive multidisciplinary program with the goal of long-term hyperphosphatemia management, the results showed a relative improvement in serum phosphate levels as long as all parts of the program are implemented [3]. Lim et al. reported that a program they implemented to educate HPs about low phosphate diets and phosphate binders in order to control serum phosphate levels managed to improve patients’ knowledge of the appropriate time of phosphate binder consumption to some extent [15]. In a study by Stumm et al., they reported that a nursing education intervention was effective in reducing hyperphosphatemia, and that the more aware the patients were about the disease and treatment, the better their adherence was to treatment [16]. Although several studies have investigated the effect of patient education and empowerment on patients’ knowledge, dietary and medication adherence, and serum phosphate levels, this was the first study on the effect of an FCEP on hyperphosphatemia management. Given the goal of this study, which was to determine the effect of an FCEP on hyperphosphatemia management, the following hypotheses were raised and tested:
-
H1: FCEP affects patients’ knowledge of phosphate control.
-
H2: FCEP affects patients’ adherence to DRPI.
-
H3: FCEP affects patients’ adherence to medication.
-
H4: FCEP affects patients’ serum phosphorus levels.
Methods
Study design and setting
This study was experimental research conducted on two groups of HPs: 1- patients participating in an FCEP (hereafter refers to as FCEPG) and 2- patients in the control group (hereafter refers to as CG). All patients were recruited from the hemodialysis ward of Shahid Beheshti Hospital in Hamadan, Iran. This ward has 30 beds in three halls and provides hemodialysis to about 70 patients every day in morning and evening sessions.
Designed as a single-blind experiment, the study was arranged such that patients remain unaware of the designated interventions so that their knowledge would not affect their behavior.
Participants and recruitment
All participants were HPs. The sample size was computed using the following formula based on the findings of Lim et al. [15], for the first type error of 0.05, the second type error of 0.10, the test power of 0.90, and the 10% sample loss. Using this method, the sample size was estimated to 40 people per group.
For sampling, the first researcher identified eligible HPs with the help of nurses. Participants of FCEPG were recruited exclusively from the morning shift and CG from the evening shift to prevent contamination. After assigning a number to each eligible HP, the numbered HPs in the morning shift were randomly assigned to FCEPG and in the evening shift to CG by casting lots. The selection of participants continued until the target sample size was reached. The two groups were matched in terms of age and gender. All participants were included in the study at the end of data collection.
Inclusion criteria were: minimum age of 35 and maximum age of 70 years, serum phosphorus level of more than 5.5 mg/dl over the last six months, presence of a first- or second-degree family member (father, mother, sibling, spouse, child, son/daughter-in-law) as the constant FCG providing care for at least six months during the dialysis session and at home, no mental illness in HP or FCG based on their report, and HP or FCG not simultaneously participating in another educational program related to diet or medication. Exclusion criteria were: HP or FCG not wanting to continue participating in the study, HP or FCG not participating in education sessions after enrollment (absence in two sessions), and deterioration of the physical condition, hospitalization, or death of HP.
Family-centered empowerment program (FCEP)
A Family-Centered Empowerment Program (FCEP) was implemented as an intervention for FCEPG. This program was prepared clearly and simply for participants because it was assumed that some participants were probably illiterate. The content was developed based on the latest scientific sources [1, 4, 8, 17,18,19] and then its content validity was confirmed by two nephrologists and a nutritionist. The program was implemented in four 15–30 min sessions held for HPs with hyperphosphatemia and their FCGs during hemodialysis. Each session comprised a lecture followed by Q&A. The goals and content of these sessions and the actions taken in each session are listed in Table 1. At weeks 2, 4, 6, and 8 after the end of the fourth session, the educational content was reviewed for HPs and FCGs during hemodialysis and their questions were answered. From the beginning of the program, FCGs were asked to continuously remind HPs of the educational material and evaluate their adherence to recommendations until the final stage of data collection.
It should be noted that participants in both CG and FCEPG also received conventional education from the hemodialysis unit. This conventional education is a short (a few minutes long) briefing about low phosphate diets that is routinely provided by a nurse or physician at discharge to HPs who have hyperphosphatemia (> 5.5 mg/dl) on the day of hemodialysis.
Outcome measurements
Primary outcomes
The primary outcomes of the program were assumed to be a change in patients’ knowledge of phosphate control, adherence to DRPI, and adherence to medication, which were measured by the researcher-made Phosphate Control Knowledge Scale, researcher-made Dietary Restriction of Phosphorus Intake Scale (DRPI-S), and the eight-item Morisky Medication Adherence Scale (MMAS-8), respectively.
Secondary outcomes
The secondary outcome of the program was assumed to be a change in serum phosphorus level.
Baseline
The first researcher collected data. Baseline measurements for FCEPG and CG were performed before interventions while HPs were undergoing hemodialysis. For illiterate HPs, the questions were read aloud and answers were recorded by the first researcher.
Follow-ups
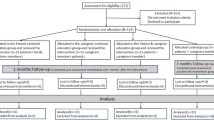
Follow-up measurements were performed once one month after FCEP (Follow-Up1) and another time three months after FCEP (Follow-Up2) at patients’ subsequent hemodialysis appointments before the start of hemodialysis. CONSORT flow chart of the study is illustrated in Fig. 1.
Measures
Sociodemographic and clinical data of participants and family caregivers
Sociodemographic and clinical information questionnaire contained 11 questions about HPs (age, gender, education level, marital status, employment status, duration of undergoing hemodialysis, primary disease, dialysis frequency, receiving vitamin D, and calcimimetics, and smoking. This questionnaire also contained seven questions about FCGs (age, gender, education level, marital status, employment status, relation to the patient, and duration of providing care to the patient).
Knowledge of phosphate control
Knowledge of phosphate control was measured by the Phosphate Control Knowledge Scale, which was a researcher-made tool. This questionnaire was developed by adapting the tools of similar studies and scientific recourses [14, 20, 21].
This tool has 16 items with the answers “true” (1 point), “false” (0 points), and “I don’t know” (0 points). Items 1, 9, 10, and 13 were scored in reverse. The higher the score, the greater the Knowledge of phosphate control. This scale’s minimum and maximum scores are 0 and 16, respectively (Table 2).
To check the validity of the Phosphate Control Knowledge Scale, it was submitted for review to 10 faculty members of Shahid Beheshti University of Medical Sciences. During this process, in addition to qualitative content validity assessment, the necessity of the questions and their relevance to the research objectives were also evaluated based on Content Validity Ratio (CVR) and Content Validity Index (CVI), respectively [22]. Based on the Lawshe table, all items earned CVR scores of more than 0.62, which confirmed their necessity [23]. The Scale-level Content Validity Index (S-CVI) was calculated to 0.93. The face validity of the scale was verified by asking 10 HPs with hyperphosphatemia to evaluate it in terms of comprehensibility, transparency, and fluency.
The reliability of this tool was established by test–retest and intra-class correlation calculation based on the responses of 10 participants who filled out the questionnaire two times with a 10-day interval. Using this method, the intra-class correlation coefficient was calculated to 0.75. The Cronbach’s alpha of the tool based on the responses of 20 HPs who were not included in the study was calculated to 0.88 that showed the instrument was reliable [22].
Adherence to dietary restriction of phosphorus intake
Adherence to DRPI was measured by the researcher-made Dietary Restriction of Phosphorus Intake Scale (DRPI-S), which was also developed by the researchers based on scientific sources [18, 19]. This scale has 10 items, each with five responses scored on a 5-point Likert scale: “Never” (1 point), “Rarely” (2 points), “Sometimes” (3 points), “Most of the time” (4 points) and “Always” (5 points). Items 8 and 9 were scored in reverse. The minimum and maximum scores of this scale are 10 and 50, respectively. The higher the score, the greater the adherence to dietary restriction of phosphorus intake (Table 3).
The validity and reliability of this tool were established in the same way as described for the Phosphate Control Knowledge Scale. All items of this tool earned CVR and CVI scores of more than 0.62 and 0.96, respectively, which confirmed their necessity and relevance. The tool’s intra-class correlation coefficient and Cronbach’s alpha were determined to be 0.91 and 0.83, respectively, which confirmed the reliability of the tool [22].
Adherence to medication
Adherence to medication was measured using the version of eight-item Morisky Medication Adherence Scale (MMAS-8)Footnote 1 [24]. US Copyright laws protect the use of the MMAS-8, and an agreement for use is required. The authors have obtained a license from the scale inventor Donald E. Morisky (Certificate number: 7668–6979-6950–5104-2081). This self-report instrument has been used in several studies to assess adherence to medication in chronic diseases. MMAS-8 is a highly credible tool for measuring patients’ adherence to their medication [25]. This tool is low-cost, noninvasive, with minimal burden on a participant, easy to administer, and offers flexible timing. It has been validated in many countries and translated into several languages [26]. The first seven items having a “Yes” (score 0), and “No” (score 1) responses, except question 5, which reverses the score. For item 8, a patient can choose an answer on a 5-point Likert scale as “Never/Rarely” (score 1), “Once in a while” (score 0.75), “Sometimes” (score 0.5), “Usually” (score 0.25), “All the time” (score 0), expressing how often happens that a patient does not take his medications. MMAS-8 scores can range from zero to 8 points. Patients who scored 8 points, < 8 to > 6 points and ≤ 6 points on the scale were considered to have high, medium and low adherence, respectively [27, 28]. The Cronbach’s alpha of MMAS-8 based on the responses of 20 HPs who were not included in the study was calculated to 0.69.
Serum phosphorus measurement
At the dialysis ward, serum phosphorus level measurement was a routine procedure for all HPs with hyperphosphatemia while fasting. This procedure involved a nurse taking a blood sample, sending it to the hospital’s laboratory, and then recording the results in the HP’s medical file at 8 AM. The first researcher (responsible for implementing the interventions and collecting the data) extracted the participating HPs’ serum phosphorus level data from their medical files and recorded them in the data collection sheets.
The blood samples of the CG participants undergoing evening hemodialysis sessions were also prepared in the morning. CG participants were asked to attend the hemodialysis department at 8 AM for the data collection sessions (baseline, follow-up 1, and follow-up 2) in a fasting state for blood sampling. The researcher went to their homes to take the blood sample for participants who did not want to go to the hemodialysis department in the morning.
Data analysis
The collected data were processed using the software SPSS version 26. The data were analyzed by descriptive statistical methods such as computing numerical measures (mean and standard deviation) and inferential tests. The independent t-test and the chi-square test were used to compare FCEPG and CG in terms of demographic variables. The independent t-test was also used to compare FCEPG and CG in terms of knowledge of phosphate control, adherence to DRPI, adherence to medication, and serum phosphorus level. The GLM-repeated measures ANOVA was used to make intra-group comparisons between the three measurement stages: Baseline, Follow-Up1 (one month after FCEP), and Follow-Up2 (three months after FCEP). For all tests and analyses, the significance level was considered to be 0.05.
Results
The mean age of HPs in FCEPG and CG was 48.16 ± 16.6 and 46.35 ± 14.86, respectively. Participants in FCEPG and CG were undergoing hemodialysis for respectively 8.63 ± 4.09 and 7.65 ± 4.17 years on average. There was no significant difference between the participants in FCEPG and CG in terms of any of the variables.
Also, the mean age of FCGs in FCEPG and CG was 38.28 ± 10.23 and 39.65 ± 10.89, respectively. There was no significant difference between the two groups in terms of the age of HPs or FCGs.
FCGs of the two groups were providing care to HPs for 9.82 ± 3.63 and 9.13 ± 3.42 years, respectively. Other demographic information of the participants is given in Table 4.
The results showed no significant difference between FCEPG and CG in terms of the mean and standard deviation of knowledge of phosphate control, adherence to DRPI, and adherence to medication (primary outcomes) at Baseline, but showed significant differences between them in these respects at Follow-Up1 and Follow-Up2 (P < 0.05), indicating a change in the scores of all four variables after the implementation of FCEP (Table 5).
Intra-group comparisons between Baseline, Follow-Up1, and Follow-Up2 showed significant changes in the mean and standard deviation of knowledge of phosphate control, adherence to DRPI, and adherence to medication in both FCEPG and CG, but this change was more pronounced in FCEPG than in CG (Table 5). The rising scores in CG may be related to the conventional hemodialysis education provided to HPs with hyperphosphatemia. As the results of Table 5 demonstrate, in FCEPG, the mean scores of all three variables increased significantly from Baseline to Follow-Up1, from Follow-Up1 to Follow-Up2, and from Baseline to Follow-Up2.
Considering the significant differences between FCEPG and CG in terms of the mean scores of knowledge of phosphate control, adherence to DRPI, adherence to medication at Follow-Up1 and Follow-Up2, and the more romanced increase in the mean scores of FCEPG compared to CG, it can be concluded that the implemented FCEP managed to affect knowledge of phosphate control, adherence to DRPI, adherence to medication, which confirms the hypotheses H1, H2, and H3.
As shown in Table 5, while there was no significant difference between FCEPG and CG in terms of serum phosphorus level (secondary outcome) at Baseline, there was such a difference between the two groups at Follow-Up1 and Follow-Up2 (P < 0.05). In both FCEPG and CG, serum phosphorus levels also significantly changed over time (P < 0.05). The point to note is that in FCEPG, serum phosphorus levels slightly increased at Follow-Up1 and then sharply dropped at Follow-Up2. According to Table 6, the increase in FCEPG serum phosphorus level from Baseline to Follow-Up1 was insignificant, but the decrease in serum phosphorus level from Baseline to Follow-Up2 and from Follow-Up1 to Follow-Up2 was significant (P < 0.05). The reason for the initial increase in serum phosphorus level at Follow-Up1 could be that the intervention has not been completely effective until week 4 after FCEP, but the level of serum phosphorus has decreased with the repeated review of the educational content in weeks 6 and 8 after FCEP. From the above results, it can be cautiously concluded that the implemented FCEP can been able to decrease the patients’ serum phosphorus level.
Discussion
The goal of this study was to investigate the effect of an FCEP on hyperphosphatemia management in HPs. The results showed that FCEP could have a positive impact on the patients’ knowledge of phosphate control, adherence to DRPI, and adherence to medication as primary outcomes and on their serum phosphorus levels as the secondary outcome.
Regarding the first research hypothesis, namely the effect of FCEP on knowledge of phosphate control, although we could not find any study on the effect of family-centered education on HPs’ knowledge, we found several studies showing that education and empowerment can improve the knowledge of patients with hyperphosphatemia. The study of Yin et al. for example showed that an intensive education program focused on phosphate control can improve HPs' phosphate control knowledge scores [1]. Hjemås et al. showed that education can increase HPs’ knowledge of the need to control hyperphosphatemia and also their knowledge of how to control it through the use of phosphate binders [20]. A systematic review also reported that educational and behavioral interventions could improve HPs’ knowledge of phosphate level control [29]. According to these results, education and empowerment appear to be an effective approach for improving the knowledge and awareness of patients with hyperphosphatemia and perhaps controlling their serum phosphate levels [30].
In relation to the second hypothesis of this study, namely the effect of FCEP on adherence to DRPI, the literature contains several studies with findings similar to ours. In one of these studies, Montazami et al. reported that home visit-based FCEP can be an effective way to improve adherence to dietary and medication regimens in patients with acute coronary syndrome [31]. Asgari et al. also reported that their FCEP managed to improve HPs’ self-care capability [32]. In a study conducted in Egypt, it was found that empowering HPs and their FCGs helped them manage their health-related problems and improved their self-efficacy [12]. In a study conducted in Australia, the results showed that education programs based on mobile texting can improve HPs’ adherence to dietary regimens [33].
Regarding the third hypothesis of the study, namely the effect of FCEP on adherence to medication, one study has shown that family-centered education is more effective than patient-centered education in improving HPs’ adherence to treatment and especially medication regimens [34]. According to a systematic review and meta-analysis, educational interventions tend to have positive effects on patients’ adherence to dietary regimens and treatment [9]. In a meta-analysis study, it was concluded that educational interventions could significantly change patients’ adherence to treatment [35]. In the study of Yin et al., the results showed that the implementation of an intensive education program focusing on phosphate control could improve HPs’ adherence to medication and consumption of phosphate binders [1]. The results of a quasi-experimental study also showed that education could improve HPs’ adherence to medication [36].
Concerning the fourth hypothesis of the study, namely the effect of FCEP on the secondary outcome, i.e. serum phosphorus level, the results of a study by Rabiei showed that FCEP could reduce the negative outcomes of CKD in patients [34]. The results of Bahramnezhad et al. showed that family-centered education is more effective than patient-centered education in reducing the complications of hemodialysis [37]. The studies of Yin et al. and Lim et al. both showed that an educational program focusing on phosphate control could increase the percentage of HPs with normal serum phosphorus levels [1, 15]. Chan et al. reported that a multidisciplinary program aimed at controlling hyperphosphatemia in HPs could be highly effective in reducing the percentage of patients with uncontrolled phosphorus levels [14]. In a study by Brauer et al., the results indicated that patients’ serum phosphorus levels can be controlled by holding education and discussion sessions about diet and phosphate binders [3]. In a meta-analysis of the literature on the subject, it was concluded that psychosocial and educational interventions can be effective in improving HPs’ adherence to treatment and control of dialysis-related factors, including serum phosphorus level [35].
The present study is significant from these two perspectives. First, it focuses on the empowerment of not only HPs but also FCGs as people who play an essential role in the health promotion of these patients. Second, in addition to exploring the effect of FCEP on primary outcomes such as knowledge of phosphate control, adherence to DRPI, and adherence to medication, this study examines the effect of FCEP on the most important outcome for patients with hyperphosphatemia, i.e. serum phosphorus level.
Conclusion
This study aimed to determine the effect of FCEP on hyperphosphatemia management in HPs. The results showed that in addition to affecting knowledge of phosphate control, adherence to DRPI, and adherence to medication as primary outcomes, FCEP could improve the serum phosphorus level of patients with hyperphosphatemia as the secondary outcome.
Considering the effect of FCEP on patients with hyperphosphatemia in terms of primary and secondary outcomes, the authors recommend the implantation of this program by healthcare workers in hospital hemodialysis wards as well as home-visiting to improve the health of hemodialysis patients with hyperphosphatemia. It is also recommended to incorporate FCEP into the continuing education programs developed for healthcare workers and the care quality evaluations as a step toward reducing the potential implications of hyperphosphatemia such as frequent hospitalization and health deterioration for this group of patients.
The authors believe that further research must still be conducted on the impact of family-centered empowerment programs focusing on home care as well as distance education on patients’ adherence to treatment and control of hyperphosphatemia. The most important limitation of this study was the poor cooperation and impatience of some participants due to the concurrence of FCEP and administration of research tools with their hemodialysis procedure, which may have affected the results. Although this study was performed in one hospital in Iran, the authors believe that the findings can be generalized to the entire country and even other countries.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon reasonable request.
Notes
The MMAS-8 Scale, content, name, and trademarks are protected by US copyright and trademark laws. Permission for use of the scale and its coding is required. A license agreement is available from MMAR, LLC., www.moriskyscale.com.
References
Yin J, Yin J, Lian R, Li P, Zheng J. Implementation and effectiveness of an intensive education program on phosphate control among hemodialysis patients: a non-randomized, single-arm, single-center trial. BMC Nephrol. 2021;22(1):243. https://doi.org/10.1186/s12882-021-02441-8.
St-Jules DE, Rozga MR, Handu D, Carrero JJ. Effect of phosphate-specific diet therapy on phosphate levels in adults undergoing maintenance hemodialysis: A systematic review and meta-analysis. Clin J Am Soc Nephrol. 2021;16(1):107–20. https://doi.org/10.2215/CJN.09360620.
Brauer A, Waheed S, Singh T, Maursetter L. Improvement in hyperphosphatemia using phosphate education and planning talks. J Ren Nutr. 2019;29(2):156–62. https://doi.org/10.1053/j.jrn.2018.06.004.
Rastogi A, Bhatt N, Rossetti S, Beto J. Management of hyperphosphatemia in end-stage renal disease: A new paradigm. J Ren Nutr. 2021;31(1):21–34. https://doi.org/10.1053/j.jrn.2020.02.003.
Umeukeje EM, Mixon AS, Cavanaugh KL. Phosphate-control adherence in hemodialysis patients: current perspectives. Patient Prefer Adherence. 2018;12:1175. https://doi.org/10.2147/PPA.S145648.
Lim JH, Chinna K, Khosla P, Karupaiah T, Daud ZAM. Understanding how nutrition literacy links to dietary adherence in patients undergoing maintenance hemodialysis: A theoretical exploration using partial least squares structural equation modeling. Int J Environ Res Public Health. 2020;17(20):7479. https://doi.org/10.3390/ijerph17207479.
Lambert K, Mullan J, Mansfield K. An integrative review of the methodology and findings regarding dietary adherence in end stage kidney disease. BMC Nephrol. 201723;18(1):318. https://doi.org/10.1186/s12882-017-0734-z.
Karavetian M, Rizk R. Patient education for hyperphosphatemia management: Improving outcomes while decreasing costs? Kidney Res Clin Pract. 2018;37(1):4–7. https://doi.org/10.23876/j.krcp.2018.37.1.4.
Yangöz ŞT, Özer Z, Boz İ. Comparison of the effect of educational and self-management interventions on adherence to treatment in hemodialysis patients: A systematic review and meta-analysis of randomized controlled trials. Int J Clin Pract. 2021;75(5):e13842. https://doi.org/10.1111/ijcp.13842.
Baumgart A, Manera KE, Johnson DW, Craig JC, Shen JI, Ruiz L, et al. Meaning of empowerment in peritoneal dialysis: focus groups with patients and caregivers. Nephrol Dial Transplant. 2020;35(11):1949–58. https://doi.org/10.1093/ndt/gfaa127.
Ashghali Farahani M, Ghane G, Sydfatemi N, Hagani H. Effect of educational program on the burden of family caregivers of hemodialysis patients. Evidence Based Care. 2016;6(1):7–18. https://doi.org/10.22038/EBCJ.2016.6703.
El-Melegy OA, Al-Zeftawy AM, Khaton SE. Effect of family centered empowerment model on hemodialysis patients and their caregivers. J Nurs Educ Pract. 2016;6(11):119–32. https://doi.org/10.5430/jnep.v6n11p119.
Shahdadi H, Rahdar Z, Mansouri A, Abdollahimohammad A. The effect of family-centered empowerment model on the level of death anxiety and depression in hemodialysis patients. Revista Publicando. 2018;5(16 (1):470–82.
Chan MW, Cheah HM, Padzil MBM. Multidisciplinary education approach to optimize phosphate control among hemodialysis patients. Int J Clin Pharm. 2019;41(5):1282–9. https://doi.org/10.1007/s11096-019-00878-4.
Lim E, Hyun S, Lee JM, Kim S, Lee M-J, Lee S-M, et al. Effects of education on low-phosphate diet and phosphate binder intake to control serum phosphate among maintenance hemodialysis patients: A randomized controlled trial. Kidney Res Clin Pract. 2018;37(1):69. https://doi.org/10.23876/j.krcp.2018.37.1.69.
Stumm E, Kirchner R, Guido L, Benetti E, Belasco A, Sesso R. Educational nursing intervention to reduce the hyperphosphatemia in patients on hemodialysis. Rev Bras Enferm. 2017;70(1):26–33. https://doi.org/10.1590/0034-7167-2016-0015.
Kawate Y, Miyata H. The importance of nutritional intervention by dietitians for hyperphosphatemia in maintained hemodialysis patients. Ren Replace Ther. 2017;3(1):1–13. https://doi.org/10.1186/s41100-017-0095-x.
Covic A, Rastogi A. Hyperphosphatemia in patients with ESRD: assessing the current evidence linking outcomes with treatment adherence. BMC Nephrol. 2013;14(1):153. https://doi.org/10.1186/1471-2369-14-153.
Li J, Wang L, Han M, Xiong Y, Liao R , Yupei Li, et al. The role of phosphate-containing medications and low dietary phosphorus-protein ratio in reducing intestinal phosphorus load in patients with chronic kidney disease. Nutr Diabetes. 2019;9(1):14. https://doi.org/10.1038/s41387-019-0080-2.
Hjemås BJ, Bøvre K, Mathiesen L, Lindstrøm JC, Bjerknes K. Interventional study to improve adherence to phosphate binder treatment in dialysis patients. BMC Nephrol. 2019;20(1):1–10. https://doi.org/10.1186/s12882-019-1334-x.
Chiang YC, Chang YP, Lin SC, Lin C, Hsu PH, Hsu YJ, Wu TJ. Effects of individualized dietary phosphate control program with a smartphone application in hemodialysis patients in Taiwan. Biol Res Nurs. 2021;23(3):375–81. https://doi.org/10.1177/1099800420975504.
Vasli P, Dehghan-Nayeri N, Khosravi L. Factors affecting knowledge transfer from continuing professional education to clinical practice: Development and psychometric properties of a new instrument. Nurse Educ Pract. 2018;28:189–95. https://doi.org/10.1016/j.nepr.2017.10.032.
Ayre C, Scally AJ. Critical values for Lawshe’s content validity ratio: revisiting the original methods of calculation. Meas Eval Couns Dev. 2014;47(1):79–86. https://doi.org/10.1177/0748175613513808.
Morisky DE, et al. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10(5):348–54. https://doi.org/10.1111/j.1751-7176.2008.07572.x.
Martinez-Perez P, Orozco-Beltrán D, Pomares-Gomez F, Hernández-Rizo JL, Borras-Gallen A, Gil-Guillen VF, et al. Validation and psychometric properties of the 8-item Morisky Medication Adherence Scale (MMAS-8) in type 2 diabetes patients in Spain. Aten Primaria. 2021;53(2):101942. https://doi.org/10.1016/j.aprim.2020.09.007.
Silavanich V, Nathisuwan S, Phrommintikul A, Permsuwan U. Relationship of medication adherence and quality of life among heart failure patients. Heart Lung. 2019;48(2):105–10. https://doi.org/10.1016/j.hrtlng.2018.09.009.
Berlowitz DR, Foy CG, Kazis LE, Bolin L, Lonroy LB, Fitzpatrick P, et al. for the SPRINT Study Research Group. Effect of intensive blood pressure therapy on patient-reported outcomes. N Engl J Med. 2017; 377(8): 733–744. https://doi.org/10.1056/NEJMoa1611179.
Bress AP, Bellows BK, King J, Hess R Beddhu S, Zhang Z, et al. for the SPRINT research group and the SPRINT Economics and Health Related Quality of Life Subcommittee. Cost-effectiveness of intensive versus standard blood pressure control. N Engl J Med. 2017; 377(8): 745–755. https://doi.org/10.1056/NEJMsa1616035.
Milazi M, Bonner A, Douglas C. Effectiveness of educational or behavioral interventions on adherence to phosphate control in adults receiving hemodialysis: a systematic review. JBI Evid Synth. 2017;15(4):971–1010. https://doi.org/10.11124/jbisrir-2015-1880.
Shimada M, Shutto-Uchita Y, Yamabe H. Lack of awareness of dietary sources of phosphorus is a clinical concern. In Vivo. 2019;33(1):11–6. https://doi.org/10.21873/invivo.11432.
Montazami M, Khalifehzadeh-Esfahani A, Keshvari M. Investigating the effect of family-centered self-care program based on home visits regarding dietary and medication regimen adherence of discharged patients with acute coronary syndrome. Iran J Nurs Midwifery Res. 2021;26(2):113. https://doi.org/10.4103/ijnmr.IJNMR_105_19.
Asgari P, Zolfaghari M, Shaabani A. Can addressing Family education improve adherence of therapeutic regimen in hemodialysis patients? A Randomized Controlled Clinical Trial. Nurs Pract Today. 2015;2(1):4–9.
Dawson J, Howell M, Howard K, Campbell KL, Craig JC, Tong A, et al. Cost-effectiveness of a mobile phone text messaging program (KIDNEYTEXT) targeting dietary behaviors in people receiving hemodialysis. J Hum Nutr Diet. 2022;35(5):765–73. https://doi.org/10.1111/jhn.12937.
Rabiei L, Eslami AA, Abbasi M, Afzali SM, Hosseini SM, Masoudi R. Evaluating the effect of family-centered intervention program on care burden and self-efficacy of hemodialysis patient caregivers based on social cognitive theory: A randomized clinical trial study. Korean J Fam Med. 2020;41(2):84. https://doi.org/10.4082/kjfm.18.0079.
Tao WW, Tao XM, Wang Y, Bi SH. Psycho-social and educational interventions for enhancing adherence to dialysis in adults with end-stage renal disease: A meta-analysis. J Clin Nurs. 2020;29(15–16):2834–48. https://doi.org/10.1111/jocn.15301.
Alikari V, Tsironi M, Matziou V, Tzavella F, Stathoulis J, Babatsikou F, et al. The impact of education on knowledge, adherence and quality of life among patients on haemodialysis. Qual Life Res. 2019;28(1):73–83. https://doi.org/10.1007/s11136-018-1989-y.
Bahramnezhad F, Asgari P, Zolfaghari M, Afshar PF. Family-centered education and its clinical outcomes in patients undergoing hemodialysis short running. Iran Red Crescent Med J. 2015;17(6). e20705. https://doi.org/10.5812/ircmj.17(5)2015.20705.
Acknowledgements
We would like to thank managers and patients at Shahid beheshti hospital in Hamedal for their assistance and cooperation.
Funding
No funding or sponsorship was received for this study or publication of this article.
Author information
Authors and Affiliations
Contributions
Conceptualization and methodology: Parvaneh Vasli, and Noushin Bakhtiari; Formal analysis and investigation: Noushin Bakhtiari, Parvaneh Vasli, and Malihe Nasiri; Writing-original draft: Parvaneh Vasli; Writing– review and editing: Meimanat Hosseini.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All the measures taken in this study were approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (SBMU), Tehran, Iran (code no. IR.SBMU.PHNM.1400.104) in agreement with the ethical standards of the 1964 Declaration of Helsinki and its later amendments. Informed consent was obtained from all the participants or legal guardians of the illiterate participants for participation in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vasli, P., Hosseini, M., Nasiri, M. et al. Family-centered empowerment approach to optimize phosphate management among hemodialysis patients: an experimental study. BMC Nephrol 24, 259 (2023). https://doi.org/10.1186/s12882-023-03311-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-023-03311-1