Abstract
Background
Up to 60% of pediatric renal transplant recipients with end-stage renal disease due to primary focal and segmental glomerulosclerosis (FSGS) may develop recurrent disease. Such recurrence is associated with poor prognosis if no remission is achieved. We report a single center experience with a protocol based on plasmapheresis and increased immunosuppression that resulted in a high long-lived remission rate.
Methods
This retrospective cohort study included consecutive pediatric renal transplant patients with recurrent FSGS treated with a standardized protocol using plasmapheresis and cyclophosphamide to supplement usual post-transplant immunosuppression with calcineurin inhibitors and steroids. Relapse was defined as urinary protein/creatinine ratio > 1.0 g/g and remission as < 0.5 g/g.
Results
Seventeen patients with FSGS recurrence post-transplant were treated. All had therapy resistant FSGS in native kidneys and had been on dialysis from 4 to 10 years. Of the 17, one died perioperatively from a pulmonary thromboembolism. Fifteen others achieved a complete remission within 3 months of treatment for FSGS recurrence. After a median follow-up period of 4 years, there were no recurrences of significant proteinuria. One patient achieved remission with rituximab.
Conclusion
The addition of plasmapheresis and cyclophosphamide to a calcineurin- and steroid-based immunosuppression regime was highly successful in inducing high remission rates with recurrent FSGS. Prospective trials are needed to evaluate further the efficacy of increased immunosuppression along with plasmapheresis in this setting.
Similar content being viewed by others
Introduction
While renal transplantation is the treatment of choice for children with end-stage renal disease (ESRD) [1], some diseases such as primary focal and segmental glomerulosclerosis (FSGS) recur in the allograft and adversely affect graft outcomes if no remission is achieved [2,3,4,5]. Recurrence rate with FSGS as high as 60.5% have been reported, and concern for recurrence is widespread when considering renal transplantation in children with FSGS [6]. Although a large number of therapies have been employed to treat FSGS recurrence, there is currently no consensus treatment [2, 7] and most of the treatments have not been evidence-based.
Historically, plasmapheresis (PLEX) is the most widely used treatment modality for recurrent FSGS in both children and adults [2, 4]. One meta-analysis comprised of a single large series of 432 patients as well as several smaller case studies found a partial or complete remission rate of 71% with PLEX [8]. There may have been substantial reporting bias in this cohort, however, and the number of PLEX treatments varied sIgnificantly, with poor definition of other potentially beneficial concurrent therapies.
Similarly, the reports of PLEX efficacy in pediatric patients has varied. A recent publication in Pediatric Transplantation reported a limited impact of PLEX in treating FSGS recurrence [9], but on the other hand, a study of recurrent FSGS in Israeli children demonstrated a 78% partial or complete response, similar to the meta-analysis results [10]. There has also been interest coupling PLEX with Rituxumab or using LDL-apheresis rather than conventional plasma exchange, though reports of these approaches have also been limited [11,12,13].
Another approach for the treatment of FSGS has focused on increased immunosuppression along with PLEX [5]. Nathanson reported that 6/14 patients with FSGS recurrence achieved complete remission by using a combination of high dose cyclosporine, PLEX, and oral cyclophosphamide [5]. To discern if there were similar efficacy, we were interested in evaluating our experience with a similar protocol that adds cyclophosphamide to calcineurin inhibitors, steroids, and PLEX for post-transplant FSGS recurrence in children and adolescents.
Methods
Setting and study population
This study was performed at Fundación Valle del Lili Hospital in Cali, Colombia, a tertiary care university institution. Our long-standing pediatric renal transplant program keeps a local registry of all renal transplant patients at the institution. In our retrospective analysis, we included all patients < 18 years of age transplanted between 1998 and 2015 due to primary FSGS who manifested FSGS recurrence post-transplant and were treated with a protocol for FSGS recurrence based on the use of PLEX and addition of cyclophosphamide to baseline immunosuppression with a calcineurin inhibitor and steroids. This study was performed in accordance with the Declaration of Helsinki and was approved by the Fundación Valle del Lili ethics board committee. Informed written consent was waived by the Fundación Valle del Lili ethics board committee (“Comité de ética en Investigación Biomédica” in Spanish) since it was a retrospective cohort study without influencing patient care.
Definitions, anthropometrics, and laboratory measurements
Recurrence was defined as a serum albumin level below 3 g/dL, either in the setting of a urinary protein/creatinine ratio (UPC) > 1 g/g presenting in the first 24 to 72 h after transplantation or the later onset of UPC > 1 g/g post-transplant distinct from other events such as acute rejection, acute kidney injury, or chronic allograft nephropathy, all documented by biopsy. Remission was defined as UPC < 0.5 g/g and serum albumin level > 3 g/dL.
Height was measured without shoes on a wall mounted stadiometer and weight was measured without heavy clothes using either a digital or balance-beam scale. Body mass index (BMI) was calculated as weight (kg)/height (m2). We calculated age- and gender- independent height and weight z-scores as previously described, using the Ped(z) app with the WHO reference intervals [14].
Blood samples were collected in anticoagulant and lithium heparin tubes. Creatinine was isotope dilution-mass spectrometry traceable and measured using a calorimetric modified Jaffe method and alkaline picrate [15]. Estimated glomerular filtration rate (eGFR) was calculated from the average of the three height measurements and serum creatinine with the new modified Schwartz formula [16].
Peri- and post-transplant management
-
(a)
All living donor (LD) recipients received 3 pre-emptive PLEX treatments during the week prior to transplantation and IV cyclosporine at 3.5 mg/Kg/day over the 24 h prior to transplant.
-
(b)
Induction therapy was chosen at the discretion of the transplant surgeon or the transplant nephrologist and varied by era of transplantation. Five patients (29.4%) received thymoglobulin at a dose of 1–1.5 mg/kg/dose for a total of 4 daily doses maximum. Twelve patients (70.5%) received a monoclonal anti IL-2 receptor antibody (basiliximab or daclizumab). Basiliximab was given at a dose of 20 mg in children < 20 Kg (n = 8 [80%]) or 30 mg in larger children, with the first dose on the day of transplant and the second dose on day 4. Daclizumab (n = 7 [41.1%]) was provided at a dose of 1 mg/kg on the day of transplant and a second similar dose 2 weeks later.
-
(c)
Steroid therapy: IV Prednisolone (10 mg/kg) daily for 3 days followed by oral prednisone tapering (1 mg/kg/day) over 2 months to a maintenance dose of 0.2 mg/kg/day for 2 years. Steroids were then tapered to alternate day for one more year and then discontinued.
-
(d)
Calcineurin inhibitor therapy: High dose microemulsified cyclosporine A was prescribed at 8–10 mg/kg/day every 12 h, targeting a C2 level of 1200–1500 mcg/L, for 3 months. If the patients had no recurrence, they were then transitioned from cyclosporine to tacrolimus at a dose of 0.1–0.2 mg/kg/day. Trough target levels of tacrolimus were 8–10 μg/L for 6 months and then 6–8 μg/L.
-
(e)
Mycophenolate mofetil (MMF) at 600–900 mg/m2/day. No MMF monitoring was employed.
-
(f)
Cytomegalovirus Prophylaxis: Since 2008, all patients received daily oral valganciclovir prophylaxis (7 mg/m2 x creatinine clearance [16]) for cytomegalovirus prophylaxis for a total of 6 months.
Treatment protocol for FSGS recurrence
-
(g)
Upon diagnosis of recurrence, PLEX was initiated with 4 daily sessions, followed by every other day sessions as long as UPC > 0.5. If after 15 PLEX sessions there was no significant improvement in proteinuria, PLEX was discontinued. PLEX treatments consisted of 1.5 plasma volume exchange swith 5% albumin as replacement fluid through a central vascular access using a Cobe Spectra System.
-
(h)
Cyclophosphamide: Oral cyclophosphamide was prescribed at 2 mg /kg/day daily once daily for 3 months in all patients who had FSGS recurrence, regardless of the cumulative dose of cyclophosphamide that may have been provided prior to transplantation to treat native FSGS. When cyclophosphamide was started, MMF was held. When cyclophosphamide was completed, MMF was re-started at 600–900 mg/m2/day.
-
(i)
Calcineurin inhibitors: As detailed above, microemulsified cyclosporine A at a dose of 8–10 mg/kg/day in two divided doses was provided, targeting a C2 level of 1200–1500 mcg/L, for 3 months. If remission were achieved, patients were then converted after 3 months to tacrolimus at a dose of 0.1–0.2 mg/kg/day, targeting through levels of 8–10 μg/L during the first year, and then 6–8 μg/L thereafter.
-
(j)
Rituximab: In one child who had persistent leukopenia during cyclophosphamide therapy, a single dose of rituximab 375 mg/m2 was provided when the cyclophosphamide therapy needed to be stopped prior to its full provision. In a second patient with partial remission after PLEX and completion of cyclophosphamide, rituximab was also provided, with four weekly doses of 375 mg/m2.
Statistical methods
Anthropometric z-scores were calculated using the app Ped(z) based on WHO growth charts [14]. We used simple descriptive statistics wherever possible. Continuous variables were analyzed for normal distribution using the D’Agostino-Pearson normality test. No adjustments were made for missing data. All calculations were performed using GraphPad Prism version 5.0f for Mac or STATA 14.0 for PC registered to LTC.
Results
Nineteen children with end-stage renal failure due to primary FSGS received their first kidney transplant at Fundación Valle del Lili and were part of the local transplant registry. Seventeen (89.4%) experienced recurrence of FSGS and were treated according to the protocol outlined above. Table 1 presents demographic and clinical management characteristics of transplanted children with recurrence.
Eleven patients (64.7%) were boys. The median age at diagnosis of primary FSGS was 8 years (IQR 6.1–10.3). None of the patients was HIV positive, diabetic, or obese, or had any other cause of secondary FSGS. Genetic studies were not performed prior to transplantation in any child.
Prior to ESRD diagnosis, 14 of the 17 patients manifested steroid-resistance, with one child showing partial responsiveness. Prior to ESRD, all children had also been treated with non-steroid immunosuppression trying to induce FSGS remission, including 7 who received cyclosporine, 17 who received cyclophosphamide, and 2 who received Rituximab.
All children reached ESRD and required dialysis prior to transplantation (range 4–10 years). Ten patients (58%) required nephrectomy prior to transplant due to ongoing nephrosis or severe proteinuria. The median age at transplant was 14.3 years (IQR 10.8–17.2). Ten patients (58.8%) had a living donor graft and 7 (41.2%) a deceased donor graft. There were no differences in patient characteristics between children who received living related and deceased donor transplants.
In the 17 patients with recurrent FSGS who received post-transplant PLEX and augmented immunosuppression per protocol, the median number of PLEX procedures provided was 9 (IQR 6–11). Complete remission was achieved by 15 patients after starting PLEX and augmenting immunosuppression, with an additional patient achieved remission with the addition of rituximab after not responding to the course of cyclophosphamide and PLEX. One patient died of a pulmonary thromboembolism within 2 weeks of transplant while receiving PLEX therapy for recurrence in a still-functioning graft.
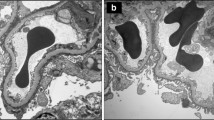
Nine patients had cellular and perihiliar variants two patients had no otherwise specified three patients had three patient had cellular variant and three had perihiliar variant [16].
Table 2 details quantification of proteinuria longitudinally. All patients who achieved remission stayed in remission without further disease recurrence during follow-up (median 4 years; IQR 2.2–7.8 years). In the single patient who did not remit, proteinuria transiently exacerbated further about 3 months after transplant concomitant with medication non-adherence, but then returned to prior levels.
Table 3 details graft function by estimated GFR. Median estimated GFR stayed stable during the first year after transplant. At last follow-up at a median of 4 years after transplant, there had been a median decline of eGFR by 15 ml/min/1.73 M2.
Regarding post-transplant infections, 2 (12%) had bacteremia due to Staphylococcus aureus, 2 (12%) 2 had bacteremia due to Kleibsella pneumoniae and 1 (6%) due to Acinetobacter baumanii. There were no cases of BKV polyoma infection, herpes virus infection or urinary tract infection. All patients received antibiotic prophylaxis during the first month after transplant.
In the child with persistent nephrosis, graft function was lost 64 months after transplant. Three other grafts were also lost during long-term follow-up: one related to inability to obtain immunosuppression and the others related to chronic allograft nephropathy. None of these patients had significant proteinuria at the time of graft loss. All patients who lost grafts subsequently died while on dialysis, two of infection, one from sequelae of a hypertensive crisis, and one as a young adult of colon cancer after having had another kidney transplant that also failed due to FSGS recurrence.
Discussion
In this single center retrospective review of 17 children transplanted due to FSGS, 15 or 88% had recurrent disease and were treated for their recurrence with a protocol using PLEX and augmentation of immunosuppression. Of the children with recurrence, 15 or 88% were able to enter a long-lived complete remission. In all but one case, the remissions occurred quickly after institution of therapy for recurrence, and only one child required supplemental therapy with the addition of rituximab after not fully remitting after PLEX and cyclophosphamide provision.
Although a large meta-analysis of patients with FSGS recurrence demonstrated a similar 71% rate of response with PLEX-based therapies, nearly 30% achieved only a partial remission, and the number of PLEX sessions and the duration of PLEX therapy was often substantial. In comparison, the children described in our report tended to have rapid and complete responses, and there were no subsequent relapses during long-term follow up. Moreover, eGFR remained acceptable long-term, with eGFR decline over time like rates seen more generally in children.
There is currently no consensus about the best overall approach for the treatment of recurrent FSGS in children [2, 6, 7], largely due to the lack of prospective randomized controlled trials. Moreover, although PLEX is quite often used as a first-line therapy for recurrence, it is almost always provided in the setting of other additional therapies, and there is little data to guide clinicians as to the specific efficacy of individual components of such multi-tiered management [17].
The decision to augment immunosuppression in FSGS recurrence in children is further complicated since most of these children have already had significant pre-transplant exposure to immunosuppression as part of attempts to reverse FSGS in their native kidneys. Concerns for cumulative toxicity of certain medications, such as cyclophosphamide, may lead to decisions to forgo the use of what may be an efficacious therapy, especially when there is not clarity as to the best overall therapy or the best population for that drug’s efficacy. In the patient with colorectal cancer, the time between the use of cyclophosphamide and the appearance of colorectal cancer was 3 years. A cause-effect relationship cannot be confirmed or ruled out.
The paucity of prospective controlled studies not only exacerbates the lack of clarity as to best current management strategies but also complicates the assessment of novel therapies as they become available. For instance, rituximab and LDL-apheresis have both been used increasingly to treat FSGS recurrence, but their utility in children with recurrent disease in general is difficult to assess when there has been little formal assessment of current therapies to allow baseline levels of expectation.
The importance of identifying the best therapies is underscored by long-term outcomes in successfully transplanted patients as compared to those with failed allografts. FSGS recurrence that does not respond to treatment leads to early graft loss and return to dialysis, and most often pretends future episodes of recurrence with subsequent transplantation. The long-term reliance on dialysis for renal replacement therapy adversely affects quality of life, requires more health care resources and is more costly, and results in significantly shorter life expectancy. In our own cohort, despite the successful treatment of recurrence in almost all patients, those who went on to lose graft function for other reasons and then required chronic dialysis as young adults all had limited life spans.
This study has some limitations. First, among patients with nephrotic syndrome, there is a low incidence of FSGS that leads to chronic kidney failure and requires a transplant, which explains the low number of patients presented in this study [18]. Second, due to the lengthy collection time, the patients were subjected to different types of management and different clinical concept, which may lead to information bias. However, this study has strengths. The study was conducted in a tertiary care center. Long-term follow-up was possible in these patients from their nephrotic syndrome diagnosis.
Although the conclusions that can be drawn from our results may not be generalizable to all children with recurrent FSGS, our report does show that in some children an aggressive approach to recurrence that uses PLEX and immunosuppression augmentation including cyclophosphamide can lead to rapid, complete, long-term remission. Rigorous assessment of proposed protocols and their effectiveness in children with FSGS should help to determine what therapies need to be studied in a randomized, controlled fashion in children and underscore the importance of sharing results such as described with this reported cohort to the pediatric nephrology community at large.
Conclusion
The addition of plasmapheresis and cyclophosphamide to a calcineurin- and steroid-based immunosuppression regime was highly successful in inducing high remission rates with recurrent FSGS. Prospective trials are needed to evaluate further the efficacy of increased immunosuppression along with plasmapheresis in this setting.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available to protect patient information but are available from the corresponding author on reasonable request.
References
Filler G. Challenges in pediatric transplantation: the impact of chronic kidney disease and cardiovascular risk factors on long-term outcomes and recommended management strategies. Pediatr Transplant. 2011;15:25–31. https://doi.org/10.1111/J.1399-3046.2010.01439.X.
Francis A, Didsbury M, McCarthy H, Kara T. Treatment of recurrent focal segmental glomerulosclerosis post-kidney transplantation in Australian and New Zealand children: a retrospective cohort study. Pediatr Transplant. 2018;22. https://doi.org/10.1111/petr.13185.
Baum MA, Ho M, Stablein D, Alexander SR. Outcome of renal transplantation in adolescents with focal segmental glomeruelosclerosis. Pediatr Transplant. 2002:488–92. https://doi.org/10.1034/j.1399-3046.2002.02036.x.
Runowski D, Prokurat S, Rubik J, Grenda R. Therapeutic plasma exchange in pediatric renal transplantation experience of one decade and 389 sessions. Transplant Proc. 2018;50:3483–6. https://doi.org/10.1016/j.transproceed.2018.07.015.
Nathanson S, Cochat P, André JL, Guyot C, Loirat C, Nivet H, et al. Recurrence of nephrotic syndrome after renal transplantation: influence of increased immunosuppression. Pediatr Nephrol. 2005;20:1801–4. https://doi.org/10.1007/s00467-005-2053-z.
Cormican S, Kennedy C, O’Kelly P, Doyle B, Dorman A, Awan A, et al. Renal transplant outcomes in primary FSGS compared with other recipients and risk factors for recurrence: a national review of the Irish transplant registry. Clin Transpl. 2018;32. https://doi.org/10.1111/ctr.13152.
Filler G, Restrepo JM. The urgent need for more research on how to treat recurrent focal and segmental glomerulosclerosis. Pediatr Transplant. 2018;22. https://doi.org/10.1111/petr.13215.
Kashgary A, Sontrop JM, Li L, Al-Jaishi AA, Habibullah ZN, Alsolaimani R, et al. The role of plasma exchange in treating post-transplant focal segmental glomerulosclerosis: a systematic review and meta-analysis of 77 case-reports and case-series. BMC Nephrol. 2016;17. https://doi.org/10.1186/s12882-016-0322-7.
Verghese PS, Rheault MN, Jackson S, Matas AJ, Chinnakotla S, Chavers B. The effect of peri-transplant plasmapheresis in the prevention of recurrent FSGS. Pediatr Transplant. 2018;22. https://doi.org/10.1111/petr.13154.
Cleper R, Krause I, Bar Nathan N, Mor M, Dagan A, Weissman I, et al. Focal segmental glomerulosclerosis in pediatric kidney transplantation: 30 years’ experience. Clin Transpl. 2016;30:1324–31. https://doi.org/10.1111/ctr.12825.
Shah L, Hooper DK, Okamura D, Wallace D, Moodalbail D, Gluck C, et al. LDL-apheresis-induced remission of focal segmental glomerulosclerosis recurrence in pediatric renal transplant recipients. Pediatr Nephrol. 2019;34:2343–50. https://doi.org/10.1007/s00467-019-04296-6.
Raina R, Krishnappa V. An update on LDL apheresis for nephrotic syndrome. Pediatr Nephrol. 2019;34:1655–69. https://doi.org/10.1007/s00467-018-4061-9.
Filler G, Lee M, Hegele RA. Barriers to the implementation of lipoprotein apheresis in Canada. Can J Cardiol. 2017;33:409–11.
de Onis M, Onyango A, Borghi E, Siyam A, Blössner M, Lutter C, et al. Worldwide implementation of the WHO child growth standards. Public Health Nutr. 2012;15:1603–10. https://doi.org/10.1017/S136898001200105X.
Matas AJ, Smith JM, Skeans MA, Thompson B, Gustafson SK, Schnitzler MA, et al. OPTN/SRTR 2012 annual data report: kidney. Am J Transplant. 2014;14(SUPPL. 1):11–44. https://doi.org/10.1111/ajt.12579.
Zhong Y, Xu F, Li X, Chen H, Liang S, Zhu X, et al. The evolution of morphological variants of focal segmental glomerulosclerosis: a repeat biopsy-based observation. Nephrol Dial Transplant. 2016;31:87–95. https://doi.org/10.1093/NDT/GFV245.
Kang HG, Ha IS, Il CH. Recurrence and treatment after renal transplantation in children with FSGS. Biomed Res Int. 2016;2016. https://doi.org/10.1155/2016/6832971.
Bouts A, Veltkamp F, Tönshoff B, Vivarelli M. European Society of Pediatric Nephrology survey on current practice regarding recurrent focal segmental glomerulosclerosis after pediatric kidney transplantation. Pediatr Transplant. 2019;23. https://doi.org/10.1111/petr.13385.
Acknowledgements
We thank the Lilibeth Caberto Kidney Clinical Research Unit, University of Western Ontario, in London Ontario, for the generous assistance with research space and infrastructure. We thank the Centro de Investigaciones Clinicas of Fundación Valle del Lili for the strong support given during the entire research process. Dra. Laura Torres-Canchala was generously supported by the International Society of Nephrology for a 2 month research sabbatical at the University of Western Ontario.
Funding
This study was supported by the International Society of Nephrology (ISN) through the ISN Sister Renal Center Program: Boston Children’s Hospital USA - Fundación Valle del Lili, Cali, Colombia.
Author information
Authors and Affiliations
Contributions
JMR conceived the study, designed the study, and obtained ethics approval. JMR was involved in all aspects of the paper generation and revised each draft, contributed to the statistical analysis, and coordinated all coauthors’ activities. HL, and EM collected all the data. LTC performed the statistical analysis. MJGS, LTC and JMR wrote the different versions. LTC also prepared the tables and figures. All authors interpreted the data. All authors provided critical input into all aspects of the design and execution of the study and participated in all phases of the study. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was in accordance with the Declaration of Helsinki and was approved by the Fundación Valle del Lili ethics board committee (“Comité de ética en Investigación Biomédica” in Spanish). Informed written consent was waived by the Fundación Valle del Lili ethics board committee (“Comité de ética en Investigación Biomédica” in Spanish) since it was a retrospective cohort study without influencing patient care.
Consent for publication
Not applicable.
Competing interests
All the authors declare no competing interest related to this research.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Restrepo, J.M., Torres-Canchala, L., Londoño, H. et al. Treatment of post-transplant recurrent FSGS in children using plasmapheresis and augmentation of immunosuppression. BMC Nephrol 23, 131 (2022). https://doi.org/10.1186/s12882-022-02768-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-022-02768-w