Abstract
Background
Chronic kidney disease (CKD) is a global public health concern, but its disease burden and risk-attributable burden in CKD has been poorly studied in low - and middle-income countries (LMICs). This study aimed to estimate CKD burden and risk-attributable burden in LMICs from 1990 to 2019.
Methods
Data were collected from the Global Burden of Disease (GBD) Study 2019, which measure CKD burden using the years lived with disability (YLDs), years of life lost (YLLs), disability-adjusted life-years (DALYs) and calculate percentage contributions of risk factors to age-standardized CKD DALY using population attributable fraction (PAF) from 1990 to 2019. Trends of disease burden between 1990 and 2019 were evaluated using average annual percent change (AAPC). The 95% uncertainty interval (UI) were calculated and reported for YLDs, YLLs, DALYs and PAF.
Results
In 2019, LICs had the highest age-standardized DALY rate at 692.25 per 100,000 people (95%UI: 605.14 to 785.67), followed by Lower MICs (684.72% (95%UI: 623.56 to 746.12)), Upper MICs (447.55% (95%UI: 405.38 to 493.01)). The age-standardized YLL rate was much higher than the YLD rate in various income regions. From 1990 to 2019, the age-standardized DALY rate showed a 13.70% reduction in LICs (AAPC = -0.5, 95%UI: − 0.6 to − 0.5, P < 0.001), 3.72% increment in Lower MICs (AAPC = 0.2, 95%UI: 0.0 to 0.3, P < 0.05). Age-standardized YLD rate was higher in females than in males, whereas age-standardized rates of YLL and DALY of CKD were all higher in males than in females in globally and LMICs. Additionally, the YLD, YLL and DALY rates of CKD increased with age, which were higher in aged≥70 years in various income regions. In 2019, high systolic blood pressure, high fasting plasma glucose, and high body-mass index remained the major causes attributable age-standardized CKD DALY. From 1990 to 2019, there were upward trends in the PAF of age-standardized DALY contributions of high fasting plasma glucose, high systolic blood pressure, and high body-mass index in Global, LICs, Lower MICs and Upper MICs. The greatest increase in the PAF was high body-mass index, especially in Lower MICs (AAPC = 2.7, 95%UI: 2.7 to 2.8, P < 0.001). The PAF of age-standardized DALY for high systolic blood pressure increased the most in Upper MICs (AAPC = 0.6, 95%UI: 0.6 to 0.7, P < 0.001).
Conclusions
CKD burden remains high in various income regions, especially in LICs and Lower MICs. More effective and targeted preventive policies and interventions aimed at mitigating preventable CKD burden and addressing risk factors are urgently needed, particularly in geographies with high or increasing burden.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is a global public health concern [1], and a risk factor for adverse outcomes in other diseases [2, 3]. CKD can be defined as a sustained damage of renal parenchyma that leads to chronic deterioration of renal function and may gradually progress to end-stage renal disease (ESRD) [4]. Without kidney replacement therapy (dialysis or kidney transplantation), ESRD remains uniformly fatal [4]. Studies have shown that kidneys are linked to Coronavirus disease 2019 (COVID-19) infection [5]. COVID-19 has been declared as a global pandemic by the World Health Organization [5], and the incidence of acute kidney injury (AKI) in patients infected with COVID-19 is around 3–15% [6, 7]. AKI can cause ESRD directly, and increase the risk of developing incident CKD and worsening of underlying CKD [8]. According to the Global Burden of Disease (GBD) study, disability-adjusted life-years (DALYs) for CKD has risen from 29th in 1990 to 18th in 2019 [9]. The global burden of CKD is rapidly increasing and is projected to become the 5th most common cause of years of life lost worldwide by 2040 [10, 11], with the burden of CKD increasing faster in low - and middle-income countries (LMICs) [12]. The burden of CKD is studied predominantly in high-income countries, with few studies in LMICs, and even fewer studies on attributable disease burden [2]. In this study, we aimed to analyzed and compared the trends of disease burden of CKD as well as its attributable disease burden in LMICs from 1990 to 2019, by using the data from the GBD 2019 study.
Methods
Data sources
Data for this study were obtained from the GBD 2019 study. The GBD 2019 provides estimates of years lived with disability (YLDs), years of life lost (YLLs), and disability-adjusted life-years (DALYs) disaggregated due to 369 diseases and injuries, and 87 risk factors and combinations of risk factors in 204 countries and territories from 1990 to 2019 [9, 13]. Detailed methods of GBD 2019 have been published elsewhere [9, 13]. The GBD 2019 attributable burden estimates followed the general framework established for comparative risk assessment (CRA) [14, 15]. Compared with previous GBD studies [16,17,18], the GBD 2019 study developed new approaches to estimate risk exposure and risk-attributable burden by integrating all accessible data from multiple epidemiological studies in various countries [13]. These studies included high-quality systematic reviews, cohorts, trials, case-control studies and other observational studies [13].
This study adherence to the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) recommendations [19]. All data used in this study were obtained from the Institute for Health Metrics and Evaluation (IHME) website [20].
In the GBD study, chronic kidney disease was recognized as a disease as well as a metabolic risk factor [21]. In this analysis, we treated chronic kidney disease as a disease. CKD was defined as eGFR (estimated glomerular filtration rate) of < 60 mL/min per 1.73 m2 [21].
Definitions
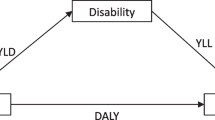
We used years lived with disability (YLDs), years of life lost (YLLs) and disability-adjusted life-years (DALYs) to measure the burden caused by CKD. YLDs measures the amount of time people lose to diseases and injuries that degrade their level of health but do not cause death. YLLs is a measure of premature death within a group of people. DALYs is a comprehensive index to evaluate the disease burden of disability and premature death, it is calculated by adding the YLLs and the YLDs [22, 23].
Due to the potential effects of climate change on human health, two new risk factors (high and low non-optimal temperatures) have been added in GBD 2019 [13]. 7 risk factors, i.e. high temperature, low temperature, lead exposure, diet high in sodium, high systolic blood pressure, high fasting plasma glucose, high body mass index, were considered to be associated with CKD in GBD 2019.
In our analyses we classified countries according to World Bank Income Levels in 2019, a total of 137 low-and middle-income countries (LMICs) were categorized into three groups: 31 low-income countries (LICs), 47 lower-middle income countries (Lower MICs) and 59 upper-middle income countries (Upper MICs).
Statistical analyses
We computed counts, and age-standardized rates (per 100,000) to quantify the burden of CKD. YLDs, YLLs and DALYs were metrics used to measure the burden of CKD and reported by specific region, year, sex, age. Age-standardized rates (per 100,000) were standardized by the global age-standard population. The percentage contributions of risk factors to age-standardized CKD DALY were calculated by the population attributable fraction (PAF). Percentage change was used to show the magnitude of the change in YLDs, YLLs, DALYs and PAF from 1990 to 2019. Trends of disease burden between 1990 and 2019 were evaluated using average annual percent change (AAPC), which were calculated by the Joinpoint Regression Program (Version 4.9.0.0. March 2021) [24]. We considered P < 0.05 to be significant.
Uncertainty interval
For each estimated rate and number of YLDs, YLLs, DALYs, and PAF of risk-attributable CKD DALYs, we reported its 95% uncertainty interval (UI). 95% UI was calculated by taking 1000 draws from the posterior distribution of each quantity and using the 25th and 975th-ordered draw of the uncertainty distribution [25].
Results
CKD-related YLDs, YLLs and DALYs increased to varying degrees in various income regions from 1990 to 2019 (Table 1). In 2019, LICs had the highest age-standardized DALY rate at 692.25 per 100,000 people (95%UI: 605.14 to 785.67) in 2019, followed by Lower MICs (684.72% (95%UI: 623.56 to 746.12)), Upper MICs (447.55% (95%UI: 405.38 to 493.01)), while HICs (292.93% (95%UI: (263.61 to 322.94)) had the lowest rate. The age-standardized YLL rate was much higher than the YLD rate at the global level and in various income regions. From 1990 to 2019, the age-standardized YLD rate all showed an upward trend in various income regions(P < 0.001), while YLL rate decreased in LICs (AAPC = − 0.7, 95%UI: − 0.7 to − 0.7), P < 0.001) and Upper MICs (AAPC = -0.3, 95%UI: − 0.4 to − 0.2, P < 0.001). The age-standardized DALY rate showed a 6.27% increment in Global (AAPC = 0.3, 95%UI: 0.2 to 0.4, P < 0.001), 12.75% increment in HICs (AAPC = 0.6, 95%UI: 0.5 to 0.7, P < 0.001), 3.72% increment in Lower MICs (AAPC = 0.2, 95%UI: 0.0 to 0.3, P < 0.05), whereas decreased 13.70% from 802.15 per 100,000 people (95%UI: 716.50 to 893.68) in 1990 to 692.25 per 100,000 people (95%UI: 605.14 to 785.67) in 2019 in LICs (AAPC = -0.5, 95%UI: − 0.6 to − 0.5, P < 0.001), and 2.25% reduction in Upper MICs (AAPC = 0.1, 95%UI: 0.0 to 0.1, P = 0.150) (Tables 2 and 3).
In terms of gender, age-standardized YLD rate was higher in females than in males, whereas age-standardized rates of YLL and DALY of CKD were all higher in males than in females in globally and LMICs (Table 2). Additionally, the YLD, YLL and DALY rates of CKD increased with age in various income regions, which were higher in aged≥70 years (Fig. 1).
Among all 137 LMICs, the highest age-standardized YLD, YLL and DALY rates of CKD in 2019 were seen in Mexico 296.40 per 100,000 people (95% UI: 206.99 to 394.46), Micronesia (Federated States of) 1895.00 per 100,000 people (95% UI: 1313.85 to 2478.01) and Micronesia (Federated States of) 2162.73 per 100,000 people (95% UI: 1584.61 to 2761.55), respectively. Whereas the lowest age-standardized YLD, YLL and DALY rates were seen in Ukraine 56.53 per 100,000 people (95% UI: 39.81 to 75.38), Belarus 69.79 per 100,000 people (95% UI: 55.13 to 89.34) and Belarus 128.92 per100 000 people (95% UI: 104.56 to 156.45), respectively. From 1990 to 2019, the growth of age-standardized DALY rate varied from − 46.83% in Mongolia to 182.92% in El Salvador. The variations in other CKD burden metrics (YLDs, YLLs and DALYs) by country in 2019 can be found in Fig. 2 and Additional file.
There was much consistency in the PAF of CKD-related age-standardized DALYs for these risk factors in various income regions. In 2019, CKD-related risk factors with the top three PAF were high systolic blood pressure, high fasting plasma glucose and high body-mass index, which all are metabolic risks (Fig. 3). The PAF of CKD-related age-standardized DALYs for risk factors in 2019 were presented in Table 4.
From 1990 to 2019, there were upward trends in the PAF contributions of high fasting plasma glucose, high systolic blood pressure, and high body-mass index to age-standardized CKD DALY in Global, LICs, Lower MICs and Upper MICs (Table 4). Notably, the greatest increase in the PAF was attributed to high body-mass in various income regions, especially in Lower MICs (111.83% (95% UI: 66.28 to 196.48); AAPC = 2.7, 95%UI: 2.7 to 2.8, P < 0.001), followed by Upper MICs (73.58% (95% UI: 48.84 to 113.01); AAPC = 1.9, 95%UI: 1.9 to 2.0, P < 0.001) and LICs (70.37% (95% UI: 40.14 to 133.32); AAPC = 2.0, 95%UI: 1.8 to 2.2, P < 0.001). In addition, the PAF of age-standardized DALYs for high systolic blood pressure increased the most in Upper MICs (16.94% (95% UI: 12.55 to 22.01); AAPC = 0.6, 95%UI: 0.6 to 0.7, P < 0.001), whereas decreased in HICs (4.82% (95% UI: − 6.9 to − 2.81); AAPC = -0.3, 95%UI: − 0.3 to − 0.2, P < 0.001) (Fig. 4).
Discussion
Chronic kidney disease (CKD) is a significant global health problem and one of the top 20 causes of death worldwide. It is a serious threat to people’s life and health [26, 27]. CKD DALYs is calculated by adding the YLLs and the YLDs, we found that the age-standardized YLL rate is much higher than the YLD rate at the global level and in various income regions, suggesting that premature death is the main cause of CKD burden. The age-standardized YLD rates all showed an upward trend in LICs, Lower MICs and Upper MICs, the age-standardized YLL rates decreased in LICs and Upper MICs, suggesting that future CKD treatment strategies should focus on improving the quality of life of CKD patients.
Our results show disparities in CKD burden were also observed in geographical regions and countries. LICs had the highest age-standardized DALY rate, followed by Lower MICs, which may be related to different exposures to risk factors, weak health systems, inadequate health care funding, access to effective health care interventions [28]. These findings call for increased planning and interventions, and developed novel and more appropriate solutions to address the burden of CKD in these areas [10]. The greatest decline in age-standardized DALY rates of CKD were all seen in LICs. This may be related to the improvement of medical technology and effective health care reform. However, the age-standardized DALY rate showed an upward trend in Lower MICs. If these trends continue, the disparities that exist in CKD burden between Lower MICs and LICs and Upper MICs will be further increased.
Furthermore, our results showed that the CKD burden showed homogeneity by gender among global and LMICs: age-standardized YLD rate was higher in females than in males, whereas age-standardized rates of YLL and DALY of CKD were all higher in males than in females. The disease burden of CKD is mainly due to premature death in males and disability in females. This difference may be related to physiological differences, estrogen levels and lifestyle between males and females [29]. This gender difference should also be taken into account by policy makers when planning future strategies and implementing preventive and control measures. Additionally, the YLD, YLL and DALY rates of CKD increased with age, which were higher in aged ≥70 years in various income regions, speculated this change is largely related to the aging population and the increase of the elderly population. More attention should be paid to the older adults in the prevention and treatment of CKD.
In 2019, except for age and other non-modifiable risk factors, high systolic blood pressure, high fasting plasma glucose, and high body-mass index remained the major causes attributable age-standardized CKD DALY in LMICs. Unfortunately, there was no remarkable decline in PAF of them since 1990. This may be related to the increased incidence and prevalence of hypertension, dyslipidemia, overweight and obesity and sedentary lifestyle in the population over the past 30 years [30]. Therefore, more efforts are needed to create healthy lifestyles. Moreover, there were upward trends in the PAF of DALYs contributions of high systolic blood pressure, high fasting plasma glucose, and high body-mass in LMICs from 1990 to 2019. Perhaps most concerning are high body mass index, especially in Lower MICs, so it is imperative that effective measures be taken to curb the rise of obesity. There is clear evidence that interventions to manage hypertension and promote weight loss are associated with reduced risks of developing CKD and better outcomes among those living with CKD [31,32,33]. Therefore, it is important to develop relevant strategies and targeted measures to prevent and manage hypertension, diabetes, and obesity.
GBD 2019 for the first time included high and low temperatures exposure as a global risk factor [13]. This study indicated that the PAF attributable to low temperature exceeded the PAF attributable to high temperature in various income regions in 2019, but the PAF attributable to low temperature showed a downward trend. Generally, infrastructure, such as the spread of heating, housing insulation, and the prevalence of air conditioning are likely explanations [34]. In 1990, high temperatures displayed a protective effect, leading to a negative high-attributable PAF in LMICs. In the context of global climate change, however, the PAF of high temperatures induced CKD is increasing in various income regions, requiring more attention and intervention. Meanwhile, this study shows that LICs and Lower MICs have larger PAF due to high temperature in 2019. This may be because, compared to HICs and Upper MICs, LICs and Lower MICs has higher poverty ratios, fewer medical resources and temperature-control facilities, and most LICs and Lower MICs are in Africa having high exposure to heat [35, 36]. Climate warming may be a potential factor in exacerbating the inter-country health and socio-economic inequalities [35, 37]. Therefore, it is necessary to consider the impact of high temperature and take measures to improve climate resilience, especially in LICs and Lower MICs.
In addition to the seven risk factors for CKD quantified by GBD 2019, there are other potential and nontraditional factors that are likely to affect future global burden of CKD, for example, food insecurity, heavy metals, air pollution, persistent organic pollutants, war and displaced refugee populations and so on [38,39,40,41]. Further study of potential risk factors for CKD is also necessary in order to facilitate the development of targeted interventions. In addition, in the context of the pandemic of coronavirus disease 2019, although COVID-19 predominantly affects the respiratory system, it also involves multiple organs, such as the cardiovascular system, the liver as well as the kidneys [42]. Adverse renal manifestations, such as acute kidney injury (AKI), have been reported as a result of COVID-19. Studies have shown that AKI can directly cause ESRD, and increase the risk of developing incident CKD and worsening of underlying CKD [8]. CKD has not been sufficiently recognized due to its inconspicuous course during COVID-19 infection, especially in the early stage [42]. As the pandemic continues, more precise prevention policies may be needed to guide patients with chronic kidney disease. COVID-19 is a huge medical challenge that health care providers should recognize early and take appropriate action as soon as possible.
Limitations
Our study has several limitations. First, since data for this study is part of GBD 2019 study, all limitations of the GBD 2019 methods outlined elsewhere also apply here [9, 13]. The major limitation of the GBD analysis of the burden of diseases is the availability of primary data [9]. For exposure measurement, patterns of data availability are non-uniform across geography and over time and, where available, might be based on less reliable modes of data collection such as self-report [13]. Then, In the estimation of YLDs, the disability weight is derived from statistical data of multiple countries around the world, which is uncertainty in the estimation of disease in LMICs. In addition, a comprehensive assessment of the burden of disease should also include the economic, family and social aspects of the burden, so a multi-dimensional analysis can be considered to improve the accuracy of the results [43].
Conclusions
This study has evaluated the burden of CKD and its risk-attributable burden in 137 LMICs from 1990 to 2019. CKD burden remains high in various income regions, especially in LICs and Lower MICs. More effective and targeted preventive policies and interventions aimed at mitigating preventable CKD burden and addressing risk factors are urgently needed, particularly in geographies with high or increasing burden.
Availability of data and materials
Data for this study were obtained from the GBD 2019 study. This study adherence to the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) recommendations. All data used in this study were obtained from the Institute for Health Metrics and Evaluation (IHME) website (http://ghdx.healthdata.org/gbd-results-tool) [20]. And the public access to the database is open.
Change history
14 February 2022
A Correction to this paper has been published: https://doi.org/10.1186/s12882-022-02686-x
Abbreviations
- GBD:
-
Global Burden of Disease
- CKD:
-
Chronic kidney disease
- LMICs:
-
Low - and middle-income countries
- LICs:
-
Low-income countries
- Lower MICs:
-
Lower-middle income countries
- Upper MICs:
-
Upper-middle income countries
- HICs:
-
High-income countries
- YLD:
-
Years lived with disability
- YLL:
-
Years of life lost
- DALY:
-
Disability-adjusted life-years
- PAF:
-
Population-attributable faction
- UI:
-
Uncertainty interval
- AAPC:
-
Average annual percentage change
- AKI:
-
Acute kidney injury
- ESRD:
-
End-stage renal disease
- COVID-19:
-
Coronavirus disease 2019
References
Levey AS, Atkins R, Coresh J, Cohen EP, Collins AJ, Eckardt KU, et al. Chronic kidney disease as a global public health problem: approaches and initiatives - a position statement from kidney disease improving global outcomes. Kidney Int. 2007;72(3):247–59.
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet (London, England). 2020;395(10225):709–33.
Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association councils on kidney in cardiovascular disease, high blood pressure research, clinical cardiology, and epidemiology and prevention. Hypertension. 2003;42(5):1050–65.
Akchurin OM. Chronic kidney disease and dietary measures to improve outcomes. Pediatr Clin N Am. 2019;66(1):247–67.
Adapa S, Chenna A, Balla M, Merugu GP, Koduri NM, Daggubati SR, et al. COVID-19 pandemic causing acute kidney injury and impact on patients with chronic kidney disease and renal transplantation. J Clin Med Res. 2020;12(6):352–61.
Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97(5):829–38.
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet (London, England). 2020;395(10229):1054–62.
Chawla LS, Kimmel PL. Acute kidney injury and chronic kidney disease: an integrated clinical syndrome. Kidney Int. 2012;82(5):516–24.
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–22.
Li PK, Garcia-Garcia G, Lui SF, Andreoli S, Fung WW, Hradsky A, et al. Kidney health for everyone everywhere-from prevention to detection and equitable access to care. J Ren Care. 2020;46(1):4–12.
Foreman KJ, Marquez N, Dolgert A, Fukutaki K, Fullman N, McGaughey M, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet (London, England). 2018;392(10159):2052–90.
Stanifer JW, Muiru A, Jafar TH, Patel UD. Chronic kidney disease in low- and middle-income countries. Nephrol Dial Transplant. 2016;31(6):868–74.
Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1223–49.
Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: global burden of disease study. Lancet (London, England). 1997;349(9063):1436–42.
Murray CJ, Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S. Comparative quantification of health risks conceptual framework and methodological issues. Popul Health Metrics. 2003;1(1):1.
GBD 2016 risk factors collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet (London, England). 2017;390(10100):1345–422.
GBD 2017 risk factor collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (London, England). 2018;392(10159):1923–94.
GBD 2017 disease and injury incidence and prevalence collaborators. Global, regional, and national incidence, prevalence, And years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet (London, England). 2018;392(10159):1789–858.
Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet (London, England). 2016;388(10062):e19–23.
GBD results tool Institute for Health Metrics and Evaluation (IHME). GBD results tool. http://ghdx.healthdata.org/gbd-results-tool. (Accessed Mar 20, 2021).
Fraser SDS, Roderick PJ. Kidney disease in the global burden of disease study 2017. Nat Rev Nephrol. 2019;15(4):193–4.
GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet (London, England). 2018;392(10159):1859–922.
Liu S, Li Y, Zeng X, Wang H, Yin P, Wang L, et al. Burden of cardiovascular diseases in China, 1990-2016: findings from the 2016 global burden of disease study. JAMA Cardiol. 2019;4(4):342–52.
Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual per cent change in trend analysis. Stat Med. 2009;28(29):3670–82.
Kyu HH, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1859–922.
Bradshaw C, Kondal D, Montez-Rath ME, Han J, Zheng Y, Shivashankar R, et al. Early detection of chronic kidney disease in low-income and middle-income countries: development and validation of a point-of-care screening strategy for India. BMJ Glob Health. 2019;4(5):e001644.
Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1736–88.
Ameh OI, Ekrikpo UE, Kengne AP. Preventing CKD in low- and middle-income countries: a call for urgent action. Kidney Int Rep. 2020;5(3):255–62.
Jianhua L. Study on gender difference in the causes of death and disease burden of the residents in Chengyang District, Qingdao City, China: Shandong University; 2014.
Zhao Y, Yan H, Marshall RJ, Dang S, Yang R, Li Q, et al. Trends in population blood pressure and prevalence, awareness, treatment, and control of hypertension among middle-aged and older adults in a rural area of Northwest China from 1982 to 2010. PLoS One. 2013;8(4):e61779.
Luyckx VA, Tuttle KR, Garcia-Garcia G, Gharbi MB, Heerspink HJL, Johnson DW, et al. Reducing major risk factors for chronic kidney disease. Kidney Int Suppl (2011). 2017;7(2):71–87.
Stenvinkel P, Zoccali C, Ikizler TA. Obesity in CKD--what should nephrologists know? J Am Soc Nephrol. 2013;24(11):1727–36.
Jun M, Hemmelgarn BR. Strategies for BP control in developing countries and effects on kidney function. Clin J Am Soc Nephrol. 2016;11(6):932–4.
Burkart KG, Brauer M, Aravkin AY, Godwin WW, Hay SI, He J, et al. Estimating the cause-specific relative risks of non-optimal temperature on daily mortality: a two-part modelling approach applied to the global burden of disease study. Lancet (London, England). 2021;398(10301):685–97.
Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Beagley J, Belesova K, et al. The 2020 report of the lancet countdown on health and climate change: responding to converging crises. Lancet (London, England). 2021;397(10269):129–70.
Ramin BM, McMichael AJ. Climate change and health in sub-Saharan Africa: a case-based perspective. EcoHealth. 2009;6(1):52–7.
Levy BS, Patz JA. Climate change, human rights, and social justice. Ann Global Health. 2015;81(3):310–22.
Banerjee T, Crews DC, Wesson DE, Dharmarajan S, Saran R, Ríos Burrows N, et al. Food insecurity, CKD, and subsequent ESRD in US adults. Am J Kidney Dis. 2017;70(1):38–47.
Kim NH, Hyun YY, Lee KB, Chang Y, Ryu S, Oh KH, et al. Environmental heavy metal exposure and chronic kidney disease in the general population. J Korean Med Sci. 2015;30(3):272–7.
Clark-Cutaia MN, Rivera E, Iroegbu C, Squires A. Disparities in chronic kidney disease-the state of the evidence. Curr Opin Nephrol Hypertens. 2021;30(2):208–14.
Bowe B, Xie Y, Li T, Yan Y, Xian H, Al-Aly Z. Particulate matter air pollution and the risk of incident CKD and progression to ESRD. J Am Soc Nephrol. 2018;29(1):218–30.
Kunutsor SK, Laukkanen JA. Renal complications in COVID-19: a systematic review and meta-analysis. Ann Med. 2020;52(7):345–53.
Fuzheng W, Yali Q, Hui L. The methodological development of disease burden’s research — comprehensive evaluation of disease burden. Chinese J Dis Control. 2003;7(6):537–9.
Acknowledgements
The authors would like to thank all members of the Institute for Health Metrics and Evaluation (IHME), and all collaborators involved in GBD 2019 study.
Funding
This study was supported by the National Natural Science Foundation of China (81872721); National Key R&D Program of China (2017YFC1310902). The funding body of this research had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
CK, SL and CW conceived the study. CK, JL and ML analyzed and interpreted data on the disease burden of CKD. CK, JL and ML wrote the paper. SL and CW guided the writing of the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
None of the authors have any conflicts of interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: the authors identified an error in Fig. 2.
Supplementary Information
Additional file 1: Table S1
. Number of YLDs, YLLs, DALYs of CKD with percent change in 137 low-and middle-income countries, 1990–2019. Table S2. Age-standardized YLD, YLL and DALY rates of CKD with percent change in 137 low-and middle-income countries, 1990–2019. Table S3. The AAPC in age-standardized rate of YLD, YLL, and DALY for CKD in 137 low-and middle-income countries, 1990–2019.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ke, C., Liang, J., Liu, M. et al. Burden of chronic kidney disease and its risk-attributable burden in 137 low-and middle-income countries, 1990–2019: results from the global burden of disease study 2019. BMC Nephrol 23, 17 (2022). https://doi.org/10.1186/s12882-021-02597-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-021-02597-3