Abstract
Background
Majeed syndrome is a rare, autosomal recessive autoinflammatory disorder first described in 1989. The syndrome starts during infancy with recurrent relapses of osteomyelitis typically associated with fever, congenital dyserythropoietic anemia (CDA), and often neutrophilic dermatosis. Mutations in the LPIN2 gene located on the short arm of chromosome 18 have been identified as being responsible for Majeed syndrome.
Case presentation
We report an 8-month-old boy, who presented with recurrent fever, mild to moderate anemia, and severe neutropenia. Erythrocyte sedimentation rate and C-reactive protein were elevated. Molecular testing identified a paternal splicing donor site variant c.2327 + 1G > C and a maternal frameshift variant c.1691_1694delGAGA (Arg564Lysfs*3) in LPIN2.
Conclusions
Only a few cases with LPIN2 mutation have been reported, mainly in the Middle East with homozygous variants. Our patient exhibited a mild clinical phenotype and severe neutropenia, different from previous reports.
Similar content being viewed by others
Background
Majeed syndrome is a rare, autosomal recessive autoinflammatory disorder first described in 1989. The syndrome starts during infancy with recurrent relapses of osteomyelitis typically associated with fever, congenital dyserythropoietic anemia (CDA), and often neutrophilic dermatosis. Mutations in the LPIN2 gene, located on the short arm of chromosome 18, have been identified as being responsible for Majeed syndrome. Here we report what we believe to be the first case of Majeed syndrome in a Chinese individual. This case is of variable severity.
Case presentation
Clinical information
This Chinese 8-month-old boy presented at the age of 6 months with recurrent fever lasting for 5–7 days, recurring every 3–7 days. Sometimes he had a slight cough. He had no physical pain or movement problems. He had no rash or other symptoms. The infant was born full term. The delivery was normal delivery with a birth weight of 3.0 kg. His parents had a non-consanguineous marriage. There was a neonatal history of jaundice. The boy had mild pallor when he was admitted to our hospital. He had no lymphadenopathy or hepatosplenomegaly. Blood routine examination showed severe neutropenia (380–400/mm3) with normal white blood cell count, microcytic anemia (hemoglobin 85–95 g/L), and slight thrombocytosis. The boy had an elevated erythrocyte sedimentation rate (79 mm/h) and C-reactive protein (39 mg/L, normal< 8 mg/L). Immunoglobulin and lymphocyte subsets were found to be normal. Rheumatoid factors were negative. Antinuclear antibody was positive with a titer of 1:80, while the anti-ds DNA antibody was negative. Antineutrophil cytoplasmic antibodies showed mild elevated anti-MPO antibody (30.2 RU/ml) and negative anti-PR3 antibody. Thyroid function was normal. Serum iron and transferrin levels were low, which indicated iron-deficiency anemia. Bone marrow hemocytology revealed myleoproliferation cells, and the proportion of myelocyte was decreased because of the granulocytosis. Red blood cells were active and tended to proliferate. Metarubricytes dominated with small, hollow, and distorted mature erythrocytes. Blood and bone marrow puncture specimens were cultured for bacteria and fungi and showed no growth. Results of viral serologic studies were also negative. Lymphocyte interferon release assay was negative. Abdominal ultrasound scan gave normal findings. Cardiac ultrasound showed no abnormalities. Chest CT showed no interstitial or parenchymal infiltration. Because he had no limbs pain, the patient did not undergo an MRI scan.
Molecular genetic studies
After obtaining informed consent, we isolated DNA from peripheral blood samples obtained from the patient and parents using the Gentra Puregene Blood Kit (Qiagen, Hilden, Germany). Whole exome library was captured by a SureSelect Human All Exon Kit (Agilent Technologies, Santa Clara, CA, USA) according to the manufacturer’s instructions. Target regions were sequenced and aligned to the GRCh37/hg19 human reference sequence. Variants were annotated and filtered by TGex (tgex-app.genecards.cn). Variants were classified following the ACMG/AMP standards and guidelines [1]. Putative pathogenic variants were confirmed by Sanger sequencing.
Discussion and conclusions
After sequencing, we identified a paternal splicing donor site variant c.2327 + 1G > C and a maternal frameshift variant c.1691_1694delGAGA (Arg564Lysfs*3) in LPIN2 (NM_014646.2, Fig. 1). c.2327 + 1G > C has not been reported in dbSNP, 1000 genome, ESP, ExAC, or gnomAD databases, indicating it is very rare in normal populations. This variant was predicted to disarrange the donor site according to Human Splicing Finder (www.umd.be/HSF3/HSF.shtml) and caused exon 17 deletion or intron 17 insertion either entirely or partly. This variant was first reported in an Arabic family. The proband was a 3-year-old girl with Majeed syndrome [2]. The author predicted this variant could produce an R776S change followed by 65 amino acids prior to encountering a stop codon in intron 17. c.1691_1694delGAGA, located in exon 12, led to premature termination codon at position 3 amino acids after mutation. It is expected to produce a truncated protein or lead to early degradation of mRNA through the mechanism of nonsense-mediated decay. This variant has not been reported in dbSNP, ESP, or 1000 genome databases. The frequency in ExAC database was 0.000008236, suggesting that the frequency was extremely low. Both variants were classified as pathogenic variants according to ACMG/AMP guidelines.
Majeed syndrome is a rare autosomal recessive disorder characterized by chronic recurrent multifocal osteomyelitis (CRMO). This is an early-onset disorder with a lifelong course and congenital dyserythropoietic anemia (CDA) that presents as hypochromic, microcytic anemia during the first year of life and ranges from mild to severe enough to render the patient transfusion dependent. Some individuals also develop a transient inflammatory dermatosis, often manifesting as Sweet syndrome (neutrophilic skin infiltration). It is often accompanied by recurrent fever. The diagnosis is based on clinical findings and molecular genetic testing of LPIN2, the only gene in which pathogenic variants are known to cause Majeed syndrome. Only a few cases with LPIN2 mutation have been reported, mainly in the Middle East with homozygous variants [2,3,4,5,6,7,8,9].
LPIN2 encodes a phosphatidate phosphatase that plays important roles in controlling the metabolism of fatty acids at different levels. The function of LPIN2 is not well known. According to a previous study, it acts as a magnesium-dependent phosphatase, converting phosphatidic acid to diacylglycerol in the biosynthesis of triglycerides, phosphatidylcholine, and phosphatidylethanolamine. It can also act as a nuclear transcriptional coactivator of PPARGC1A and so regulate lipid metabolism [10, 11]. Homozygous knock out Lpin2 mice displayed increases in mean platelet volume, red blood cell distribution, and lymph nodes and decreases in mean corpuscular hemoglobin, bone mineral density, and overall bone mass. They also had abnormal circulating phosphate level, hydrometra, and preweaning lethality with incomplete penetrance. LPIN2 has 19 exons and 3 lipin domains located in N-terminal (amino acid: 1–108), middle (amino acid: 469–561), and C-terminal (amino acid: 677–831), respectively (Fig. 2). Lipin domains are highly conserved in lipin proteins and lipin homologues from Saccharomyces cerevisiae (Smp2, PAH1) and Schizosaccharomyces pombe (Ned1) and the function of these domains was still unclear. Mutations on lipin domains in mice lead to fatty liver dystrophy.
Distribution of variants in exonic location of LPIN2 and domain structure of the Lipin2 protein The structure of the protein is shown in the upper row with crucial domains, drawn approximately to scale. The structure of the LPIN2 is shown in the lower row. Two structures are linked by a dashed line to indicate exonic locations of respective domains. Variants above (red) are reported in this study. Variants shown in black below are previously reported in the literature. c.2327 + 1G > C has already been reported by Al-Mosawi (2007)
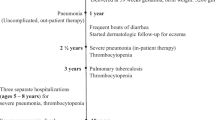
We here report the first case of Majeed syndrome in the individual of Chinese heritage and with variable severity. Our patient exhibited a mild clinical phenotype, unlike in previously reported cases (Table 1). He had recurrent fever and mild to moderate hypochromic and microcytic anemia without severe CRMO. He had no physical pain, swelling, or movement disorders. Majeed reported a Palestinian Arab boy who presented at the age of 2 months with recurrent episodes of high fever and irritability [12]. At the age of 9 months, these episodes began to be associated with periarticular swellings with heat, tenderness, and limitation of movement. Therefore, the patient’s signs and symptoms need to be observed continuously. Our patient had severe neutropenia from the age of 6 months, and his absolute neutrophil count was 380–400/mm3. This phenotype has been reported in few cases. Mosawi reported an Arabic female with Majeed syndrome who had mild neutropenia (1080/mm3) in the neonatal period [3]. RAO reported a 15-year-old boy with Majeed syndrome complicated by mild neutropenia [5]. Those cases suggest that neutropenia may be part of the phenotype. More cases must be studied to confirm this phenotype. Treatment with IL-1 blockade was reported in Majeed syndrome [13]. Our patient did not use IL-1 blockade because of his age and the mildness of his phenotype.
Majeed syndrome is an autosomal recessive, autoinflammatory disorder. It is characterized by CRMO and CDA. Our patient had the compound heterozygous LPIN2 pathogenic variant and exhibited a mild clinical phenotype, unlike in previously reported cases.
Availability of data and materials
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CDA:
-
Congenital dyserythropoietic anemia
- CRMO:
-
Chronic recurrent multifocal osteomyelitis
- CRP:
-
C-Reactive protein
References
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Al-Mosawi ZS, Al-Saad KK, Ijadi-Maghsoodi R, El-Shanti HI, Ferguson PJ. A splice site mutation confirms the role of LPIN2 in Majeed syndrome. Arthritis Rheum. 2007;56:960–4.
Ferguson PJ, Chen S, Tayeh MK, Ochoa L, Leal SM, Pelet A, Munnich A, Lyonnet S, Majeed HA, El-Shanti H. Homozygous mutations in LPIN2 are responsible for the syndrome of chronic recurrent multifocal osteomyelitis and congenital dyserythropoietic anaemia (Majeed syndrome). J Med Genet. 2005;42:551–7.
Herlin T, Fiirgaard B, Bjerre M, Kerndrup G, Hasle H, Bing X, Ferguson PJ. Efficacy of anti-IL-1 treatment in Majeed syndrome. Ann Rheum Dis. 2013;72:410–3.
Rao AP, Gopalakrishna DB, Bing X, Ferguson PJ. Phenotypic variability in Majeed syndrome. J Rheumatol. 2016;43:1258–9.
Monies D, Abouelhoda M, AlSayed M, Alhassnan Z, Alotaibi M, Kayyali H, Al-Owain M, Shah A, Rahbeeni Z, Al-Muhaizea MA, et al. The landscape of genetic diseases in Saudi Arabia based on the first 1000 diagnostic panels and exomes. Hum Genet. 2017;136:921–9.
Moussa T, Bhat V, Kini V, Fathalla BM. Clinical and genetic association, radiological findings and response to biological therapy in seven children from Qatar with non-bacterial osteomyelitis. Int J Rheum Dis. 2017;20:1286–96.
Omoyinmi E, Standing A, Keylock A, Price-Kuehne F, Melo GS, Rowczenio D, Nanthapisal S, Cullup T, Nyanhete R, Ashton E, et al. Clinical impact of a targeted next-generation sequencing gene panel for autoinflammation and vasculitis. PLoS One. 2017;12:e0181874.
Marzano AV, Ortega-Loayza AG, Ceccherini I, Cugno M. LPIN2 gene mutation in a patient with overlapping neutrophilic disease (pyoderma gangrenosum and aseptic abscess syndrome). JAAD Case Rep. 2018;4:120–2.
Donkor J, Zhang P, Wong S, O'Loughlin L, Dewald J, Kok BP, Brindley DN, Reue K. A conserved serine residue is required for the phosphatidate phosphatase activity but not the transcriptional coactivator functions of lipin-1 and lipin-2. J Biol Chem. 2009;284:29968–78.
Gropler MC, Harris TE, Hall AM, Wolins NE, Gross RW, Han X, Chen Z, Finck BN. Lipin 2 is a liver-enriched phosphatidate phosphohydrolase enzyme that is dynamically regulated by fasting and obesity in mice. J Biol Chem. 2009;284:6763–72.
Majeed HA, Al-Tarawna M, El-Shanti H, Kamel B, Al-Khalaileh F. The syndrome of chronic recurrent multifocal osteomyelitis and congenital dyserythropoietic anaemia. Report of a new family and a review. Eur J Pediatr. 2001;160:705–10.
Roy NBA, Zaal AI, Hall G, Wilkinson N, Proven M, McGowan S, Hipkiss R, Buckle V, Kavirayani A, Babbs C. Majeed syndrome: description of a novel mutation and therapeutic response to bisphosphonates and IL-1 blockade with anakinra. Rheumatology (Oxford). 2019:1–3.
Acknowledgements
We thank all the people who have been involved in our study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All of the authors had access to the full dataset (including the statistical reports and tables) and take responsibility for the integrity of the data and the accuracy of the data analysis. BPX, CJH, JL and XYH conceived the study. ZPZ, RLG, JG and WL collected the data and designed the analysis. JL and XYH wrote the first draft of the paper. BPX reviewed and approved the final report. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All participants or their legal representatives signed informed consent and the study was approved by the Ethics Committee of Beijing Children’s Hospital Affiliated to Capital Medical University.
Consent for publication
The patient’s parents had written informed consent to publish this information.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Liu, J., Hu, XY., Zhao, ZP. et al. Compound heterozygous LPIN2 pathogenic variants in a patient with Majeed syndrome with recurrent fever and severe neutropenia: case report. BMC Med Genet 20, 182 (2019). https://doi.org/10.1186/s12881-019-0919-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12881-019-0919-3