Abstract
Background and objective
Numerous previous studies have assessed the prognostic role of 18F-fluorodeoxyglucose positron-emission tomography (18F FDG PET) in patients with biliary tract cancer (BTC), but those results were inconsistent. The present study aims to determine the predictive value of 18F FDG PET in BTC patients via a meta-analysis.
Methods
The underlying studies related to 18F FDG PET and BTC patients` outcomes were searched and identified in the online databases. The interested parameters include total lesion glycolysis (TLG), metabolic tumor volume (MTV), primary tumor and metastatic lymph node (LN) maximum standardized uptake value (SUVmax), as well as change of SUVmax (ΔSUVmax) during treatment. Overall survival (OS), disease-free survival (DFS), and progression-free survival (PFS) were considered as the primary endpoints. Hazard ratio (HR) and corresponding 95% confidence intervals (CIs) were defined as the effective measure and calculated by a pooled analysis. Publication bias was assessed by funnel plot, Bagg’s and Egger’s tests.
Results
Totally, 23 studies involving 1478 patients were included in the present meta-analysis. After a pooled analysis, it revealed that a high SUVmax was significantly associated with a poor OS (HR:2.07, 95%CI: 1.74–2.46, P = 0.000) and DFS (HR: 2.28, 95%CI: 1.53–3.41, P = 0.000). In addition, an increased TLG level contributed to a shorter OS (HR:1.91, 95%CI: 1.26–2.90, P = 0.002) and DFS (HR: 4.34, 95%CI: 1.42–13.27, P = 0.01). Moreover, we confirmed that an elevated MTV was significantly associated with increased mortality (HR:2.04, 95%CI:1.26–3.31, P = 0.004) and disease relapse (HR: 3.88, 95%CI:1.25–12.09, P = 0.019) risks. Besides, the present study uncovered that increased ΔSUVmax could predict poor OS (HR:1.26, 95%CI:1.06–1.50, P = 0.008) instead of PFS (HR: 1.96, 95%CI: 0.82–4.72, P = 0.280). Lastly, we found that LN SUVmax did not link to OS (HR: 1.49, 95%CI: 0.83–2.68, P = 0.178). No obvious publication bias was detected in the present study.
Conclusion
18F FDG PET parameters, including SUVmax, TLG, MTV, and ΔSUVmax, could be applied as convenient and reliable factors for predicting BTC patients` outcomes.
Similar content being viewed by others
Introduction
As a highly heterogeneous disease, biliary tract cancer (BTC), including intrahepatic, perihilar, and distal cholangiocarcinoma, as well as gallbladder and ampulla cancer, is a low-incidence but fatal neoplasm with poor prognosis [1]. The global morbidity of intrahepatic cholangiocarcinoma (ICC) is rising gradually, especially in low-income countries [2]. Despite the application and development of several examination methods and treatment options, patients` overall survival (OS) remains limited [3]. Surgical resection is the primary curative option for early-stage BTC patients. Unfortunately, most patients develop locally advanced or metastatic disease when diagnosed due to a lack of particular symptoms in the early stage. Their survival is restricted, although palliative chemotherapy has been recommended. In addition, most postoperative patients would suffer from disease relapse, which limited their 5-year OS rate to approximately 20–60% [4]. So far, the recurrent and mortality risks of BTC remain less understood. It is essential to explore the underlying prognostic factors to identify the high-risk population in order to achieve precision management.
As an imaging technique based on glucose metabolism to assess a variety of physiological and disease processes, 18F-fluorodeoxyglucose positron-emission tomography (18F FDG PET) has been defined and applied in staging and managing multiple cancers, including BTC. Interestingly, numerous previous meta-analyses determined that some parameters of 18F FDG PET could be utilized as prognostic factors in patients with gastric cancer [5], pancreatic cancer [6], and lung cancer [7] instead of BTC. Meanwhile, the predictive significance of 18F FDG PET parameters has been assessed in BTC by previous clinical studies. However, these results were inconsistent due to different sample sizes and study designs. For example, the cohort studies conducted by Seo et al. [8] and Yho et al. [9] demonstrated that the maximum standardized uptake value (SUVmax) of primary tumor mass was an independent predictor for disease-free survival (DFS) and OS. By contrast, some investigators demonstrated that SUVmax did not contribut to BTC patients` outcomes [10, 11]. Therefore, we performed the present meta-analysis to re-assess the prognostic value of multiple 18F FDG PET parameters, including total lesion glycolysis (TLG), metabolic tumor volume (MTV), primary tumor, and metastatic lymph nodes (LN) SUVmax, as well as change of SUVmax (ΔSUVmax) during treatment in patients with BTC.
Methods
Search strategy
Published studies potentially related to BTC and 18F FDG PET were searched from the PubMed, Embase, Cochrane Library, and Web of Science databases in August 2022. The keywords “biliary tract cancer,” “cholangiocarcinoma,” “positron-emission tomography,” and “prognosis,” as well as related abbreviations, were used for the screening and identification of candidate studies to be included in the meta-analysis. Multiple synonyms were also utilized.
Inclusion and exclusion criteria
Eligible studies were identified using the following criteria: (1) studies addressing the relationship between the outcomes of patients with BTC and metabolic parameters of 18F FDG PET, (2) diagnosis of all BTC participants by pathological examination. (3) reported in English.
The exclusion criteria for this meta-analysis were: (1) other types of articles (i.e., reviews, conference abstracts, case reports, or comments); (2) in vivo or in vitro research studies; (3) lack of data on DFS, PFS or OS; (4) lack of hazard ratios (HRs) and 95% confidence intervals (CIs) as practical measurements; (5) involving other pathological types of cancer patients.
Data management and outcome assessment
According to the above criteria, two investigators independently screened and reviewed available publications through abstract and full-text reading. If there was any disagreement between them, a consensus was reached through discussion with a senior investigator. We collected and defined the HRs and 95% CIs of OS and DFS as the effective measurements. The HRs and 95% CIs calculated by multivariate analysis were preferentially selected for the pooled analysis for better accuracy.
Quality assessment
The evidence level of the studies was estimated by the UK Cochrane Centre of Evidence (2009). Newcastle-Ottawa Scale [12] was utilized to assess the quality of the retrospective cohort studies. The selection of patients, comparability of the study groups, and assessment of outcome represent the critical factors of this scale, with the maximum total score of 9. Studies with scores ≥6 were defined as high-quality studies, and this was a presetting selection criterion in this report.
Statistical analysis
The HRs and associated 95% CIs were calculated to pool the functional outcomes. Statistical heterogeneity among the studies was assessed using chi-square tests with the significance set to P < 0.05 or I2 > 50%. A fixed-effects model was utilized if there was no evident heterogeneity; otherwise, we selected a random-effects model to minimize the heterogeneity, followed by subgroup and sensitivity analysis. Funnel plots, Egger’s, and Begg’s tests were used to examine publication bias. All statistical analyses were performed using STATA version 14.0 (Stata statistical software, College Station, TX, USA).
Results
Characteristics of included studies
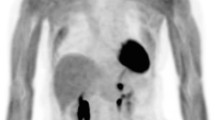
After removing duplicated articles (n = 229), 751 studies were identified for review and screening. We excluded 303 unrelated studies, 171 reviews, 65 conference abstracts, 132 case reports, and 9 in vivo or in vitro studies by reading their titles and abstracts. According to the above criteria, 48 studies were excluded after full-text review due to the following reasons: 1) lack of data on OS or DFS (n = 30); 2) including non-biliary tract original cancers (n = 8); lack of HR and relevant 95%CIs (n = 10) (Fig. 1).
Totally, this meta-analysis enrolled 23 retrospective cohort studies with 1478 patients with BTC patients, which contains intrahepatic cholangiocarcinoma (ICC), extrahepatic cholangiocarcinoma (ECC), as well as gallbladder and ampullary cancer [8,9,10,11, 13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]. The level of evidence is 2a. Based on the Newcastle–Ottawa Scale, all studies received a quality score of 6–9. The interested metabolic parameters of 18F-PET/CT included primary tumor maximum standardized uptake value (SUVmax) (n = 19), total lesion glycolysis (TLG) (n = 5), metabolic tumor volume (MTV) (n = 5), lymph nodes SUVmax (n = 2), and change of SUVmax (ΔSUVmax) (n = 3). (Table 1).
Prognostic role of primary tumor SUVmax in OS and DFS
Nineteen studies, including 1326 patients, described the relationship between SUVmax of primary tumor and OS. Based on the result of heterogeneity (I2 = 13.8%, P = 0.740), a fixed-effect model was carried out for analysis of these data. It was revealed that an increased SUVmax was significantly associated with a worse OS (HR:2.07, 95%CI: 1.74–2.46, P = 0.000) (Fig. 2A, Table 2). Similarly, a higher SUVmax contributed obviously to a worse DFS (HR: 2.28, 95%CI: 1.53–3.41, P = 0.000) after a pooled analysis of 8 studies with 458 patients using a random-effect model (I2 = 69.5%, P = 0.005) (Fig. 2B, Table 2).
The predictive value of TLG in OS and DFS
There were 5 studies (including 202 cases) focused on the correction of TLG and OS. After a pooled analysis with a fixed-effect model (I2 = 0.0%, P = 0.484), we found that an increased TLG linked to a higher risk of mortality (HR:1.91, 95%CI: 1.26–2.90, P = 0.002) (Fig. 3A, Table 2). Additionally, 2 studies with 49 patients reported the relationship between TLG and disease recurrence risk. When analyzed with a fixed-effect model (I2 = 0.0%, P = 0.660), it revealed that an increased TLG was obviously associated with poor DFS (HR: 4.34, 95%CI: 1.42–13.27, P = 0.01) (Fig. 3B, Table 2).
Prognostic significance of MTV in OS and DFS
Totally, 5 studies involving 202 cases analyzed the relationship between MTV and patients` survival. As the result of pooled analysis with a fixed-effect model (I2 = 8.6%, P = 0.357), it was confirmed that an elevated MTV was significantly associated with worse OS (HR:2.04, 95%CI:1.26–3.31, P = 0.004) (Fig. 4A, Table 2). In addition, we demonstrated that a lower MTV contributed to better DFS significantly (HR: 3.88, 95%CI:1.25–12.09, P = 0.019) when analyzing 2 studies (including 49 cases) using a random-effect model (I2 = 52.1%, P = 0.148) (Fig. 4B, Table 2).
Prognostic significance of ΔSUVmax and lymph nodes SUVmax in OS and PFS
Three studies with 136 patients reported the correction of ΔSUVmax and patients` survival. The ΔSUVmax were defined as the changes of SUVmax between pre- and post-treatment. The intervals were about 42 days, 2 months, and 3 months, respectively. After a pooled analysis with a fixed-effect model (I2 = 26.6%, P = 0.256), it demonstrated that an elevated ΔSUVmax was significantly associated with the mortality risk (HR:1.26, 95%CI:1.06–1.50, P = 0.008) (Fig. 5A, Table 2). 2 studies with 110 patients reported the relationship between ΔSUVmax and cancer progression risk. When analyzed with a random-effect model, we found that an increased ΔSUVmax was not associated with PFS (HR: 1.96, 95%CI: 0.82–4.72, P = 0.280) (Fig. 5B, Table 2).
In contrast with primary tumor SUVmax, we found that lymph nodes SUVmax (LN SUVmax) did not contribute to OS (HR: 1.49, 95%CI: 0.83–2.68, P = 0.178) after a pooled analysis on 2 studies (involving 301 cases) with a fixed-effect model (Fig. 5C, Table 2).
Publication bias
Publication bias was examined by Begg’s and Egger’s tests, as well as funnel plots. All P-values obtained from Egger’s and Begg’s tests for each parameter and endpoint were > 0.05 (Table 2). Additionally, the visual inspection of the funnel plots did not show pronounced asymmetry (Fig. 6). These results confirmed the absence of publication bias risk among the included studies in the present meta-analysis.
Discussion
Due to different origin sites and cancer biology, the outcomes of BTC patients are heterogeneous [32]. Therefore, the identification of reliable prognostic factors is crucial in an era of precision medicine and helps to understand the risk of disease progression and patients` mortality. The clinical-pathological features, including tumor staging information and demographic factors remain the critical consideration for clinical practice and prognosis. Interestingly, the metabolic parameters of 18F FDG PET may provide important biological information beyond the clinical-pathological characteristics in patients with BTC. Therefore, the predictive role of these parameters must be determined.
The diagnostic and staging significance of 18F FDG PET have been determined by previous meta-analyses [33,34,35]. However, few meta-analysis assessed and reviewed the prognostic value of this novel imaging tool. According to available studies, we performed the present meta-analysis and demonstrated that higher values of SUVmax, MTV, and TLG predicted a higher risk of disease recurrence or death in patients with BTC. In addition, the emerging parameters such as LN SUVmax and ΔSUVmax have also been focused by our study, but the prognostic value needs further investigation due to insufficient published studies. These findings suggest that 18F FDG PET is not only a diagnostic tool but may be used to distinguish BTC patients who are at high risk of tumor recurrence or death and may benefit from subsequent, more aggressive treatments.
SUVmax is the most commonly used parameter in 18F FDG PET diagnosis and response monitoring because of its high reproducibility and availability. FDG uptake can reflect the metabolic activity of the tumor tissue. SUVmax has been shown to correlate with tumor mitotic count and with prognosis in cancer patients [36]. Previous studies demonstrated that the value of SUVmax was associated with multiple clinical-pathological features, including histological grade [37]. In addition, it has been uncovered that SUVmax was significantly correlated with programmed cell death ligand 1 (PD-L1) (P = 0.02) and glucose transporter 1 (GLUT1) (P < 0.01) expression in patients with pulmonary squamous-cell carcinoma [38]. Besides, SUVmax has been revealed as a marker associated with low tumor-infiltrating lymphocyte levels [39]. These results suggested that SUVmax, as a prognostic factor, could reflect cancer immune microenvironment. Interestingly, SUVmax was also associated with tumor tissue hypoxia and angiogenesis, contributing to cancer progression [40, 41].
MTV and TLG, which are a combination of volumetric and metabolic parameters, may be utilized in metabolic analyses of radiotracer activity, reflecting both properties of the tumor tissues. These parameters were also related to angiogenesis [41] and cancer immunity [42]. Taken these considerations, the above parameters in 18F PDF PET were associated to glucose intake, which regards cancer metabolism activity, tumor microenvironment, and immunity. These biological features contribute to tumor growth, cancer relapse, treatment resistance, and metastasis. Thereby, 18F PDF PET could be considered as a prognostic tool in patients with cancer including BTC.
previous studies demonstrated that glycolysis, as metabolic reprogramming, contributed significantly to cholangiocarcinoma initiation and progression [43, 44] Glycolic pathways and enzymes, including pyruvate kinase M2 [45, 46], Aldolase A [47] and lactate dehydrogenase A [48], play a critical role in BTC and have been utilized as biomarkers to predict patients` outcomes. Targeting glycolysis could be considered as a promising treatment option in BTC [49,50,51].
Nevertheless, some limitations in the present study should be acknowledged. Firstly, all included investigations were retrospective cohort studies with a small sample size and a modest level of evidence. Moreover, most participants in these studies were from Asian countries (e.g., Korea and Japan), which may be restricted to other regions. In addition, the cut-off value of interested parameters in each study was inconsistent, which needs further exploration of standard and optimal values for clinical practice. Besides, the included studies about some parameters (i.e., TLG, MTV,ΔSUVmax and LN SUVmax) were insufficient. Lastly, several HRs and their 95% CIs were extracted from univariate analysis, which might lead to an overestimation of the prognostic value of these markers.
Conclusion
In conclusion, this study demonstrated that 18F FDG PET parameters are associated with the risk of death. Especially SUVmax, TLG, MTV, and ΔSUVmax perform well in BTC patients` future survival analysis. Despite some limitations, we confirmed that 18F FDG PET could be a valuable method to help predict survival outcomes in biliary cancer patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 18F FDG PET:
-
18F-fluorodeoxyglucose positron-emission tomography
- TLG:
-
Total lesion glycolysis
- MTV:
-
Metabolic tumor volume
- SUVmax:
-
Maximum Standardized uptake value
- ΔSUVmax:
-
Change of maximum Standardized uptake value
- BTC:
-
Biliary tract cancer
- ICC:
-
Intrahepatic cholangiocarcinoma
- ECC:
-
Extrahepatic cholangiocarcinoma
- LN:
-
Lymph node
- OS:
-
Overall survival
- DFS:
-
Disease-free survival
- PFS:
-
Progression-free survival
- HR:
-
Hazard ratio
- CIs:
-
Confidence intervals
- PD-L1:
-
Programmed cell death ligand 1
- GLUT1:
-
Glucose transporter 1
References
Valle JW, Kelley RK, Nervi B, et al. Biliary tract cancer. Lancet. 2021;397(10272):428–44.
Sung H, Ferlay J, Siegel RL, et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Rizzo A, Ricci AD, Brandi G. Recent advances of immunotherapy for biliary tract cancer. Expert Rev Gastroenterol Hepatol. 2021;15(5):527–36.
Cillo U, Fondevila C, Donadon M, et al. Surgery for cholangiocarcinoma. Liver Int. 2019;39(Suppl 1):143–55.
Zou H, Zhao Y. 18FDG PET-CT for detecting gastric cancer recurrence after surgical resection: a meta-analysis. Surg Oncol. 2013;22(3):162–6.
Zhu D, Wang L, Zhang H, et al. Prognostic value of 18F-FDG-PET/CT parameters in patients with pancreatic carcinoma: a systematic review and meta-analysis. Medicine (Baltimore). 2017;96(33):e7813.
Christensen TN, Andersen PK, Langer SW, et al. Prognostic value of (18)F-FDG-PET parameters in patients with small cell lung Cancer: a Meta-Analysis and Review of Current Literature. Diagnostics (Basel). 2021;11(2).
Seo S, Yoh T, Morino K, et al. The relationship between (18)F-FDG uptake on PET/CT and markers of systemic inflammatory response in patients undergoing surgery for intrahepatic cholangiocarcinoma. Anticancer Res. 2019;39(1):341–6.
Yoh T, Seo S, Morino K, et al. Reappraisal of prognostic impact of tumor SUVmax by (18)F-FDG-PET/CT in intrahepatic cholangiocarcinoma. World J Surg. 2019;43(5):1323–31.
Lee EJ, Chang SH, Lee TY, et al. Prognostic value of FDG-PET/CT Total lesion glycolysis for patients with Resectable distal bile duct adenocarcinoma. Anticancer Res. 2015;35(12):6985–91.
Kubo M, Kobayashi S, Gotoh K, et al. Preoperative FDG-positive lymph nodes predict the postoperative prognosis in Resectable biliary tract cancers. Ann Surg Oncol. 2022;29(2):935–44.
Lo CK, Mertz D, Loeb M. Newcastle-Ottawa scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45.
Cho KM, Oh DY, Kim TY, et al. Metabolic characteristics of advanced biliary tract Cancer using 18F-Fluorodeoxyglucose positron emission tomography and their clinical implications. Oncologist. 2015;20(8):926–33.
Furukawa H, Ikuma H, Asakura K, et al. Prognostic importance of standardized uptake value on F-18 fluorodeoxyglucose-positron emission tomography in biliary tract carcinoma. J Surg Oncol. 2009;100(6):494–9.
Harimoto N, Hoshino K, Muranushi R, et al. Impact of metabolic parameters of (18)F-Fluorodeoxyglucose positron-emission tomography after hepatic resection in patients with intrahepatic cholangiocarcinoma. Anticancer Res. 2019;39(2):971–7.
Haug AR, Heinemann V, Bruns CJ, et al. 18F-FDG PET independently predicts survival in patients with cholangiocellular carcinoma treated with 90Y microspheres. Eur J Nucl Med Mol Imaging. 2011;38(6):1037–45.
Hwang JP, Moon JH, Kim HK, et al. Prognostic value of metabolic parameters measured by pretreatment dual-time-point 18F-fluorodeoxyglucose positron emission tomography/computed tomography in patients with intrahepatic or perihilar cholangiocarcinoma: a STROBE study. Medicine (Baltimore). 2021;100(21):e26015.
Kim NH, Lee SR, Kim YH, et al. Diagnostic performance and prognostic relevance of FDG positron emission tomography/computed tomography for patients with extrahepatic cholangiocarcinoma. Korean J Radiol. 2020;21(12):1355–66.
Kitamura K, Hatano E, Higashi T, et al. Prognostic value of (18)F-fluorodeoxyglucose positron emission tomography in patients with extrahepatic bile duct cancer. J Hepatobiliary Pancreat Sci. 2011;18(1):39–46.
Kobayashi S, Nagano H, Hoshino H, et al. Diagnostic value of FDG-PET for lymph node metastasis and outcome of surgery for biliary cancer. J Surg Oncol. 2011;103(3):223–9.
Lee JY, Kim HJ, Yim SH, et al. Primary tumor maximum standardized uptake value measured on 18F-fluorodeoxyglucose positron emission tomography-computed tomography is a prognostic value for survival in bile duct and gallbladder cancer. Korean J Gastroenterol. 2013;62(4):227–33.
Lee Y, Yoo IR, Boo SH, et al. The role of F-18 FDG PET/CT in intrahepatic cholangiocarcinoma. Nucl Med Mol Imaging. 2017;51(1):69–78.
Levillain H, Duran Derijckere I, Ameye L, et al. Personalised radioembolization improves outcomes in refractory intra-hepatic cholangiocarcinoma: a multicenter study. Eur J Nucl Med Mol Imaging. 2019;46(11):2270–9.
Pak K, Kim SJ, Kim IJ, et al. Splenic FDG uptake predicts poor prognosis in patients with unresectable cholangiocarcinoma. Nuklearmedizin. 2014;53(2):26–31.
Park MS, Lee SM. Preoperative 18F-FDG PET-CT maximum standardized uptake value predicts recurrence of biliary tract cancer. Anticancer Res. 2014;34(5):2551–4.
Sabaté-Llobera A, Gràcia-Sánchez L, Reynés-Llompart G, et al. Differences on metabolic behavior between intra and extrahepatic cholangiocarcinomas at (18)F-FDG-PET/CT: prognostic implication of metabolic parameters and tumor markers. Clin Transl Oncol. 2019;21(3):324–33.
Seo S, Hatano E, Higashi T, et al. Fluorine-18 fluorodeoxyglucose positron emission tomography predicts lymph node metastasis, P-glycoprotein expression, and recurrence after resection in mass-forming intrahepatic cholangiocarcinoma. Surgery. 2008;143(6):769–77.
Yi HK, Park YJ, Bae JH, et al. Inverse prognostic relationships of (18)F-FDG PET/CT metabolic parameters in patients with distal bile duct Cancer undergoing curative surgery. Nucl Med Mol Imaging. 2018;52(5):334–41.
Choi MK, Choi JY, Lee J, et al. Prognostic and predictive value of metabolic tumor volume on (18)F-FDG PET/CT in advanced biliary tract cancer treated with gemcitabine/oxaliplatin with or without erlotinib. Med Oncol. 2014;31(7):23.
Jo J, Kwon HW, Park S, et al. Prospective evaluation of the clinical implications of the tumor metabolism and chemotherapy-related changes in advanced biliary tract Cancer. J Nucl Med. 2017;58(8):1255–61.
Zhu AX, Meyerhardt JA, Blaszkowsky LS, et al. Efficacy and safety of gemcitabine, oxaliplatin, and bevacizumab in advanced biliary-tract cancers and correlation of changes in 18-fluorodeoxyglucose PET with clinical outcome: a phase 2 study. Lancet Oncol. 2010;11(1):48–54.
Wardell CP, Fujita M, Yamada T, et al. Genomic characterization of biliary tract cancers identifies driver genes and predisposing mutations. J Hepatol. 2018;68(5):959–69.
Parida GK, Panda RA, Agrawal K. Impact of fluorine-18-fluorodeoxyglucose PET/computed tomography in staging of patients with gallbladder cancer: a systematic review and meta-analysis. Nucl Med Commun. 2021;42(8):846–54.
Hu JH, Tang JH, Lin CH, et al. Preoperative staging of cholangiocarcinoma and biliary carcinoma using 18F-fluorodeoxyglucose positron emission tomography: a meta-analysis. J Investig Med. 2018;66(1):52–61.
Huang X, Yang J, Li J, et al. Comparison of magnetic resonance imaging and 18-fludeoxyglucose positron emission tomography/computed tomography in the diagnostic accuracy of staging in patients with cholangiocarcinoma: a meta-analysis. Medicine (Baltimore). 2020;99(35):e20932.
Kadota K, Kachala SS, Nitadori J, et al. High SUVmax on FDG-PET indicates pleomorphic subtype in epithelioid malignant pleural mesothelioma: supportive evidence to reclassify pleomorphic as nonepithelioid histology. J Thorac Oncol. 2012;7(7):1192–7.
Sun XY, Chen TX, Chang C, et al. SUVmax of (18) FDG PET/CT predicts histological grade of lung adenocarcinoma. Acad Radiol. 2021;28(1):49–57.
Kasahara N, Kaira K, Bao P, et al. Correlation of tumor-related immunity with 18F-FDG-PET in pulmonary squamous-cell carcinoma. Lung Cancer. 2018;119:71–7.
Kasahara N, Kaira K, Yamaguchi K, et al. Fluorodeoxyglucose uptake is associated with low tumor-infiltrating lymphocyte levels in patients with small cell lung cancer. Lung Cancer. 2019;134:180–6.
Groves AM, Shastry M, Rodriguez-Justo M, et al. 18 F-FDG PET and biomarkers for tumour angiogenesis in early breast cancer. Eur J Nucl Med Mol Imaging. 2011;38(1):46–52.
Kaymak ZA, Karahan N, Erdoğan M, et al. Correlation of (18)F-FDG/PET SUV (max), SUV (mean), MTV, and TLG with HIF-1α in patients with colorectal Cancer. Mol Imaging Radionucl Ther. 2021;30(2):93–100.
Imai H, Kaira K, Hashimoto K, et al. Tumor immunity is related to (18) F-FDG uptake in thymic epithelial tumor. Cancer Med. 2021;10(18):6317–26.
Pant K, Richard S, Peixoto E, Gradilone SA. Role of glucose metabolism reprogramming in the pathogenesis of cholangiocarcinoma. Front Med (Lausanne). 2020;7:113.
Raggi C, Taddei ML, Rae C, et al. Metabolic reprogramming in cholangiocarcinoma. J Hepatol. 2022;77(3):849–64.
Fu K, Yang X, Wu H, et al. Diabetes and PKM2 affect prognosis in patients with intrahepatic cholangiocarcinoma. Oncol Lett. 2020;20(5):265.
Qian Z, Hu W, LV Z, et al. PKM2 upregulation promotes malignancy and indicates poor prognosis for intrahepatic cholangiocarcinoma. Clin Res Hepatol Gastroenterol. 2020;44(2):162–73.
Li X, Yu C, Luo Y, et al. Aldolase A enhances intrahepatic cholangiocarcinoma proliferation and invasion through promoting glycolysis. Int J Biol Sci. 2021;17(7):1782–94.
Thonsri U, Seubwai W, Waraasawapati S, et al. Overexpression of lactate dehydrogenase A in cholangiocarcinoma is correlated with poor prognosis. Histol Histopathol. 2017;32(5):503–10.
Cai J A-O, Cui Z, Zhou J, et al. METTL3 promotes glycolysis and cholangiocarcinoma progression by mediating the m6A modification of AKR1B10. Cancer Cell Int. 2022;22(1):385.
Li L, Wang C, Qiu Z, et al. Triptolide inhibits intrahepatic cholangiocarcinoma growth by suppressing glycolysis via the AKT/mTOR pathway. Phytomedicine. 2023;109:154575.
Lu S, Ke S, Wang C, et al. NNMT promotes the progression of intrahepatic cholangiocarcinoma by regulating aerobic glycolysis via the EGFR-STAT3 axis. Oncogenesis. 2022;11(1):39.
Acknowledgements
Not applicable.
Funding
1. National Natural Science Foundation of China (NO. 82204800).
2. Jiangsu Provincial Medical Key Discipline (Laboratory) (N0. ZDXYS202208–3).
Author information
Authors and Affiliations
Contributions
Zheng Xia and Shi Yue conceived and designed the study. Cheng Ying and Kulabieke Delida helped searched database, selected studies, extracted data. Wang Zihao preformed statistical analysis. Zheng Xia and Shi Yue wrote the draft of the manuscript. Jun Qian reviewed and edited the final manuscript critically for vital intellectual content. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, X., Shi, Y., Kulabieke, D. et al. Prognostic significance of 18F-Fluorodeoxyglucose positron-emission tomography parameters in patients with biliary tract cancers: a meta-analysis. BMC Med Imaging 24, 9 (2024). https://doi.org/10.1186/s12880-023-01182-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-023-01182-4