Abstract
Purpose
Our study aimed to diagnose benign or malignant thyroid nodules larger than 4 cm using quantitative diffusion-weighted imaging (DWI) analysis.
Methods
Eighty-two thyroid nodules were investigated retrospectively and divided them into benign (n = 62) and malignant groups (n = 20). We calculated quantitative features DWI and apparent diffusion coefficient (ADC) signal intensity standard deviation (DWISD and ADCSD), DWI and ADC signal intensity ratio (DWISIR and ADCSIR), mean ADC and minimum ADC value (ADCmean and ADCmin) and ADC value standard deviation (ADCVSD). Univariate and multivariate logistic regression were conducted to identify independent predictors, and develop a prediction model. We performed receiver operating characteristic (ROC) analysis to determine the optimal threshold of risk factors, and constructed combined threshold models. Our study calculated diagnostic performance including area under the ROC curve (AUC), accuracy, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and unnecessary biopsy rate of all models were calculated and compared them with the American College of Radiology Thyroid Imaging Reporting and Data System (ACR-TIRADS) result.
Results
Two independent predictors of malignant nodules were identified by multivariate analysis: DWISIR (P = 0.007) and ADCmin (P < 0.001). The AUCs for multivariate prediction model, combined DWISIR and ADCmin thresholds model, combined DWISIR and ADCSIR thresholds model and ACR-TIRADS were 0.946 (0.896–0.996), 0.875 (0.759–0.991), 0.777 (0.648–0.907) and 0.722 (0.588–0.857). The combined DWISIR and ADCmin threshold model had the lowest unnecessary biopsy rate of 0%, compared with 56.3% for ACR-TIRADS.
Conclusion
Quantitative DWI demonstrated favorable malignant thyroid nodule diagnostic efficacy. The combined DWISIR and ADCmin thresholds model significantly reduced the unnecessary biopsy rate.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Main points
-
The multivariate prediction model demonstrated satisfactory diagnostic performance with an AUC of 0.946 (0.896–0.996).
-
Combined DWISIR and ADCmin thresholds model demonstrated a high specificity with an unnecessary biopsy rate of 0%.
-
The multivariate prediction model and the combined threshold models are better than the ACR-TIRADS.
Introduction
Thyroid nodules manifest in up to 50–60% of the general population as detected by high-resolution ultrasound, while only around 10% of these nodules are malignant [1,2,3]. Since 2014, the overall incidence of thyroid cancer incidence rate has decreased, but the incidence and mortality rate of tumors larger than 4 cm are still rising [4]. Thyroid nodules larger than 4 cm are important for surgical decision-making in adult patients with thyroid nodules, according to the 2017 Thyroid Cancer Staging Manual of the American Joint Committee on Cancer (AJCC) [5]. Ultrasonography (US) is currently the main imaging technique for evaluating thyroid nodules [6,7,8,9]. US characteristics of thyroid nodules, such as the American College of Radiology Thyroid Imaging Reporting and Data System (ACR-TIRADS), have been employed for risk stratification [10]. However, the interobserver agreement on the TI-RADS remains only fair to moderate [11, 12] and these methods mainly focus on thyroid nodules smaller than 4 cm. Although biopsy is regarded as the gold standard for the preoperative diagnosis of thyroid cancer, it has reduced sensitivity when applied to thyroid nodules larger than 4 cm [13,14,15].
Diffusion-weighted imaging (DWI), a non-contrast magnetic resonance imaging (MRI) technology, detects water molecule random mobility and offers information on tissue microstructure and cell density. The apparent diffusion coefficient (ADC) map can be further calculated from DWI to quantify the diffusion characteristic of tissues [16, 17]. DWI was used to diagnose benign and malignant tumors [18,19,20,21]. Although earlier research has demonstrated its effectiveness of DWI in distinguishing between benign and malignant thyroid nodules, those studies have included nodules of all sizes [22, 23]. For larger lesions, DWI has a superior diagnostic value, but there were limited researcher on the diagnostic value of DWI for thyroid nodules larger than 4 cm. Meanwhile, accurate pre-operative assessment of thyroid nodules is crucial for subsequent treatment. Accordingly, it is important to distinguish between benign and malignant nodules larger than 4 cm before surgery [24].
Consequently, this study aimed to evaluate approaches using quantitative DWI, and compare them with ACR-TIRADS to differentiate between benign and malignant thyroid nodules larger than 4 cm preoperatively.
Materials and methods
Patients and study design
The study followed the Declaration of Helsinki (revised 2013). The Institutional Ethics Committee of Minhang Hospital affiliated with Fudan University approved this observational, retrospective study (approval number: 2021–008-01 K) with a waiver of informed consent.
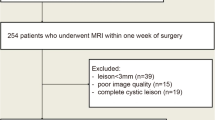
We reviewed consecutive patients with thyroid nodules who had pathology results at our institution between 2017 and 2022. The inclusion criteria included: 1) lesion diameter larger than 4 cm; 2) patients who underwent preoperative thyroid MRI; 3) complete pathology of postoperative specimens. The exclusion criteria included: 1) incomplete clinical and imaging data; 2) poor image quality; 3) lack of contrast enhancement on MRI. Figure 1 displays the study flowchart.
The study flowchart. Abbreviations: MRI, Magnetic resonance imaging; DWI, diffusion weighted imaging; ADC, apparent diffusion coefficient; SIR, signal intensity rate; ADCmin, minimum apparent diffusion coefficient value; ACR-TIRADS, American College of Radiology Thyroid Imaging Reporting and Data System; TR, TI-RADS; AUC, area under the receiver operating characteristic curve
Finally, 82 lesions from 78 patients (32 males and 50 females; age: 50.26 ± 16.20 years; age range: 15–78 years) met the inclusion criteria. Lesions were categorized into benign (n = 62) and malignant (n = 20) groups according to the postoperative pathology.
MRI acquisition
The 1.5 T MRI scanner (Excite HD; GE Healthcare, Waukesha, WI, USA) used for all MRI examinations was set up with an 8-channel customized neck surface coil (Chenguang Medical Technology Ltd, Shanghai, China). The scan covered the thoracic inlet to the base of the cranium were covered by the scan. The MRI sequences used (CE-T1WI) included axial and coronal fat-suppressed T2-weighted imaging (T2WI), axial T1-weighted imaging (T1WI), single-shot spin-echo echo-planar imaging (SS-SE-EPI) DWI at b values of 0 and 800 s/mm2, and axial multiphasic contrast-enhanced T1WI comprised the MRI sequences used (CE-T1WI). A gadolinium contrast agent (Magnevist; Bayer Healthcare, Berlin, Germany) was injected for the CE-T1WI acquisition at a dose of 0.2 mL/kg and a rate of 3 mL/s, followed immediately by 20 mL of physiological saline flushing. Following the injection of the contrast agent, six phases were recorded at intervals of 30, 60, 120, 180, 240, and 300 s intervals while the patients were asked to hold their breath. Table S1 lists detailed acquisition parameters.
Image analysis
ADC maps were automatically created from DWI images (b = 0 and 800 s/mm2) on the console using mono-exponential fitting. Quantitative DWI parameters were measured by two MRI diagnosticians who were blind to the lesion pathology (a chief physician with eight years of experience and a resident with one year each in thyroid MRI diagnosis), using picture archiving and communication system (PACS) and Advantage Workstation 4.5 (GE Healthcare, Waukesha, WI, USA). The section of the whole solid leision portion of the lesion with maximum transverse diameter (excluding cystic, hemorrhage, necrosis, calcium, and vascular structures) was selected to delineate the first region of interest (ROI 1). The following quantitative features in the ROI 1 were measured: 1) mean DWI signal intensity (DWISI); 2) mean ADC signal intensity (ADCSI); 3) mean ADC value (ADCmean) and minimum ADC value (ADCmin). Another ROI with an 8–10 mm2 area is also outlined as a relatively homogeneous solid part without cystic, hemorrhage, necrosis, calcium and vascular structures in the lesion and contralateral to the normal thyroid tissue. The following quantitative features of the ROI 2 were measured in the lesion: 1) DWI signal intensity standard deviation (DWISD) and ADC signal intensity standard deviation (ADCSD) and ADC value standard deviation (ADCVSD); 2) mean DWI signal intensity and mean ADC signal intensity of contralateral normal thyroid tissue (DWINSI and ADCNSI). The following formulas, DWISIR = DWISI / DWINSI and ADCSIR = ADCSI / ADCNSI, were used to calculate the DWI signal intensity rate (DWISIR) and ADC signal intensity rate (ADCSIR). DWI images (b = 800 s/mm2) and ADC map generated from DWI images (b = 0 and 800 s/mm2) were used for quantitative parameters extraction. All measurements were performed twice and averaged. Figure 2a demonstrates representative images of ROI delineation.
Representative DWI quantitative measurements. Lesions as indicated by blue arrows. a shows an example diagram of the ROI sketch. The black line outlines ROI 1, which is the whole solid portion of the slice with maximum transverse diameter for the lesion. The red line outlines ROI 2 of 8-10 mm2, the red dashed line is the interior of the lesion, and the red solid line is the contralateral-normal thyroid tissue. b and c show a patient with thyroid adenoma. b shows a DWI image with DWISD and DWISIR of 22 and 1.07. c shows ADC images with ADCSD, ADCSIR, ADCmin, ADCmean and ADCVSD of 110, 0.97, 1.15, 152 and 171. d and e show a patient with papillary thyroid cancer. d is a DWI image with DWISD and DWSIR of 24.7 and 1.56. e is an ADC image with ADCSD, ADCSIR, ADCmin, ADCmean and ADCVSD of 83, 0.74, 0.65, respectively, 1.04 and 69.59, respectively. Abbreviations: DWI, diffusion weighted imaging; ADC, apparent diffusion coefficient; SI, signal intensity; SD, standard deviation; ADCmin, minimum apparent diffusion coefficient value; ADCmean, mean apparent diffusion coefficient value; ADCVSD, standard deviation of apparent diffusion coefficient value
ACR-TIRADS
Two US experts retrospectively reviewed US images of thyroid lesions, reaching a consensus without knowledge of the lesion pathology. All lesions with category ≥ 4 were considered malignant according to ACR-TIRADS.
Statistical analysis
SPSS statistical software (version 26.0; IBM Corp, Armonk, NY, USA) and MedCalc (version 20.100; MedCalc Software, Ostend, Belgium) were used for all statistical analyses, and P values < 0.05 were deemed statistically significant. Quantitative MRI parameters and categorical variables of the malignant and benign groups were compared using independent t-tests, Chi-square tests, and Fisher's exact tests, respectively. Interobserver agreement was assessed using the intraclass correlation coefficient (ICC).
The malignancy prediction model was built using independent factors that were found using univariate and multivariate logistic stepwise regression. By optimizing the Youden's index, receiver operating characteristic (ROC) curve analysis was used to determine the ideal threshold values for the pertinent parameters. Combined thresholds approaches were established based on malignancy-related parameters (Supplementary Method). Individual parameters and models were evaluated using ROC curves, with the area under the ROC curve (AUC) compared by the DeLong test. Unnecessary biopsy rate was defined as the percentage of benign lesions for those requiring biopsy. The diagnostic performance measures for each model, including as accuracy, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and unnecessary biopsy rate were calculated, comparing the ACR-TIRADS result was compared.
Results
Clinicopathological characteristics
Table 1 lists the clinicopathological features of thyroid nodules. Except for the location (P = 0.015), there was no difference in the distribution of other features in the benign and malignant thyroid nodules. Table S2 demonstrates the pathological types of thyroid nodules.
Diagnostic performance of quantitative parameters
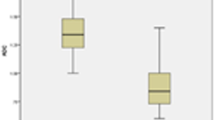
Figure 2 shows representative DWI images and the ROI delineation. Moreover, Table 2 demonstrates the results of the univariate and multivariate logistic regression analyses in predicting malignant thyroid nodules. Malignant nodules displayed significantly greater DWISD (P = 0.002) and DWISIR (P = 0.007) than benign nodules. Additionally, malignant nodules had significantly lower ADCSD (P = 0.005), ADCSIR (P = 0.008), ADCmin (P < 0.001), and ADCmean (P < 0.001) than benign nodules. The ICCs of DWISD, DWISIR, ADCSD, ADCSIR, ADCmin and ADCmean were 0.776, 0.758, 0.720, 0.923, 0.789, 0.783 and 0.743, respectively. ADCmin was the best-performing parameter with an AUC of 0.933 (0.874—0.992). Figure 3a and Table 3 represent the ROC curves and diagnostic performance metrics at the optimal threshold of relevant individual parameters, respectively.
The ROC curves. a is ROC curves of meaningful single parameters. b is multivariate prediction model, combined thresholds models and ACR-TIRADS for malignant and benign thyroid nodules. Abbreviations: DWI, diffusion weighted imaging; ADC, apparent diffusion coefficient; SD, standard deviation; SIR, signal intensity rate; ADCmin, minimum value of apparent diffusion coefficient; ADCmean, mean apparent diffusion coefficient value; ADCVSD, standard deviation of apparent diffusion coefficient value
The optimal threshold values were 1.13 × 10–3 mm2/s for ADCmin, 1.25 for ADCSIR, and 1.20 for DWISIR, showing their distribution in Fig. 4. For benign and malignant nodules, DWISIR, ADCSIR, and ADCmin overlapped; however, malignant nodule ADCmin was comparatively low.
Comparison of the diagnostic performance with ACR-TIRADS
Table 4 and Fig. 3b depict the diagnostic performance of the multivariate prediction model, combined threshold model, and ACR-TIRADS for malignant and benign thyroid nodules. The multivariate prediction model had the best diagnostic performance with an AUC of 0.946 (0.896–0.996) at a cutoff value of 0.198, which was higher than the AUC achieved by the combined threshold model (DWISIR and ADCmin), with insignificance difference (P = 0.500). The AUC of combined threshold model (DWISIR and ADC SIR) and ACR-TIRADS were 0.777 (0.648–0.907) and 0.722 (0.588–0.857), respectively. Figure 5 reveals the grouped scatter plots of the two combined threshold models, and Table S3 summarizes the Delong test results for AUC comparison among different models.
The grouped scatter plots of the two combined thresholds models. The blue dots are benign lesions, and the red dots are malignant lesions. a is the scatter plot of DWISIR and ADCmin of the lesions. b is the scatter plot of DWISIR and ADCmin of the lesions. Abbreviations: DWI, diffusion weighted imaging; ADC, apparent diffusion coefficient; SIR, signal intensity rate; ADCmin, minimum apparent diffusion coefficient value
The sensitivity (90.0%) and NPV (96.6%) were the highest in the multivariate prediction model. The results showed three false negative lesions, all follicular thyroid carcinoma, and seven false positive lesions: three nodular goiters, three adenomatous nodular goiters, and one adenoma. The best specificity and PPV (both 100%) were achieved by the combined threshold model (DWISIR and ADCmin), where five false negative lesions were all follicular thyroid carcinomas. The combined DWISIR and ADCmin had the lowest unnecessary biopsy rate with no false positive cases. The accuracy, sensitivity, specificity, PPV and NPV of the combined thresholds model (DWISIR and ADCSIR) were 81.7%, 70%, 85.5%, 60.9% and 89.2%, respectively. Compared with ACR-TIRADS, the quantitative DWI parameter-based models significantly improved differentiating benign and malignant thyroid nodules.
Discussion
This study proposed diagnostic models based on quantitative DWI parameters without enhancement to differentiate between benign and malignant thyroid nodules larger than 4 cm. The combined threshold model (DWISIR and ADCmin) demonstrated satisfactory diagnostic efficacy with significantly reduced unnecessary biopsy rate.
ADC map, derived from DWI, measures water diffusion in tissue and provides a new imaging biomarker for the diagnosis of benign and malignant tumours [25]; it has proven to be effective in predicting tumor malignancy [26]. Malignant thyroid nodules had much lower ADC values than the benign thyroid nodules, according to numerous studies [22, 27, 28], but they were for nodules smaller than 4 cm. We measured ADCmin, ADCmean and ADCSD, and found that the former two were associated with malignancy. In a meta-analysis of 2137 thyroid nodules, ADCmean was demonstrated to be a useful tool for differentiating between benign and malignant thyroid tumors and should be used in routine preoperative clinical testing. The ADCmean was 1.88 × 10–3 mm2/s in the benign nodules and 1.15 × 10–3 mm2/s in the malignant [22]; herein, for lesions larger than 4 cm, the ADCmean value was 1.74 × 10–3 mm2/s in benign nodules and 1.08 × 10–3 mm2/s in malignant nodules. ADCmin was found to be an independent predictor in our study. One study of benign and malignant lymph node metastases in the breast indicated that ADCmean had better diagnostic efficacy than ADCmin [29]. However, in a study of benign and malignant prostate tumors, ADCmin was found to be superior to ADCmean [30], which was similar to our results. Due to the multicollinearity between ADCmin and ADCmean in the combined threshold model, we chose ADCmin as it had a greater AUC value in the univariate analysis.
We also investigated the signal intensity-related parameters of DWI and corresponding ADC images on PACS. Leila et al. [31] reported that static MRI measurements like signal intensity and heterogeneity were unuseful in distinguishing between benign and malignant lesions. However, Wang et al. [32] showed that DWISIR was lower in benign nodules than in malignant ones, corroborating our findings. Our study found that DWISIR was another independent predictor of malignant nodules, with malignant nodules showing a higher DWISIR. which corroborated with our findings. DWISIR can complement ADCmin, and using the combined threshold model (DWISD and ADCmin) reduced the number of false positive cases by four and resulted in the highest specificity (100%). According to ACR-TIRADS, the biopsy is recommended for lesions with TR ≥ 4 and diameter > 1.5 cm. Therefore, all nodules with TR ≥ 4 in this study required biopsy to determine their benignity and malignancy, and the unnecessary biopsy rate was up to 56.3%. The combined threshold model (DWISIR and ADCmin) had the lowest unnecessary biopsy rate. DWI may be performed before preparation for biopsy and assisted in determining the need for biopsy and surgery based on quantitative DWI. Quantitative DWI may become a method of thyroid nodules larger than 4 cm surveillance to aid clinicians in their medical decisions.
In addition to ADCmin, we also measured ADCSIR, which is easily available on PACS. ADCSIR was lower in malignant nodules than in benign nodules significantly, which may be because malignant lesions have dense parenchymal cells, narrow cell spaces, and relatively limited extracellular water molecule diffusion. While the combined threshold model (DWISIR and ADCSIR), while it was inferior to the combined threshold model (DWISIR and ADCmin), it still resulted in nine fewer false positive cases than ACR-TIRADS alone.
This study found that individual parameters performed poorly in distinguishing the benignity of follicular thyroid neoplasm. The difference between follicular carcinoma and benign follicular neoplasm is the invasion of the envelope invasion, which can only be detected by postoperative pathology. Our measurements are limited to the substantial lesion component, and this pathological level of distinction is difficult to detect on images.
Although this study provided important insights, there were several limitations. First, selection bias is unavoidable in a retrospective observational study. Second, the sample size was relatively small, necessitating additional validation. Third, reviewing static ultrasound images and reports may differ from real-life clinical practice, introducing some bias. Finally, the study only used a b-value of 800 s/mm2. Therefore, more research must be conducted with various b-values to find the best value.
In conclusion, quantitative DWI parameters can separate benign from malignant thyroid nodules larger than 4 cm. The multivariate prediction and combined threshold model (DWISIR and ADCmin) demonstrated satisfactory diagnostic performance. Our results suggested that quantitative DWI parameters can assess benign and malignant nodules with sizes larger than 4 cm and assist clinicians in pre-operative decision-making.
Availability of data and materials
The data sets generated and/or analyzed in the current study were not made public because patients' personal information was included. Available from the corresponding author upon reasonable request.
Abbreviations
- DWI:
-
Diffusion-weighted imaging
- ADC:
-
Apparent diffusion coefficient
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the receiver operating characteristic curve
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- ACR-TIRADS:
-
American College of Radiology Thyroid Imaging Reporting and Data System
- DWISIR :
-
Diffusion-weighted imaging signal intensity rate
- ADCmin :
-
Minimum apparent diffusion coefficient value
- TNM:
-
Tumor, lymph node, metastasis
- AJCC:
-
American Joint Committee on Cancer
- MRI:
-
Magnetic resonance imaging
- T1WI:
-
T1-weighted imaging
- T2WI:
-
T2-weighted imaging
- SS-SE-EPI:
-
Single-shot spin-echo echo-planar imaging
- PACS:
-
Picture archiving and communication system
- ROI:
-
Region of interest
- DWISI :
-
Diffusion-weighted imaging signal intensity
- ADCSI :
-
Apparent diffusion coefficient signal intensity
- ADCmean :
-
Mean apparent diffusion coefficient value
- ADCmin :
-
Minimum apparent diffusion coefficient value
- DWISD :
-
Signal intensity standard deviation
- ADCSD :
-
Signal intensity standard deviation
- ADCVSD :
-
Standard deviation of apparent diffusion coefficient value
- DWISIR :
-
Diffusion-weighted imaging signal intensity rate
- ADCSIR :
-
Apparent diffusion coefficient signal intensity rate
- ICC:
-
Intraclass correlation coefficient
- PTC:
-
Papillary thyroid carcinoma
- FTC:
-
Follicular thyroid carcinoma
References
Alexander EK, Cibas ES. Diagnosis of thyroid nodules. Lancet Diabetes Endocrinol. 2022;10(7):533–9.
Durante C, Grani G, Lamartina L, Filetti S, Mandel SJ, Cooper DS. The Diagnosis and Management of Thyroid Nodules: A Review. JAMA. 2018;319(9):914–24.
Gharib H, Papini E, Garber JR, Duick DS, Harrell RM, Hegedus L, Paschke R, Valcavi R, Vitti P. Nodules AAATFoT: American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi Medical Guidelines for Clinical Practice for the Diagnosis and Management of Thyroid Nodules–2016 Update. Endocr Pract. 2016;22(5):622–39.
Megwalu UC, Moon PK. Thyroid Cancer Incidence and Mortality Trends in the United States: 2000–2018. Thyroid. 2022;32(5):560–70.
Perrier ND, Brierley JD, Tuttle RM. Differentiated and anaplastic thyroid carcinoma: Major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2018;68(1):55–63.
Ahn HS, Lee JB, Seo M, Park SH, Choi BI. Distinguishing benign from malignant thyroid nodules using thyroid ultrasonography: utility of adding superb microvascular imaging and elastography. Radiol Med. 2018;123(4):260–70.
Han RL, Wang J, Zhang FJ, Zhao N, Gao BL. Ultrasound Risk Assessment Combined with Molecular Markers of Galectin-3, c-MET, HBME-1 and CK19 for Diagnosis of Malignant and Benign Thyroid Nodules. Pathol Oncol Res. 2019;25(3):1075–81.
Qin P, Wu K, Hu Y, Zeng J, Chai X. Diagnosis of Benign and Malignant Thyroid Nodules Using Combined Conventional Ultrasound and Ultrasound Elasticity Imaging. IEEE J Biomed Health Inform. 2020;24(4):1028–36.
Zhou H, Wang K, Tian J. Online Transfer Learning for Differential Diagnosis of Benign and Malignant Thyroid Nodules With Ultrasound Images. IEEE Trans Biomed Eng. 2020;67(10):2773–80.
Tessler FN, Middleton WD, Grant EG, Hoang JK. Re: ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. J Am Coll Radiol. 2018;15(3 Pt A):381–2.
Persichetti A, Di Stasio E, Coccaro C, Graziano F, Bianchini A, Di Donna V, Corsello S, Valle D, Bizzarri G, Frasoldati A, et al. Inter- and Intraobserver Agreement in the Assessment of Thyroid Nodule Ultrasound Features and Classification Systems: A Blinded Multicenter Study. Thyroid. 2020;30(2):237–42.
Tappouni RR, Itri JN, McQueen TS, Lalwani N, Ou JJ. ACR TI-RADS: Pitfalls, Solutions, and Future Directions. Radiographics. 2019;39(7):2040–52.
Godazandeh G, Kashi Z, Zargarnataj S, Fazli M, Ebadi R, Kerdabadi EH. Evaluation the Relationship Between Thyroid Nodule Size with Malignancy and Accuracy of Fine Needle Aspiration Biopsy (FNAB). Acta Inform Med. 2016;24(5):347–50.
Karadeniz E, Yur M, Temiz A, Akcay MN. Malignancy risk for thyroid nodules larger than 4 cm and diagnostic reliability of ultrasound-guided FNAB results. Turk J Surg. 2019;35(1):13–8.
Yilmaz N, Cansu GB, Toru S, Sari R, Ocak GG, Arici C, Altunbas HA, Balci MK. Cytopathology-histopathology correlation and the effect of nodule diameter on diagnostic performance in patients undergoing thyroid fine-needle aspiration biopsy. J Cancer Res Ther. 2020;16(Supplement):S53–8.
Lee SH, Shin HJ, Moon WK. Diffusion-Weighted Magnetic Resonance Imaging of the Breast: Standardization of Image Acquisition and Interpretation. Korean J Radiol. 2021;22(1):9–22.
Surov A, Meyer HJ, Wienke A. Associations between apparent diffusion coefficient (ADC) and KI 67 in different tumors: a meta-analysis. Part 1: ADCmean. Oncotarget. 2017;8(43):75434–44.
Egnell L, Vidic I, Jerome NP, Bofin AM, Bathen TF, Goa PE. Stromal Collagen Content in Breast Tumors Correlates With In Vivo Diffusion-Weighted Imaging: A Comparison of Multi b-Value DWI With Histologic Specimen From Benign and Malignant Breast Lesions. J Magn Reson Imaging. 2020;51(6):1868–78.
Ge YX, Hu SD, Wang Z, Guan RP, Zhou XY, Gao QZ, Yan G. Feasibility and reproducibility of T2 mapping and DWI for identifying malignant lymph nodes in rectal cancer. Eur Radiol. 2021;31(5):3347–54.
Turkoglu S, Kayan M. Differentiation between benign and malignant ovarian masses using multiparametric MRI. Diagn Interv Imaging. 2020;101(3):147–55.
Zhu M, Zhang C, Yan J, Sun J, Zhao X, Zhang L, Yin L. Accuracy of quantitative diffusion-weighted imaging for differentiating benign and malignant pancreatic lesions: a systematic review and meta-analysis. Eur Radiol. 2021;31(10):7746–59.
Meyer HJ, Wienke A, Surov A. Discrimination between malignant and benign thyroid tumors by diffusion-weighted imaging - A systematic review and meta analysis. Magn Reson Imaging. 2021;84:41–57.
Wang H, Wei R, Liu W, Chen Y, Song B. Diagnostic efficacy of multiple MRI parameters in differentiating benign vs. malignant thyroid nodules. BMC Med Imaging. 2018;18(1):50.
Sencar ME, Calapkulu M, Bostan H, Sakiz D, Hepsen S, Kizilgul M, Unsal IO, Ozcelik O, Arslan E, Ucan B, et al. Effect of thyroid nodule size on cytology reliability and incidence of malignancy: A large cohort of 1205 patients from a single center. Ann Endocrinol (Paris). 2023;84(2):238-41.
Padhani AR, Liu G, Koh DM, Chenevert TL, Thoeny HC, Takahara T, Dzik-Jurasz A, Ross BD, Van Cauteren M, Collins D, et al. Diffusion-weighted magnetic resonance imaging as a cancer biomarker: consensus and recommendations. Neoplasia. 2009;11(2):102–25.
Surov A, Meyer HJ, Wienke A. Correlation between apparent diffusion coefficient (ADC) and cellularity is different in several tumors: a meta-analysis. Oncotarget. 2017;8(35):59492–9.
Feeney C, Lingam RK, Lee V, Rahman F, Nagendran S. Non-EPI-DWI for Detection, Disease Monitoring, and Clinical Decision-Making in Thyroid Eye Disease. AJNR Am J Neuroradiol. 2020;41(8):1466–72.
Yuan L, Zhao P, Lin X, Yu T, Diao R, Ning G. T1 mapping and reduced field-of-view DWI at 3.0 T MRI for differentiation of thyroid papillary carcinoma from nodular goiter. Clin Physiol Funct Imaging. 2023;43(3):137-45.
Fardanesh R, Thakur SB, Sevilimedu V, Horvat JV, Gullo RL, Reiner JS, Eskreis-Winkler S, Thakur N, Pinker K. Differentiation Between Benign and Metastatic Breast Lymph Nodes Using Apparent Diffusion Coefficients. Front Oncol. 2022;12:795265.
Fan C, Sun K, Min X, Cai W, Lv W, Ma X, Li Y, Chen C, Zhao P, Qiao J, et al. Discriminating malignant from benign testicular masses using machine-learning based radiomics signature of appearance diffusion coefficient maps: Comparing with conventional mean and minimum ADC values. Eur J Radiol. 2022;148:110158.
Aghaghazvini L, Sharifian H, Yazdani N, Hosseiny M, Kooraki S, Pirouzi P, Ghadiri A, Shakiba M, Kooraki S. Differentiation between benign and malignant thyroid nodules using diffusion-weighted imaging, a 3-T MRI study. Indian J Radiol Imaging. 2018;28(4):460–4.
Wang Q, Guo Y, Zhang J, Ning H, Zhang X, Lu Y, Shi Q. Diagnostic value of high b-value (2000 s/mm2) DWI for thyroid micronodules. Medicine (Baltimore). 2019;98(10):e14298.
Acknowledgements
Not applicable.
Funding
This work was supported by the Nature Science Foundation of Shanghai (grant number: 19ZR1446200), Science and Technology Commission of Minhang District, Shanghai (grant number: 2021MHZ065).
Author information
Authors and Affiliations
Contributions
All authors and co-authors have significantly contributed. T.Z. contributed to data collection, writing and editing of manuscript. X.X. contributed to pathological data and writing of manuscript. Z.N. contributed to surgical and medical practices and writing of manuscript. L.T. contributed to ultrasound data and writing of manuscript. P.W. contributed to review and editing of manuscript. B.S. contributed to study design, review of manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Ethics Committee of Minhang Hospital affiliated with Fudan University approved this observational, retrospective study (approval number: 2021–008-01 K) with a waiver of informed consent.The study complied with the Declaration of Helsinki (revised 2013).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table
S1. Parameters of MRI Sequence. Figure S1. Flowchart of combined thresholds models. Table S2. Pathological types. Table S3. Delong test results for AUCs between different models.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, T., Xie, X., Ni, Z. et al. Quantitative evaluation of diffusion-weighted MRI for differentiating benign and malignant thyroid nodules larger than 4 cm. BMC Med Imaging 23, 212 (2023). https://doi.org/10.1186/s12880-023-01141-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-023-01141-z