Abstract
Background
Ultrasound imaging is used for diagnosis, treatment, and blood vessel visualization during venous catheter placement. However, various physiological factors (e.g., body temperature and exercise) influence vein diameters, which are expected to exhibit daily or diurnal fluctuations. Therefore, this study aimed to determine the intraday (short-term) and interday (long-term) reproducibility of repeated measurements of the depth and diameter of peripheral superficial veins.
Methods
Twenty-three healthy young women (mean age, 21.7 ± 0.8 years) participated in the study to examine the short- and long-term reproducibility of the depth and diameter of the cutaneous vein in the left elbow fossa acquired by ultrasound imaging. Short-term measurement intervals were 10 s, and the probe was released from the skin for each acquisition, which was repeated five consecutive times. Long-term measurements were performed at the same time on the next day following the same procedure. The acquired images were analyzed for vein depth and diameter using ImageJ software. The intraclass correlation coefficient (ICC) was calculated to determine the short- and long-term reproducibility of the measurements. The relationship between the venous depth and venous diameter intra-individual variation was analyzed, as well as the influence of body composition (body fat and muscle mass) on the venous diameter and depth.
Results
For vein depth measurements, the short- and long-term ICCs were 0.94–0.96 and 0.88, respectively. For the vein diameter, the short- and long-term ICCs were 0.94–0.97 and 0.67, respectively. The short-term ICCs for both vein depth and diameter exceeded 0.9, indicating that the ultrasound vascular measurement was sufficiently reliable. However, long-term reproducibility was slightly lower, especially for the vein diameter. No correlation was found between the intra-individual variation of the vein diameter and vein depth. Although the vein diameter and body fat mass uncorrelated, the vein depth and body fat mass significantly correlated (r = 0.675, 95% confidence interval = 0.281–0.830).
Conclusions
The long-term reproducibility of vein diameters was somewhat lower than that of the short-term reproducibility. This could be attributed to fluctuations in the physiological state of the participant rather than to the instability of the measurement. Therefore, ultrasound measurement of the peripheral superficial vein is sufficiently reliable.
Similar content being viewed by others
Background
Ultrasound imaging is an essential technique for diagnosis and treatment. Unlike computed tomography, X-ray, or magnetic resonance imaging, ultrasound imaging does not require large equipment and is free from the risk of X-ray exposure. Therefore, ultrasound imaging at the bedside is relatively easy, and a timely diagnosis can be made owing to real-time image acquisitions. Specifically, ultrasound imaging technology has evolved significantly over the past two decades, with devices becoming smaller and lighter [1], enabling its applications in various healthcare fields [2]. For example, it can be used for the assessment of cardiac dynamics in patients with heart failure and dialysis, focused assessment with sonography for trauma in the emergency room, and examination of bladder capacity and constipation [3,4,5,6]. In these imaging procedures, inter- and intra-observer agreements are important because the measurement accuracy might depend on the observer [7, 8].
Ultrasound imaging can be also utilized for blood vessel visualization during venous catheter placement [9]. Ultrasound-guided catheter insertion into difficult-to-access veins improves success rates compared with conventional blind insertion [10, 11]. This method can be also used to evaluate venous vasodilation interventions. Vessels with higher success rates for peripheral vein catheter insertion are more visible and palpable [9, 12, 13] and have larger diameters [14, 15]. Therefore, in previous studies on various interventions to facilitate venipuncture (e.g., local heating and postural changes), the vein diameter was used to evaluate their effectiveness [16,17,18,19,20].
Vein diameters are known to exhibit diurnal fluctuations [21]. Specifically, the inferior vena cava and peripheral veins of the lower extremities show great physiological variabilities [22, 23].
Several studies have been made on the intra- and inter-observer agreement of ultrasound vascular measurements, and the results were nearly perfect for intra-observer and considerably high for inter-observer [24,25,26,27]. Therefore, the accuracy of vein measurement depends on the magnitude of vasomotion, not on the reliability of the observer.
This study aimed to determine the intraday (short-term) and interday (long-term) reproducibility of repeated measurements of the depth and diameter of peripheral superficial veins.
Methods
Participants
The study enrolled 23 healthy young women who were not patients, smokers, or pregnant. Table 1 presents the demographic characteristics of the participant. The sample did not include obese individuals. During the study period, alcohol consumption was prohibited, and the participants were required to sleep at least 6 h beforehand. The participants also avoided strenuous exercise after waking up on the experiment day, finished eating at least 2 h before the experiment, and limited intake of stimulants and caffeine.
The study was approved by the ethics committee of the university where the study was conducted. The researchers explained the study’s content and obtained verbal and written informed consent before starting the study.
Procedures
This study was conducted for two consecutive days in October 2021. The air temperature in the laboratory was maintained at 25 °C. Initially, the participants changed into T-shirts and shorts made of the same material, and their body temperature, pulse rate, blood pressure, and height were measured. In addition, the total body muscle mass and body fat were recorded using a body composition analyzer (Inbody 270; Inbody, Tokyo, Japan). Then, the participants sat on a chair and placed their forearms on an 83-cm-high platform for 15 min. The elbow joint was aligned with the mark on the table, the forearm was kept extended, and the arm was fixed with a belt to prevent the arm from moving.
The same operator obtained B-mode transverse images of the median cutaneous vein or radial vein of the left elbow fossa by ultrasound imaging (Versana Active; GE Health Care, Tokyo, Japan) with a 10–12 MHz linear probe. During measurements, the probe was fixed to the stand and maintained at the same height. A 1-cm thick layer of gel was used to avoid compressing the vein with the probe’s pressure. The same probe was used for all measurements, and the scanner was set to an observable image depth of 20 mm. Gain was optimized for each participant. The skin at the probe application site was marked, and the beam was applied to the same vein each time. The interval between each imaging acquisition was approximately 10 s, and the probe was released once for each acquisition.
Image analysis
All images were saved on the device and converted to jpeg files, and these jpeg files were converted to 256-bit grayscale using ImageJ [28], a public domain software used for processing and analyzing scientific images: 1 pixel = 0.034 mm The images were analyzed at a resolution of 0.034 mm.
Figure 1 shows the analysis of the vein depth and diameter. First, a line was drawn on the skin surface, and the intima of the vein was traced manually while moving the line downward by 1 pixel. The vein depth was defined as distance from the skin surface to the intima and the vein diameter as the distance between the intima. The acquired images were analyzed blindly and randomly, and the participants were de-identified.
Statistical analysis
The intraclass correlation coefficient (ICC) was calculated for short-term and long-term reproducibility of measurements. Strictly, the ICC shown in this study is the reproducibility of one measurement (ICC [1,1]) and does not include interrater variation. The coefficients of variation (CVs) for the intra-individual variation in the depth and diameter measurements were also analyzed according to a previous study [29]. For the results of both vein depth and diameter, the average of five measurements for each experimental day was determined, and Bland–Altman plots were performed on the difference between 2-day measurements. A fixed bias and a proportional bias were tested by a paired t-test and Pearson correlation coefficient (r). Pearson’s correlation coefficients were also calculated to examine the relationship between vein depth and intra-individual variation of the diameter. Furthermore, the correlation of the vein depth and diameter against the body composition were also analyzed. Statistical analyses were performed using R software, version 4.1.0.
Results
Tables 2 and 3 show the results for depth and diameter, respectively. The mean vein depths ranged from 2.43 to 2.59 mm. Short-term and long-term ICCs ranged from 0.94 to 0.96 and 0.88, respectively. By contrast, vein diameters averaged 2.48 at 2.53 mm. Despite the high short-term ICC of 0.94–0.97, it decreased between days, resulting in a long-term ICC of 0.67. Tables 2 and 3 show the CVs for the depth and diameter measurements, respectively. Vein depth exhibited a 6–7% intra-individual variation for both long- and short-term variabilities. The CVs for the vein diameter were approximately 5–6% and 9% for the short-term and long-term variabilities, respectively.
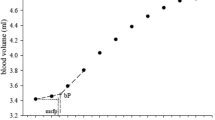
The Bland–Altman plots for vein depth and diameter are demonstrated in Fig. 2. For vein depth, there was no significant difference between two experimental days (p = 0.12), thus no fixed bias in vein depth. As for proportional bias, a positive correlation (r = − 0.30) was found although it is not significant (p = 0.16). As for vein diameter, fixed bias (p = 0.69) and proportional bias (r = − 0.13, p = 0.54) were also insignificant.
Bland–Altman plots for vein depth (left) and vein diameter (right). The differences (y axis) between the mean values obtained in 2 experimental days were plotted against their mean value (x axis). Dashed lines designated upper and lower limits of 95% confidence interval of the difference. Fixed and proportional biases were not found in either vein depth or vein diameter
A correlation between the mean vein depth and intra-individual CV of the vein diameter is shown in Fig. 3. The correlation coefficient (r) was 0.056; thus, the correlation was not significant.
Body fat mass and total body muscle mass were examined in relation to the vein depth and diameter, respectively (Figs. 4 and 5). Body fat mass was significantly positively correlated with the vein depth (r = 0.675, 95% CI = 0.281–0.830) but not with the muscle mass (r = 0.138, 95% CI = − 0.318–0.515). Furthermore, neither body fat mass nor muscle mass correlated with the vein diameter.
Discussion
In this study, to examine the reproducibility of the ultrasound measurement of the vein diameter and vein depth, repeated measurements were performed with short- (10 s) and long-term (24 h) intervals. For short-term reproducibility, ICCs ranged from 0.94 to 0.97 for vein diameter and 0.94–0.96 for vein depth. The long-term reproducibility was 0.67 for vein diameter and 0.88 for depth. Short-term reproducibility did not differ much between the vein diameter and depth, but the long-term reproducibility of vein diameter was considerably lower than that of depth.
This study also examined the relationships between body composition, vein depth, and vein diameter. Vein depth and body fat mass positively correlated, whereas vein diameter did not correlate with either body fat mass or total body muscle mass.
Sharp et al. [30] reported that the body mass index (BMI) had little effect on the vein diameter. Kim et al. [31] did not find a relationship between the vein diameter and BMI, although BMI influenced depth. The results of the present study were consistent with their findings.
Since fat mass is unlikely to change in a few days, it appears reasonable that depth is more reproducible over time than diameter.
As shown in Table 3, the peripheral forearm vein diameter indicated approximately 5% (short-term) or 9% (long-term) variability. Previous studies have demonstrated 18–75% variation in the diameter of the inferior vena cava and 7–10% for the veins of the lower extremities [22, 23]. Although the methods of measurement and analysis differed between the previous study and the present study, the variation of the forearm superficial vein was much smaller than that of the inferior vena cava and almost the same as that of lower extremity veins when roughly recognized. Venous variation might be greater in the center and smaller in the periphery. Most studies on venous variability have focused on the central vein, such as the inferior vena cava [22, 32]. In contrast, the present study focus was on the peripheral superficial veins. The novelty of the current study is the quantitative demonstration of the variation of the forearm superficial veins.
The main cause of the variation in the diameter of the vein (e.g., inferior vena cava, axillary vein) is respiration [22, 32]—the diameter of the vein is known to contract with inspiration and to dilate with expiration [33, 34]. Therefore, respiratory modulation would be expected in the peripheral superficial vein as same as the inferior vena cava. We cannot determine whether the variability could be attributed to respiratory modulation because respiration was not measured in this study. Further studies on the effect of respiration on peripheral superficial vein diameters are required.
This study has some limitations. First, the presented results on short-term reproducibility are limited to variations of a few minutes. In this study, long-term measurements were conducted at the same time on different days; therefore, the results excluded the effects of diurnal variation. Further research is needed to determine the factors that affect the reproducibility of vein diameter measurements. Second, the participants of this study were limited to young healthy women. Sharp et al. [30] reported that men tend to have larger venous diameters than women. Therefore, there could be sex differences also in diameter variability. Future studies are expected to take into account the influence of demographics such as age and race in addition to sex.
Conclusions
Short-term measurements of the depth and diameter of peripheral superficial veins showed excellent reproducibility. The vein diameter indicated a slightly lower long-term reproducibility than the short term. The larger day-to-day variations in vein diameter can be attributed to the variation in the physiological condition of the participants rather than to the instability of the measurement. Therefore, ultrasound measurement of the peripheral superficial vein is sufficiently reliable.
Availability of data and materials
The datasets used and/or analyzed in the current study are available from the corresponding author on reasonable request.
Abbreviations
- ICC:
-
Intraclass correlation coefficient
- CV:
-
Coefficient of variation
- SD:
-
Standard deviation
- CI:
-
Confidence interval
- BMI:
-
Body mass index
References
Lee L, DeCara JM. Point-of-care ultrasound. Curr Cardiol Rep. 2020;22:149.
Mariani PJ, Setla JA. Palliative ultrasound for home care hospice patients. Acad Emerg Med. 2010;17:293–6.
Steinwandel U, Gibson NP, Rippey JC, Towell A, Rosman J. Use of ultrasound by registered nurses-a systematic literature review. J Ren Care. 2017;43:132–42.
Totenhofer R, Luck L, Wilkes L. Point of care ultrasound use by registered nurses and nurse practitioners in clinical practice: an integrative review. Collegian. 2021;28:456–63.
Suzuki M, Iguchi Y, Igawa Y, Yoshida M, Sanada H, Miyazaki H, Homma Y. Ultrasound-assisted prompted voiding for management of urinary incontinence of nursing home residents: efficacy and feasibility. Int J Urol. 2016;23:786–90.
Matsumoto M, Yoshida M, Yabunaka K, Nakagami G, Miura Y, Fujimaki S, et al. Safety and efficacy of a defecation care algorithm based on ultrasonographic bowel observation in Japanese home-care settings: a single-case, multiple-baseline study. Geriatr Gerontol Int. 2020;20:187–94.
Lan Y, Li N, Song Q, Zhang M-b, Luo Y-k, Zhang Y. Correlation and agreement between superb micro-vascular imaging and contrast-enhanced ultrasound for assessing radiofrequency ablation treatment of thyroid nodules: a preliminary study. Image and clinical analysis of common carotid web: a case report. BMC Med Imaging. 2021;21:175.
Schlunk F, Kuthe J, Harmel P, Audebert H, Hanning U, Bohner G, et al. Volumetric accuracy of different imaging modalities in acute intracerebral hemorrhage. BMC Med Imaging. 2022;22:9.
Van Loon FHJ, Buise MP, Claassen JJF, Dierick-van Daele ATM, Bouwman ARA. Comparison of ultrasound guidance with palpation and direct visualisation for peripheral vein cannulation in adult patients: a systematic review and meta-analysis. Br J Anaesth. 2018;121:358–66.
Bahl A, Pandurangadu AV, Tucker J, Bagan M. A randomized controlled of ultrasound for nurse-performed IV placement in difficult access ED patients. Am J Emerg Med. 2016;34:1950–4.
Duran-Gehring P, Bryant L, Reynolds JA, Aldridge P, Kalynych CJ, Guirgis FW. Ultrasound-guided peripheral intravenous catheter training results in physician-level success for emergency department technicians. J Ultrasound Med. 2016;35:2343–52.
Yalçınlı S, Akarca FK, Can Ö, Şener A, Akbinar C. Factors affecting the first-attempt success rate of intravenous cannulation in older people. J Clin Nurs. 2019;28:2206–13.
Van Loon FHJ, Van Hooff LWE, De Boer HD, Koopman SSHA, Buise MP, Korsten HHM, et al. The modified A-DIVA scale as a predictive tool for prospective identification of adult patients at risk of a difficult intravenous access: a multicenter validation study. J Clin Med. 2019;8:144.
Witting MD, Schenkel SM, Lawner BJ, Euerle BD. Effects of vein width and depth on ultrasound-guided peripheral intravenous success rates. J Emerg Med. 2010;39:70–5.
Panebianco NL, Fredette JM, Szyld D, Sagalyn EB, Pines JM, Dean AJ. What you see (sonographically) is what you get: vein and patient characteristics associated with successful ultrasound-guided peripheral intravenous placement in patients with difficult access. Acad Emerg Med. 2009;16:1298–303.
Yamagami Y, Tomita K, Tsujimoto T, Inoue T. Tourniquet application after local forearm warming to improve venodilation for peripheral intravenous cannulation in young and middle-aged adults: a single-blind prospective randomized controlled trial. Int J Nurs Stud. 2017;72:1–7.
Tokizawa Y, Tsujimoto T, Inoue T. Duration of venodilation for peripheral intravenous cannulation, as induced by a thermal stimulus on the forearm. Biol Res Nurs. 2017;19:206–12.
Yamagami Y, Tsujimoto T, Inoue T. How long should local warming for venodilation be used for peripheral intravenous cannulation? A prospective observational study. Int J Nurs Stud. 2018;79:52–7.
Sharp R, Childs J, Bulmer AC, Esterman A. The effect of oral hydration and localised heat on peripheral vein diameter and depth: a randomised controlled trial. Appl Nurs Res. 2018;42:83–8.
Yamagami Y, Inoue T. Patient position affects venodilation for peripheral intravenous cannulation. Biol Res Nurs. 2020;22:226–33.
Aellig WH. Clinical pharmacology, physiology and pathophysiology of superficial veins-1. Br J Clin Pharmacol. 1994;38:181–96.
Gignon L, Roger C, Bastide S, Alonso S, Zieleskiewicz L, Quintard H, et al. Influence of diaphragmatic motion on inferior Vena cava diameter respiratory variations in healthy volunteers. Anesthesiology. 2016;124:1338–46.
Shibasaki S, Kishino T, Yokoyama T, Sunahara S, Harashima K, Nakajima S, et al. Sonographic detection of physiological lower leg oedema in the late afternoon in healthy young women. Clin Physiol Funct Imaging. 2020;40:381–4.
Sharp R, Gordon A, Mikocka-Walus A, Childs J, Grech C, Cummings M, Esterman A. Vein measurement by peripherally inserted central catheter nurses using ultrasound: a reliability study. JAVA J Assoc Vasc Access. 2013;18:234–8.
Steinwandel U, Gibson N, Towell A, Rippey JJR, Rosman J. Can a renal nurse assess fluid status using ultrasound on the inferior vena cava? A cross-sectional interrater study. Hemodial Int. 2018;22:261–9.
Fields JM, Lee PA, Jenq KY, Mark DG, Panebianco NL, Dean AJ. The interrater reliability of inferior Vena cava ultrasound by bedside clinician sonographers in emergency department patients. Acad Emerg Med. 2011;18:98–101.
Mesin L, Giovinazzo T, D’Alessandro S, Roatta S, Raviolo A, Chiacchiarini F, et al. Improved repeatability of the estimation of pulsatility of inferior Vena cava. Ultrasound Med Biol. 2019;45:2830–43.
Schindelin J, Arganda-Carreras I, Frise E, Kaynig V, Longair M, Pietzsch T, et al. Fiji: an open-source platform for biological-image analysis. Nat Methods. 2012;9:676–82.
Kobayashi H. Inter- and intra-individual variations of heart rate variability in Japanese males. J Physiol Anthropol. 2007;26:173–7.
Sharp R, Cummings M, Childs J, Fielder A, Mikocka-Walus A, Grech C, Esterman A. Measurement of vein diameter for peripherally inserted central catheter (PICC) insertion: an observational study. J Infus Nurs. 2015;38:351–7.
Kim IS, Kang SS, Park JH, Hong SJ, Shin KM, Yoon YJ, Kim MS. Impact of sex, age and BMI on depth and diameter of the infraclavicular axillary vein when measured by ultrasonography. Eur J Anaesthesiol. 2011;28:346–50.
Ma Q, Shi X, Ji J, Chen L, Tian Y, Hao J, et al. The diagnostic accuracy of inferior vena cava respiratory variation in predicting volume responsiveness in patients under different breathing status following abdominal surgery. BMC Anesthesiol. 2022;22:1–12.
Lim KJ, Lee JM, Byon HJ, Kim HS, Kim CS, Lee SK, et al. The effect of full expiration on the position and size of the subclavian vein in spontaneously breathing adults. Anesth Analg. 2013;117:109–13.
Folino A, Benzo M, Pasquero P, Laguzzi A, Mesin L, Messere A, et al. Vena cava responsiveness to controlled isovolumetric respiratory efforts. J Ultrasound Med. 2017;36:2113–23.
Acknowledgements
We would like to express our sincere gratitude to all participants for their time participating in this study.
Funding
This study was supported by JSPS KAKENHI Grant Number JP 20K19023.
Author information
Authors and Affiliations
Contributions
MM contributed to the conception, study design, data acquisition, analysis and interpretation, and drafting of the manuscript. HN contributed to study design, data acquisition, and critical revision of the manuscript. KH contributed to study design, data analysis and interpretation, and writing of the manuscript and critical revision of the manuscript. All authors read and approved the submitted version.
Authors’ information
Matsumoto Miharu is affiliated with the Department of Nursing, Kyushu University, and is also enrolled in the doctoral program at Ishikawa Prefectural College of Nursing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted following the ethical principles stated in the Declaration of Helsinki. Ethical approval for the study was obtained from the Clinical Research Ethics Committee of Kyushu University Hospital (Approval no. 2021–276). We provided written informed consent to the participants and obtained their approval.
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Miharu, M., Nobuko, H. & Hiromitsu, K. Short- and long-term reproducibility of peripheral superficial vein depth and diameter measurements using ultrasound imaging. BMC Med Imaging 22, 212 (2022). https://doi.org/10.1186/s12880-022-00945-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-022-00945-9