Abstract
Background
HIV/AIDS has left a profound impact, leading to significant mortality, morbidity, economic strain, and disability on a global scale. The introduction of antiretroviral therapy (ART) has played a pivotal role in mitigating the economic burden of HIV and enhancing overall productivity. However, the emergence of virological failure presents a critical contemporary challenge within global health, reflecting the complexity of effectively managing HIV treatment outcomes in the 21st century.
Methods
An institutional based, cross-sectional study was conducted. Data were collected using a pretested, structured checklist. Data were edited and cleaned using Microsoft Excel 2016 and analyzed using SPSS version 25. Baseline demographic and clinical data were summarized using descriptive statistics. Multiple logistic regression analysis was run to identify association between dependent and independent variables, by computing odds ratio and 95% confidence interval. A p-value < 0.05 was considered significant.
Results
The study delved into the health profile of 117 individuals who were receiving treatment with a third-line antiretroviral therapy (ART) regimen. The findings revealed that the median age of the participants stood at 44 (IQR = ± 17) years and male accounted 53%. The median duration of after HIV diagnosis was found to be 14.25 (± IQR = 5.71) years. Overall virological suppression after third line ART was 76.9% at 6 months. Following adjustment with multiple variable logistic regression, good adherence to medication showed statistical significance in achieving virologic suppression (AOR = 8.48(95% CI: 2.3–30.8), p = 0.001). In contrast, the absence of a change in the second line regimen (AOR = 3.0(95% CI: 0.36–24.8), p = 0.31) and receiving second-line medication for less than three years (AOR = 1.07(95% CI: 0.39–2.95), p = 0.89), and baseline viral load above 100,000 (AOR = 1.74(0.64–2.95), p = 0.27) shows statistically non-significant association with virologic suppression.
Clinical trial number:
Not applicable.
Conclusion
This multicenter study provides strong evidence on virological suppression following the use of third-line antiretroviral therapy drugs in Ethiopia. The results of the study indicate rate of Virological suppression after starting third-line ART drugs is significantly linked to good adherence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
HIV/AIDS stands as one of the most pervasive global communicable diseases [1, 2], posing significant challenges in its control and prevention throughout the 21st century [2]. Its impact is notably pronounced in low and middle-income countries, where it exerts a substantial burden on various fronts, including mortality, morbidity, disability, and economic loss [1,2,3]. A comprehensive assessment of the global burden of diseases has brought to light the staggering the prevalence of HIV/AIDS, with an estimated 36.85 million cases reported globally in 2019 [2, 3]. This substantial figure underscores the continued impact of this pervasive infectious disease on a global scale. Tragically, the data also indicates that a significant number of individuals succumbed to HIV/AIDS-related complications, with approximately 860,000 deaths and 47.63 million DALYS recorded worldwide in the 2019 [3]. The human immunodeficiency virus (HIV) is a virus with reverse transcriptase activity that mainly target the body’s immune system and expose to opportunistic infection and malignancies which finally results in a disease called acquired immunodeficiency syndrome (AIDS) [1]. The introduction of antiretroviral therapy (ART) has significantly impacted the reduction of HIV-related morbidity and mortality, effectively transforming the infection from a once formidable and devastating disease into a condition that is now largely manageable. This transformation underscores the profound positive influence of ART on the lives of individuals living with HIV, marking a pivotal shift in the management and outlook of the infection [4]. In addition, ART restores immune function, reduces HIV related adverse outcomes and prolong life expectancy of HIV-infected individuals; However, the long duration of treatment decreases the therapeutic and preventive effects of ART drugs resulted in treatment failure. Treatment failure in HIV/AIDS management is a critical stage marked by the progression of the disease despite the initiation of antiretroviral (ARV) drugs. In 2025, a total of 28.5 million person-years of Antiretroviral Therapy (ART) will be administered [5]. Of this total, 24.3 million person-years were on first-line treatment, 3.5 million person-years were on second-line treatment, and 0.6 million person-years were on third-line treatment [5]. Several observational studies conducted in various countries have illuminated varying rates of virological response subsequent to the administration of third-line antiretroviral therapy (ART) drugs. These studies have revealed that the response to third-line ART regimens can differ across diverse geographic locations, indicating unique patterns and challenges in achieving virological suppression following the implementation of advanced treatment protocols. A large clinical trial involving 545 participants who had virological failure for second line ART, aiming to assess the efficacy of a third-line antiretroviral therapy (ART) intervention, was a major, multi-country endeavor conducted across various low- and middle-income countries (LMIC) in 19 urban sites located across 10 different countries with encompassed a population representing a wide spectrum of cultural, socioeconomic, and geographic backgrounds, revealed a virological failure rate of 36% [6]. This outcome underscores the challenges and complexities associated with managing HIV/AIDS in diverse populations, signaling the need for targeted and adaptable approaches to treatment in the context of varied cultural, socioeconomic, and virological landscapes. In a cohort of 257 patients in Thailand who initiated third-line regimens, the study found that a high percentage of them achieved viral load suppression to less than 200 copies/ml at various time points. At 48 weeks into the treatment, 87% of the patients had successfully achieved viral load suppression. This percentage slightly decreased to 86% at 96 weeks, indicating a sustained response to the treatment over time. By 144 weeks, the percentage of patients with viral load suppression dropped to 83%, suggesting some variability in treatment response among individuals. Finally, at 168 weeks, 80% of the patients still maintained viral load suppression, highlighting the long-term effectiveness of the third-line regimens in managing HIV infection in this cohort [7]. A meta-analysis of 33 studies involving a total of 18,550 participants found that the rate of second-line antiretroviral therapy failure requiring third-line treatment was 15 per 100 individuals in the Sab-Sahara region [8].
In numerous observational studies, a multitude of risk factors have consistently been associated with virological failure following the administration of third-line antiretroviral therapy (ART) drugs [8,9,10,11]. These findings emphasize the diverse array of factors that play crucial roles in impacting the virological response to advanced ART regimens, highlighting the need for comprehensive and multifaceted approaches to address virological failure in this context [9, 11]. Several comprehensive studies have identified a range of significant risk factors linked to virological failure following the initiation of antiretroviral therapy (ART). These factors include poor adherence, low CD4 cell count at treatment initiation, the presence of HIV-related stigma, substance use, low income, the number of administered drugs, duration of ART use, and the co-infection of tuberculosis and HIV. These findings collectively underscore the multifaceted nature of HIV treatment, emphasizing the importance of addressing a spectrum of factors to optimize treatment outcomes and overall patient well-being [8, 9, 11].Addressing the challenges associated with the high burden of HIV/AIDS, the rising demand for third-line ART drugs, and the increasing rate of virological failure of third-line ART regimens requires a comprehensive local study that considers various important attribute factors associated to the problem.
Methods and materials
Study area and setting study setting, design and period
Institutional based multicenter cross-sectional study was conducted from January 01 to January 24, 2024 at Public hospitals of Addis Ababa, Ethiopia which are currently providing third line HIV treatment. Addis Ababa is the capital and largest city of Ethiopia. The current estimated population of the city is 5.7 million. According to FMOH there are 13 hospitals and 98 health centers in the city [6]. Third line ART is being given in two hospitals under the city administration and three federal hospitals. These hospitals are Yekatit 12 Hospital medical college, Zewditu Memorial Hospital, St Paul’s Hospital Millennium medical college, ALERT hospital and Tikur Anbessa Specialized hospital. This study included all these hospitals except Tikur Anbessa Specialized hospital. Currently the four hospitals are providing third line HIV treatment for 140 patients.
Source population and study population
The study included all HIV patients age >/=18 on third line HIV treatment having follow-up in Yekatit 12 Hospital medical college, Zewditu Hospital, St Paul’s Hospital Millennium medical college, and ALERT hospital. Those patients without documented Viral load at the start of treatment as well as at 6th months of treatment and patients with incomplete socio-demographic and clinical data were excluded from the study.
Sample size determination and sampling techniques
The sample size for this study is calculated using a single population proportion formula. Taking Virological suppression rate of third line ART at 6 month 64% from an earlier large multicenter including multiple African countries [7] the sample size is calculated as: \(\:\text{n}=\frac{{\left(\frac{\text{Z}\text{a}}{2}\right)}^{2.}}{{\text{d}}^{2}}\text{p}.\text{q}\)=\(\:\frac{{\left(1.645\right)}^{2}}{{\left(0.05\right)}^{2}}\text{*}0.64\text{*}0.36\)=249.4, where n = the required sample size; p = Virological suppression rate of third line ART at 6 month = 0.64; Z = the critical value at 90% confidence level = 1.645, and e = margin of error = 5%. Accordingly, the minimum required sample size became\(\:250\). But the total number of patients on third line ART was 140 which is less than the calculated sample size we took all patients into the study and we used non probability sampling techniques. The confidence interval of the rate was calculated with Poisson distribution and formula.
Study variables
Viral load at 6 month of Third line ART was the dependent variable and the independent variables were Age, Sex, Marital status, Religion, Educational status, Occupation, Duration of HIV, Base line viral load, Functional status, WHO clinical stage, Presence of opportunist infection, Drug adherence, The last Second-line ART regimen before switch to 3rd line, Duration on second line regimen, History of regimen change during 2nd line treatment, Third-line ARV regimen and Follow-up site of second line regimen.
Operational definitions
Virologic suppression was defined as viral load result equal to or less than 1000 copies/ml at 6th month of treatment. Virological failure was defined as viral load above 1000 copies/ml at 6th month of treatment. Poor adherence was defined as >/=1 documented poor (P) or Fair (F) adherence on the monthly follow-up chart within 6 months and Good adherence was defined as all adherence documented as good (G) on the monthly follow-up chart within 6 months. The Baseline Viral load was the viral load before a patient is switched to third line ART [5].
Data collection procedures
A structured data collection tool developed in English after reviewing different literatures. Data was extracted using structured and pretested collection tool from chart review and electronic medical records. Data was extracted by trained general practitioners and ART expert Nurses.
Data quality control and confidentiality
Data collection tool was developed after reviewing different validated questioner from previous published literature. The tool was pretested by 5% before data collection. Training was given for data collectors. Checking of the questioner was done at the end of each day of data extraction for consistency, completeness, clarity and accuracy.
Data analysis
After checking the data for consistency, completeness, clarity and accuracy it was coded manually, fed into a spreadsheet and analyzed using Statistical Package for Social Sciences (SPSS) version 25.0. Descriptive information was determined to describe the socio demographic. Categorical variables described as proportions, and chi-square or Fisher’s exact tests used to compare them. Continuous variables were tested for normality by Shapiro Wilk test and presented as mean with standard deviation (SD) (Mean ± SD) when the data was normally distributed or median with interquartile range (IQR) (Median ± IQR) when the data was not normally distributed. Bivariate analysis was performed to test factors associated with Virological failure at 6month after Third line ART drug. Variables with p-value 0.25 and less in the bivariate analysis entered into the multivariable binary logistic model. A multiple logistic regression model was done using backward selection to identify independent risk factors. P-value less than 0.05 was considered to determine the statistical significance of the association and odds ratio with a 95% confidence interval was used to determine the presence, strength, and direction of association between covariates and the outcome variable.
Results
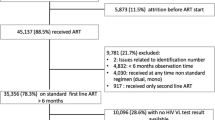
The comprehensive examination of the demographic, social, and occupational attributes of the individuals receiving third-line ART treatment are described in Table 1. The study delved into the health profile of 140 patients who received treatment with a third-line ART regimen and from these 23 were excluded based on the exclusion criteria while 117 individuals who fulfilled the inclusion criteria were studied. The findings revealed that the median age of the participants stood at 44 (± IQR = 17) years. The study highlighted that the individuals were predominantly engaged in government (29.9%) and private employment (26.6%). The findings indicated that the majority of the individuals possessed a workable (92.3%) functional status(Table 1).
The median duration of HIV was found to be 14.25 (± IQR = 5.71) years, signifying a prolonged period of medication exposure. The World Health Organization (WHO) staging of the patients predominantly revealed that most individuals were classified under Stage 1 (67.5%) and Stage 3 (20.5%). The findings revealed that a majority of the patients exhibited good adherence (87.2%) to their ART regime. An analysis of the patient group revealed that 23.1% (95%CI:14.4–31.8%) of these individuals exhibited a virological failure after 6 months of initiation of third line ART and viral suppression was 76.9% (95%CI: 61–93%). (Table 2)
Virological suppression after third-line antiretroviral therapy (ART) can be attributed to a variety of factors, including patient-related, clinical, and drug-related factors. Bivariate analysis has shown that good drug adherence is the only factor that was statistically significant associated factor with virological suppression in this study. The crude odds ratio (COR) for good drug adherence in relation to virological suppression was 10 (95%CI: 3.3, 32.97), p = 0.000. Although factors such as being male, having a duration of HIV infection of less than 10 years, being at an early WHO stage, high baseline viral load and having a higher level of education were associated with virological suppression, these associations did not reach statistical significance in the study. In the bivariate analysis, the following findings were observed: workable functional status (COR = 1.15(95% CI: 0.34–3.81), p = 0.82), age below 44-year (COR = 1.59(95% CI: 0.66–3.80) p = 0.29) and absent opportunistic infection (COR = 1.35(95% CI: 0.35–5.14), p = 0.66) (Table 3). In multiple variable logistic regression, good adherence to medication showed statistical significance in achieving viral suppression (AOR = 8.48(95% CI: 2.3–30.8), p = 0.001). In contrast, the absence of a change in the second line regimen (AOR = 3.0(95% CI: 0.36–24.8), p = 0.31) and baseline viral load above 100,000 (AOR = 1.74(0.64–2.95), p = 0.27) were not statistically significant factors associated with virologic suppression (Table 4).
Discussion
The study, encompassing 117 patients from multi-center receiving third-line ART drugs, identified a significant virological suppression rate of 76.9% at the 6-month assessment point. This outcome holds substantial implications, shedding light on the challenges associated with managing treatment-resistant HIV cases and prompting critical considerations for patient care and therapeutic strategies. Several observational studies and randomized control trials conducted in various countries have illuminated varying rates of virological response subsequent to the administration of third-line ART drugs [6, 7, 9]. These studies have revealed that the response to third-line ART regimens can differ across diverse geographic locations, indicating unique patterns and challenges in achieving virological suppression following the implementation of advanced treatment protocols [6, 7, 10]. A retrospective analysis of 232 PLWHIV patients who started third-line antiretroviral therapy at a single center in New Delhi India revealed a virological failure rate of 71.5% at the 6-month [10]. In a recent study conducted across multiple centers in Zimbabwe, researchers found a virological failure rate of 79% at the 6-month after the initiated third line ART drugs. A large clinical trial involving 545 participants who had virological failure for second line ART, aiming to assess the efficacy of a third-line ART intervention, was a major, multi-country endeavor conducted across various low- and middle-income countries (LMIC) in 19 urban sites located across 10 different countries with encompassed a population representing a wide spectrum of cultural, socioeconomic, and geographic backgrounds, revealed a virological failure rate of 64% [6]. The absence of studies reporting virological failure rates after third-line ART drugs in Ethiopia amidst varying rates reported across different regions underscores a critical gap in our understanding of HIV management and difficulty in comparing with the current rate to forecast the progress.
These finding raise questions about the factors contributing to this high rate of treatment failure across different countries of the world. Possible reasons for the high virological failure rate could include issues such as medication adherence, drug resistance, healthcare infrastructure limitations, and socio-economic factors [9]. Several observational studies have consistently pointed to a significant correlation between poor drug adherence and virological failure subsequent to the use of third-line ART drugs. This association has been a recurring finding across various research endeavors, highlighting the critical impact of medication adherence on treatment outcomes in the context of advanced HIV management [9]. In our univariate analysis, we found statistical significance in the association between good drug adherence and virological suppression subsequent to the use of third-line ART drugs. Our findings suggest that poor drug adherence is a significant contributing factor to virological failure in the context of third-line ART, shedding light on the critical impact of medication adherence on treatment outcomes. In multiple observational studies, a range of factors including the WHO stage, low CD4 count, comorbidities, BMI, opportunistic infections, and sociodemographic elements have been consistently associated with virological failure subsequent to the utilization of third-line ART drugs. These findings underscore the multifaceted nature of virological outcomes and emphasize the importance of considering various clinical, health, and demographic factors in understanding virological responses to advanced ART regimens.
HIV/AIDS along high rate of virological failure exerts profound toll on affected communities and healthcare systems, contributing to increased mortality rates, illness, and disability among affected individuals. Moreover, its impact extends to economic spheres, where the associated burden is felt through increased healthcare costs, loss of productivity, and a strain on socioeconomic resources.
Addressing the challenges associated with the high burden of HIV/AIDS, the rising demand for third-line ART drugs, and the increasing rate of virological failure of third-line ART regimens requires a comprehensive approach that considers various important attribute factor. Poor adherence to ART medications is a common factor contributing to virological failure. Strategies to improve treatment adherence, such as patient education, counseling, reminder systems, and support services, are essential to ensure the effectiveness of ART regimens [9]. Regular monitoring of viral load levels and drug resistance testing is crucial for detecting early signs of virological failure and adjusting treatment regimens accordingly. Healthcare providers need access to reliable testing facilities and guidelines for interpreting test results to effectively manage drug-resistant HIV strains. Ensuring equitable access to second and third-line ART drugs is essential for individuals who experience treatment failure or develop drug resistance. Efforts to expand access to these medications, reduce costs, and improve distribution channels are needed to meet the growing demand for advanced treatment options. Continued research into new antiretroviral drugs, treatment strategies, and technologies is essential for addressing the evolving challenges of HIV/AIDS treatment. Investing in research and development initiatives can lead to the discovery of more effective and tolerable ART regimens for individuals with drug-resistant HIV strain. Strengthening healthcare infrastructure, training healthcare providers, and building capacity in HIV/AIDS treatment and management are critical for ensuring quality care and support for individuals living with HIV/AIDS. Investing in healthcare systems and workforce development can enhance the delivery of ART services and improve patient outcomes. Engaging communities, raising awareness about HIV/AIDS prevention and treatment, and providing social support services are important for promoting adherence to treatment regimens, reducing stigma, and empowering individuals living with HIV/AIDS. Community-based interventions can play a significant role in improving treatment outcomes and addressing the challenges associated with virological failure. This data emphasizes the urgent need for continued research, public health interventions, and resource allocation to effectively address the challenges posed by HIV/AIDS, reduce its impact, and improve the prospects for those affected by this formidable global health challenge.
The limitation of this study was use of a single viral load measurement and inability to assess additional factors like substance use, comorbidity status and body mass index because of poor medical record documentation. Drug resistance testing’ was not done which can be one of the most important reasons for virological non suppression.
Conclusion
This multicenter study provides strong evidence on virological suppression following the use of third-line antiretroviral therapy drugs in Ethiopia. The results of the study indicate a concerning rate of virological failure after starting third-line ART drugs, which is significantly linked to poor adherence.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AIDS:
-
Acquired immune deficiency syndrome
- ART:
-
Antiretroviral therapy
- ARV:
-
Anti retroviral
- BMI:
-
Body mass index
- DRV/r:
-
Darunavir boosted with ritonavir
- DTG:
-
Dolutegravir
- EFV:
-
Efavirnez
- FDA:
-
Food and drugs administration
- FLD:
-
First line drug
- HAART:
-
Highly active antiretroviral therapy
- HIV:
-
Human immunodeficiency virus
- HIVTF:
-
Human immune virus treatment failure
- INSTI:
-
Integrase strand transfer inhibitor
- MRN:
-
Medical record number
- OI:
-
Opportunistic infection
- PIs:
-
Protease inhibitors
- PLHIV:
-
People living with HIV
- PYs:
-
Person years
- RVI:
-
Retroviral infected
- SSA-:
-
Sub-Saharan Africa
- SLD-:
-
Second line drug
- TDF-:
-
Tenofovir Disoproxil Fumarat
- UNAIDS-:
-
Joint United Nations Programme on HIV/AIDS
- 2e-:
-
AZT + 3TC + LPV/r
- 2f -:
-
AZT + 3TC + ATV/r
- 2 g-:
-
TDF + 3TC+-LPV/r
- 2 h-:
-
TDF + 3TC + ATV/r
- 2i-:
-
ABC + 3TC + LPV/r
- 2j- :
-
Other adult second line regimen
- 3a-:
-
DRV/r + DTG + AZT + 3TC
- 3b-:
-
DRV/r + DTG + TDF + 3TC
- 3D-:
-
DRV/r + ABC + EFV + 3TC
- 3c-:
-
Other adult third line regimen
- 5j-:
-
Other pediatric 2nd line regimen
- 5n-:
-
AZT + 3TC + DTG
References
WHO HIV 2022: [Accessed Feb 1. 2024: https://www.who.int/data/gho/data/themes/hiv-aids
Sashini, Payagala. Anton Pozniak:The global burden of HIV:Clinics in Dermatology;2024, 42(2) Pages 119–127, ISSN 0738-081X,:https://doi.org/10.1016/j.clindermatol.2024.02.001
Tian X, Chen J, Wang X, Xie Y, Zhang X, Han D, Fu H, Yin W, Wu N. Global, regional, and national HIV/AIDS disease burden levels and trends in 1990–2019: a systematic analysis for the global burden of disease 2019 study. Front Public Health. 2023;11:1068664. https://doi.org/10.3389/fpubh.2023.1068664. PMID: 36875364; PMCID: PMC9975742.
Katabira ET, Oelrichs RB. Scaling up antiretroviral treatment in resource-limited settings: successes and challenges. AIDS. 2007;21 Suppl 4:S5-10. https://doi.org/10.1097/01.aids.0000279701.93932.ef. PMID: 17620753.
Gupta A, Juneja S, Vitoria M, Habiyambere V, Nguimfack BD, Doherty M, Low-Beer D. Projected uptake of New Antiretroviral (ARV) Medicines in adults in low- and Middle-Income countries: a Forecast Analysis 2015–2025. PLoS ONE. 2016;11(10):e0164619. https://doi.org/10.1371/journal.pone.0164619. PMID: 27736953; PMCID: PMC5063297.
Grinsztejn B, Hughes MD, Ritz J, Salata R, Mugyenyi P, Hogg E, Wieclaw L, Gross R, Godfrey C, Cardoso SW, Bukuru A, Makanga M, Faesen S, Mave V, Wangari Ndege B, Nerette Fontain S, Samaneka W, Secours R, van Schalkwyk M, Mngqibisa R, Mohapi L, Valencia J, Sugandhavesa P, Montalban E, Avihingsanon A, Santos BR, Kumarasamy N, Kanyama C, Schooley RT, Mellors JW, Wallis CL, Collier AC. A5288 Team. Third-line antiretroviral therapy in low-income and middle-income countries (ACTG A5288): a prospective strategy study. Lancet HIV. 2019;6(9):e588-e600. doi: 10.1016/S2352-3018(19)30146-8. Epub 2019 Jul 29. PMID: 31371262; PMCID: PMC6857629.
Avihingsanon A, Hughes MD, Salata R, Godfrey C, McCarthy C, Mugyenyi P, Hogg E, Gross R, Cardoso SW, Bukuru A, Makanga M, Badal-Aesen S, Mave V, Ndege BW, Fontain SN, Samaneka W, Secours R, Van Schalkwyk M, Mngqibisa R, Mohapi L, Valencia J, Sugandhavesa P, Montalban E, Munyanga C, Chagomerana M, Santos BR, Kumarasamy N, Kanyama C, Schooley RT, Mellors JW, Wallis CL, Collier AC, Grinsztejn B. A5288 study team. Third-line antiretroviral therapy, including raltegravir (RAL), darunavir (DRV/r) and/or etravirine (ETR), is well tolerated and achieves durable virologic suppression over 144 weeks in resource-limited settings: ACTG A5288 strategy trial. J Int AIDS Soc. 2022;25(6):e25905. https://doi.org/10.1002/jia2.25905. PMID: 36039892; PMCID: PMC9332128.
Edessa D, Sisay M, Asefa F. Second-line HIV treatment failure in sub-Saharan Africa: A systematic review and meta-analysis. PLoS One. 2019;14(7):e0220159. https://doi.org/10.1371/journal.pone.0220159. Erratum in: PLoS One. 2019;14(9):e0223158. PMID: 31356613; PMCID: PMC6663009.
SeyedAlinaghi S, Afsahi AM, Moradi A, Parmoon Z, Habibi P, Mirzapour P, Dashti M, Ghasemzadeh A, Karimi E, Sanaati F, Hamedi Z, Molla A, Mehraeen E, Dadras O. Current ART, determinants for virologic failure and implications for HIV drug resistance: an umbrella review. AIDS Res Ther. 2023;20(1):74. https://doi.org/10.1186/s12981-023-00572-6. PMID: 37884997; PMCID: PMC10604802.
Subramanian A, Mohan A, Kataria S, Krishnan R. Third line antiretroviral treatment in India: Cohort Analysis and Treatment outcomes from a Public Health Facility. AIDS Patient Care STDs. 2021;35(3):69–74.
Mata-Marín JA, Huerta-García G, Domínguez-Hermosillo JC, Chavez-García M, Banda-Lara MI, Nuñez-Rodríguez N, Cruz-Herrera JE, Sandoval-Ramírez JL, Martínez-Abarca I, Villagómez-Ruíz AF, Manjarrez-Tellez B, Gaytán-Martínez J. Effectiveness and risk factors for virological outcome of darunavir-based therapy for treatment-experienced HIV-infected patients. AIDS Res Ther. 2015;12:31. https://doi.org/10.1186/s12981-015-0072-9. PMID: 26413132; PMCID: PMC4582634.
Acknowledgements
We would like to express our sincere gratitude to Yekatit 12 Hospital Medical College, the Department of Internal Medicine, and the School of Public Health for providing us with the invaluable opportunity to conduct this research. Your support has been instrumental in our endeavors.
.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
Authors’ contributionsAAB conceived and designed the study, involved in the proposal development, data analysis, interpretation, and manuscript writing. All other of the authors contributed to data analysis and interpretation, drafting and revising the manuscript. All gave final approval of the final version to be submitted, and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research study obtained ethics approval from the Institutional Review Board (IRB) of Yikatit Medical College ((Protocol No.331/2023). Additionally, the Addis Ababa City Administration’s ethical review board also granted approval prior to the commencement of data collection. The clearance letter was submitted to each study site before the actual data collection for the study. Letter of cooperation was obtained from the Department of Internal Medicine. The information collected was kept anonymous and confidential. The informed consent of the patient to participate in this study was waived by an Institutional Review Board (IRB) of Yikatit Medical College (Protocol No.331/2023).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Berhane, A.A., Chimdesa, H.F., Awedew, A.F. et al. Virologic suppression rate and associated factors for third-line HIV treatment in Addis Ababa, Ethiopia. BMC Infect Dis 24, 1068 (2024). https://doi.org/10.1186/s12879-024-10002-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-10002-1