Abstract
Background
The World Health Organization (WHO) recommends that HIV treatment scale-up is accompanied by a robust assessment of drug resistance emergence and transmission. The WHO HIV Drug Resistance (HIVDR) monitoring and surveillance strategy includes HIVDR testing in adults both initiating and receiving antiretroviral therapy (ART). Due to limited information about HIVDR in Mozambique, we conducted two nationally representative surveys of adults initiating and receiving first-line ART regimes to better inform the HIV program.
Methods
We carried out a cross-sectional study between March 2017 and December 2019. Adults (older than 15 years) living with HIV (PLHIV) initiating ART or receiving first-line ART for between 9-15 months at 25 health facilities across all eleven provinces in Mozambique were included. Genotypic HIVDR was assessed on dried blood spots (DBS) when viral loads were ≥ 1000 copies/ml. Genotypic resistance for non-nucleoside reverse transcriptase inhibitors (NNRTIs), nucleoside reverse transcriptase inhibitors (NRTIs), and protease inhibitors (PIs) was determined using the Stanford HIV database algorithm 9.5 and calibrated population resistance tool 8.1.
Results
Of 828 participants -enrolled, viral load (VL) testing was performed on 408 initiators and 409 ART experienced. Unsuppressed VL was found in 68.1% 419 initiators and 18.8% (77/409) of the ART experienced. Of the 278 initiators and 70 ART experienced who underwent sequencing, 51.7% (144/278) and 75.7% (53/70) were sequenced successfully. Among the new initiators, pretreatment drug resistance (PDR) for NNRTI and PI was found in 16.0% (23/144) and 1.4% (2/144) of the participants, respectively. Acquired drug resistance (ADR) was found in 56.5% (30/53) of the ART-experienced participants of whom 24.5% (13/53) were resistant to both NRTI and NNRTI.
Conclusion
High rates of PDR and ADR for NNRTI and ADR for NRTI were observed in our study. These findings support the replacement of NNRTIs with dolutegravir (DTG) but high levels of NRTI resistance in highly treatment-experienced individuals still require attention when transitioning to new regimens. Moreover, the study underlines the need for routine VL testing and HIVDR surveillance to improve treatment management strategies.
Similar content being viewed by others
Background
According to the 2023 global report by the Joint United Nations Program on HIV/AIDS (UNAIDS), there has been a substantial decrease in the number of new HIV infections by 57% for southern Africa from 1.2 million in 2015 to 660,000 in 2022 [1]. Widespread access to antiretroviral therapy (ART) has significantly contributed to this success, and by 2022, 29.8 million people living with HIV (PLHIV) were on ART worldwide [2]. Mozambique is located in southern Africa and is highly affected by the HIV epidemic; the estimated treatment coverage in 2022 was 82% in adults with 1.8 out of 2.2 million PLHIV on ART [3]. In 2019–2020, Mozambique transitioned to Dolutegravir (DTG)-based ART regimens, as recommended by the World Health Organization (WHO) [4], and currently 99% of adults are receiving DTG-based regimens [3].
Although the benefits of ART are evident, its rapid scale-up comes with challenges that include retention in care, treatment adherence, and -the emergence of viral strains carrying HIV drug resistance (HIVDR) mutations in treatment-experienced individuals and subsequent transmission of such strains [5, 6]. Acquired (ADR) and transmitted drug resistance (TDR) can compromise viral suppression in patients on ART contributing to ongoing transmission and to morbidity and morbidity. A lack of systematic HIVDR surveillance can lead to the use of suboptimal regimens and put the third 95 target (ensuring 95% of patients on ART have suppressed viral load) at risk with a direct impact on the number of new infections [7].
To detect and monitor the emergence and transmission of HIVDR, the WHO developed surveillance strategies for Low- and Middle-Income Countries (LMICs) [8, 9]. One crucial objective of these strategies is to inform HIV prevention and treatment programs and future therapeutic recommendations. Several countries, particularly LMICs, that conducted HIVDR WHO surveys during 2014-2017 observed pretreatment resistance to nevirapine (NVP) and efavirenz (EFV) above the 10% threshold rate [10, 11]. Following this, in 2018, the WHO recommended the use of dolutegravir (DTG) in first and second-line -ART regimens [12]. DTG is more effective, has a higher genetic barrier, and is more tolerable and easier to take (once daily dose) compared to other ARVs [13]. For Mozambique, a study in Maputo and Tete provinces in 2017 also showed levels of NNRTI-PDR above the 10% threshold, [14] which triggered the country’s decision to transition to tenofovir and lamivudine combined with dolutegravir (TLD) in 2019–2020. Currently, regimens based on DTG are the preferred first-line for both children and adults and the preferred second-line for adults, and currently, 99% of adults are on TLD [3]. Following recommendations by the WHO, we conducted two nationally representative surveys for both Pre-Treatment Drug Resistance (PDR) and Acquired Drug Resistance (ADR).
Materials and methods
Study design, population, and enrollment
A cross-sectional survey was conducted in 25 health facilities distributed across all 11 provinces of Mozambique (Supplementary Table 1). The facilities were selected using WHO guidance for sampling ART clinics in countries that combined ADR and PDR surveys [15]. Probability proportional to size (PPS) sampling was used to achieve a nationally representative sample designed to estimate the proportion of adults initiating ART with viral suppression with a precision of +/- 5%. More details about how the desired sample size was computed and how health facilities were selected can be found in Supplementary Information S1. The survey enrolled both ART initiators and ART-experienced adults until a sample size of 16 participants per health facility was achieved for each group, with a total target of 400 participants per group. Patients were considered ART initiators if either ART-naïve or pre-exposed to first-line ART and re-initiating first-line ART after at least 3 months of treatment interruption consistent with the WHO definition [16]. Patients were considered ART-experienced if receiving treatment for 12 months (+/- 3 months) at the time of the survey. Consecutive eligible participants were enrolled between March 2017 and December 2019 until the predetermined sample sizes for both groups had been reached for each health facility.
Demographic and clinical information for each patient was collected using a standardized data collection form. Venous blood samples (5 ml) were collected in ethylene-diamine-tetra-acetic acid (EDTA) tubes and dried blood spot samples (DBS) were prepared following WHO guidance [17]. From each participant, five DBS spots, each containing 75 µl of blood, were prepared. All samples were shipped to the Instituto Nacional de Saúde located in Marracuene, Maputo Province for further laboratory testing.
Ethical considerations
The study protocol was approved by the National Bioethics Committee in Mozambique (reference number 123/CNBS/20) and by the Health Research Ethics Committee of Stellenbosch University (reference number S19/10/198). Written informed consent and demographic information were obtained from all participants before blood collection. For participants with difficulty in signing, a fingerprint on the informed consent form was obtained. Individuals aged 15–17 years were also included since they also received the same ART regimens as adults. As these participants are legally considered minors, their caregivers’ (parents or guardians) permission to participate in the study was obtained along with their assent.
HIV-1 molecular diagnosis and viral load testing
Viral load (VL) testing was performed using one DBS with the COBAS® AmpliPrep/COBAS® TaqMan® HIV-1 Test, v2.0 (Roche Molecular Diagnostics, Branchburg, NJ) kit according to the manufacturer’s instructions. HIV-1 infection was assessed with the COBAS® AmpliPrep/COBAS® TaqMan® HIV-1 Qualitative Test v2.0 [18, 19] kit for all ART initiators with an undetectable VL [18, 19].
RNA extraction, PCR, and genotyping
HIVDR resistance testing was performed on all samples that had a VL result ≥ 1000 copies/mL according to the WHO/HIV ResNet Laboratory Operational Framework [20] and using a previously published protocol for HIV sequencing using DBS [21]. Total nucleic acid (TNA) was extracted from DBS using the Nuclisens EasyMag platform (BioMérieux, Portugal) according to the manufacturer’s instructions [22]. RNA was first reverse transcribed to cDNA and then amplified by a nested PCR using the HIV-1 Genotyping Kit: Amplification Module version 1.0 (Applied Biosystems, Thermo Fisher Scientific, Foster City, CA, USA). The resulting gene product consisted of the protease (codons 6–99) and reverse transcriptase (codons 1–251) regions of the HIV-1 polymerase gene. The amplified product was visualized in 1.0% agarose gel. The sequencing reaction was performed using six primers in the Cycle Sequencing Module of the HIV-1 Genotyping Kit and sequences were generated from 3500XL Genetic Analyzer (Applied Biosystems). Sequences were considered good quality if 90% of the reverse transcriptase and protease regions were successfully sequenced.
Sequence analysis
Sequences were assembled and edited using the sequence analysis tool ReCall (British Columbia Centre for Excellence in HIV/AIDS, Vancouver, Canada) [23]. Drug resistance mutations (DRMs) and drug susceptibility were interpreted using Stanford HIV Drug Resistance Database Version 8 (Stanford University, California, U.S.A.). To estimate the proportion of sequences with any surveillance drug resistance mutation (SDRM) according to the WHO [24] at a population level, the Calibrated Population Resistance (CPR) tool version 8.1 was used [25]. Analysis was according to the 2009 WHO list of mutations The overall population prevalence HIVDR rate was calculated for each class of ARVs in both groups and only mutations that confer high-level resistance as per the 2009 WHO list were used for analysis. HIV-1 subtype was assigned using BioAfrica REGA HIV-1 automated subtyping tool v3.0 [26] and Jumping Profile Hidden Markov Models [27].
Statistical analysis
Descriptive analysis included estimation of medians and interquartile ranges (IQR), and proportions with 95% confidence intervals (CI). Prevalence for DRMs and ARVs susceptibility predictions was calculated by dividing the number of patients with the resistance mutations by the total number of participants sequenced for each group.
Results
Study population characteristics
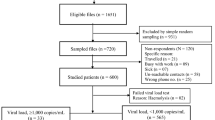
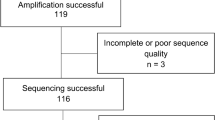
A total of 828 participants were enrolled between March 2017 and December 2019, of whom 419 were ART initiators or re-initiators and 409 were ART-experienced. The majority were females, 58.5% (245/419) among the ART initiators and 62.6% (256/409) among the ART-experienced. The median ages of participants were 36 and 32 years for ART initiators and ART-experienced, respectively. Detailed characteristics of the study population are presented in Table 1. Of the 419 ART initiators enrolled, 11 (2.6%) samples were excluded due to insufficient blood and the remaining 408 underwent VL testing (Figs. 1), Of these, 18.4% (75/408) had an undetectable VL (Target Not Detected, TND), 13.5% (55/408) had VL ≤ 1000 cp/ml, and the remaining 68.1% (278/408) had ≥ 1000 copies/ml. For the participants initiating or re-initiating treatment with undetectable VL (n = 75), HIV molecular diagnosis was performed in 74 samples of whom one had an invalid VL result and 12.2% (n = 9) were HIV-target not detected. Of the ART initiators only 0.7% (3/419) reported previous exposure to ART, with one being exposed to Nevirapine (NVP) for prevention of mother-to-child transmission (PMCT) and the remaining two had been pre-exposed to the first-line ART regimen, TDF + 3TC + EFV (TLE). From the 409 ART-experienced participants that underwent VL testing, 81.2% (332/409) had suppressed viral load according to the 2016 WHO Consolidated guidelines [28] and the remaining 18.8% (77/409) had unsuppressed VL. Of these, seven samples were excluded from sequencing due to insufficient remaining dried blood spots to perform sequencing and the remaining 70 underwent sequencing (17.1%). Samples with successful sequencing rates were found in 51.8% (144/408) among the ART initiators and in 75.7% (53/70) for the ART-experienced.
Study flow chart for both ART initiators and ART-experienced participants from 25 health facility in Mozambique 2017–2019, from enrollment to viral load testing, molecular diagnosis, and HIVDR testing. Abbreviations PDR, pre-treatment drug resistance, ADR, acquired drug resistance; VL, viral load; SDRM, surveillance drug resistance mutation
HIV subtype analysis
HIV subtype determination was based on the pol region sequences (Supplementary Figure S1), with 144 and 53 sequences were generated from ART initiators and ART-experienced patients, respectively. Subtype C was the most frequent subtype with 93.0%(134/144) and 92.4%(49/53). for ART initiators and experienced, respectively Subtype A1 was identified in 6% (9/144) among ART initiators and 2% (1/53) in the ART-experienced group. Mosaic mixture of A1 and D was observed in one participant initiating ART and a mosaic of A1 and C in one ART-experienced participant. Subtypes G and D were only found in ART-experienced participants in 1.9% (1/53) each.
Drug resistance mutations and susceptibility in newly initiating patients
Twenty-five initiators had at least one Surveillance Drug Resistance Mutation (SDRM) representing an overall PDR of 17.4% (95% CI 11–24). NNRTI and PI resistance mutations were observed in 16.0% (23/144) (95% CI 10–22) and 1.4% (2/144) (2, 95% CI 0–3), respectively (Fig. 2a). The most common NNRTI resistance mutations were K1013N (14/144, 9.7%), followed by polymorphic mutation E138A with 6.9% (10/144) and major mutation G190A with 6.2% (9/144) (Fig. 2b). For NRTI resistance mutations, non-thymidine analog mutations (non-TAMs) that prevent NRTI incorporation were detected in our study. M184V which confers high-level resistance to lamivudine (3TC) was the most common non-TAM with 1.3% (2/144). Moreover, thymidine analog mutation (TAMs) D67N with 0.7% (n = 1) and K70Q/E/R with 1.3% (2/144) were also observed. The PI resistance mutations M46L and Q58E, which are known to be associated with reduced susceptibility to atazanavir (ATV) and lopinavir (LPV), were observed in two participants with 0.7% (1/144) . When considering individual drug susceptibility prediction, high-level resistance for Efavirenz (EFV) and NVP was detected in 13.1% (19/144) and 16.6% (24/144) respectively (Fig. 3). There was no intermediate to high-level resistance for tenofovir disoproxil fumarate (TDF) among the new initiators, but 1.3% (2/144) of the participants showed high-level PDR to 3TC. Low proportions below 5% among the initiators showed intermediate to high-level resistance to etravirine (ETR) a second-generation NNRTI and Rilpivirine (RPV) that is used in combination with cabotegravir (CAB) as a long-acting INSTI and NNRTI combination ARV.
Pre-treatment (PDR) and acquired drug resistance (ADR) pproportion of successfully sequenced samples and mutation pattern profiles, 2017–2019, Mozambique. (A) Proportion of sequences among the ART initiators and ART-experienced with any surveillance drugs resistance mutation (SDRMs) to the different classes of ARVs. Prevalence was determined using the calibrated population resistance (CPR) version 8.1,. (B) PDR mutation profile prevalence rate for the different class of ARVs, *major drug resistance mutations, ^TAM, thymidine analogue mutations
Predicted resistance to individual antiretroviral drug among viremic ART initiators and ART-experienced participants, 2017–2019, Mozambique. Resistance is classified as per NNRTI, NRTI, PI scoring algorithms from the Stanford HIV Drug Resistance Database Version 8.8.0. Abbreviations ARV, antiretroviral therapy; NRTI, nucleoside reverse transcriptase inhibitors; NNRTI, non-nucleoside reverse transcriptase; INSTI, integrase strand transfer inhibitor; ABC, abacavir; AZT, azidothymidine (zidovudine); D4T, stavudine; FTC, emtricitabine; 3TC, lamivudine; TDF, tenofovir; DOR, doravirine; EFV, efavirenz; ETR, etravirine; NVP, nevirapine; RPV, rilpivirine; ATV, atazanavir; DRV, Darunavir; LPV, lopinavir; TPV, tipranavir
Drug resistance mutation and susceptibility for the -ART-experienced
Among the ART-experienced participants with viral load ≥ 1000 copies/ml and good quality sequences (n = 53), 30 had at least one SDRM representing an overall prevalence of resistance of 56.6% (30/53) (95% CI 42–70) (Fig. 2a). Mutations that confer resistance for both NRTI and NNRTI were observed in 24.5% (13/53). The most common NNRTI resistance mutation was K103N with 47.2% (n = 25/53), followed by P225H with 7.5% (4/53) and G190A with 5.6% (3/53) (Fig. 2b). All mutations mentioned above (K103N, G190A, P225H) are associated with high-level resistance to EFV and NVP. Polymorphic mutation E138A was also prevalent, with 7.5% (4/53). NRTI resistance mutation M184V which confers high-level resistance to lamivudine (3TC) was the most common in this group with 20.7% (11/53). K65R resistance mutation associated with high-level resistance to TDF and abacavir (ABC) was also found in 9.4% (5/53). Furthermore, low levels of TAMs (D67N and K70Q/E/R) and K219Q/E with 5.6% (3/53) were detected. High-level resistance to EFV and NVP was observed in 56.6% (30/53) (Fig. 3). Intermediate to high-level resistance for 3TC and tenofovir (TDF) was observed in 22.6% (12/53) and 9.4% (5/53) participants, respectively. For the second-generation NNRTIs, intermediate to high-level resistance was observed in 7.7% (6/53) for ETR and in 12.3% (7/53) for RPV.
Discussion
Our study confirms findings from other PDR and ADR surveys conducted in Maputo and Tete [14] provinces of Mozambique and several other studies in Southern and Eastern Africa reporting PDR and ADR to NNRTI that exceeds 10% [29,30,31]. In our study PDR and ADR were primarily driven by the K103N mutation which causes over 20-fold increased resistance to EFV [32] and is slower to revert than other mutations with a viral fitness similar to wild type [33]. Most of the ART initiators in our study were susceptible to TDF and 3TC, and only one participant presented high-level resistance to 3TC. Altogether, these findings support the transition from NNRTI-first line-based regimens to TLD for people initiating treatment. Besides this, DTG is also known to be a very potent ARV, with fewer side effects, more tolerable, and with a higher genetic barrier. In addition, DTG can be used in combination with other nucleoside ARVs as a first-line treatment regimen in a single tablet form used once daily [34, 35].
Thus, among the viremic ART-experienced participants, a relatively high proportion of NRTI resistance mutation M184V/1 above the 10% threshold and K65R close to 10% associated with increased resistance to 3TC and TDF were detected. Both ARVs compromise the recommended TLD regimen backbone. Although mutation M184V/I provides an advantage to the virus in the presence of 3TC, it comes at a fitness cost, which means that the replication capacity of the virus is reduced compared to the wild type [35]. While recent findings show successful treatment outcomes for patients harboring NRTI mutations after transitioning to DTG-based regimens, there are still conflicting data about the real long-term impact of pre-existing NRTI resistance mutations on patients who transitioned to TLD from previous first-line treatment with TLE after the rapid roll-out in LMICS [36,37,38]. As reported before [37], resistance to 3TC and TDF can result in DTG functional monotherapy and subsequent emergence of DTG resistance. Our results highlight the need to closely monitor patients on TLD who have experienced virological failure with previous first-line regimens, such as TLE. Therefore, more research addressing this in LMICs is needed as resistance to NRTI in highly treated patients experiencing virological failure is common in these settings. These results underline the need to better monitor patients with a history of virological failure from previous treatment regimens that have transitioned to TLD.
High PDR levels observed in our study among those initiating treatment suggest that transmission of HIV strains resistant to EFV and NVP has been happening in Mozambique which might have jeopardized previous first-line ART regimen outcomes [39]. The presence of some mutations such as Y181C and E138A among the initiators and ART experienced may in future have an impact on second-generation NNRTIs, such as ETR and long-acting CAB/RPV [40] Such findings emphasize the need for continued surveillance to better inform programs on new treatment strategies such as second-generation NNRTIs, particularly in LMICs.
Even though Mozambique still faces challenges in achieving the UNAIDS 95-95-95 target, the prevalence of viral load suppression (VLS) increased from 81.2% in 2017 from our study and to 88% in 2019 according to the national HIV program of report of Mozambique [3]. Such improvements may be associated with the introduction of TLD in 2019, but HIVDR can still put the third UNAIDS target at risk. Therefore, systematic VL testing, improved ART failure management, and periodic resistance monitoring at a population level are vital in achieving the third target.
Among the new ART initiators, 18.4% had an undetectable VL, of which 12.2% had a subsequent HIV-1 target not detected with a molecular test. The high proportion of undetectable VL tests is surprising given that in the absence of ART, control of viral replication to below 50 copies/ml, known as elite control, is rare albeit possible possibly [41]. Another explanation for this would be undisclosed ART use or misinterpretation of results when two consecutive tests are used [42]. Such false diagnosis can lead people who are not infected being enrolled in ART. This finding underscores the need for ongoing research of such phenomena as well as monitoring of testing procedures and strategies to minimize such errors, particularly in settings with high HIV burden and under-resourced staff where mistakes can easily happen. Moreover, our result also shows the under-reporting of ART use in our study resulting in misclassifying ART-experienced with ART initiators most likely driven by stigma [43], or as a result of integrity issues of DBS samples that might have affected our results.
Study limitations
Our study has several limitations. Limited resources for patient enrollment and data collection hampered the questionnaire data’s quality and accuracy, and it took longer than expected to achieve the desired sample size. As a result, potentially important factors that include social, demographic, and clinical (e.g. number of sex partners, employment status, history of tuberculosis) information that could contribute to a more comprehensive understanding of clinical and demographic factors associated with PDR and ADR at a population level were overlooked because most of the questions in the questionnaires were not addressed at the sites as initially planned. Further, prior exposure to ART was based on verbal reporting and patient file information, which might have resulted in the inadvertent inclusion of undisclosed ART-experienced patients, as evidenced also by the undetectable VL results among some ART initiators. Fourthly, a sequencing success rate below 80% was observed in both the ART initiators and the ART-experienced participants, which can be partially explained by the sample type used. While well-collected and properly stored DBS samples provide similar yields compared to plasma samples, ideal DBS conditions are rarely met in low-resource settings where they have been confirmed to have a lower sequencing success rate compared to plasma [44]. The long delays until sample pick-up from health facilities may also have influenced sample quality. While our sample was designed to be representative of the patient population in Mozambique, we are presenting unweighted results rather than population estimates. Lastly, the low sample size for the ADR being analyzed might have not truly represented the actual resistance.
Conclusions
In summary, we found concerning evidence of pre-treatment NVP and EFV resistance, which supports the transition from an NNRTI-based regimen to DTG in Mozambique. However, high-level acquired NRTI resistance suggests a need for urgent attention for patients with previously confirmed virological failure when transitioning to DTG since the risk of failure is higher. To safeguard current treatment options in Mozambique, rigorous VL monitoring and periodic HIVDR surveillance in both ART initiators and ART-experienced patient populations is vital to fill in programmatic gaps and design public health strategies. These gaps can promote the emergence of HIVDR which can hinder the efficacy of future ART regimens and compromise current UNAIDS targets.
Data availability
All the data generated or analyzed during this study are included in this published article sequences are available in GenBank with accession numbers: PP511921- PP511973, PP512312- PP512455.
References
The path that ends AIDS: UNAIDS Global AIDS Update. 2023. Geneva: Joint United Nations Program (cited on 18 March 2024). https://thepath.unaids.org/wp-content/themes/unaids2023/assets/files/2023_report.pdf.
Global HIVstatistics. 2023 Fact Sheet (cited on 18 March 2024). https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf.
MISAU PNC ITS HIV/SIDA Relatórios Anuais. (cited on 18. March 2024). http://www.misau.gov.mz/index.php/relatorios-anuais.
The World Health. Organization warns of increasing HIV drug resistance and issues new guidelines to address threat. Pharm J. 2017.
Caro-Vega Y, Alarid-Escudero F, Enns EA, Sosa-Rubí S, Chivardi C, Piñeirúa-Menendez A et al. Retention in Care, Mortality, loss-to-Follow-Up, and viral suppression among antiretroviral Treatment-Naïve and experienced persons participating in a nationally Representative HIV Pre-treatment Drug Resistance Survey in Mexico. Pathogens. 2021;10(12).
Ortblad KF, Baeten JM, Cherutich P, Wamicwe JN, Wasserheit JN. The arc of HIV epidemics in sub-saharan Africa: new challenges with concentrating epidemics in the era of 90-90-90. Curr Opin HIV AIDS. 2019;14(5):354–65.
Collier DA, Monit C, Gupta RK. The impact of HIV-1 drug escape on the Global Treatment Landscape. Cell Host Microbe. 2019;26(1):48–60.
World Health Organization. (2016). HIV drug resistance surveillance guidance, 2015 update. (cited on 18 March 2024). https://iris.who.int/handle/10665/204471.
World Health Organization. (2017). Guidance for sampling ART clinics in countries combining surveillance of pre-treatment HIV drug resistance and acquired HIV drug resistance at 12 and 48 + months. World Health Organization. https://iris.who.int/handle/10665/259740.
World Health Organization. 2017. Global action plan on HIV drug resistance 2017–2021. (cited on 18 March 2024). https://www.who.int/publications/i/item/978-92-4-151284-8.
HIV drug resistance report 2021. (cited. 3rd November 2023). https://www.who.int/publications/i/item/9789240038608.
World Health Organization. Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach. World Health Organization. editor. Geneva: World Health Organization; 2021. (cited 18 March 2024. https://www.who.int/publications/i/item/9789240031593.
Dow DE, Bartlett JA. Dolutegravir, the second-generation of integrase strand transfer inhibitors (INSTIs) for the treatment of HIV. Infect Dis Ther. 2014;3(2):83–102.
Carnimeo V, Pulido Tarquino IA, Fuentes S, Vaz D, Molfino L, Tamayo Antabak N, et al. High level of HIV drug resistance informs dolutegravir roll-out and optimized NRTI backbone strategy in Mozambique. JAC Antimicrob Resist. 2021;3(2):dlab050.
World Health Organization. 2017.Guidance For Sampling ART Clinics In Countries Combining Surveillance Of Pre-Treatment HIV Drug Resistance And Acquired HIVDrug Resistance At 12 And 48 + Months. (cited 18 of March 2024). https://iris.who.int/bitstream/handle/10665/259740/WHO-HIV-2017.38-eng.pdf.
Surveillance of HIV drug. Resistance in adults initiating antiretroviral therapy - pre-treatment HIV drug resistance (cited 15 August 2023). https://www.who.int/publications/i/item/9789241507196.
Guidelines for Using HIV Testing Technologies in Surveillance. Selection, evaluation and implementation: 2009 update. Geneva: World Health Organization; 2009.
COBAS® AmpliPrep/COBAS®. TaqMan® HIV-1 Test, v2.0. (cited 10 August 2023). https://diagnostics.roche.com/global/en/products/params/cobas-ampliprep-cobas-taqman-hiv-1-test-v2-0.html.
COBAS® AmpliPrep/COBAS® TaqMan® HIV-1 Qualitative Test. (cited 10. August 2023).https://diagnostics.roche.com/global/en/products/params/cobas-ampliprep-cobas-taqman-hiv-1-qualitative-test-v2-0.html.
World Health Organization. 2020. WHO HIVResNet HIV drug resistance laboratory operational framework, second edition. (cited 18 of March 2024). https://iris.who.int/bitstream/handle/10665/336169/9789240009875-eng.pdf?sequence=1.
Yang C, McNulty A, Diallo K, Zhang J, Titanji B, Kassim S, et al. Development and application of a broadly sensitive dried-blood-spot-based genotyping assay for global surveillance of HIV-1 drug resistance. J Clin Microbiol. 2010;48(9):3158–64.
NUCLISENS® EASYMAG® | bioMérieux South Africa. (cited 10 August 2034). https://www.biomerieux.co.za/product/nuclisensr-easymagr.
Woods CK, Brumme CJ, Liu TF, Chui CKS, Chu AL, Wynhoven B, et al. Automating HIV drug resistance genotyping with RECall, a freely accessible sequence analysis tool. J Clin Microbiol. 2012;50(6):1936–42.
HIV Drug Resistance Database. (cited 21. June 2024). https://hivdb.stanford.edu/page/who-sdrm-list/.
Gifford RJ, Liu TF, Rhee S-Y, Kiuchi M, Hue S, Pillay D, et al. The calibrated population resistance tool: standardized genotypic estimation of transmitted HIV-1 drug resistance. Bioinformatics. 2009;25(9):1197–8.
Pineda-Peña A-C, Faria NR, Imbrechts S, Libin P, Abecasis AB, Deforche K, et al. Automated subtyping of HIV-1 genetic sequences for clinical and surveillance purposes: performance evaluation of the new REGA version 3 and seven other tools. Infect Genet Evol. 2013;19:337–48.
Schultz A-K, Zhang M, Bulla I, Leitner T, Korber B, Morgenstern B et al. jpHMM: improving the reliability of recombination prediction in HIV-1. Nucleic Acids Res. 2009;37(Web Server issue):W647–51.
WHO. 2016: Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations – 2016 update. (cited 16 April 2023). https://www.who.int/publications/i/item/9789241511124.
Bacheler L, Jeffrey S, Hanna G, D’Aquila R, Wallace L, Logue K, et al. Genotypic correlates of phenotypic resistance to efavirenz in virus isolates from patients failing nonnucleoside reverse transcriptase inhibitor therapy. J Virol. 2001;75(11):4999–5008.
Wertheim JO, Oster AM, Johnson JA, Switzer WM, Saduvala N, Hernandez AL, et al. Transmission fitness of drug-resistant HIV revealed in a surveillance system transmission network. Virus Evol. 2017;3(1):vex008.
Bangalee A, Hanley S, Bangalee V. Medicine and the law. S Afr Med J. 2022;112(10):787–90.
Wainberg MA. The impact of the M184V substitution on drug resistance and viral fitness. Expert Rev Anti Infect Ther. 2004;2(1):147–51.
Naeger LK, Harrington P, Komatsu T, Deming D. Effect of dolutegravir functional monotherapy on HIV-1 virological response in integrase strand transfer inhibitor resistant patients. Antivir Ther (Lond). 2016;21(6):481–8.
Rolle C-P, Nguyen V, Hinestrosa F, DeJesus E. Virologic outcomes of switching to dolutegravir functional mono- or dual therapy with a non-cytosine nucleoside analog: a retrospective study of treatment-experienced, patients living with HIV. AIDS Res Ther. 2021;18(1):26.
Paton NI, Musaazi J, Kityo C, Walimbwa S, Hoppe A, Balyegisawa A, et al. Efficacy and safety of dolutegravir or darunavir in combination with lamivudine plus either zidovudine or tenofovir for second-line treatment of HIV infection (NADIA): week 96 results from a prospective, multicentre, open-label, factorial, randomised, non-inferiority trial. Lancet HIV. 2022;9(6):e381–93.
Hamers RL, Schuurman R, Sigaloff KCE, Wallis CL, Kityo C, Siwale M, et al. Effect of pretreatment HIV-1 drug resistance on immunological, virological, and drug-resistance outcomes of first-line antiretroviral treatment in sub-saharan Africa: a multicentre cohort study. Lancet Infect Dis. 2012;12(4):307–17.
Steegen K, Chandiwana N, Sokhela S, Venter WDF, Hans L. Impact of rilpivirine cross-resistance on long-acting cabotegravir-rilpivirine in low and middle-income countries. AIDS. 2023;37(6):1009–11.
Walker BD. Elite control of HIV infection: implications for vaccines and treatment. Top HIV Med. 2007;15(4):134–6.
Gupta RK, Gregson J, Parkin N, Haile-Selassie H, Tanuri A, Andrade Forero L, et al. HIV-1 drug resistance before initiation or re-initiation of first-line antiretroviral therapy in low-income and middle-income countries: a systematic review and meta-regression analysis. Lancet Infect Dis. 2018;18(3):346–55.
Riou J, Dupont C, Bertagnolio S, Gupta RK, Kouyos RD, Egger M, et al. Drivers of HIV-1 drug resistance to non-nucleoside reverse-transcriptase inhibitors (NNRTIs) in nine southern African countries: a modelling study. BMC Infect Dis. 2021;21(1):1042.
Ntamatungiro AJ, Kagura J, Weisser M, Francis JM. Pre-treatment HIV-1 drug resistance in antiretroviral therapy-naive adults in Eastern Africa: a systematic review and meta-analysis. J Antimicrob Chemother. 2022;77(12):3231–41.
Fogel JM, Wang L, Parsons TL, Ou S-S, Piwowar-Manning E, Chen Y, et al. Undisclosed antiretroviral drug use in a multinational clinical trial (HIV Prevention trials Network 052). J Infect Dis. 2013;208(10):1624–8.
Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(3 Suppl 2):18640.
Omooja J, Bbosa N, Lule DB, Nannyonjo M, Lunkuse S, Nassolo F, et al. HIV-1 drug resistance genotyping success rates and correlates of dried-blood spots and plasma specimen genotyping failure in a resource-limited setting. BMC Infect Dis. 2022;22(1):474.
Acknowledgements
We would like to thank all staff of the health facilities and the study participants who provided support to implement the study. In addition, we acknowledge the HIV sequencing laboratory staff of the Instituto Nacional de Saúde in Mozambique for testing the samples.
Funding
This publication has been supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC) the terms of GH000080 and GH002021. Furthermore, the work was also supported by the Bill and Melinda Gates Foundation (BMFG) (Grant number OPP1148264) and the US National Institute of Health (NIH/Fogarty International Center (FIC) grant titles: Pitt-Mozambique Training Program (Pitt-MozHRTP) in COVID-19, cardiovascular disease, and Diabetes in People with HIV (D43TW011827). The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the funding agencies.
Author information
Authors and Affiliations
Contributions
Conceptualization of the study, A.V, N.I, NM, J.dS, P.M, E.R, N.W, A.R, I.M, and H.G; funding acquisition, E.R, A.R, A.V, D.B and N.M; sample, data collection and testing, N.I, I.M, H.G, A.V, P.M and N.M. Data analysis, cleaning and curation N.I, H.G and I.M; research administration and resources, A.V, N.M, N.I and I.M; writing of the original draft N.I, O.L, C.M, I.M, M.H and H.G, writing, reviewing, and editing A.V, W.P, T.O, J.dS, E.R, D.B, A.R, N.M, P.M, C.B, L.M.H and E.W.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ismael, N., Gemusse, H., Mahumane, I. et al. HIV-1 pretreatment and acquired antiretroviral drug resistance before tenofovir/ lamivudine /dolutegravir (TLD) roll-out in Mozambique. BMC Infect Dis 24, 748 (2024). https://doi.org/10.1186/s12879-024-09579-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09579-4