Abstract
Background
Late human immunodeficiency virus (HIV) diagnosis is the most prominent cause of HIV/AIDS-related mortality and also increases the risk of transmission and spread of the disease in society. Adolescents are the most vulnerable population’s age group for HIV infection in several settings, but expanding access to early HIV testing remains a challenge. Consequently, a significant proportion of adolescents are still dying of HIV-related causes, and the current study aimed at assessing the effect of late presentation on HIV-related mortality among adolescents living with HIV.
Methods
An institutional-based retrospective cohort study was conducted from August 21–November 21, 2022, at selected public hospitals in the North Showa Zone of Oromiya, Ethiopia. All adolescents living with HIV who had received no ART and presented for ART follow-up at public hospitals from September 1, 2012, to August 31, 2021, were included in the study. Data entry was done by Epi-data version 3.1.1 software and exported to Stata version 16 for further analysis. Both bi-variable and multivariable analyses were performed using the Cox proportional hazard model to compare the HIV-related mortality of early and late-presented adolescents using an adjusted hazard ratio at a 95% confidence interval (CI).
Results
A total of 341 medical records of adolescents were included in the study, contributing an overall incidence rate of 3.15 (95% CI: 2.21–4.26) deaths per 100 person-years of observation throughout the total follow-up period of 1173.98 person-years. Adolescents with late presentation for HIV care had three times the higher hazard of mortality (adjusted hazard ratio (aHR) = 3.00; 95% CI: 1.22–7.37) as compared to those with early presentation for HIV/AIDS care. Adolescents within the age range of 15–19 years old (aHR = 3.56; 95% CI: 1.44–8.77), rural residence (aHR = 2.81; 95% CI: 1.39–5.68), poor adherence to ART (aHR = 3.17; 95% CI: 1.49–6.76), and being anemic (aHR = 3.09; 95% CI: 1.52–6.29) were other independent predictors of HIV-related mortality.
Conclusion
The study found a substantial link between HIV late presentation to care and mortality among adolescents. Residence, age, antiretroviral therapy (ART) medication adherence, and anemia status were also found to be other independent predictors of HIV-related mortality. To achieve the ultimate aim of lowering mortality among adolescents living with HIV, rigorous emphasis must be placed on early presentation for HIV/AIDS care. In addition, counseling on adherence and prompt diagnosis and treatment of anemia are highly recommended to reduce mortality.
Similar content being viewed by others
Background
The human immunodeficiency virus (HIV) continues to be a major global health problem, and millions of people have died since it was originally discovered and isolated forty years ago. Worldwide, there were around 1.5 million new infections and 680,000 deaths from acquired immunodeficiency syndrome (AIDS) related causes in 2020 [1]. Adolescents (10 to 19 years of age) were the most severely affected age group by the epidemic, and they made up an increasing share of new HIV infections, accounting for about 5% of all people living with HIV and about 11% of new HIV infections among adults. Globally, in 2020, about 150,000 adolescents were newly infected and 32,000 died [2, 3]. HIV/AIDS is the second cause of mortality in adolescents worldwide, and the first in Africa [4, 5].
Late presentation to HIV care adversely affects the prognosis of AIDS by reducing the effectiveness of antiretroviral therapy (ART). It also increases the chance of transmission and spread of the disease, thereby increasing the risk of morbidity and mortality among the patients [6,7,8]. Studies revealed that some HIV-positive adolescents may die within the first year after starting [9, 10], and one of the prominent contributors to those deaths could be late presentation to HIV/AIDS care [11, 12]. In addition, adolescents are one of the unique age groups for whom HIV late presentation to care has a major impact on the outcome of the disease [13,14,15].
Despite the widespread availability of tests, expanding adolescent access to HIV testing (targeted and tailored testing strategies) continues to be a challenge, including index-linked testing, assisted partner notification, social network-based testing, and other novel modalities that boost the efficiency of testing programs [2]. As a result, adolescents become the age group most likely to be unaware of their diagnosis [16]. Some other unique contributing factors, like age of consent laws and low parent-adolescent communication about HIV/AIDS-related issues, can be barriers to adolescents accessing relevant HIV/AIDS services, resulting in late presentation to care and early mortality [17, 18].
In 2003, the Ethiopian government introduced its ART program and began implementing prevention, treatment, and care interventions to reduce HIV-related morbidity and mortality, improve the quality of life of patients living with HIV (PLWH), and mitigates some of the epidemic’s impacts. Also, drug and testing services are becoming more widely available in basic health care institutions and via campaign programs [19]. Even though in most developing countries like Ethiopia, where HIV testing and ART services are free, most adolescents present late for HIV/AIDS care and follow-up [13, 15]. The presence of some unique biological, physical, and social factors makes adolescents a more vulnerable age group in the population [16,17,18], and HIV-related deaths continue to be recorded in high numbers [7, 20]. Thus, designing and implementing high-impact, evidence-based interventions are necessary to reduce HIV-related mortality among adolescents. Therefore, this study aimed at determining the effect of HIV late presentation to care and other possible predictors on HIV-related mortality among adolescents attending ART clinics in public hospitals.
Methods
Study design and areas
A hospital-based retrospective cohort study was conducted from August 21–October 21, 2022, in selected public hospitals in the North Showa Zone of Oromiya region, Ethiopia. North Showa Zone has a total population of 1.6 million, with the capital city of Fitche located 114 km to the north of Addis Ababa. It is divided into 13 rural districts and two town administrations. There are 64 health centers and five public hospitals in the North Showa community that provide health care services. The study was carried out in three selected public hospitals, namely Salale University Comprehensive Specialized Hospital (SUCSH), Kuyu General Hospital, and Gundo-Meskel Primary Hospital.
Study population and sampling
The source populations were all adolescents living with HIV who had received no ART and presented for ART follow-up at public hospitals in the North Showa Zone of Oromiya, Ethiopia. Adolescents who presented for ART follow-up from September 1, 2012, to August 31, 2021, at the three selected public hospitals were considered the study population and included in the study.
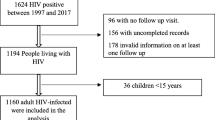
A standardized table of lists was prepared to extract eligible patients’ medical record numbers (MRNs) from the electronic databases of each health facility. The study included all patient charts that met the eligibility criteria. Patients’ charts that didn’t have full formal record information or had incomplete medical records for essential variables such as treatment outcome, age, and cluster of differentiation 4 (CD4) results, as well as those who didn’t have at least one documented clinic visit, were excluded from the study.
Study variables
The study’s outcome variable was HIV/AIDS-related mortality. The primary exposure variable was the time of presentation to HIV care, which was categorized as early presentation versus late presentation for HIV care. Exposed patients are those with HIV late presentation to care (who present with a CD4 count below 350 cells/mm3), whereas non-exposed patients are those with early presentation for HIV/AIDS care (who present with a CD4 count ≥ 350 cells/mm3).
Other independent variables
Socio-demographic variables such as age, sex, level of education and residence, past medical history of any opportunistic infections (OI) and clinical factors such as weight or body mass index (BMI), functional status, world health organization (WHO) clinical staging, and hemoglobin level.
Data collection procedures and quality assurance
A data collection checklist was used to extract data from the patients’ charts. The tool was developed based on routine data registration protocols using standardized HIV care and follow-up forms (HIV/AIDS care monitoring and evaluation sheet) employed by ART clinics in health facilities in Ethiopia. Laboratory requests and ART intake forms were considered as a source of data and incorporated in the study. In each of the three selected hospitals, two data collectors were appointed to extract data from patients’ records, and another senior nurse supervised the data collection process. The patient’s chart was picked up from the chart room using MRN, and then data was extracted from the patient’s medical charts by using the prepared tool. During data collection, information that was not available on medical records was checked on smart care and other related registrations.
At Fiche number one health center, pre-testing was done with 5% of the total sample size. Based on the results of the pre-test, the check list was amended and modified. Training was given for the data collectors and supervisors on the entire data collection process. The supervisors checked the collected data on a daily basis for completeness and consistency.
Data management and analysis procedures
Data entry was done by Epi-data version 3.1.1 software (Odense, Denmark) and then exported to Stata version 16 software for analysis. Prior to analysis, the data was cleaned for completeness using frequency and cross-tabulation. Recoding, categorization, and sorting of data were done using Stata software. Person-Month of follow-up was calculated by subtracting the date of HIV-related death (the last date of follow-up for censoring) from the date of HIV confirmation of patients.
During the analysis, descriptive statistics like frequency distribution, ratio, means, median, percentages, inter-quartile range (IQR), and standard deviation were calculated. Survival curves were used to further illustrate differences in hazard rations (HR), and with the Kaplan-Meier method, the survival probabilities of the exposed and unexposed groups were compared and interpreted accordingly. The log rank test was used to determine if the survival probabilities in the exposed and unexposed groups were significantly different. Both bivariable and multivariable Cox proportional hazard regression models were used to verify the effect of late presentation on HIV-related death of patients and other independent predictors of mortality, with an HR of 95% CI at 5% level of significance (α). Only variables with a P-value < 0.25 in the bivariable analysis were entered into the final model. The assumptions like proportionality of hazards over time, normality, and multi-collinearity were checked. The P-value of the proportionality of hazards over time in global test, using Schoenfeld residuals, was 0.914. Variables that were significant (P-value < 0.05) in the multivariable analysis were considered independent predictors of HIV-related mortality. Finally, the result was presented using texts, tables, figures, and diagrams.
Operational definitions
Late presentation for HIV/AIDS care
defined as the enrollment of individuals for HIV/AIDS care with a CD4 count below 350 cells/mm3 [21].
Early presentation for HIV/AIDS care
defined as the enrollment of individuals for HIV/AIDS care with a CD4 count ≥ 350 cells/mm3.
HIV/AIDS related death or mortality
Defined as any recorded AIDS-related deaths other than deaths due to accidents like car accident, bullet injury, and any suicidal act while a patient is on ART and occurred in hospitals and any setting confirmed by the hospitals [22].
Censored patients
are those who had some information about individual survival time, but the exact time of presence of the outcome variable is unknown [23]. These individuals didn’t provide us the information whether HIV/AIDS related mortality had occurred or not. Adolescents who were alive beyond the end of follow-up period (August 31, 2021), lost/ drop from follow up, transferred out to other facilities, and if the cause of death was not HIV/AIDS related (accidental), considered as censored patients.
Functional status of patients
Classified according to the WHO criteria as working (W): capably to perform usual work in or out of the house, harvest, go to school or, for children, normal activities or playing; Ambulatory (A): capable to perform activities of daily living like self-care and going to the toilet unsupported; Bed-ridden (B): cannot perform activities of daily living like unable to go even to the toilet unsupported [24].
Anemia
In this study anemia is defined as anemic or not-anemic based on WHO criteria: i.e. Hemoglobin concentration < 12 g/dl for females and < 13 g/dl for males [25].
Nutritional status
Determined by the computed BMI and it shall be compared against a BMI- for- Age reference chart (BMI-for-Age Z-score), to decide whether the computed BMI indicates malnutrition or not; severely malnourished (< -3 SD), moderately malnourished (-2 to -3 SD), mildly malnourished (-1 to -2 SD) and normal weight (> -1 SD) [26].
Results
Socio-demographic characteristics of cohorts
The descriptive statistics extracted from the ART clinics of the three selected public hospitals revealed that the total number of adolescents on the ART cohort for the 10 years follow-up were 341 adolescents. After reviewing 341 medical records, 32 were excluded due to incompleteness, and 309 were included in the final analysis. The median age of participants was 17 years (IQR, 14–19 years); more than two-thirds, 220 (71.2%), of them were between 15 and 19 years of age. More than half, 181 (58.58%), of adolescents were females, and more than three-quarters, 209 (67.64%), lived in urban environments. Regarding participants’ occupations, 209 (67.64%) were students, and two-thirds, 186 (60.19%), were primary school students (Table 1).
Baseline clinical, laboratory and ART information
Regarding the baseline clinical and laboratory characteristics of adolescents living with HIV, 164 (53.07%) of them were late presented to HIV/AIDS care, and 145 (46.93%) were presented earlier. Most adolescents, 145 (46.93%), started ART after a week of being confirmed positive for HIV infection; 34 (11%) started within a week; and 130 (42.07%) started on the same day of confirmation.
At the time of enrollment, ALHIV had a median hemoglobin level of 12.9 mg/dl (IQR, 11.9–13.5 mg/dl); two-fifths, 124 (40.13%), were anemic. One hundred thirty-four (43.37%) adolescents were malnourished, and about 127 (41.1%) were given nutritional supplements at enrollment. Nearly half, 147 (47.57%), were categorized as having working functions, and about 6 (1.94%) adolescents were presented with edema. Regarding the patient’s tuberculosis (TB) co-infection status, 63 (20.39%) had a past TB treatment history, and nearly half of ALHIV, 150 (48.54%), had at least one OI (Table 2).
More than half of the study participants, 161 (52.1%), were stage III or stage IV by WHO clinical staging. During the enrollment period, there were only 26 (8.41%) pregnant adolescents, and none of the others had received family planning services. More than four-fifths, 271 (87.7%), had good adherence levels for the ART drug in the first three months of follow-up, and more than two-thirds of adolescents, 204 (66.02%), were taking the 1e (tenofovir disoproxil fumarate” + lamivudine + efavirenz) ART drug regimen at the time of enrollment. Throughout the 10-year follow-up period, 37 (11.97%) adolescents were found to have died of direct HIV-related causes (Table 2).
Incidence of HIV/AIDS-related mortality
From a total of 309 adolescents, two-thirds, 190 (61.49%), were active (alive on ART) at the end of the follow-up period, and 44 (14.24%) of them were transferred out to other health facilities. Throughout the 10-year follow-up period, about 25 (8.09%) adolescents were dropped from follow-up and 11 (3.56%) were lost. There were 2 (0.65%) participants who died due to other conditions. Out of the total 37 (11.97%) deaths directly related to HIV/AIDS causes, 31 (10.03%) adolescents died from late presentation to HIV/AIDS care, and 6 (1.94%) died from early presented to HIV/AIDS care.
The Kaplan–Meier survival plot from this study showed that the curve for unexposed group was consistently higher than that of exposed group. This indicated that early presented to HIV/AIDS care had a higher survival probability than those with lately presented throughout the ten years follow-up period. Moreover, as the number of years increases, the two curves appeared to get farther apart, suggesting that the beneficial effects of early presence to HIV/AIDS care over late presence are greater the longer one stays alive (Fig. 1). Survival of HIV patients within the ten years retrospective follow-up using Kaplan–Meier (the log rank) test for equality of survival function showed that there is a statistically significant difference between lately presented and early presented (P-value = 0.0001). The cumulative probability of surviving or being free from the event of interest at the end of 1, 4, 6 and 10 years was 94.4%, 86.6%, 84.7% and 83.2%, respectively.
The study participants contributed an overall 1173.98 person-years of follow-up. The person-year incidence of death was 1.08 per 100 adolescents-years in the unexposed group and 4.99 per 100 adolescents-years in the exposed group, with an overall incidence rate of 3.15 (95% CI: 2.21–4.26) per 100 adolescents-years. The attributable risk, which is the risk that is attributable only to the exposure group among the selected adolescents, is 3.92 per 100 adolescents-years of observation.
Predictors of HIV-related mortality
Since there were multiple exposure variables, Hosmer and Lemeshow criteria for model development were utilized to find possible predictors of HIV-related mortality among adolescents. As a result, HIV late presentation to care in adolescents had a significantly higher hazard of HIV-related mortality with adjusted hazard ratio (aHR) = 3.00, 95% confidence interval (CI) 1.22–7.37, than early presentation to HIV/AIDS care (Table 3).
Adolescents within the age range of 15–19 years old had more than 3.5 times the higher hazard of death as compared to those within 10–14 years old (aHR = 3.56; 95% CI: 1.44–8.77). Rural residences had more than 2.8 times the higher hazard of mortality as compared to patients with urban residences (aHR = 2.81; 95% CI: 1.39–5.68). Patients with poor medication adherence had more than three times the higher hazard of death as compared to adolescents with good or fair adherence (aHR = 3.17; 95% CI: 1.49–6.76). ALHIV with a low baseline laboratory hemoglobin result (anemic) had a three times higher hazard of death as compared to adolescents with a normal baseline hemoglobin (non-anemic) status (aHR = 3.09; 95% CI: 1.52–6.29) (Table 3). Even though the baseline WHO clinical stage had significant statistics in the crude analysis, it was not included in the final model because it demonstrated collinearity with the main exposure variable (baseline CD4 cell count).
Discussion
This research, using a multi-facility retrospective follow-up approach, is intended to investigate the influence of late presentation on HIV-related mortality among adolescents living with HIV in the selected public hospitals of North Showa Zone. The study found a significant association between late HIV presentation to care and mortality among ALHIV. It also indicated that place of residence; age, medication adherence, and anemia status were independent predictors of HIV-related death among ALHIV.
The overall incidence rate among ALHIV receiving ART was 3.15 per 100 person-years, with a total follow-up time of 1173.98 adolescent years. In this study, the mortality rate for ALHIV was lower than the rate identified in previous single-country studies, such as in India (4.9 deaths per 100 person-years) [27] and Zimbabwe (5.46 deaths per 100 person-years) [28]. The disparity may be attributed to variations in clinical features of research participants, as well as differences in study periods and different adolescents’ ages between studies (including children under the age of nine in their samples). However, the overall mortality rate in this study was higher than the rate reported by a global cohort collaboration across seven regions, with 0.97 deaths per 100 person-years [13]; in Ethiopia’s Amhara region, 1.52 deaths per 100 person-years [29]; and in another study done in Addis Ababa and the southern nations’, nationalities’, and peoples’ region (SNNPR), Ethiopia, 2.29 deaths per 100 person-years [19]. The difference in mortality rates between our study and previous studies, as well as the variation in mortality rates between these studies, could be attributed to sample sizes, categorizing ALHIV with an age of less than 15 years as an age proxy for perinatally acquired infection, and study settings, as this study included only hospitals.
Individuals with HIV late presentation to care had a three-fold higher hazard of death compared to adolescents with early presentation. Low CD4 counts at baseline were linked with an increased risk of death within one year after starting ART, and 16 adolescents died during the first year of follow-up. This is in line with the results of a worldwide cohort of collaborative research including adolescents living with HIV in Asia Pacific, the Caribbean, Central and South America, and Sub-Saharan Africa, which found that adolescents with low CD4 were more likely to die within a year of diagnosis [13]. Similar results were seen in numerous other studies from Haiti [30], Thailand [16], and Tanzania [9] which confirmed the present study’s conclusion that baseline CD4 cell count is a strong laboratory predictor of HIV-related mortality. In fact, CD4 cell count at ART initiation is the most significant predictor of disease development and dictates opportunistic infection (OI) risk categorization. It is also a direct indicator of a patient’s immunological state [8]. It is well known that a low CD4 count is a critical threshold for increased risk of death and is used similarly to the current WHO definition of advanced HIV disease [8]. In order to properly treat HIV/AIDS, infection should be detected as soon as feasible; when the person’s CD4 cell count exceeds 350 cells/mm3 [31]. This study’s findings also reinforce the previously stated fact by identifying HIV late presentation to care as a predictor of HIV-related mortality among ALHIV.
In this research, baseline blood hemoglobin levels were also a predictor of survival among HIV-positive adolescents. This conclusion was consistent with previous research from India and Ethiopia’s two regions, Addis Ababa and the SNNPR, which found that ALHIV with low baseline hemoglobin levels (clinically anemic) were more likely to die of HIV/AIDS than their counterparts [14, 27]. This could be explained by the fact that anemia at the baseline could be the result of HIV disease, particularly at an advanced stage, and it could also be a result of co-infection. Thus, HIV-infected patients with common hematologic complications have a higher mortality risk because anemic HIV-positive individuals take longer to recover from their disease or become completely unable to recover from their illness while on ARV drugs. Eventually, the illness’s horrible relationship with a significantly quicker rate of disease progression, poorer quality of life, and a strong prognostic marker for death [32, 33].
According to other studies, poor ART adherence in the first three months of enrollment may also contribute to adolescent mortality [29]. This might be explained by the fact that patients who do not comply with their therapy are in danger of developing medication resistance and, ultimately, treatment failure, which can lead to death if not caught early, since adherence is essential for suppressing viral replication and improving treatment success [34]. The importance of ART adherence in reducing ALHIV mortality and illness is a consistent finding [35].
Adolescents living in rural areas had a higher risk of death than urban patients and were found to be a significant predictor of HIV-related mortality. In keeping with current findings, several other studies have shown that rural residency is a demographic predictor of HIV survival in adolescents [15, 36]. The explanation for this similarity is that the research sites and study regions are comparable in resource-limited situations, where people living in rural areas have difficulty accessing health care information and services. In resource-limited settings, poor retention of adolescents throughout the HIV care cascade is also [30]. Being from a rural area may also be an indirect indication of poorer care quality in distant parts of the country [14].
In line with research undertaken in Sub-Saharan Africa (SSA) [37] this study found that being an older adolescent (15–19 years old) increased the risk of HIV/AIDS-related mortality when compared to younger adolescents (10–14 years old). The disparity in mortality rates between age groups may be due to evidence of differences in service delivery by age group; children under the age of 15 were more likely to enroll in designated pediatric care clinics, whereas youth over the age of 15 would have been enrolled and followed in the adult care clinic. It is probable that pediatric programs were better able to retain patients than adult programs [38, 39]. Furthermore, dealing with the potential of lifetime therapy is intimidating for older adolescents due to their typical maturation problems—emotionally, mentally, physically, and sexually [40].
The main limitation of this study is that, due to the retrospective nature of the research’s design, there were some missing data, some details of the patients’ clinical condition were underestimated, and there were incomplete records of variables or charts. Furthermore, the study’s small sample size may impair the precision of the results. Moreover, the study did not measure health-care quality, which may have an impact on HIV-related deaths.
Conclusion
The study found a substantial link between HIV late presentation to care and mortality among adolescents living with HIV. HIV late presentation to care has increased mortality; hence, detecting HIV-infected adolescents as early as feasible might be one of the absolute answers to controlling death from HIV/AIDS. Rural residence, the age group of 15–19 years, poor medication adherence, and a low baseline hemoglobin level were also independent predictors of HIV-related death among ALHIV. To achieve the ultimate goal of lowering mortality among ALHIV, rigorous emphasis must be placed on ALHIV with poor baseline clinical and laboratory results, since their illness progression is faster and leads to death early. The study’s findings also highlight additional dimensions that future researchers should consider in large-scale prospective study designs.
Data availability
A supporting document (research ethics approval letter), that could be considered in the review and assessment of our manuscript, is provided within the related information file.
Abbreviations
- 1c:
-
Zidovudine + Lamivudine + Nevirapine
- 4c:
-
Zidovudine + Lamivudine + Nevirapine
- 1e:
-
Tenofovir Disoproxil Fumarate + Lamivudine + Efavirenz
- 1j:
-
Tenofovir Disoproxil Fumarate + Lamivudine + Dolutegravir
- AIDS:
-
Acquired immunodeficiency syndrome
- aHR:
-
Adjusted Hazard Ratio
- ALHIV:
-
Adolescents Living with Human Immunodeficiency Virus
- ART:
-
Antiretroviral Therapy
- BMI:
-
Body Mass Index
- CD4:
-
Cluster of Differentiation 4
- cHR:
-
Crude Hazard Ratio
- CPT:
-
Cotrimoxazole preventive therapy
- Hgb:
-
Hemoglobin
- HIV:
-
Human Immunodeficiency Virus
- HR:
-
Hazard Ratio
- INH:
-
Isoniazid
- IQR:
-
Inter-Quartile Range
- IRB:
-
Institutional Review Board
- LTFU:
-
Lost to Follow-Up
- MRN:
-
Medical Record Number
- OI:
-
Opportunistic Infection
- PMTCT:
-
Prevention of Mother to Child Transmission
- SSA:
-
Sub-Saharan Africa
- SUCSH:
-
Salale University Comprehensive Specialized Hospital
- TB:
-
Tuberculosis
- UNAIDS:
-
United Nations Program on HIV/AIDS
- UNICEF:
-
United Nations International Children’s Emergency Fund
- WHO:
-
World Health Organization
References
UNAIDS. UNAIDS data 2021. Geneva: Joint United Nations Programme on HIV/AIDS; 2021.
UNICEF. UNICEF 2021world AIDS Day Report Stolen Children, Lost Adolescent. NY 10017, USA: UNICEF;: United Nations Plaza New York; 2021. p. 28.
UNICEF, Adolescent, HIV prevention - UNICEF DATA [Internet]. 2021 [cited 2022 Feb 23]. https://data.unicef.org/topic/hivaids/adolescents-young-people/
UNAIDS, Global HIV. & AIDS statistics — Fact sheet | UNAIDS [Internet]. 2022 [cited 2022 Feb 22]. https://www.unaids.org/en/resources/fact-sheet
Ammon N, Mason S, Corkery JM. Factors impacting antiretroviral therapy adherence among human immunodeficiency virus–positive adolescents in Sub-saharan Africa: a systematic review. Public Health. 2018;157:20–31.
Mayer KH, Venkatesh KK. Antiretroviral therapy as HIV Prevention: Status and prospects. Am J Public Health. 2010;100(10):1867–76.
Belay H, Alemseged F, Angesom T, Hintsa S, Abay M. Effect of late HIV diagnosis on HIV-related mortality among adults in general hospitals of Central Zone Tigray, northern Ethiopia: a retrospective cohort study. Dove Press J HIV/AIDS - Res Palliat Care. 2017;9:187–92.
Ford N, Meintjes G, Vitoria M. The evolving role of CD4 cell counts in HIV care. Curr Opin HIV AIDS. 2017;12:123–8.
Amour MA, Shayo GA, Matee MM, Machumi L, Rugarabamu A, Aris EA, et al. Predictors of mortality among adolescents and young adults living with HIV on antiretroviral therapy in Dar Es Salaam, Tanzania : a retrospective cohort study. J Int AIDS Soc. 2022;25:1–8.
Teeraananchai S, Puthanakit T, Kerr SJ, Chaivooth S, Kiertiburanakul S, Chokephaibulkit K, et al. Attrition and treatment outcomes among adolescents and youths living with HIV in the Thai National AIDS Program. J Virus Erad. 2019;5(1):33–40.
The Late Presentation Working Groups in EuroSIDA and COHERE. Estimating the burden of HIV late presentation and its attributable morbidity and mortality across Europe 2010–2016. BMC Infect Dis. 2020;20:728.
Ang LW, Toh MPHS, Wong CS, Boudville IC, Archuleta S, Lee VJM, et al. Short-term mortality from HIV-infected persons diagnosed from 2012 to 2016: impact of late diagnosis of HIV infection. Med (Baltim). 2021;100:26.
Kariminia A, Law M, Davies M, Vinikoor M, Wools-kaloustian K, Leroy V et al. Mortality and losses to follow-up among adolescents living with HIV in the IeDEA global cohort collaboration. J Int AIDS Soc. 2018;178.
Id DJ, Abebe W, Taye K, Ruff A, Hallstrom I. Adolescents living with HIV are at higher risk of death and loss to follow up from care: analysis of cohort data from eight health facilities in Ethiopia. PLoS ONE. 2019;14(10):e0223655.
Koech E, Teasdale CA, Wang C, Fayorsey R, Alwar T, Mukui IN, et al. Characteristics and outcomes of HIV-infected youth and young adolescents enrolled in HIV care in Kenya. AIDS. 2014;28(18):2729–38.
Gutman CK, Middlebrooks L, Camacho-gonzalez A. Asymptomatic adolescent HIV: in the Pediatric Emergency Department. AIDS Patient Care STDS. 2020;34(9):373–9.
McKinnon B, Vandermorris A. National age-of-consent laws and adolescent HIV testing in sub-saharan Africa: a propensity-score matched study. Bull World Health Organ. 2019;97(1):42–50.
Fiseha L, Terefe G, Yohannes H, Shimeles O. Assessment of Parent-Adolescent Communication on HIV/AIDS Prevention in Kemebata Temebaro Zone, Southern Ethiopia. J Infect Dis Epidemiol. 2016;2(1):008.
FMOH. National guidelines for Comprehensive HIV Prevention, Care and Treatment. Addis Abeba: Federal democratic republic of Ethiopia Minstriy of health; 2018.
Ayalew J, Moges H, Sahu O, Worku A. Identifying factors related to the survival of AIDS patients under the follow-up of antiretroviral therapy (ART): the case of South Wollo. Int J Data Envel Anal *Operations Res. 2014;1(2):21–7.
Antinori A, Coenen T, Costagiola D, Dedes N, Ellefson M, Gatell J, et al. Late presentation of HIV infection: a consensus definition. HIV Med. 2011;12:61–4.
Tesfaye B, Ermias D, Moges S, Astatkie A. Effect of the test and treat strategy on Mortality among HIV-Positive adult clients on antiretroviral treatment in Public hospitals of Addis Ababa, Ethiopia. Dove Press J HIV/AIDS -. Res Palliat Care. 2021;13:349–60.
Kleinbaum DG, Klein M. Survival Analysis: A Self-Learning Text. third edit. Gail M, Krickeberg K, Samet JM, Tsiatis A, Wong W, editors. New York: Springer Science + Business Media, LLC; 2012. 5–8 p.
Aemro A, Jember A, Anlay DZ. Incidence and predictors of tuberculosis occurrence among adults on antiretroviral therapy at Debre Markos referral hospital, Northwest Ethiopia : retrospective follow-up study. BMC Infect Dis. 2020;20:245.
WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity [Internet]. Geneva: World Health Organization. 2011. 1–6 p. https://apps.who.int/iris/bitstream/handle/10665/85839/WHO_NMH_NHD_MNM_11.1_eng.pdf
WHO Multicentre Growth Reference Study (MGRS). WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development [Internet]. World Health Organization, Department of Nutrition for Health and Development. Geneva, Switzerland: World Health Organization. 2006. 312 p. https://apps.who.int/iris/bitstream/handle/10665/43413/924154693X_eng.pdf
Nimkar S, Valvi C, Kadam D, Rewari BB, Kinikar A, Gupte N, et al. Loss to follow-up and mortality among HIV-infected adolescents receiving antiretroviral therapy in Pune, India. HIV Med. 2018;19(6):395–402.
Vogt F, Rehman AM, Kranzer K, Nyathi M, Van Griensven J, Dixon M, et al. Relationship between time to initiation of antiretroviral therapy and treatment outcomes: a cohort analysis of ART eligible adolescents in Zimbabwe. J Acquir Immune Defic Syndr. 2017;74(4):390–8.
Leshargie CT, Demant D, Burrowes S, Frawley J. Incidence and predictors of mortality among adolescents on antiretroviral therapy in Amhara Region, Ethiopia : a retrospective cohort analysis. BMJ Open. 2022;12.
Reif LK, Bertrand R, Benedict C, Lamb MR, Rouzier V, Verdier R, et al. Impact of a youth-friendly HIV clinic: 10 years of adolescent outcomes in Port-au-Prince, Haiti. J Int AIDS Soc. 2016;19(1):20859.
Op De Coul ELM, Van Sighem A, Brinkman K, Van Benthem BH, Van Der Ende ME, Geerlings S, et al. Factors associated with presenting late or with advanced HIV disease in the Netherlands, 1996 2014: results from a national observational cohort. BMJ Open. 2016;6(1):1–10.
Chet L, Hamid SA, Bachok N, Chidambaram S, Adnan WAW. Survival and prognostic factors of HIV-positive patients after antiretroviral therapy initiation at a Malaysian referral hospital. Saudi J Med Med Sci. 2021;9(2):135.
Tamir Z, Alemu J, Tsegaye A. Anemia among HIV infected individuals taking ART with and without zidovudine at Addis Ababa, Ethiopia. Ethiop J Health Sci. 2018;28(1):73–82.
Yu Y, Luo D, Chen X, Huang Z, Wang M, Xiao S. Medication adherence to antiretroviral therapy among newly treated people living with HIV. BMC Public Health. 2018;18(1):825.
MacArthur RD, Schaecher KL. Participating faculty: addressing adherence challenges associated with antiretroviral therapy: focus on noninfectious diarrhea. Am J Manag Care. 2013;19(12 SUPPL.).
Winston SE, Chirchir AK, Muthoni LN, Ayuku D, Koech J, Nyandiko W, et al. Prevalence of sexually transmitted infections including HIV in street-connected adolescents in western Kenya. BMJ. 2015;91:353–9.
AL Slogrove AS. The global epidemiologyof adolescents living with HIV: time for more granular data to improve adolescent health outcomes. Curr Opin HIV AIDS. 2018;13(3):170–8.
Gilliam PP, Ellen JM, Leonard L, Jevitt CM, Straub DM. Transition of adolescents with HIV to Adult Care: characteristics and current practices of the Adolescent Trials Network for HIV / AIDS interventions. J Assoc Nurses AIDS Care. 2011;22(4):283–94.
Cervia JS. Easing the transition of HIV-Infected adolescents to Adult Care. AIDS Patient Care STDS. 2013;27(12):692–6.
Idele P, Gillespie A, Porth T, Suzuki C, Mahy M, Kasedde S, et al. Epidemiology of HIV and AIDS among adolescents: current status, inequities, and data gaps. J Acquir Immune Defic Syndr. 2014;66(SUPPL 2):144–53.
Acknowledgements
We would like to express our special gratitude to Salale University for funding the study. We also gratefully appreciate health facility administrators in Salale University Comprehensive Specialized Hospital, Kuyu General Hospital, and Gundo-Meskel Primary Hospital for granting us permission to collect the necessary data. At last, but not least, our admiration goes to the data collectors and supervisors, as well as all other persons who contributed significantly, for their polite, sensitive, and cooperative approach, which results in obtaining excellent data.
Funding
Salale University funded the study.
Author information
Authors and Affiliations
Contributions
M.K. was responsible for data management, statistical analysis and interpretation, and wrote the original draft of the manuscript. T.B. and L.A. interpreted and supervised statistical analysis. C.K. and H.A. critically revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Salale University- College of Health Science ethical review committee, and an official letter was written to each selected hospital for their permission to undergo the study in their institution and for their possible cooperation and participation. Since this study was a retrospective record review, informed consent from individual patients was not feasible. The records, however, were accessed with written permission from the authorities of the three selected hospitals. Also, personal identifiers were not included in the final data file to ensure anonymity.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gabre, M.K., Tafesse, T.B., Geleta, L.A. et al. The effect of late presentation on HIV related mortality among adolescents in public hospitals of north showa zone Oromiya, Ethiopia; 2022: a retrospective cohort study. BMC Infect Dis 24, 644 (2024). https://doi.org/10.1186/s12879-024-09550-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09550-3