Abstract
In January 2020, a different cervical cancer screening program started in Germany. Women above the age of 35 are recommended to have a combined HPV and cytology swab every three years. Showing persistent high-risk human papillomavirus (hrHPV), cytologic negative cervical samples at baseline and after 12 months, patients are referred to colposcopy. Entailing considerable additional workload due to the required colposcopies, we analyzed the risk of high-grade cervical intraepithelial neoplasia (CIN 3) in cytologic negative and persistent hrHPV women according to their hrHPV genotypes.
Methods In this single center retrospective study, patients with persistent hrHPV, cytology negative cervical samples from our certified Colposcopy Unit in 2020 and 2021 were analyzed. Patient demographics, hrHPV types, biopsy rates and histological reports were collected.
Results During the study, 69 patients were enrolled. Most frequent hrHPV genotypes were: hrHPV other 72.5%; HPV 16, 20.3% and HPV 18, 7.2%. Colposcopy showed no or minor changes in 92.7% and major changes in 7.2%. CIN 3 was found in 7 patients (10.1%). Prevalence of CIN 3 by hrHPV genotypes was 27.3% for HPV16, 20.0% for HPV18 and 7.1% for HPVO. A statistically significant dependency between hrHPV and cervical intraepithelial neoplasia was demonstrated (p = 0.048).
Conclusion Within this single center study of persistent hrHPV, cytologic negative samples, patients with HPV 16 were more likely to have high-grade disease compared to other hrHPV subtypes. Larger prospective randomized trials are needed to substantiate our results and obtain adjusted cervical cancer screening time intervals according to the hrHPV genotypes.
Similar content being viewed by others
Introduction
Cervical cancer is the fourth most frequently diagnosed cancer worldwide and the second leading cause of cancer death in women with a cervix [1]. In Germany the prevalence of cervical cancer and precancerous lesions has declined over the last 30 years due to opportunistic screening and increased vaccination rates against high-risk human papillomavirus (hrHPV) types [2,3,4]. Nevertheless, the focus on prevention and early diagnosis of cervical cancer remains crucial. It is widely acknowledged that high-grade cervical intraepithelial neoplasia and invasive cervical cancers are caused by persistent hrHPV infections [5]. The human papillomavirus (HPV) genotypes 16 and 18 are responsible for more than 75% of cervical carcinomas and the precursor lesions. The risk of persistence and neoplastic progression to high-grade cervical intraepithelial neoplasia and cervical cancer differs markedly by HPV genotype. Although several HPV types have been characterised as high-risk HPV with carcinogenic potential, they do not appear to display a comparable carcinogenicity. Infection with HPV 16 has the greatest tendency to persist and the highest probability for causing neoplastic progression, followed by infection with HPV 18, HPV 31 and HPV 33 [6, 7]. These facts indicate the potential value of additional genotyping in cervical cancer screening. In Germany, cervical cancer screening is conducted in accordance with the 2020 oKFE-RL Cancer Screening Guidelines, which recommend co-testing for cytology and HPV DNA in patients aged 35 years and older. Joint cytology and HPV screening at 3-year intervals appears to constitute a low risk of CIN 3 in patients who were negative for both HPV and cytology testing at baseline, and they are referred to repeating co-testing every 3 years. Patients with normal Papanicolaou (PAP) smear (PAP I) and the detection of high-risk HPV DNA at baseline and one year thereafter are referred to colposcopy due to the increased risk of developing CIN 3.
The introduction of this new approach to cervical cancer screening has led to an increase in the number of colposcopies required in cytology- negative patients.The aim of this study was to analyse the risk of high-grade cervical intraepithelial neoplasia in cytologically negative and persistent hrHPV patients according to their HPV genotypes.
Methods
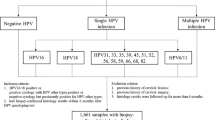
This retrospective study was conducted in the dysplasia unit of the Klinikum Dortmund gGmbH. Only patients above the age of 35 with negative cytology and persistent positive hrHPV for at least 12 months met the inclusion criteria and were identified through the institutional dysplasia database. The results of cytological examinations and HPV tests were obtained from patients` gynaecologists. Cytology was performed in accordance with standard procedure. The specific HPV tests chosen were not explicitly specified. The results differentiated between HPV 16 or HPV 18 or HPVO (= others) positivity. The subgroup “others” comprises the WHO defined high risk subtypes except 16 and 18 (31,33,35,39,45,51,52,56,58,59,66). Colposcopic examination was conducted by two senior consultants. Histopathological findings and detailed information were extracted from the database of the Institute of Pathology. Patient demographics, HPV genotype, colposcopic assessment, biopsy rates and histologic diagnosis were recorded.
A comprehensive descriptive and exploratory analysis of the data was performed, including frequencies and percentages. Fisher´s Exact Test was applied to test the global hypothesis of an association between HPV genotypes and histology diagnoses [8]. Furthermore, the influence of hrHPV genotype on the categories of cervical intraepithelial neoplasia was examined using a proportional odds model that also accounted for covariates such as colposcopy results, transformation zone and age [9]. For all statistical tests, a level of significance of 0.05 was considered. All statistical analyses were conducted using the statistical software R (version 4.3.0) [10]. In addition, the R package ordinal was used for modelling [11].
The study was approved by the ethics committee of the university Witten/Herdecke (S-03/2023). It was performed in accordance with the principles of good clinical practice and the Declaration of Helsinki. As the study involved retrospective evaluation of routine data, the Ethics committee granted exemption from the requirement of informed consent.
Results
Following referral with persistently positive hrHPV, cytologically negative cervical samples, 69 patients were examined as new patients in the certified Colposcopy Unit between 1/1/2020 and 12/31/2021 according to the oKFE-RL´s new referral pathway (Fig. 1).
Patient characteristics
Median age at referral was 51 years (range: 35–82 years). The grouped age frequencies are listed in Table 1. The most frequent hrHPV was HPVO with 72.5% (n = 50), followed by HPV 16 with 20.3% (n = 14) and HPV 18 with 7.2% (n = 5). Transformation zone (TZ) 3 was the predominant zone in 68.1% of patients (n = 47), in contrast to TZ 1 and 2 in 31.9% of patients (n = 22). In 84.1% of patients (n = 58), a target biopsy or endocervical curettage (ECC) was performed during the colposcopy assessment.
Outcomes from colposcopy
Adequate colposcopy assessment was performed by the two senior consultants in all examined patients. 56.5% (n = 39) showed normal colposcopy, minor and major changes were detected in 36.2% (n = 23) and 7.2% (n = 5), respectively. In the subgroup of HPV 16 positive patients, normal colposcopy, minor and major changes were found in 50.0%, 35.7% and 14.3%, respectively. In comparison, in HPVO positive patients, normal colposcopy was predominant with 62.0%, followed by 34.0% with minor and 4.0% with major changes. In the subgroup of HPV 18 positive patients, only one colposcopy assessment was normal (20.0%), three patients (60.0%) showed minor, and one patient major changes (20.0%).
Thirty-two biopsies showed normal histology. In this group, 14 patients (43.8%) exhibited minor and two patients (6.2%) exhibited major changes in colposcopy, whereas eight out of ten patients with CIN 2 had normal colposcopy assessments. This discrepancy can be attributed to the fact that the majority of patients with CIN 2 had TZ 3 (90.0%), which represents one of the most challenging aspects of colposcopy. Only one patient with histological confirmation of CIN 3 exhibited normal colposcopy findings (14.3%). For CIN 3, the majority of patients demonstrated minor changes (57.1%).
Histological diagnosis and HPV genotype
A total of 11 patients without biopsies were excluded from the subsequent statistical analysis. The remaining 58 patients are the focus of our discussion. During the study period, no cancers were detected in patients referred with persistently positive hrHPV samples whose cytology was negative. In total, 15.5% of referrals were diagnosed with CIN I (n = 9), 17.2% with CIN 2 (n = 10), and 12.1% with CIN 3 (n = 7). Furthermore, the histologic results were analysed in the context of hrHPV genotypes. Table 2 and the corresponding mosaicplot in Fig. 2 illustrate the frequency distribution of histology findings for the biopsied patients, stratified by HVP 16, 18, and HPVO.
Among patients with HPV 16, CIN 2 was observed only once, whereas CIN 1 and 3 were diagnosed in 27.3% (n = 3) of cases, respectively. In HPV 18 positive patients, CIN 1 was found in 40.0% of cases (n = 2). Other CIN stages were observed only once each (20.0% each). In patients with HPVO the prevalence of CIN 3 was 7.1% (n = 3). Normal histology was most frequently observed within HPVO (64.3%). Based on Table 2 Fisher’s Exact Test demonstrated a statistically significant dependency between hrHPV genotypes and cervical intraepithelial neoplasia (p = 0.048).
To quantify the relationship between histologic findings and hrHPV genotypes, a proportional odds model was developed to consider colposcopy results, transformation zone, and age.
The proportional odds model did not yield statistically significant results, which is likely due to the limited sample size in this study.
Discussion
In recent years, it has been established that high-grade cervical neoplasia and invasive cervical cancers are caused by persistent infection with hrHPV [6, 12]. Primary HPV screening is significantly more sensitive for high-grade disease prediction than cytology alone [13]. Long-term data from HPV screening trials indicate a low risk of high-grade CIN in HPV negative and cytologically negative patients [14, 15]. Conversely, in patients with negative cytology and persistent hrHPV infection, high-grade CIN and cervical cancer rates are notably higher [14].
Following the implementation of HPV-based cervical cancer screening in several countries (Australia, Italy, Netherlands, New Zealand, Sweden or the UK) for an extended period, the introduction of HPV- and cytology-based screening in Germany commenced in 2020. The growing number of colposcopies resulting from the implementation of the new co-testing (cytology and test for high-risk HPV), has been the subject of considerable debate, as under the new national guidelines hrHPV positive patients with normal cytology are now additionally referred for colposcopy [16]. At our institution, we observed a noteworthy increase of 30% in the number of colposcopies completed.
In this study,we present data on the risk of CIN 3 according to the hrHPV genotype in cytologically negative patients. Regarding the quality of colposcopy, only adequate colposcopic settings were performed by two senior consultants. The rate of inadequate colposcopy in patients with persistent hrHPV varies in literature between 0.59% [17], and 4.8% [13].
In our sample, transformation zone 3 (TZ 3) was predominant with 68.1% while transformation zone 1/2 occurred in 31.9%. This is likely due to the median age of 51 years in our group. Furthermore, the new screening is intended for patients over the age of 35. These findings are consistent with a German cohort analysis which demonstrated TZ 3 in 62.6% and TZ 1/2 in 37.5%, respectively [17].
The colposcopic appearance is thought to depend on the HPV high-risk subtype. In the case of HPVO, 62.0% of patients exhibited normal colposcopy, while in HPV 16, minor and major changes were observed in 50.0%. Jeronimo et al. 2007 reported increased detection of abnormalities in colposcopy in the presence of HPV 16, while van der Marel et al. 2014 denied any relationship between colposcopic characteristics and HPV 16 [18, 19]. The question of whether certain hrHPV genotypes have an impact on colposcopic appearance remains open.
The biopsy rate in our study was 84.1%. which is considerably higher than the rates reported in the literature. A review of European studies that investigated the efficacy of HPV-based screening revealed biopsy rates ranging from 2 to 11%. In contrast a biopsy rate of 31% was found in a retrospective cohort study in England [13, 15].
No cases of invasive cancer were identified in our cohort, but 15.5%, 17.2%, and 12.1% of participants exhibited CIN 1, CIN 2 and CIN 3,respectively. The increased detection of CIN 1 and CIN 2 may give rise to concerns regarding the potential for overtreatment of early lesions, as CIN 1 and CIN 2 may regress spontaneously in 60% and 55% of cases, respectively [20]. The regression rate of CIN 1 and 2 was significantly higher in hrHPV negative patients younger than 30 years.The overall progression to invasive cancer was less than 0.5% [20]. Therefore, conservative treatment might be considered. The incidence of CIN 3 (12.1%) observed in our study is consistent with other authors who found 13.0% of CIN 2 + in their register analysis of 1139 cytologic negative, hrHPV positive patients [21]. A focus on the hrHPV genotypes revealed that normal histology was the predominant finding in HPVO (64.3%), followed by HPV 16 (36.4%) and HPV 18 (20.0%). In contrast CIN 3 was mainly observed in HPV 16 (27.3%), followed by HPV 18 (20.0%) and HPVO (7.1%).
Our findings are supported by a danish cohort study.This study demonstrated that CIN 3 occurs in 26.7% of cases with HPV 16 and 19.1% of cases with HPV 18 [6]. The HPV testing strategy employed in this study included a differential testing of 13 high-risk HPV subtypes. The data from this study group also revealed that HPV 31 and 33 exhibited noteworthy carcinogenic potential (14.3%, and 14.9%, respectively) [6]. All remaining hrHPV subtypes were summarized as HPVO with an estimated probability of CIN 3 of 6.0%. Our study revealed a higher risk of developing high-grade cervical neoplasia in patients with HPV 16 compared to other HPV types. This is consistent with other authors who have demonstrated that HPV 16 has the highest oncogenic potential and the highest likelihood of developing CIN 3, [6, 22,23,24].
The limitation of our study results from the retrospective data collection and the small number of patients in a single centre dysplasia unit. We only obtained both the results of cytology and the HPV-testing from the gynaecologists. Cytology was performed conventionally as Thin prep is not supported by the healthcare system. The HPV test chosen was not explicitly specified. The results were divided into HPV 16 or HPV 18 or HPV others. HPV- “Others” is a generally accepted summary of the remaining WHO recognized subtypes (31,33,35,39,45,51,52,56,58,59,66). A complete typification was not available in our study.
Our retrospective data suggest that extended screening intervals could be possible without risk in cytologic negative hrHPV positive patients that is not 16 or 18 as the risk of CIN was relevantly lower in our HPVO subgroup.
For future investigations prospective data collection containing complete HPV genotyping will be of great interest. The results might exactly demonstrate the statistical risk of developing cervical precusor lesions, CIN 3 in particular, according to hrHPV genotype and will possibly have an impact on screening intervals without comprising patient safety.
Availability of data and materials
The datasets generated or analyzed during the current study are not publicly available but are available from the correspondig author upon reasonable request.
Abbreviations
- HPV:
-
Human papilloma virus
- hrHPV:
-
High-risk human papillomavirus
- DNA:
-
Desoxyribonucleic acid
- CIN:
-
Cervical intraepithelial neoplasia
- PAP:
-
Papanicolaou
- HPVO:
-
Human papillomavirus type others (high-risk, not 16,18)
- WHO:
-
World health organization
- TZ:
-
Transformation zone
- ECC:
-
Endocervical curettage
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660. (Epub 2021 Feb 4 PMID: 33538338).
Nancy M. McClung, Julia W. Gargano, Nancy M. Bennett, Linda M. Niccolai, Nasreen Abdullah, Marie R. Griffin, Ina U. Park, Angela A. Cleveland, Troy D. Querec, Elizabeth R. Unger, Lauri E. Markowitz; for the HPV-IMPACT Working Group, Trends in Human Papillomavirus Vaccine Types 16 and 18 in Cervical Precancers, 2008–2014. Cancer Epidemiol Biomarkers Prev. 2019;28(3):602–609.
Guan P, Howell-Jones R, Li N, Bruni L, de Sanjosé S, Franceschi S, Clifford GM. Human papillomavirus types in 115,789 HPV-positive women: a meta-analysis from cervical infection to cancer. Int J Cancer. 2012;131(10):2349–59. https://doi.org/10.1002/ijc.27485. (Epub 2012 Mar 20 PMID: 22323075).
Muñoz N, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah KV, Snijders PJ, Meijer CJ; International Agency for Research on Cancer Multicenter Cervical Cancer Study Group. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348(6):518–27. https://doi.org/10.1056/NEJMoa021641. PMID: 12571259.
de Sanjose S, Quint WG, Alemany L, Geraets DT, Klaustermeier JE, Lloveras B, Tous S, Felix A, Bravo LE, Shin HR, Vallejos CS, de Ruiz PA, Lima MA, Guimera N, Clavero O, Alejo M, Llombart-Bosch A, Cheng-Yang C, Tatti SA, Kasamatsu E, Iljazovic E, Odida M, Prado R, Seoud M, Grce M, Usubutun A, Jain A, Suarez GA, Lombardi LE, Banjo A, Menéndez C, Domingo EJ, Velasco J, Nessa A, Chichareon SC, Qiao YL, Lerma E, Garland SM, Sasagawa T, Ferrera A, Hammouda D, Mariani L, Pelayo A, Steiner I, Oliva E, Meijer CJ, Al-Jassar WF, Cruz E, Wright TC, Puras A, Llave CL, Tzardi M, Agorastos T, Garcia-Barriola V, Clavel C, Ordi J, Andújar M, Castellsagué X, Sánchez GI, Nowakowski AM, Bornstein J, Muñoz N, Bosch FX; Retrospective International Survey and HPV Time Trends Study Group. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11(11):1048–56. https://doi.org/10.1016/S1470-2045(10)70230-8. Epub 2010 Oct 15. PMID: 20952254
Kjær SK, Frederiksen K, Munk C, Iftner T. Long-term absolute risk of cervical intraepithelial neoplasia grade 3 or worse following human papillomavirus infection: role of persistence. J Natl Cancer Inst. 2010;102(19):1478–88. https://doi.org/10.1093/jnci/djq356. Epub 2010 Sep 14. PMID: 20841605; PMCID: PMC2950170.
Bernard, Erik et al. “Comparing human papillomavirus prevalences in women with normal cytology or invasive cervical cancer to rank genotypes according to their oncogenic potential: a meta-analysis of observational studies.” BMC Infect Dis . 2013;13:373. https://doi.org/10.1186/1471-2334-13-373
Mehta CR, Patel NR. A network algorithm for performing fisher’s exact test in r × c contingency tables. J Am Stat Assoc. 1983;78(382):427–34. https://doi.org/10.1080/01621459.1983.10477989.
Agresti A. Categorical Data Analysis. 2nd ed. New York: Wiley; 2002. https://doi.org/10.1002/0471249688.
R Core Team: R: A Language and Environment for Statistical Computing, R Foundation for Statistical Computing, Vienna, Austria. (2023). https://www.R-project.org/.
Christensen R. H. B.: ordinal - Regression Models for Ordinal Data, R package version 2022.11–16. (2022).
Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007;370(9590):890–907. https://doi.org/10.1016/S0140-6736(07)61416-0. (PMID: 17826171).
Macdonald M, Crossley J, Ellis K, Dudding N, Lyon R, Smith JHF, Tidy JA, Palmer JE. Prevalence of high-grade cervical intraepithelial neoplasia in women with persistent high-risk HPV genotypes and negative cytology. Cytopathology. 2018;29(2):133–42. https://doi.org/10.1111/cyt.12516. (Epub 2018 Jan 19 PMID: 29350424).
Dijkstra MG, van Zummeren M, Rozendaal L, van Kemenade FJ, Helmerhorst TJ, Snijders PJ, Meijer CJ, Berkhof J. Safety of extending screening intervals beyond five years in cervical screening programmes with testing for high risk human papillomavirus: 14 year follow-up of population based randomised cohort in the Netherlands. BMJ. 2016;4(355):i4924. https://doi.org/10.1136/bmj.i4924.Erratum.In:BMJ.2016Oct27;355:i5782. (PMID: 27702796).
Ronco G, Dillner J, Elfström KM, Tunesi S, Snijders PJ, Arbyn M, Kitchener H, Segnan N, Gilham C, Giorgi-Rossi P, Berkhof J, Peto J, Meijer CJ; International HPV screening working group. Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet. 2014;383(9916):524–32. https://doi.org/10.1016/S0140-6736(13)62218-7. Epub 2013 Nov 3. Erratum in: Lancet. 2015 Oct 10;386(10002):1446. PMID: 24192252.
Gemeinsamer Bundesausschuss (G-BA). Beschluss des Gemeinsamen Bundesausschusses über eine Änderung der Krebsfrüherkennungs-Richtlinie und eine Änderung der Richtlinie für organisierte Krebsfrüherkennungsprogramme: Programm zur Früherkennung von Zervixkarzinomen. (2018). https://www.g-ba.de/downloads/39–261–3597/2018–11–22_oKFE-RL_Zervixkarzinom.pdf. Accessed 12 June 2023
Wittenborn J, Kupec T, Iborra S, Najjari L, Kennes LN, Stickeler E. CIN2 + detection in high-risk HPV patients with no or minor cervical cytologic abnormalities: a clinical approach validated by machine learning. Arch Gynecol Obstet. 2023;307(3):881–90. https://doi.org/10.1007/s00404-023-06953-6. Epub 2023 Feb 13. PMID: 36780042; PMCID: PMC9984503.
Jeronimo J, Massad LS, Schiffman M. National Institutes of Health/American Society for Colposcopy and Cervical Pathology (NIH/ASCCP) Research Group. Visual appearance of the uterine cervix: correlation with human papillomavirus detection and type. Am J Obstet Gynecol. 2007;197(1):47.e1–8. https://doi.org/10.1016/j.ajog.2007.02.047.
van der Marel J, van Baars R, Rodriguez A, Quint WG, van de Sandt MM, Berkhof J, Schiffman M, Torné A, Ordi J, Jenkins D, Verheijen RH, Helmerhorst TJ, Ter Harmsel B, Wentzensen N, Del Pino M. The increased detection of cervical intraepithelial neoplasia when using a second biopsy at colposcopy. Gynecol Oncol. 2014;135(2):201–7. https://doi.org/10.1016/j.ygyno.2014.08.040. (Epub 2014 Sep 7 PMID: 25204846).
Loopik, Diede L. MD, PhD1; Bentley, Heidi A. MD2; Eijgenraam, Maria N. MsC1; IntHout, Joanna PhD3; Bekkers, Ruud L. M. MD, PhD4,5; Bentley, James R. MB, ChB, FRCSC6. The Natural History of Cervical Intraepithelial Neoplasia Grades 1, 2, and 3: A Systematic Review and Meta-analysis. J Lower Genital Tract Dis. 2021;25(3):221–231. https://doi.org/10.1097/LGT.0000000000000604.
Henes M, Mann E, Hirchenhain C, Bauer E, Kentner A, Quaas J, Koßagk C, Gallwas J, Henes L, Schumacher A, Küppers V. Registry Study of the Working Group on Cervical Pathology and Colposcopy (AGCPC) on the diagnostic algorithm for the new cervical cancer screening - initial data. Geburtshilfe Frauenheilkd. 2023;83(10):1250–62.https://doi.org/10.1055/a-2159-7510. PMID:37808262;PMCID:PMC10556876.
Sand FL, Munk C, Frederiksen K, Junge J, Iftner T, Dehlendorff C, Kjaer SK. Risk of CIN3 or worse with persistence of 13 individual oncogenic HPV types. Int J Cancer. 2019;144(8):1975–82. https://doi.org/10.1002/ijc.31883. (Epub 2019 Jan 10 PMID: 30246864).
Thomsen LT, Frederiksen K, Munk C, Junge J, Iftner T, Kjaer SK. Long-term risk of cervical intraepithelial neoplasia grade 3 or worse according to high-risk human papillomavirus genotype and semi-quantitative viral load among 33,288 women with normal cervical cytology. Int J Cancer. 2015;137(1):193–203. https://doi.org/10.1002/ijc.29374. (Epub 2014 Dec 12 PMID: 25471319).
Naucler P, Ryd W, Törnberg S, Strand A, Wadell G, Hansson BG, Rylander E, Dillner J. HPV type-specific risks of high-grade CIN during 4 years of follow-up: a population-based prospective study. Br J Cancer. 2007;97(1):129–32. https://doi.org/10.1038/sj.bjc.6603843. Epub 2007 Jun 5. PMID: 17551490; PMCID: PMC2359659.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
BK and EU conceived of and designed the study, EU performed data collection, BK supervised all data collection and completed the manuscript ; CvM performed the data analysis and prepared tables. All authors substantially revised the manuscript, suggested modifications and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of the University Witten/Herdecke (study-number: S-03/2023).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kipp, B., Ulrich, E., van Meegen, C. et al. Risk of cervical high-grade squamous intraepithelial neoplasia in cytologic negative and persistently high-risk human papillomavirus positive patients according to genotypes: a retrospective single center analysis. BMC Infect Dis 24, 558 (2024). https://doi.org/10.1186/s12879-024-09449-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09449-z