Abstract
Streptococcus suis is one of the most common zoonotic pathogens, in humans and can cause meningitis, endocarditis, arthritis and sepsis. Human cases of Streptococcus suis infection have been reported worldwide, and most of those cases occurred in Asia. Hearing loss is the most common sequela of Streptococcus suis meningitis. Streptococcus suis infection complicated with acute cerebral infarction has rarely been reported. Therefore, to provide a reference for this disease, we reported a case of acute multiple brain infarctions associated with Streptococcus suis infection. In our report, a 69yearold male patient had Streptococcus suis meningitis and sepsis, which were associated with multiple acute cerebral infarctions in the pons and bilateral frontotemporal parietal occipital lobes. After treatment, the patient exhibited cognitive impairment, dyspraxia and irritability. There are limited case reports of cerebral infarction associated with Streptococcus suis infection, and further research is needed to determine the best treatment method.
Similar content being viewed by others
Introduction
Streptococcus suis is one of the most common zoonotic pathogens in humans and can cause meningitis, endocarditis, arthritis and sepsis after direct contact with pigs or pork [1,2,3]. Patients with severe infection may present with Streptococcal Toxic Shock-Like Syndrome (STSLS) or Streptococcus meningitis syndrome. Human cases of S. suis infection have been reported worldwide, and most of these cases are in Asia [3]. S. suis strains are classified serologically into 35 serotypes; serotype 2 is the most virulent and is closely associated with human and pig diseases [3]. Hearing loss is the most common sequela of S. suis meningitis [2, 3]. Patients may also present with other neurological sequelae, such as cognitive impairment, tinnitus and other symptoms [2]. This article reports a case of Streptococcus suis infection associated with acute cerebral infarction.
Case presentation
A 69-year-old male patient was admitted to the hospital on 22 September 2022 due to fever lasting for 4 h and coma for 2.5 h. At midnight on 22nd September the patient developed vomiting and loss of consciousness. Then, the spouse called 120 and took him to the emergency department of our hospital. The patient was soon admitted to our Department of Neurology due to an unexplained coma. The patient was a retired corporate executive, and his job was not associated with pigs or pork. The patient cut his left hand with a kitchen knife before onset, and this could have led to an infection. The spouse denied that the patient had any history of hypertension, heart disease, or diabetes. The spouse denied that the patient had a history of substance abuse. Physical examination after admission revealed a body temperature of 39.5℃, pulse rate of 142 beats/minute, respiratory rate of 45 breaths/minute, and blood pressure of 188/102 mmHg. His Glasgow coma scale score was 6 points. There was a 0.5 cm wound on the left index finger. His pupils were equal in size, and his pupillary reflexes were intact. There was no signs of meningeal irritation. The muscle strength of the right upper limb was roughly measured at grade 3. The right lower limb and left limb could not be lifted and could only move on the bed, so the muscle strength of the right lower limb and left limb were roughly measured at grade 2. The extremity tendon reflexes of the patient were normal, and he had a negative bilateral Babinski sign. His National Institutes of Health Stroke Scale (NIHSS) score was 24 points. Because the patient had shortness of breath, the patient was transferred to the intensive care unit (ICU) a few hours after admission. He was mechanically ventilated and underwent lumbar puncture.
His routine blood test results were as follows: white blood cell count, 16.27 × 109/L; neutrophil ratio, 90.8%; neutrophil count, 14.77 × 109/L; hemoglobin, 141 g/L; and platelet count, 128 × 109/L. The creatinine concentration was 107 µmol/L, the serum procalcitonin concentration was 32 ng/mL, the lactic acid concentration was 10.2mmol/L, the glucose concentration was 21.3 mmol/L, the cholesterol concentration was 5.24 mmol/L, the triglyceride concentration was 2.59 mmol/L and the low-density lipoprotein was 2.82 mmol/L. The patient had normal liver function. A cerebrospinal fluid analysis revealed a glucose level of 1.4 mmol/L, a protein concentration of 1.46 g/L, a chloride concentration of 101 mmol/L, a white blood cell count of 4400 × 106/L and a cerebrospinal fluid pressure of 330 mmH2O. Blood and cerebrospinal fluid cultures revealed S. suis serotype 2, which was resistant to tetracycline and clindamycin. Table 1 lists the laboratory data of the patients.
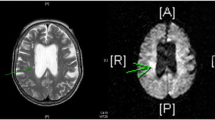
Brain computed tomography (CT) revealed lacunar cerebral infarction of the pons, left basal ganglia, and bilateral corona radiata. Computer tomography angiography (CTA) revealed severe stenosis in the M2 segment of the left middle cerebral artery and the P2 segment of the posterior cerebral artery; moreover, moderate stenosis was detected in the basilar artery, the A3 segment of the left anterior cerebral artery and the M2 segment of the right middle cerebral artery. The P2 segment of the posterior cerebral artery and the basilar artery are shown in Fig. 1.
Imaging examination of the patient. Diffusion-weighted magnetic resonance imaging of the brain revealed high signals in the pons and bilateral frontotemporal parietal occipital lobes (A, B, C). Computed tomography angiography showed severe stenosis in the P2 segment of the posterior cerebral artery and moderate stenosis in the basilar artery (D)
At first, the patient was empirically given anti-infection treatment with 2 g of meropenem q8h. To reduce intracranial pressure and inflammation, dexamethasone therapy(20 mg qd) were administered. At the same time, the patient was given antiplatelet treatment with clopidogrel, hypolipidemic treatment with atorvastatin, antihypertensive treatment with amlodipine besylate, sugars were controlled with insulin, and cerebral circulation improvement with butyphthalide. For antishock treatment, blood volume was supplemented and norepinephrine was implemented. A clear diagnosis of S. suis meningitis was obtained on 23 September, and the antibiotic treatment was changed to ceftriaxone 3 g q24h combined with penicillin 4.8 million units q6h from 23 September to 26 September. After 5 days of treatment, the patient’s condition was stable, but he was still unconscious. Considering the delayed appearance of cerebral infarction lesions on CT, brain magnetic resonance imaging was performed, which revealed multiple acute cerebral infarctions in the pons and bilateral frontotemporal parietal occipital lobes (Fig. 1). After being weaned off the ventilator and after his state of shock improved, the patient was transferred to the Department of Neurology on 4 October. His temperature decreased to normal from 17 October. Antibiotics were discontinued on 24 October. After treatment, the patient gradually became conscious but showed symptoms of irritability, aggression, and insomnia, and was verbally abusive. He could execute simple commands, such as raising his hands and closing his eyes. He always answered questions wrong and often talked to himself. Olanzapine and alprazolam were initiated to alleviate the symptoms. The patient was transferred to the rehabilitation department on 11 November, and he was discharged on 2 December. At the time of discharge, the patient exhibited cognitive impairment and irritability. The muscle strength of the limbs was grade 4. Due to his cognitive impairment, the patient’s hearing in both ears and Mini-Mental State Examination (MMSE) score could not be checked. His NIHSS score was 4 points, and his modified Rankin scale (mRS) score was 3 points.
Discussion
Streptococcus suis, a heterogeneous Gram-positive bacterium, can cause zoonotic diseases. People who are occupationally exposed to pigs and/or pork are the main risk groups. Contact with pigs or pork products and consuming raw pig meat or blood are important routes of infection. Many reported human cases of S. suis infection have been reported worldwide, with approximately 83.6% occurring in Vietnam, Thailand, and China. This has created serious health problems for China [4]. S. suis serotype 2 is most closely associated with human infections [3, 5] and may cause a variety of symptoms, including purulent meningitis and sepsis, the most common of which is purulent meningitis. Patients often present with fever, headache, neck stiffness, altered consciousness, and nausea or vomiting [2]. Infections of other a-hemolytic streptococci, such as Streptococcus pneumoniae, viridans group streptococci, ‘Group D streptococci’, and enterococci, may cause similar symptoms, and culture, polymerase chain reaction (PCR) and serum agglutination tests can help to differentiate among the various species [1, 3]. The key treatment is the use of antibiotics based on sensitivity testing, and ceftriaxone and penicillin are often chosen [2]. Most patients have a good prognosis, and approximately one-third of patients recover without sequelae [2]. The fatality rate of meningitis caused by S. suis is 2.9% [2].
The most common sequela of patients who have recovered from purulent meningitis caused by S. suis infection is hearing loss. Up to one-half of patients indicate hearing loss can occur at presentation or a few days later.
The use of dexamethasone may improve hearing impairment [6]. We attempted to evaluate the patient’s hearing, but more detailed professional tests were not available due to the uncooperative nature of the patient. The presence and extent of hearing loss in our patient was uncertain. In this report, the patient also exhibited cognitive impairment. Compared with hearing loss, cognitive impairment is a rare sequela of S. suis, and previous research has suggested that cognitive impairment was present in only 2 of 286 patients (0.70%) [2]. Poststroke dementia is also a concern. However unfortunately, we were unable to assess the extent of the patient’s dementia, and a diagnosis of poststroke dementia could not be made during the current course of the disease. At the time of discharge, the patient still had difficulty communicating and living independently.
In this case, after considering that the patient had meningitis and sepsis, combination therapy with ceftriaxone and penicillin was given. Streptococcus suis is generally susceptible to a variety of antibiotics, such as penicillin, ampicillin, amoxicillin, flucloxacillin, cephalosporin and ceftriaxone [3, 7]. Ceftriaxone and penicillin are most often selected for treatment [2]. However, previous studies have suggested that the use of penicillin and ceftriaxone alone is not always effective for severe cases [8, 9]. For severe cases, combination therapy with multiple antibiotics is reasonable [1].
Ischemic stroke is a common complication of bacterial meningitis and occurs in 10–29% of cases [10]. However, S. suis complicated with acute cerebral infarction has rarely been reported. Xing et al. [11] reported a case of S. suis meningitis with acute cerebral infarction. However, it was a lacunar cerebral infarction, and after treatment, the patient had no obvious neurological sequelae except for hearing loss in both ears. Previous research has suggested that Streptococcus causes cerebral ischemia by augmenting atherosclerosis, causing systemic inflammation [12], and promoting thrombosis [13]. Autopsies of patients who died of S. suis infection revealed multiple organ hemorrhage, cerebral edema, leptomeningeal congestion and disseminated intravascular coagulation [14]. These changes may promote cerebral ischemia. It is worth noting that the patient suffered from hypertension, diabetes and hyperlipidemia, and the CTA also showed that his cerebral blood vessels had multiple stenosic lesions. This patient was at a high risk of cerebral infarction, and we hypothesize that S. suis infection may be a trigger for cerebral infarction rather than a major cause; however more research is needed in the future to determine this relationship.
Conclusion
In the present study, we reported a case of cerebral infarction associated with S. suis infection. For anti-infection treatment, meropenem, penicillin, and ceftriaxone were used and the treatment lasted from September 22 to October 24. After treatment, the patient exhibited cognitive impairment, dyspraxia and irritability. There are limited case reports of cerebral infarction associated with S. suis infection, and further research is needed to determine the best treatment method.
Data availability
Data are available on request from the corresponding author upon reasonable request.
References
Lun Z-R, Wang Q-P, Chen X-G, Li A-X, Zhu X-Q. Streptococcus suis: an emerging zoonotic pathogen. Lancet Infect Dis. 2007;7(3):201–9. https://doi.org/10.1016/s1473-3099(07)70001-4.
Small PLC, van Samkar A, Brouwer MC, Schultsz C, van der Ende A, van de Beek D. Streptococcus suis Meningitis: a systematic review and Meta-analysis. PLoS Negl Trop Dis. 2015;9(10). https://doi.org/10.1371/journal.pntd.0004191.
Dutkiewicz J, Sroka J, Zając V, Wasiński B, Cisak E, Sawczyn A, Wójcik-Fatla A. Streptococcus suis: a re-emerging pathogen associated with occupational exposure to pigs or pork products. Part I– epidemiology. Ann Agric Environ Med. 2017;24(4):683–95. https://doi.org/10.26444/aaem/79813.
Goyette-Desjardins G, Auger J-P, Xu J, Segura M, Gottschalk M. Streptococcus suis, an important pig pathogen and emerging zoonotic agent—an update on the worldwide distribution based on serotyping and sequence typing. Emerg Microbes Infections. 2019;3(1):1–20. https://doi.org/10.1038/emi.2014.45.
Gottschalk M, Segura M, Xu J. Streptococcus suis infections in humans: the Chinese experience and the situation in North America. Anim Health Res Rev. 2007;8(1):29–45. https://doi.org/10.1017/s1466252307001247.
Huong VT, Ha N, Huy NT, Horby P, Nghia HD, Thiem VD, Hirayama K. Epidemiology, clinical manifestations, and outcomes of Streptococcus suis infection in humans. Emerg Infect Dis. 2014;20(7):1105–14. https://doi.org/10.3201/eid2007.131594.
Hlebowicz M, Jakubowski P, Smiatacz T. Streptococcus suis Meningitis: Epidemiology, clinical presentation and treatment. Vector-Borne Zoonotic Dis. 2019;19(8):557–62. https://doi.org/10.1089/vbz.2018.2399.
Watkins EJ, Brooksby P, Schweiger MS, Enright SM. Septicaemia in a pig-farm worker. Lancet. 2001;357(9249). https://doi.org/10.1016/s0140-6736(00)03570-4.
François B, Gissot V, Ploy MC, Vignon P. Recurrent septic shock due to Streptococcus suis. J Clin Microbiol. 1998;36(8):2395. https://doi.org/10.1128/jcm.36.8.2395-2395.1998.
Tsalta-Mladenov M, Dimitrova V, Georgieva D, Andonova S. Streptococcus Agalactiae Meningitis presented with cerebral infarction in adult patient– clinical case and review. Neurol India. 2022;70(5). https://doi.org/10.4103/0028-3886.359190.
Xing W, Zhang W, Zhu M, He J. Streptococcus suis meningitis complicated with acute cerebral infarction: a case report. Heliyon. 2022;8(8):e10418. https://doi.org/10.1016/j.heliyon.2022.e10418.
Dénes Á, Pradillo JM, Drake C, Sharp A, Warn P, Murray KN, Allan SM. Streptococcus pneumoniae worsens cerebral ischemia via interleukin 1 and platelet glycoprotein Ibα. Ann Neurol. 2014;75(5):670–83. https://doi.org/10.1002/ana.24146.
Chan O-W, Lin J-J, Hsia S-H, Lin C-Y, Lin K-L. Methylprednisolone pulse therapy as an adjuvant treatment of Streptococcus pneumoniae meningitis complicated by cerebral infarction—a case report and review of the literature. Child’s Nerv Syst. 2020;36(2):229–33. https://doi.org/10.1007/s00381-019-04485-6.
Zhu J, Tang J, Guo H, Zhuang Y, Tao K. Epidemiologic and pathogenic study on an outbreak of acute streptococcal disease in pigs. J Prev Med Chin People’s Liberation Army. 2000;04257–60. https://doi.org/10.13704/j.cnki.jyyx.2000.04.008.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Wenxin Wei (First Author): Investigation, Project administration, Writing - Original Draft; Zhenhu Qiao: Investigation, Writing - Original Draft; Donghua Qin: Supervision, Investigation; Yu Lan (Corresponding Author): Supervision, Writing - Review & Editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of Committee of Medical Ethics of the Minzu Hospital Affiliated of Guangxi Medical University and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors. Informed consent was obtained from all individual participants included in the study.
Consent to publish
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wei, W., Qiao, Z., Qin, D. et al. Acute multiple brain infarctions associated with Streptococcus suis infection: a case report. BMC Infect Dis 24, 447 (2024). https://doi.org/10.1186/s12879-024-09318-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09318-9