Abstract
Background
Actinomyces turicensis is rarely responsible of clinically relevant infections in human. Infection is often misdiagnosed as malignancy, tuberculosis, or nocardiosis, therefore delaying the correct identification and treatment. Here we report a case of a 55-year-old immunocompetent adult with brain abscess caused by A. turicensis. A systematic review of A. turicensis infections was performed.
Methods
A systematic review of the literature was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The databases MEDLINE, Embase, Web of Science, CINAHL, Clinicaltrials.gov and Canadian Agency for Drugs and Technology in Health (CADTH) were searched for all relevant literature.
Results
Search identified 47 eligible records, for a total of 67 patients. A. turicensis infection was most frequently reported in the anogenital area (n = 21), causing acute bacterial skin and skin structure infections (ABSSSI) including Fournier’s gangrene (n = 12), pulmonary infections (n = 8), gynecological infections (n = 6), cervicofacial district infections (n = 5), intrabdominal or breast infections (n = 8), urinary tract infections (n = 3), vertebral column infections (n = 2) central nervous system infections (n = 2), endocarditis (n = 1). Infections were mostly presenting as abscesses (n = 36), with or without concomitant bacteremia (n = 7). Fever and local signs of inflammation were present in over 60% of the cases. Treatment usually involved surgical drainage followed by antibiotic therapy (n = 51). Antimicrobial treatments most frequently included amoxicillin (+clavulanate), ampicillin/sulbactam, metronidazole or cephalosporins. Eighty-nine percent of the patients underwent a full recovery. Two fatal cases were reported.
Conclusions
To the best of our knowledge, we hereby present the first case of a brain abscess caused by A. turicensis and P. mirabilis. Brain involvement by A. turicensis is rare and may result from hematogenous spread or by dissemination of a contiguous infection. The infection might be difficult to diagnose and therefore treatment may be delayed. Nevertheless, the pathogen is often readily treatable. Diagnosis of actinomycosis is challenging and requires prompt microbiological identification. Surgical excision and drainage and antibiotic treatment usually allow for full recovery.
Similar content being viewed by others
Background
Actinomyces are filamentous Gram-positive anaerobic bacteria [1], generally found as commensals of the oropharynx and gastrointestinal or urogenital tracts [2]. Actinomycosis is a non-opportunistic and generally polymicrobial progressive granulomatous disease, characterized by subacute or chronic abscess formation, frequently misdiagnosed as malignancy, tuberculosis, or nocardiosis [1, 3]. It is characterized by tiny yellow clumps called sulfur granules, constituted by a biofilm of bacteria. These, together with necrosis and filamentous Gram-positive fungal-like bacteria, are the typical microscopic findings [3].
Actinomycosis generally involves the cervicofacial region (50%), the thoraco-pulmonary (30%) or the abdominopelvic tract (20%) [1]. The infection is acquired by minor trauma or aspiration rather than via hematogenous spread [4]. Actinomyces israelii is the most common species in human infections and in most clinical forms of actinomycosis, while A. turicensis is rarely responsible for clinically relevant infections in humans [3, 4].
The disease is generally readily treatable but often misdiagnosed [2]. The microbiological identification of the pathogen is mandatory, especially since the infection is often polymicrobial. In addition to culture, which takes at least 5 days and up to 15–20 days and could frequently result sterile, genotypic methods, such as comparative 16S ribosomal RNA (rRNA) gene sequencing and matrix-assisted laser desorption ionization time-of-flight (MALDI-TOF), are quicker and more accurate tools for Actinomyces identification. Actinomyces generally retain sensitivity to a wide spectrum of antimicrobials, including β-lactams, clarithromycin, erythromycin, doxycycline, and clindamycin. Long-term treatments are generally required, in addition to surgical debridement.
We report the case of a 55-year-old man with polymicrobial brain abscesses involving Actinomyces turicensis; to the best of our knowledge this is the first case in an adult patient with a history of previous alcohol abuse but no other reasons for immunosuppression. We also performed a systematic review of the literature, to summarize cases of infections due to A. turicensis. Because of the paucity of reports, we believe this work might be of interest to Infectious Diseases and Internal Medicine practitioners, to better understand the clinical presentations, diagnostic approach, and current treatment strategies of actinomycosis due to A. turicensis.
Case report
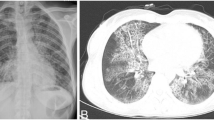
A 55-year-old man with a history of alcohol abuse and recurrent otitis was found on the ground and brought to the emergency room with confusion and seizures. On physical examination, he presented with hypotension and severe hypothermia. He had a Glasgow Coma Scale (GCS) of 8 and was intubated for airway protection. The initial laboratory analysis revealed an increase in inflammatory markers (white blood cell [WBC] count 22.570 /μL, C-reactive protein [CRP] 218 mg/L [reference range 0–5], procalcitonin [PCT] 8.16 ng/mL) and blood tests were compatible with signs of rhabdomyolysis (creatin kinase [CK] 1602 UI/L, creatinine 2.35 mg/dl, lactate dehydrogenase [LDH] 376 U/L, myoglobin 3075 ng/ml). Brain computed tomography (CT) was performed, which showed two brain lesions in the left temporal-occipital site, measuring 3.9 × 1.8 cm and 2.4 × 1.5 cm respectively, with vasogenic edema and 0.9 cm left-to-right midline shift. Signs of inflammation of the paranasal sinuses were also reported (Fig. 1).
Chest and abdominal CT scan were also performed in order to rule out local pathologies and possible septic embolisms. Blood cultures resulted negative and transthoracic echocardiogram showed no vegetations or signs of endocarditis. Serology for HIV and Toxoplasma gondii resulted negative. Antiedema (mannitol) and anticonvulsant (valproate) therapy was initiated along with empiric antibiotic treatment with ceftriaxone, 2 g every 12 hours, metronidazole, 500 mg every 6 hours, and linezolid 600 mg every 12 hours. The culture of the brain abscess aspirate, collected during neurosurgery, identified Actinomyces turicensis and Proteus mirabilis on two different samples. Specifically, an intraoperative sample was collected in Amies elution medium and cultivated on three agar plates (Sabouraud dextrose agar, Columbia CNA agar and MacConkey agar), while another sample was collected in the absence of medium and cultivated on the same plates plus two additional ones (Chocolate agar and microaerophilic Columbia CNA agar). The plates were incubated at 37° degrees and first bacterial growth was observed at 36 hours. Microbiological identification was performed by MALDI-TOF (Bruker Biotyper®), showing high log (score) value (2.17 and 1.97 for each sample respectively). The antimicrobial susceptibility testing was performed by microdilution and Vitek-2 (bioMerieux®) automated system respectively for the anaerobic and the aerobic bacteria (Table 1).
After obtaining the antimicrobial susceptibility test results, antibiotic therapy was simplified to ceftriaxone 2 g every 12 hours. Metronidazole and linezolid were discontinued.
After treatment optimization, the patient developed a fever and an initially vesiculopapular, then necrotizing, lesion of the upper lip and oral cavity (Fig. 2).
In the suspicion of a herpetic lesion, patient was started on acyclovir for 5 days, with progressive resolution of the lesion. To rule out a possible cutaneous involvement by A. turicensis, a wound swab was performed, resulting positive for Herpes simplex virus-1 (HSV-1) and a carbapenem-resistant Acinetobacter baumannii. Therefore, antimicrobial therapy was enhanced with the addition of ampicillin/sulbactam 3 g every 6 hours for improved coverage of both the brain abscess (A. turicensis) and the mucosal lesion isolate (A. baumannii). Five weeks after surgery, a brain magnetic resonance (MR) showed a reduction of the abscesses and resolution of edema and midline shift (Fig. 3).
The patient was then discharged to a neurorehabilitation facility with indication to continue the antimicrobial treatment with oral amoxicillin-clavulanate for a total of 8 weeks of therapy.
Systematic review
Materials and methods
The present study was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [5].
Search strategy and database selection
The search was conducted on the databases MEDLINE, EMBASE, Web of Science, CINAHL, Clinicaltrials.gov and Canadian Agency for Drugs and Technology in Health (CADTH), including all available records from inception to August 30th, 2023. Each included database was searched with the search term “Actinomyces turicensis” as an all-terms strategy. No filter was applied to the search engines. The search strategy as elaborated by the search engine, together with the corresponding records found divided by database is available in additional files (see Additional file 1).
Obtained records were merged on the online tool Rayyan, where duplicates were identified and removed from the included list. The first round of selection for relevance and eligibility was performed on the same platform [6]. Search and selection were performed in blind. Discrepancies in selection were resolved by discussion. A list of records obtained after the primary screening by title and abstract was then downloaded and entered into a computerized database for further analysis by reading the full text of the study. A final list of included records was then generated, and each study was examined for relevant data. Extracted information included author and journal information, year, study design, demographic information about included patient/s, site of infection, clinical presentation, diagnostic procedures, treatment, and outcome. Additional anamnestic information about possible predisposing conditions was also gathered. All extracted information was then summarized in figures and tables and added to the present study.
Inclusion and exclusion criteria
Records were identified as eligible if they reported clinical data about infections by A. turicensis. No restrictions were made in terms of study design, peer-review, year of publication, country, language, patient age, or type of patient. In vitro or animal studies were excluded. Records reporting aggregated data only were excluded as well.
Quality appraisal of included studies
Included studies were evaluated for their risk of bias by means of the most appropriate eligible reference scale when their design was either interventional or observational. For observational and randomized studies, the Newcastle-Ottawa scale (NOS) and the Cochrane Risk of Bias Tool 2 (ROB2) were used, respectively [7, 8]. The risk of bias analysis was performed, in blind, by AI, LVR and ADL. Discrepancies were solved by discussion.
Results
Our search on the six databases has identified 215 records, of which 103 were duplicates and were removed. Therefore, 112 records were screened for relevance and eligibility from the analysis of abstract and title only, resulting in 63 records. A subsequent examination of the relevant data in the full text was conducted, resulting in the exclusion of 16 records. At the end of the study selection process, 47 records were included in the systematic review. A flowchart describing the selection process is reported below (Fig. 4).
Included records were published between 2002 and 2023, with a prevalence in the last 5 years (26/47, 55%). Most of the studies were conducted in the USA (19/47, 40%), Europe (15/47, 32%) and China (3/47, 6%). Among the included records, we observed 43 Case reports, [1, 9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50] and 4 Case series [51,52,53,54], resulting in an overall population of 67 patients.
Clinical, demographics and microbiological records of the overall population are reported below (Tables 2 and 3).
Some of the included cases did not provide enough information about immunosuppression conditions, symptoms, or treatments; therefore, the lack of data was considered when calculating the incidences, to minimize underestimation of the data.
Demographic features and underlying conditions
Published cases showed an almost equal distribution of males and females (35 vs. 32) with a median age of 42 (IQR 23–57). From the analysis of the patient anamnestic data, 21 patients (21 out of the 52 patients for which data was available, i.e. 40%) resulted to have had some cause of comorbidity or immunosuppression, particularly smoking (9), diabetes (6), obesity (5), chemotherapy or immunotherapy (4), high dose steroids (3), alcohol abuse (3). Moreover, in relation to the site of infection, a supposed predisposing condition was reported in 27 patients (27/52, 52%). No information about predisposing condition or immunosuppression were reported for 15 patients.
Site of infection and associated symptoms
Among the overall population, we observed 21 infections of the anogenital district, 12 Acute Bacterial Skin and Skin Structure Infections (ABSSSI) of which 2 were defined as Fournier’s gangrene, 8 lung infections (4 empyema and 4 abscesses), 6 gynecological infections, 5 infections of the cervicofacial district, 4 infections of the breast, 4 abdominal infections (1 peritonitis, 2 liver abscesses, 1 infection of the adrenal gland), 3 urinary tract infections, 2 infections of the vertebral column, 2 central nervous system infections, 1 endocarditis. One patient had both the cervicofacial region and urinary tract infections. Interestingly, 36 (36/67, 54%) infections presented as abscesses and 7 infections (7/67, 19.4%) presented with a concomitant bacteremia. Among the symptoms described at admission, fever (25 out of the 42 patients for which such data were available, i.e. 60%), local pain (18/42, 43%), local swelling and erythema (8/42, 19%), vomiting (6/42, 1%), dysuria (4/42, 10%), were the most frequently reported. Furthermore, 7 patients (7/42, 17%) presented with hypotension or shock and 5 patients (5/42, 12%) presented with altered state of consciousness. In the case of 25 patients, no information about symptoms was reported.
Microbiology
In all cases where the data were available, the microbiological identification of A. turicensis was allowed by culture examination. This was conducted on tissue samples (31/62, 50%), purulent drainage fluid (14/62, 22.5%), intraoperative samples (6/62, 9,6%), blood samples (7/62, 11.2%), Broncho-Alveolar Lavage (BAL) fluid (2/62, 3.2%), cerebrospinal fluid (1/62, 1.6%), urine sample (1/62, 1.6%). Fifty-seven percent of the infections were polymicrobial (n = 38). Reported co-infections were identified by tissue/pus culture or molecular assays and are reported in Table 3. Co-infecting agents were almost invariably part of the anaerobic flora.
Treatment
Out of the 67 cases described in the literature, abscess drainage was performed in 10 patients (15%), surgical debridement was performed in 41 cases (61%), an antibiotic approach without surgery was chosen for 15 patients (22%), while no information about surgical procedures was reported for one patient. Surgery was considered curative, i.e. without any antibiotic therapy, in 8 out of 67 patients, though insufficient data was reported for the antibiotic treatment for 11 patients. Specifically, 4 received an unspecified broad-spectrum antibiotic regimen, while for 7 patients no data was reported.
In the other 48 cases, a wide range of antibiotic use was reported, as summarized in Table 4.
Broad-spectrum antibiotics, active on both Gram-positive and Gram-negative bacteria, were the most frequent first choice treatment, favoring intravenous administration in severe infections. Particularly, piperacillin/tazobactam was used in 7 patients, vancomycin was prescribed in 6 cases, carbapenems where the treatment of choice in 5 patients, while metronidazole or cephalosporin were used in 3 cases each. Regarding targeted therapy, the most frequently administered antibiotics were amoxicillin/clavulanate (n.17 cases), amoxicillin (n.13 cases), ampicillin/sulbactam (n.6 cases), penicillin (n. 6 cases) and ampicillin (n. 4 cases). Metronidazole (n.15 cases) or cephalosporin (n.6 cases) were added in case of suspected or documented polymicrobial infections.
Regarding the overall duration of therapy, data were available for 46 out of 67 patients. Mean treatment duration was 80 days, while median duration was 38.5 days (IQR 7.5–172.5). Shorter treatment, i.e. less than 1 month, was the most frequently observed (14/46, 30%), followed by a duration of 1–3 months (10/46, 22%), 3–6 months (8/46, 17%) and more than 6 months (6/46, 13%). The remaining cases underwent no antimicrobial therapy as surgery was considered curative (8/46, 17%). As expected, longer treatments were reported in cases of abscesses.
Outcome
Among the included studies, clinical outcome data were available for 44 out of 67 cases (65.6%). Thirty-nine patients (89%) showed a full recovery, while 3 patients (7%) experienced recurrence or superinfection and 2 patients (5%) died.
Discussion and conclusions
To the best of our knowledge, this is the first case in the literature of a brain abscess caused by A. turicensis and P. mirabilis in an adult patient. Brain involvement in actinomycosis is uncommon [57, 58], generally resulting from hematogenous spread or contiguous infection of the ear, sinus, and cervicofacial region [46, 58, 59]. In our case, the brain CT showed inflammation of the paranal sinuses but excluded ear involvement, even if a history of frequent otitis was reported.
Brain abscesses caused by opportunistic pathogens are frequently in patient with Human Immunodeficiency virus (HIV) infection or other causes of immunosuppression, whereas bacteria are the most common cause in immunocompetent patients [60]. While actinomycosis is a non-opportunistic disease, central nervous system involvement is very rare. Therefore, possible causes of immunosuppression must always be excluded. Our patient had a history of alcohol abuse [61, 62], which is considered a pro-inflammatory and nutritionally impaired condition often associated with immune deficiency.
The diagnosis of actinomycosis is challenging and requires an invasive approach for diagnosis. Literature suggests a surgical intervention for any brain abscess measuring at least 2.5 cm in diameter [63, 64]. Our patient underwent surgical excision of abscesses with consequent microbiological identification. Brain abscesses are frequently polymicrobial [46, 65, 66]; indeed P. mirabilis was also identified in our case [66].
Furthermore, growth of Actinomyces is generally slow and the bacteriological identification is difficult. Culture could frequently result sterile due to previous antibiotic therapy, concomitant microorganisms and inadequate sampling or incubation conditions. Surgical sampling of biopsy or pus seems to be the most appropriate clinical specimen [3].
Although often difficult to diagnose, actinomycosis is generally readily treatable, showing susceptibility to many antimicrobials including β-lactams, clarithromycin, erythromycin, doxycycline, and clindamycin. Therefore, thanks to the wide susceptibility and availability of treatment, several are the drugs of choice and there is no univocal indication. However, penicillin G or amoxicillin are the most used [3].
In our case, ceftriaxone was considered as target therapy with addiction to ampicillin/sulbactam for a week, as strengthening of the brain abscesses treatment. The prompt clinical and laboratory response in our patient allowed the switch to oral therapy with amoxicillin-clavulanic acid, which has proven to be non-inferior to standard intravenous treatment [67].
Our systematic review of the literature identified 47 articles reporting infections caused by A. turicensis. All included records are case reports (43) and case series (4), with an increased number of published papers in the last 20 years, probably due to the improvement of microbiological techniques, spectrometry, and molecular assay, that allow to better identification of Actinomyces species. Since the diagnosis of actinomycosis requires bacteriological identification, a lack of correct microbiological data, in the past, may have led to a misinterpretation of the risk and an underestimate of the incidence.
Although A. israelii is the main cause of disease within the species [4], we identified 67 cases of infections due to A. turicensis. From the present literature revision, most A. turicensis cases were anogenital, gynecological and urinary tract infections (30), lung infections (8) or cervicofacial infections (5).
As reported in the literature, actinomycosis is generally due to local dissemination of the pathogen rather than hematogenous spread [4]. Among the analyzed articles, a concomitant bacteremia was indeed found in 10% (7/67) of cases only, while a predisposing condition of local dissemination was supposed in at least 40% (27/52) of cases. Notably, while actinomycosis is a non-opportunistic disease, a reason for immune system impairment has been found in at least 52% (21/52%) of the cases.
Interestingly, only two central nervous system infections were reported among the included records, both presenting a history of ear infections (i.e. mastoiditis and otitis). In our cases, although a previous history of recurrent otitis was reported, no acute ear infection was present at patient admission. Concerning treatment options and outcome, a wide range of therapies is reported and a relatively low mortality (5%), confirming to be a readily treatable infection when promptly diagnosed [2].
In 76% of cases drainage or surgical debridement was performed, representing not only a therapeutical approach but also as a diagnostic procedure.
In conclusion, diagnosis of actinomycosis is challenging and requires prompt microbiological identification. Surgical excision or drainage together with long-term antibiotics is essential to achieve clinical recovery. Further investigations are needed to assess the optimal antibiotic regimen and its duration.
Availability of data and materials
All data generated or analyzed during this study are included in this article and its supplementary materials.
Abbreviations
- ABSSSI:
-
Acute bacterial skin and skin structure infection
- AMC:
-
Amoxicillin/clavulanic acid
- AMP:
-
Ampicillin
- AMX:
-
Amoxicillin
- BAL:
-
Broncho alveolar lavage
- CADTH:
-
Canadian agency for drugs and technology in health
- CARBA:
-
Carbapenem
- CFP:
-
Cefoperazone
- CIP:
-
Ciprofloxacin
- CK:
-
Creatine Kinase
- CLI:
-
Clindamycin
- CRO:
-
Ceftriaxone
- CRP:
-
C Reactive Protein
- CT:
-
Computed tomography
- CTX:
-
Cefotaxime
- CXM:
-
Cefuroxime
- DAP:
-
Daptomycin
- GEN:
-
Gentamicin
- HIV:
-
Human immunodeficiency virus
- HSV:
-
Herpes Simplex Virus
- IQR:
-
InterQuartile Range
- LDH:
-
Lactate dehydrogenase
- LVX:
-
Levofloxacin
- LZD:
-
Linezolid
- MALDI-TOF:
-
Matrix assisted laser desorption ionization – time of flight
- MIC:
-
Minimum inhibitory concentration
- MR:
-
Magnetic resonance
- MTZ:
-
Metronidazole
- N.A.:
-
Not Available
- NOS:
-
Newcastle-ottawa scale
- GCS:
-
Glasgow coma scale
- PCT:
-
Procalcitonin
- PEN:
-
Penicillin
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- RIF:
-
Rifampin
- S:
-
Sentitive
- SAM:
-
Ampicillin/sulbactam
- STX:
-
Trimethoprim/sulfamethoxazole
- R:
-
Resistant
- TZP:
-
piperacilline/tazobactam
- VAN:
-
Vancomycin
References
Tabaksert A, Kumar R, Raviprakash V, Srinivasan R. Actinomyces turicensis parapharyngeal space infection in an immunocompetent host: first case report and review of literature. Access Microbiol. 2021;3:000241.
Wong VK, Turmezei TD, Weston VC. Actinomycosis. BMJ. 2011;343:d6099.
Valour F, Sénéchal A, Dupieux C, Karsenty J, Lustig S, Breton P, et al. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist. 2014;7:183–97.
Olson TS, Seid AB, Pransky SM. Actinomycosis of the middle ear. Int J Pediatr Otorhinolaryngol. 1989;17:51–5.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 Statement: an updated guideline for reporting systematic reviews. BMJ. 2021;n71.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019:l4898.
Lo CK-L, Mertz D, Loeb M. Newcastle-Ottawa scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45.
Panwar K, Duane TM, Tessier JM, Patel K, Sanders JM. Actinomyces turicensis necrotizing soft-tissue infection of the thigh in a diabetic male. Surg Infect. 2019;20:431–3.
Alaq Al-Abayechi, MD1, Divya Chandramohan, MD2, Hasan Baher, MD1, James Saca, MD1. RARE PATHOGENS ENCOUNTERED IN MAGGOT-INFESTED FOOT WOUNDS. Abstract published at SHM Converge 2023. Abstract 458 Journal of Hospital Medicine.
Unigarro L, Marín K, Alvear C, Salgado J, Basantes E. Choque séptico por Actinomyces turicensis, asociado a cáncer de cérvix. Reporte de caso. Mexican J Oncol. 2023;22:128–32.
Baher H, Jones L, Al-Abayechi A, Peters JI. A rare case of actinomyces turicensis empyema in an iv drug user. Chest. 2022;162:A1378.
Gandhi K, van der Woerd BD, Graham ME, Barton M, Strychowsky JE. Cervicofacial Actinomycosis in the pediatric population: presentation and management. Ann Otol Rhinol Laryngol. 2022;131:312–21.
Fisher M, Soller D, Khaskia Y, Schellenberg J. Double rarity: a CASE of ACTINOMYCES in pulmonary sequestration. CHEST. 2021;160:A1713.
Lin Jinming XB, Zhu Q, Xu ZY, Chen Q. A case of multiple sinuses in the buttocks caused by Actinomyces turicensis. Chin J Dermatol. 2021;54:155–7. https://doi.org/10.35541/cjd.20190779.
JCDR - Actinomycetaceae, Bacteremia, Kidney disorder https://www.jcdr.net/article_fulltext.asp?issn=0973-709x&year=2020&month=June&volume=14&issue=6&page=DD01&id=13734. Accessed 8 Sep 2023.
Herrmann AA, Othman SI, DeFoe KM, Carolan EJ, Rosenbloom MH. Spinal epidural abscess: esophageal fistula as a potential infection source. Interdiscip Neurosurg. 2019;16:42–3.
Lowry D, Grossman C, Boakye-Wenzel HN, Warren M, Dy RV. An Atypical case of waxing and waning lung lesions due to Actinomyces. In: D57. Atypical pneumonias and other infections. American Thoracic Society; 2019. p. A6827–A6827.
Pyometra. Consultant360. 2018. https://www.consultant360.com/article/consultant360/womens-health/pyometra. Accessed 8 Sep 2023.
Snead JA, Ruggiero N, Sangha R, Joseph L, Mukherji R. Actinomyces turicensis bacteremia secondary to a decubitus ulcer: a case report and review of the literature. Infect Dis Clin Pract. 2018;26:e16.
Gibson AL, Liu S, Naifeh M. Actinomyces epidural abscess: a virtually unheard of process in the virtual age. United States, New Orleans, LA: J. Invest. Med; 2018. p. 487–8.
Elborno D, Pandya L, Chor J. Case report: pelvic Actinomyces in an adolescent with microperforate hymen. J Pediatr Adolesc Gynecol. 2016;29:191.
Matela A, Ali Z, Changawala N, Desai A, Musta A, Nair GB. An unusual case of Actinomyces Turicensis pulmonary infection presenting as a lung mass. In: A48. Pulmonary infections: CASE studies (bacterial). American Thoracic Society; 2015. p. A1840–A1840.
Abstracts from the 37th annual meeting of the Society of General Internal Medicine. J Gen Intern Med. 2014;29:1–545.
Shkolnik I, Hassani A, Miceli M, Big C, Bagdasarian N. A unique case of Actinomyces turicensis pulmonary abscess. Infect Dis Clin Pract. 2014;22:e37.
Palacios D, Wallace HC. Recurrent Peri-clitoral abscess with positive Actinomyces turicensis culture. Case Rep Obstet Gynecol. 2023;2023:9912910.
Doldán L, Huarachi-Chirilla Y, Vargas C, Domínguez C, Chediack V, Cunto E. Cervical carcinoma abscessed by Schaalia turicensis. Medicina (B Aires). 2023;83:341.
Cronin JT, Richards BW, Skedros JG. Schaalia (formerly Actinomyces) turicensis infection following open rotator cuff repair. Cureus. 2023;15:e34242.
Khan A, Gidda H, Murphy N, Alshanqeeti S, Singh I, Wasay A, et al. An Unusual Bacterial Etiology of Fournier’s Gangrene in an Immunocompetent Patient. Cureus. 2022;14:e26616.
Mao T, Zhou X, Tian M, Zhang Y, Wang S. A rare case of male Fournier’s gangrene with mixed Actinomyces turicensis infection. BMC Urol. 2022;22:25.
Nia A, Ungersboeck A, Uffmann M, Leaper D, Assadian O. Septic hip abscess due to Fusobacterium nucleatum and Actinomyces turicensis in an immunocompetent SARS-CoV-2 positive patient. Anaerobe. 2021;71:102420.
Agrafiotis AC, Lardinois I. Pleural empyema caused by Actinomyces turicensis. New Microbes New Infect. 2021;41:100892.
Johnson SW, Billatos E. Polymicrobial empyema; a novel case of Actinomyces turicensis. Respir Med Case Rep. 2021;32:101365.
Barnes A, Kaur A, Augenbraun M. An unusual presentation of prostatic abscess due to Actinomyces turicensis and Peptostreptococcus. Cureus. 2020;12:e8665.
Jin W, Miao Q, Wang M, Zhang Y, Ma Y, Huang Y, et al. A rare case of adrenal gland abscess due to anaerobes detected by metagenomic next-generation sequencing. Ann Transl Med. 2020;8:247.
Kansara T, Majmundar M, Doshi R, Ghosh K, Saeed M. A case of life-threatening Actinomyces turicensis bacteremia. Cureus. 2020;12:e6761.
Le Bihan A, Ahmed F, O’Driscoll J. An uncommon cause for a breast abscess: Actinomyces turicensis with Peptoniphilus harei. BMJ Case Rep. 2019;12:e231194.
Vassa N, Mubarik A, Patel D, Muddassir S. Actinomyces turicensis: an unusual cause of cervicofacial actinomycosis presenting as ludwig angina in an immunocompromised host - case report and literature review. IDCases. 2019;18:e00636.
Kocsis B, Tiszlavicz Z, Jakab G, Brassay R, Orbán M, Sárkány Á, et al. Case report of Actinomyces turicensis meningitis as a complication of purulent mastoiditis. BMC Infect Dis. 2018;18:686.
Cobo F. Breast abscess due to Actinomyces turicensis in a non-puerperal woman. Enferm Infecc Microbiol Clin (Engl Ed). 2018;36:388–9.
Gatti M, Gasparini LE, Grimaldi CM, Abbati D, Clemente S, Brioschi PR, et al. Septic shock due to NSTI caused by Actinomyces Turicensis: the role of clinical pharmacology. Case report and review of the literature. J Chemother. 2017;29:372–5.
Eenhuis LL, de Lange ME, Samson AD, Busch ORC. Spontaneous bacterial peritonitis due to Actinomyces mimicking a perforation of the proximal jejunum. Am J Case Rep. 2016;17:616–20.
Oh HB, Abdul Malik MH, Keh CHL. Pilonidal abscess associated with primary Actinomycosis. Ann Coloproctol. 2015;31:243–5.
Hagiya H, Ogawa H, Takahashi Y, Kimura K, Hasegawa K, Otsuka F. Actinomyces turicensis bacteremia secondary to Pyometra. Intern Med. 2015;54:2775–7.
Kottam A, Kaur R, Bhandare D, Zmily H, Bheemreddy S, Brar H, et al. Actinomycotic endocarditis of the eustachian valve: a rare case and a review of the literature. Tex Heart Inst J. 2015;42:44–9.
Miller S, Walls T, Atkinson N, Zaleta S. A case of otitis media complicated by intracranial infection with Actinomyces turicensis. JMM Case Rep. 2014;1:e004408.
Abdulrahman GO, Gateley CA. Primary actinomycosis of the breast caused by Actinomyces turicensis with associated Peptoniphilus harei. Breast Dis. 2015;35:45–7.
Ong C, Barnes S, Senanayake S. Actinomyces turicensis infection mimicking ovarian tumour. Singap Med J. 2012;53:e9-11.
Zautner AE, Schmitz S, Aepinus C, Schmialek A, Podbielski A. Subcutaneous fistulae in a patient with femoral hypoplasia due to Actinomyces europaeus and Actinomyces turicensis. Infection. 2009;37:289–91.
Riegert-Johnson DL, Sandhu N, Rajkumar SV, Patel R. Thrombotic thrombocytopenic purpura associated with a hepatic abscess due to Actinomyces turicensis. Clin Infect Dis. 2002;35:636–7.
Tan CY, Javed MA, Artioukh DY. Emerging presence of Actinomyces in perianal and pilonidal infection. J Surg Case Rep. 2022;2022:rjac367.
Chudácková E, Geigerová L, Hrabák J, Bergerová T, Liska V, Scharfen J. Seven isolates of Actinomyces turicensis from patients with surgical infections of the anogenital area in a Czech hospital. J Clin Microbiol. 2010;48:2660–1.
Attar KH, Waghorn D, Lyons M, Cunnick G. Rare species of actinomyces as causative pathogens in breast abscess. Breast J. 2007;13:501–5.
Böttger S, Zechel-Gran S, Schmermund D, Streckbein P, Wilbrand J-F, Knitschke M, et al. Odontogenic Cervicofacial necrotizing fasciitis: microbiological characterization and Management of Four Clinical Cases. Pathogens. 2022;11:78.
Sarumathi D, Gopichand P, Sejpal K, Priyamvada P, Mandal J. Actinomyces turicensis causing urinary tract infection in nephrotic syndrome patient- a case report. JCDR. 2020; https://doi.org/10.7860/JCDR/2020/44091.13734.
Nickoloff S, Sharma A, Martin J. An uncommon presentation of a rare pathogen: considering the cause of prolonged hiccups. San Diego, CA, United States: Journal of General Internal Medicine; 2014. p. S309–10.
Rahiminejad M, Hasegawa H, Papadopoulos M, MacKinnon A. Actinomycotic brain abscess. BJR Case Rep. 2016;2:20150370.
Perez A, Syngal G, Fathima S, Sandkovsky U. Actinomyces causing a brain abscess. Proc (Bayl Univ Med Cent). 2021;34:698–700.
Smego RA Jr. Actinomycosis of the central nervous system. Rev Infect Dis. 1987;9:855–65.
Sonneville R, Ruimy R, Benzonana N, Riffaud L, Carsin A, Tadié J-M, et al. An update on bacterial brain abscess in immunocompetent patients. Clin Microbiol Infect. 2017;23:614–20.
Watzl B, Watson RR. Role of alcohol abuse in nutritional immunosuppression. J Nutr. 1992;122(3 Suppl):733–7.
Zhang P, Bagby GJ, Happel KI, Raasch CE, Nelson S. Alcohol abuse, immunosuppression, and pulmonary infection. Curr Drug Abuse Rev. 2008;1:56–67.
Kameda-Smith MM, Ragulojan M, Hart S, Duda TR, MacLean MA, Chainey J, et al. A Canadian National Survey of the neurosurgical management of intracranial abscesses. Can J Neurol Sci. 2022;1–8.
Mamelak AN, Mampalam TJ, Obana WG, Rosenblum ML. Improved management of multiple brain abscesses: a combined surgical and medical approach. Neurosurgery. 1995;36:76–85 discussion 85–86.
Abo-Zed A, Yassin M, Phan T. A rare case of polymicrobial brain abscess involving Actinomyces. Radiol Case Rep. 2021;16:1123–6.
Muddassir R, Khalil A, Singh R, Taj S, Khalid Z. Intracranial Abscess and Proteus mirabilis: A Case Report and Literature Review. Cureus. 2020;12:e12326.
Bodilsen J, Brouwer MC, van de Beek D, Tattevin P, Tong S, Naucler P, et al. Partial Oral antibiotic treatment for bacterial brain abscess: an open-label randomized non-inferiority trial (ORAL). Trials. 2021;22:796.
Acknowledgements
Not applicable.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Study was designed by AI and LVR. LVR, AI, and ADL performed all phases of the systematic review. Data extraction was performed by LVR and AI. Extracted data was checked by ADL, MI, LS and VM. Microbiological data were provided and controlled by AA, CDA, SM and MCB. DGB, MD and IG and all other authors were involved in patient care, and substantially contributed to the production of the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
A written informed consent was obtained from the patient described in the case report for publication of both clinical information, pictures, and radiological scans.
Competing interests
LS received a research grant from Gilead and fee for lectures and expertise from Merck, Gilead, Pfizer. MA reports honoraria for lectures and research grants from Merk, Gilead, Abbvie, Angelini SpA. V.M. received honoraria for lectures from Janssen-Cilag. M.I. received honoraria for lectures from Biogen Italia, AIM Educational, MICOM srl and research grants from Gilead.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Imeneo, A., Rindi, L.V., Di Lorenzo, A. et al. Brain abscess caused by Actinomyces turicensis in a non-immunocompromised adult patient: a case report and systematic review of the literature. BMC Infect Dis 24, 109 (2024). https://doi.org/10.1186/s12879-024-08995-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-08995-w