Abstract
Background
Urinary tract infection (UTI) is considered one of the most prevalent infections that may lead to many renal complications. They account for almost 10% of all infections in Saudi Arabia, making them the second most common cause of emergency department admissions. Bacterial pathogens, primarily Escherichia coli, Klebsiella spp., Enterococcus spp., Proteus spp., and Staphylococcus spp. are the most causative agents of UTI. This study aims to evaluate the prevalence and antimicrobial susceptibility patterns of uropathogens in adult patients from Madinah, Saudi Arabia.
Methods
A retrospective cross-sectional study was performed using data collected from patients who visited King Fahad General Hospital in Madinah, Saudi Arabia. Data included 16,803 urine bacterial cultures and their antimicrobial susceptibility profiles collected between January 2019 and October 2021.
Results
Among the 16,803 tested samples, 3937 (23.4%) showed positive results for urine bacterial cultures. UTI prevalence was slightly higher in women (52.1%) than men (47.9%). Escherichia coli (29.8%) was the most prevalent, followed by Klebsiella spp. (23.2%) and Pseudomonas spp. (8.4%). As for Gram-positive bacteria, Enterococcus spp. (10.8%) were most common, followed by Streptococcus spp. (8%) and Staphylococcus spp. (3.3%). Gram-negative bacteria exhibited high resistance rates toward aztreonam (> 83.3%), ampicillin (78.8%), and cephalexin (68.5%). Enterococcus spp. displayed elevated resistance rates (> 62.3%) against ciprofloxacin, gentamicin, and tetracycline. Conversely, Streptococcus spp. showed substantial resistance rates (> 76.6%) toward colistin and trimethoprim/sulfamethoxazole.
Conclusion
To optimize therapy and minimize the risk of multidrug-resistant uropathogenic infections, physicians should consider the local epidemiological trends and antimicrobial resistance patterns of prevalent uropathogens prior to initiating any empirical antibacterial therapy.
Similar content being viewed by others
Background
Urinary tract infection (UTI) is one of the most prevalent and serious infections worldwide, with more than 150 million new cases reported each year [1]. In Saudi Arabia, UTI represents almost 10% of all infection cases, which makes it the second most common cause of emergency admission [2]. It affects the urinary tract and prostate, causing significant complications and major health problems such as urinary tract dysfunction, bacterial septicemia, or even prominent kidney damage [3, 4].
UTI is an inflammation of the urinary tract caused by abnormal colonization of harmful microorganisms [5]. Normally, the urinary tract is free from any microorganisms, as it resists long-term colonization via different mechanisms. The protective mechanisms can be either mechanical (e.g., bladder emptying during micturition that washes off any residing microorganism) or physiological (e.g., host immunity, mucus production, and increased urea production) [6]. However, the inflammation disrupts the normal urinary tract function, which leads to incomplete microorganism clearance and eventually UTI development [6]. Nevertheless, acquiring the infection depends on several risk factors such as age, sex, period of hospitalization, pregnancy, diabetes, usage of urinary catheters, and genitourinary tract or immune system abnormalities [5, 7,8,9]. UTI can be either symptomatic (e.g., burning sensation during urination, fever, dysuria, and lower abdominal pain) or asymptomatic [5].
The type of UTI usually depends on the source of infection. For instance, community-acquired infection in healthy individuals is typically caused by rectal flora contamination via bacterial ascension to the urethra [10]. This type of infection is more common in women than in men owing to their genitourinary structures [11]. In contrast, nosocomial infection usually develops 48 h or later in hospitalized patients. Prosthetic devices such as urinary catheters also contribute to the occurrence of UTI in patients with nosocomial infection [12].
Several microorganisms are commonly involved in UTI, including bacteria, fungi, and viruses. However, bacteria are the most common causative agents for such an infection [1]. According to the literature and previous reports, Gram-negative bacteria account for nearly 90% of all UTI cases, while Gram-positive bacteria are responsible for only 10%. The most frequently identified uropathogen is Escherichia coli. However, other uropathogens, including Klebsiella spp., Staphylococcus spp., Streptococcus spp., Proteus spp., and Pseudomonas spp., may also be involved in UTI development [13,14,15,16,17,18].
The prevalence of uropathogens has been well established worldwide [5]. Nevertheless, the common uropathogen can be largely dependent on the geographical location. Each geographical region may exhibit a different pattern of uropathogens [19]. For example, more isolated regions or communities tend to share similar uropathogens when compared with multicultural or overlapped societies. Similarly, antimicrobial susceptibility patterns may vary among regions depending on public awareness and antibiotic usage [19]. This divergence underscores the challenge of handling uropathogens that exhibit resistance to important antibiotics, such as ß-lactams, aminoglycosides, polyketide, fluoroquinolones, sulfonamides and carbapenems [20,21,22,23]. This scenario places a substantial burden on healthcare, particularly when determining empirical therapy before urine culture outcomes are known. Consequently, comprehending the prevalence of UTI antimicrobial resistance becomes pivotal in guiding antibiotic choices for both empirical and precise therapeutic strategies.
In the current study, we investigated the prevalence of uropathogens in Madinah, Saudi Arabia. Madinah City is a well-known multicultural city that is visited by approximately 6–8 million Muslims from all over the world every year [24]. Thus, it is important to evaluate the prevalence and antimicrobial susceptibly trends of uropathogens, which could play a crucial role in determining the optimal empirical antibacterial therapy.
Methods
Sample collection and exclusion criteria
This retrospective cross-sectional study was performed using data collected from patients who visited King Fahad General Hospital in Madinah, Saudi Arabia, between January 2019 and October 2021. The collected data included both bacterial culture and antimicrobial susceptibility testing (AST) results from 16,803 patients suspected to have UTI. The study included all patients aged 18 years or older with suspected UTI. The urine sample culture was considered positive when bacterial counts exceeded 105 CFU/mL, and the data from patients with positive results were included in the study. Meanwhile, all data collected from patients with urinary catheters or negative results (bacterial counts fewer than 105 CFU/mL) were excluded.
Bacterial culture, identification, and antimicrobial susceptibility testing
The samples were cultured on Cystine Lactose Electrolyte deficient (CLED) agar media (BD, USA) and incubated overnight at 37 °C. The bacterial isolates were initially identified based on the microbiology department protocol implemented in the hospital which included performing Gram staining and biochemical tests such as indole production, citrate utilization, urease test, and oxidase test for Gram-negative isolates while Gram-positive cocci were identified using catalase and coagulase tests. All isolates were also confirmed using different automated identification systems, including VITEK 2 (bioMérieux, USA) or Phoenix (BD, USA) chosen based on reagents availability. The AST was also performed using these systems according to the manufacturer’s protocol. This test covers up to 22 antibiotics including Amoxicillin + Clavulanic Acid, Amikacin, Ampicillin, Aztreonam, Ceftazidime, Cephalexin, Ciprofloxacin, Colistin, Cefuroxime, Cefazolin, Cefepime, Cefoxitin, Gentamicin, Imipenem, Levofloxacin, Meropenem, Nitroxoline, Trimethoprim/Sulfamethoxazole, Tigecycline, Piperacillin + Tazobactam for Gram-negative bacteria. While for Gram-positive bacteria the following antibiotics were used; Amoxicillin + Clavulanic Acid, Amikacin, Ampicillin, Aztreonam, Ceftazidime, Cephalexin, Ciprofloxacin, Colistin, Ceftriaxone, Cefotaxime, Cefuroxime, Cefazolin, Cefepime, Cefoxitin, Gentamicin, Imipenem, Levofloxacin, Meropenem, Nitroxoline, Norfloxacin, Trimethoprim/Sulfamethoxazole, Tigecycline, Piperacillin + Tazobactam, Penicillin, Erythromycin, Vancomycin, Oxacillin, High Gentamicin, Linezolid. The results were represented as sensitive, intermediate, or resistant and extracted automatically.
Statistical analysis
Data were presented as numbers and percentages. All data were analyzed using GraphPad Prism v. 9.0 software (San Diego, USA).
Results
Number of positive cases and distribution of demographic data
Between January 2019 and October 2021, a total of 16,803 urine samples were sent for bacterial identification. These samples were collected from different hospital wards. A total of 3937 (23.4%) positive urine bacterial cultures were confirmed using VITEK 2 and Phoenix. The number of positive UTI cases was slightly higher in women (n = 2051; 52.1%) than in men (n = 1886; 47.9%) (Table 1). Saudi nationals showed the highest prevalence of positive cultures (n = 2959; 75.1%), while the remaining were non-Saudi patients (n = 978; 24.9%) (Table 1).
Distribution of the etiological agents of UTI
Gram-negative bacteria were the most prevalent isolated group (n = 2998; 76.14%), while Gram-positive bacteria accounted for 22.7% of the cases (n = 894). The Enterobacterales family was the most frequently identified uropathogen (n = 2496; 63.4%). Among this family, Escherichia spp. were the most prevalent species (n = 1173; 29.8%), followed by Klebsiella spp. (n = 914; 23.2%). Meanwhile, Enterococcus spp. were the most prevalent Gram-positive bacteria (n = 426; 10.8%), followed by Streptococcus spp. (n = 315; 8%) (Fig. 1; Table 2).
A total of 16 bacterial genera represented by 75 bacterial species were successfully isolated from the positive cultures (Fig. 1; Table 2). E. coli was the most predominant species within its genus (n = 1172; 99.9%) (Fig. 2A), while Klebsiella pneumoniae was the most commonly identified isolate among its genus (n = 890; 97.4%) (Fig. 2B). Pseudomonas aeruginosa and Proteus mirabilis were the most prevalent among their genera (n = 323; 98.2% and n = 193; 92%, respectively) (Fig. 2C and D). Meanwhile, Enterococcus faecalis, Streptococcus agalactiae, and Staphylococcus aureus were the most frequently identified isolates among their genera (n = 301; 70.7%, n = 269; 85.4%, and n = 103; 79.2%, respectively) (Fig. 2E–G).
Prevalence of antimicrobial resistance among the identified uropathogens
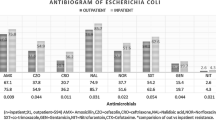
The AST data for the most prevalent bacterial genera/species E. coli, Klebsiella spp., Proteus spp., Pseudomonas spp., Acinetobacter spp., Enterococcus spp., Streptococcus spp., and Staphylococcus spp. were included (Fig. 3; Table 3). E. coli showed high resistance rates (> 50%) to ampicillin, aztreonam, cephalexin, ciprofloxacin, cefazolin, cefepime, levofloxacin, and trimethoprim/sulfamethoxazole. In contrast, E. coli was highly sensitive (> 88%) to imipenem, meropenem, and amikacin (Fig. 3A and Table 3).
Antimicrobial sensitivity pattern of the most prevalent uropathogens. A; Escherichia spp., B; Klebsiella spp., C; Proteus spp., and D; Pseudomonas spp., E; Acinetobacter spp., F; Enterococcus spp., G; Streptococcus spp., and H; Staphylococcus spp. R; Resistant, I; Intermediate, S; Sensitive, AMC; Amoxicillin + Clavulanic acid, AMK; Amikacin, AMP; Ampicillin, ATM; Aztreonam, CAZ; Ceftazidime, CEP; Cephalexin, CIP; Ciprofloxacin, COL; Colistin, CRO; Ceftriaxone, CLI; Clindamycin, CTX; Cefotaxime, CXM; Cefuroxime, CZO; Cefazolin, FEP; Cefepime, E; Erythromycin, FOX; Cefoxitin, GEH; High Gentamicin, GEN; Gentamicin, IPM; Imipenem, LNZ; Linezolid, LVX; Levofloxacin, MEM; Meropenem, NIT; Nitroxoline, NOR; Norfloxacin, OXA; Oxacillin, PEN; Penicillin G, SXT; Trimethoprim/sulfamethoxazole, TCY; Tetracycline, TGC; Tigecycline, TZP; Piperacillin + tazobactam, VAN; Vancomycin
Klebsiella spp., including the most isolated K. pneumoniae, showed high resistance rates (≥ 60%) to most of the tested antibiotics. In particular, the resistance rates to ampicillin and aztreonam were > 89%. In contrast, Klebsiella spp. demonstrated high sensitivity rates (> 55%) to colistin and gentamicin (Fig. 3B; Table 3). A similar pattern of antibiotic resistance (resistance rate of approximately ≥ 50%) was seen in Proteus spp., but the sensitivity rate to meropenem was relatively high (80.3%). In contrast to Klebsiella spp., Proteus spp. showed high resistance rates (98%) to nitroxoline and tigecycline (Fig. 3C; Table 3). Amikacin and meropenem were the most effective antibiotics against Proteus spp. at sensitivity rates of 80.3% and 73.8%, respectively. Pseudomonas spp. were almost 50% sensitive to 7 of 10 antibiotics and 60.2% resistant to imipenem (Fig. 3D; Table 3). In contrast, Acinetobacter spp. showed the highest resistance rates (> 55%) among all identified bacteria; colistin was the only effective antibiotic at a sensitivity rate of 100% (Fig. 3E; Table 3).
Among the Gram-positive bacteria, Enterococcus spp. were the most predominantly identified genera in 426 samples (10.8%). They demonstrated sensitivity rates of > 73% to ampicillin, linezolid, nitroxoline, and vancomycin (Fig. 3F; Table 3) and resistance rates of > 62% to ciprofloxacin, gentamicin, and tetracycline. Streptococcus spp. and Staphylococcus spp. were isolated from 315 (8%) and 130 (3.3%) samples, respectively. Streptococcus spp. showed sensitivity rates of > 85% to Augmentin, ampicillin, cephalexin, and penicillin, while Staphylococcus spp. demonstrated resistance rates of ≥ 50% to the same antibiotics (Fig. 3G and H; Table 3). Meanwhile, Staphylococcus spp. showed higher sensitivity rates to colistin and trimethoprim/sulfamethoxazole than did Streptococcus spp. However, nitroxoline was effective against both genera at a resistance rate of < 3.8%.
Discussion
This retrospective study was conducted to determine the prevalence, etiology, and antimicrobial susceptibility patterns of uropathogens isolated from patients who visited King Fahad General Hospital in Madinah, Saudi Arabia, between January 2019 and October 2021.
Herein, nearly one-quarter of all culture samples were positive for certain bacteria. The prevalence of positive cultures in our study was 23.4%, consistent with that in other studies conducted in Saudi Arabia and Iraq [25, 26]. In Hai’l, Saudi Arabia, and Baghdad and Erbil, Iraq, the prevalence has been demonstrated to be 19.6% [25] and 26.58% and 22%, respectively [26]. However, conflicting findings regarding the prevalence of UTI have also been reported [27, 28]. For instance, a high prevalence rate (32.3%) was documented in a study conducted at different hospitals in Uganda [5]. Another study conducted in Italy reported that 541 of 1745 (31%) urine samples showed positive bacterial cultures [29]. Meanwhile, lower prevalence rates (< 9.8%) have been reported in India, Bangladesh, Ethiopia, and Peru [6, 30,31,32]. These discrepancies could be attributed to the geographical distribution where the studies were conducted as well as the sample size, hygienic practices, awareness, educational level, community customs and traditions, and sex [26].
Regarding sex, women had a higher prevalence of UTI (52.1%) than men (47.9%). This finding is consistent with most previous reports [5, 6, 31, 32]. Several studies have proposed factors that could increase the prevalence of UTI among certain patients, including the proximity of the urethra to the anus and less acidic pH of the vaginal surface in women, wider and shorter urethra, sexual behavior, incontinence, and poor hygienic practices [11, 33, 34].
The samples collected from Saudi patients with suspected UTI showed the highest prevalence of positive cultures (74.2%), which could be attributed to the higher proportion of Saudis than that of non-Saudis in this study. Conversely, other nationalities with large communities in Madinah such as Pakistanis and Mauritanians demonstrated the highest prevalence among the non-Saudis (Table 1).
The Gram-negative bacteria were the most prevalent isolates from our patients’ urine samples. The Enterobacterales family was the predominant bacterial family. E. coli was the most prevalent isolated bacterial species (n = 1172; 29.8%), followed by K. pneumoniae (n = 889; 22.4%) and P. aeruginosa (n = 323; 5.1%) (Table 2). Despite the multicultural nature of Madinah, our findings concerning the most predominant Gram-negative bacteria are consistent with several reports in Saudi Arabia and elsewhere [5, 6, 25,26,27, 31, 32, 35].
Among the Gram-positive isolates, E. faecalis was the most frequently identified species (n = 301; 7.6%), followed by S. agalactiae (n = 269; 6.8%). Consistent with our findings, several studies, including a study conducted in Sakaka, Saudi Arabia, reported Enterococcus spp. as the most commonly isolated Gram-positive uropathogen [31, 35, 36]. However, other uropathogens such as S. aureus, S. agalactiae, and coagulase-negative Staphylococcus have also been reported as the most frequently identified Gram-positive bacteria [25, 37]. These discrepancies could be attributed to the methodology implemented in the data collection, sensitivity of bacteria identification systems, or differences in the inclusion criteria or sample size. Nevertheless, other factors, including hygienic practices, awareness, and educational level within the studied community, may also contribute to the etiological variations, which must be considered in future studies [26].
In the AST, E. coli showed > 50% resistance to 10 of 18 tested antibiotics. It exhibited the highest resistance rates to aztreonam, ampicillin, and cephalexin at 85.2%, 78.8%, and 71.2%, respectively (Table 3). These findings agree with other reports of resistance rates between 70% and 90% against these antibiotics [31, 36, 38]. On the contrary, E. coli was highly sensitive to imipenem, meropenem, and amikacin at the rates of 92.3%, 89.4%, and 88.5%, respectively. The high sensitivity rates in this study are closely similar to those in the previous work by Rahman et al. (97.89%, 80.87%, and 88.65%, respectively) [31] (Table 3).
Klebsiella spp. has a resistance pattern that is relatively similar to that of E. coli although with a higher resistance rate (Table 3). Notably, Klebsiella spp. demonstrated 59.7% and 44.7% resistance rates to meropenem and imipenem, respectively, compared with E. coli. Moreover, the resistance to imipenem occurred at a much faster rate owing to the higher intermediate resistance level. These findings contradict other reports within Saudi Arabia that imipenem and meropenem are still effective against Klebsiella spp. at resistance rates of < 24%. Colistin has been shown to be effective against Klebsiella spp. at a resistance rate of 8.3%; in this study, a much higher resistance rate (38.8%) was observed [35].
For Proteus spp., a previous study has shown meropenem as the most effective antibiotic at a sensitivity rate of 100% and nitroxoline as the least effective antibiotic at a resistance rate of 80% [37]. Our study showed increased resistance rates for both antibiotics (Fig. 3C; Table 3). Nevertheless, the same previous study has reported high sensitivity rates to meropenem and imipenem (90%), in contrast to our sensitivity rates of 60.2% and 53.3%, respectively (Fig. 3C; Table 3). Herein, Acinetobacter spp. showed high resistance rates to almost all tested antibiotics, except for colistin, which showed a 100% sensitivity rate (Fig. 3E; Table 3), similar to that reported in Northern Saudi Arabia [35].
Enterococcus spp. showed a 17.3% resistance rate to vancomycin and a 4.3% resistance rate to linezolid (Fig. 3F; Table 3). Similarly, Taher et al. reported that Enterococcus spp. had a resistance rate of 13% to vancomycin and 7.5% to linezolid [35]. In addition, Rahman et al. reported a sensitivity rate of 94.05% and 79.76% to vancomycin and linezolid, respectively [31]. Staphylococcus spp. were most highly sensitive to vancomycin (100%), followed by nitroxoline (95.3%). However, they showed high resistance rates of > 51% to ampicillin, erythromycin, and oxacillin, consistent with previously reported data [31, 36]. Streptococcus spp. showed a high resistance rate to trimethoprim/sulfamethoxazole (92.1%) which is markedly higher than the 25% resistance rate that had been reported in Hai’l, Saudi Arabia [25].
A notable limitation of this study is the localized scope, which does not fully capture the broader population trends or account for potential UTI patterns. Moreover, although the findings are valuable, their relevance to the entirety of Saudi Arabia might be limited due to the country’s substantial geographical expanse and diverse environments. In addition, the challenge of antibiotic shortages posed a significant obstacle, given the vital importance of thoroughly investigating the antibiotic sensitivity patterns of all isolated bacteria. Thus, the availability of antibiotics is essential to provide a comprehensive idea about the antibiogram in a specific community. Furthermore, it would be valuable to expand the scope of the study findings by incorporating an examination of UTI prevalence and antimicrobial patterns within specific risk groups and different hospitals.
Conclusions
Incorrect practices performed by healthcare practitioners, including erroneous prescriptions or over-prescription of antibiotics, are considered a main contributor to developing and spreading bacterial resistance. Physicians usually follow general guidelines in treating patients with UTIs. Thus, the local epidemiological trends and antimicrobial sensitivity rates of common bacteria are typically neglected. In this retrospective study, we focused on the prevalence, etiology, and antimicrobial sensitivity trends of uropathogens in a local setting. This study could provide insights into a successful antimicrobial selection for UTI treatment. We strongly suggest that any empirical antibiotic selection should consider the local epidemiological trends and resistance patterns of the most common uropathogens rather than implementing a universal guideline. The findings could also serve as a basis for implementing new policies to control the emergence of multidrug-resistant uropathogens.
Data Availability
The data are available upon request in accordance with confidentiality and privacy regulations from the corresponding author.
Abbreviations
- UTI:
-
Urinary tract infection
- AST:
-
Antimicrobial susceptibility test
References
Stamm WE, Norrby SR. Urinary tract infections: disease panorama and challenges. J Infect Dis. 2001;183(Suppl 1):1–4.
Alanazi MQ, Al-Jeraisy MI, Salam M. Prevalence and predictors of antibiotic prescription errors in an emergency department, Central Saudi Arabia. Drug Healthc Patient Saf. 2015;7:103–11.
Mathur NB, Agarwal HS, Maria A. Acute renal failure in neonatal sepsis. Indian J Pediatr. 2006;73(6):499–502.
Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13(5):269–84.
Odoki M, Almustapha Aliero A, Tibyangye J, Nyabayo Maniga J, Wampande E, Drago Kato C, et al. Prevalence of bacterial urinary tract infections and Associated factors among patients attending hospitals in Bushenyi District, Uganda. Int J Microbiol. 2019;2019:4246780.
Yenehun Worku G, Belete Alamneh Y, Erku Abegaz W. Prevalence of bacterial urinary tract infection and Antimicrobial susceptibility patterns among diabetes Mellitus Patients attending Zewditu Memorial Hospital, Addis Ababa, Ethiopia. Infect Drug Resist. 2021;14:1441–54.
Emiru T, Beyene G, Tsegaye W, Melaku S. Associated risk factors of urinary tract infection among pregnant women at Felege Hiwot Referral Hospital, Bahir Dar, North West Ethiopia. BMC Res Notes. 2013;6:292.
Raz R, Chazan B, Kennes Y, Colodner R, Rottensterich E, Dan M, et al. Empiric use of trimethoprim-sulfamethoxazole (TMP-SMX) in the treatment of women with uncomplicated urinary tract infections, in a geographical area with a high prevalence of TMP-SMX-resistant uropathogens. Clin Infect Dis. 2002;34(9):1165–9.
Storme O, Tiran Saucedo J, Garcia-Mora A, Dehesa-Davila M, Naber KG. Risk factors and predisposing conditions for urinary tract infection. Ther Adv Urol. 2019;11:1756287218814382.
Handley MA, Reingold AL, Shiboski S, Padian NS. Incidence of acute urinary tract infection in young women and use of male condoms with and without nonoxynol-9 spermicides. Epidemiology. 2002;13(4):431–6.
Al-Badr A, Al-Shaikh G. Recurrent urinary tract infections management in women: a review. Sultan Qaboos Univ Med J. 2013;13(3):359–67.
Klein RD, Hultgren SJ. Urinary tract infections: microbial pathogenesis, host-pathogen interactions and new treatment strategies. Nat Rev Microbiol. 2020;18(4):211–26.
Karlowsky JA, Hoban DJ, Decorby MR, Laing NM, Zhanel GG. Fluoroquinolone-resistant urinary isolates of Escherichia coli from outpatients are frequently multidrug resistant: results from the north american urinary tract infection Collaborative Alliance-Quinolone Resistance study. Antimicrob Agents Chemother. 2006;50(6):2251–4.
Terlizzi ME, Gribaudo G, Maffei ME. UroPathogenic Escherichia coli (UPEC) infections: virulence factors, bladder responses, antibiotic, and non-antibiotic antimicrobial strategies. Front Microbiol. 2017;8:1566.
Seifu WD, Gebissa AD. Prevalence and antibiotic susceptibility of Uropathogens from cases of urinary tract infections (UTI) in Shashemene referral hospital, Ethiopia. BMC Infect Dis. 2018;18(1):30.
Muhammad A, Khan SN, Ali N, Rehman MU, Ali I. Prevalence and antibiotic susceptibility pattern of uropathogens in outpatients at a tertiary care hospital. New Microbes New Infect. 2020;36:100716.
Merga Duffa Y, Terfa Kitila K, Mamuye Gebretsadik D, Bitew A. Prevalence and Antimicrobial susceptibility of bacterial uropathogens isolated from Pediatric patients at Yekatit 12 Hospital Medical College, Addis Ababa, Ethiopia. Int J Microbiol. 2018;2018:8492309.
Rowe TA, Juthani-Mehta M. Diagnosis and management of urinary tract infection in older adults. Infect Dis Clin North Am. 2014;28(1):75–89.
Tandogdu Z, Wagenlehner FM. Global epidemiology of urinary tract infections. Curr Opin Infect Dis. 2016;29(1):73–9.
Ameshe A, Engda T, Gizachew M. Antimicrobial resistance patterns, extended-spectrum beta-lactamase production, and Associated Risk factors of Klebsiella Species among UTI-Suspected patients at Bahir Dar City, Northwest Ethiopia. Int J Microbiol. 2022;2022:8216545.
Marialouis XA, Santhanam A, Antibiotic Resistance. RAPD- PCR typing of multiple drug resistant strains of Escherichia Coli from urinary tract infection (UTI). J Clin Diagn Res. 2016;10(3):DC05–9.
Jafri SA, Qasim M, Masoud MS, Rahman MU, Izhar M, Kazmi S. Antibiotic resistance of E. coli isolates from urine samples of urinary tract infection (UTI) patients in Pakistan. Bioinformation. 2014;10(7):419–22.
Khonsari MS, Behzadi P, Foroohi F. The prevalence of type 3 fimbriae in Uropathogenic Escherichia coli isolated from clinical Meta Gene. 2021;28.
Argaam. Four Saudi cities among world’s top 100 destinations in 2019 2019 [Available from: https://www.argaam.com/en/article/articledetail/id/1333386.
Bazaid AS, Saeed A, Alrashidi A, Alrashidi A, Alshaghdali K, S AH, et al. Antimicrobial surveillance for bacterial uropathogens in Ha’il, Saudi Arabia: a five-year Multicenter Retrospective Study. Infect Drug Resist. 2021;14:1455–65.
Al-Gasha’a FAS, Al-Baker SM, Obiad JM, Alrobiai FA. Prevalence of urinary tract infections and Associated Risk factors among patients attending Medical City Hospital in Baghdad City, Iraq. Am J Infect Dis. 2020;16(2):77–84.
Alanazi MQ, Alqahtani FY, Aleanizy FS. An evaluation of E. coli in urinary tract infection in emergency department at KAMC in Riyadh, Saudi Arabia: retrospective study. Ann Clin Microbiol Antimicrob. 2018;17(1):3.
Kalal BS, Nagaraj S. Urinary tract infections: a retrospective, descriptive study of causative organisms and antimicrobial pattern of samples received for culture, from a tertiary care setting. Germs. 2016;6(4):132–8.
Folliero V, Caputo P, Della Rocca MT, Chianese A, Galdiero M, Iovene MR et al. Prevalence and Antimicrobial susceptibility patterns of bacterial pathogens in urinary tract infections in University Hospital of Campania Luigi Vanvitelli between 2017 and 2018. Antibiotics (Basel). 2020;9(5).
Mohapatra S, Panigrahy R, Tak V, Chaudhuri JVSKCS. Prevalence and resistance pattern of uropathogens from community settings of different regions: an experience from India. Access Microbiol. 2022;4(2):000321.
Rahman F, Akhter H, Hasnat S, Begum N. Prevalence and antimicrobial sensitivity profile of uropathogens in a tertiary care hospital of Dhaka city. Bangladesh J Med Microbiol. 2020;14(2):3–11.
Medina M, Castillo-Pino E. An introduction to the epidemiology and burden of urinary tract infections. Ther Adv Urol. 2019;11:1756287219832172.
Minardi D, d’Anzeo G, Cantoro D, Conti A, Muzzonigro G. Urinary tract infections in women: etiology and treatment options. Int J Gen Med. 2011;4:333–43.
Olorunmola FO, Kolawole DO, Lamikanra A. Antibiotic resistance and virulence properties in Escherichia coli strains from cases of urinary tract infections. Afr J Infect Dis. 2013;7(1):1–7.
Taher I, Almaeen A, Aljourfi H, Bohassan E, Helmy A, El-Masry E, et al. Surveillance of antibiotic resistance among uropathogens in Aljouf region northern Saudi Arabia. Iran J Microbiol. 2019;11(6):468–77.
Sohail M, Khurshid M, Saleem HG, Javed H, Khan AA. Characteristics and antibiotic resistance of urinary tract pathogens isolated from Punjab, Pakistan. Jundishapur J Microbiol. 2015;8(7):e19272.
Sain Mirza Z, Rafeeq M, Murad HAS, Hussain MB. Isolation and drug susceptibility pattern of uropathogens in saudi diabetic and non-diabetic patients with urinary tract infection. Bioinformation. 2022;18(8).
Ali AH, Reda DY, Ormago MD. Prevalence and antimicrobial susceptibility pattern of urinary tract infection among pregnant women attending Hargeisa Group Hospital, Hargeisa, Somaliland. Sci Rep. 2022;12(1):1419.
Acknowledgements
We acknowledge the generous help provided by Dr. Abdullah Almutairi (Head of the Microbiology Department, King Fahad General Hospital, Madinah, Saudi Arabia) in facilitating the data collection.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interpretation of results, and manuscript writing.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This study was approved by the Ethics Committee of King Salman bin Abdulaziz Medical City (Institutional Review Board (IRB) no. 22 − 014). As the study relied on previously examined laboratory culture data without any direct involvement of patients, informed consent was not required and was waived by the King Salman bin Abdulaziz Medical City IRB. Patient’s identities remained confidential, with numerical codes used to represent the cases. All methods in this study were conducted in compliance with the relevant guidelines and regulations pertaining to studies involving human subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Almutawif, Y.A., Eid, H.M.A. Prevalence and antimicrobial susceptibility pattern of bacterial uropathogens among adult patients in Madinah, Saudi Arabia. BMC Infect Dis 23, 582 (2023). https://doi.org/10.1186/s12879-023-08578-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08578-1