Abstract
Background
To date, few cases of TSS caused by coagulase negative (CoN) staphylococci have been reported in the literature. Recent data show that CoN staphylococci are capable of secreting a number of enterotoxins and cytotoxins, normally produced by S. aureus. Herewith, we describe a case of TSS caused by Staphylococcus epidermidis with a favorable outcome.
Case presentation
We report a case of a 46-year-old man who developed TSS from S. epidermidis. The patient was admitted for a 7-day history of general malaise and headache following a recent influenza infection and a 3-day history of vomiting, diarrhea, diffuse erythroderma, and fever. The main laboratory findings on admission were leukopenia (WBC 800/mm3), thrombocytopenia (Plt count 78.000/mm3), elevated urea, creatine levels and increased inflammatory markers (CRP 368 mg/ml). The patient had clinical and radiological evidence of pneumonia with chest computed tomography (CT) showing diffuse bilateral airspace opacifications with air bronchogram. On the second day, a methicillin resistant S. epidermidis (MRSE) strain was detected in both sets of blood cultures, but the organism was unavailable for toxin testing. All other cultures and diagnostic PCR tests were negative. His clinical signs and symptoms fulfilled at that stage four out of five clinical criteria of TSS with a fever of 39 °C, diffuse erythroderma, multisystem involvement and hypotension. On the same day the patient was admitted to the ICU due to acute respiratory failure. The initial treatment was meropenem, vancomycin, levofloxacin, clindamycin, IVIG and steroids. Finger desquamation appeared on the 9th day of hospitalization, fulfilling all five clinical criteria for TSS.
Conclusions
To our knowledge, this is the first adult case with TSS induced by CoNS (MRSE) secondary to an influenza type B infection, who had favorable progression and outcome. Further research is warranted to determine how TSS is induced by the CoNS infections.
Similar content being viewed by others
Background
A common cause of severe influenza pathogenesis is superinfection with bacterial pathogens, most frequently, Staphylococcus aureus and Streptococcus pneumoniae [1]. Regardless of the infectious agent, bacterial superinfections are associated with increased morbidity and mortality rates during influenza pandemic and epidemic outbreaks [2]. According to the literature, the resolution of inflammation following an episode of influenza infection, is regarded as a period of enhanced susceptibility to several respiratory bacterial infections, resulting in bacterial superinfection, bacterial pneumonia and bacterial dissemination from the lungs [3]. This co-pathogenesis is characterized by complex interactions between co-infecting pathogens and the host, leading to dysregulation of immune responses and delays in a return to homeostasis [4].
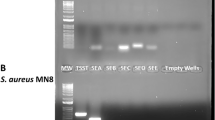
Coagulase-negative staphylococci are under-appreciated as a cause of severe clinical conditions, including TSS [5,6,7]. Previous studies have shown that coagulase-negative staphylococci do not produce the toxin TSST-1, but they are capable of secreting a number of staphylococcal enterotoxins and cytotoxins, normally produced by S. aureus [6, 7]. Recently Staphylococcal enterotoxins A, D, and E were detected in Staphylococcal epidermidis strains playing the role of superantigens [11]. An immune reaction to the proliferation of CoNS organisms that causes cytokine activation has been proposed as an additional possible pathophysiological mechanism of CoNS induced TTS [8]. In particular, strains of Staphylococcus epidermidis isolated from patients with toxic shock symptoms have been reported to carry genes related to stimulation of human monocytes fostering the production of the cytokines TNF alpha, IL-1 beta and IL-6 [8]. To date, the incidence of TSS induced by CoNS is largely not known and only few cases have been reported in the literature [8,9,10,11].
Case presentation
We report a case of a 46-year-old man, without chronic underlying conditions, who developed TSS from S. epidermidis following an influenza type B infection. The patient was brought to the hospital on an ambulance. He was admitted to the hospital for a 7-day history of general malaise, headache following a recent influenza type B infection, who gradually developed vomiting, diarrhea, diffuse erythroderma and fever during the last three days before admission. The consciousness level on admission, body temperature, blood pressure, pulse rate, respiratory rate, and peripheral oxygen saturation were E3V4M6, 39 °C, 87/50 mmHg, 130 beats/minute, 38 breaths/minute, and 91%, respectively. The main laboratory findings on admission were as following: leukopenia (WBC 800/mm3), thrombocytopenia (Plt count 78,000/mm3), elevated urea, creatine levels and increased inflammatory markers (CRP 248 mg/ml) [Table 1]. The patient had clinical and radiological evidence of pneumonia with chest computed tomography (CT) showing diffuse bilateral airspace opacification [Fig. 1]. Head CT was normal.
On the second day, both sets of blood cultures obtained from two different peripheral venous sites (left and right arm) were positive for S. epidermidis, but the organism was unavailable for toxin testing. According to the antibiogram, the strain was resistant to methicillin (Methicillin resistant Staphylococcus epidermidis, MRSE). Urine cultures were negative. After intubation for sedation and procedures, both sputum and endotracheal cultures showed growth of only normal upper respiratory flora. The results of the full respiratory pathogen PCR panel, including SARS-CoV-2, were negative. The patient’s condition deteriorated on the same day, presenting acute respiratory failure, and he was admitted to the ICU. His clinical signs and symptoms fulfilled at that stage four out of five clinical criteria of TSS with a fever of 39 °C, diffuse erythroderma, multisystem involvement and hypotension [Table 2] [12]. Based on the clinical diagnosis of probable CoNS induced TTS and the critical condition of the patient, the following treatment was initiated during the first days of hospitalization: meropenem (1 g every 8 h), vancomycin (1 g every 12 h), levofloxacin (750 mg 24 h), clindamycin (600 mg every 8 h). The choice of the initial empirical antibiotic therapy was based on local guidelines due to high antimicrobial resistant rates (AMR) rates. The addition of clindamycin was based on the high suspicion of TTS. IVIG (2 g/kg) and hydrocortisone (100 mg every 8 h) were administrated to the patient due to high suspicion of TTS The mechanism responsible for the efficacy of gamma-globulin (IVIG) therapy may be neutralization of the circulating toxins, inhabitation of TNF-alpha production via nonspecific inhabitation of monocyte or T-cell activation, or inhibition of other staphylococcal virulence factors. The patient became afebrile within the first 72 h of ICU admission. During the first 5 days of ICU stay, his PLT and WBC count reached its nadir. Finger desquamation mainly on his feet appeared on the 9th day of hospitalization, fulfilling at that stage five out of five clinical criteria for TSS [Fig. 2]. During the ICU stay, the patient presented acute renal failure and he received renal replacement therapy with hemofiltration for 21 days. The platelet count remained low and due to the increased risk of central nervous system (CNS) bleeding, the patient received additionally after PLTs transfusions, PLT growth factor, eltrombopag (75 mg 24 h), and dexamethasone (8 mg every 8 h) for 4 consecutive days, after having a hematologist expert consultation with the indication of persistent refractory thrombocytopenia. All drug doses were accordingly adjusted. The patient gradually improved over the following 2 months, and he was discharged from the hospital without sequelae.
Discussion and conclusion
The current patient was diagnosed with TSS, as he fulfilled all five diagnostic criteria proposed by the Council of State and Territorial Epidemiologists (USA) and Centers for Disease Control and Prevention (US) [12]. To the best of our knowledge this is the first adult case with a TSS syndrome induced by Staphylococcus epidermitis following an influenza type B infection, who had favorable progression and outcome.
According to the literature, both clinically and experimentally, bacterial complications (super-infections) are most pronounced after 5–7 days of acute influenza infection, which was evident also in our case [13]. Deciphering the mechanisms of bacterial superinfections (loss of the epithelial barrier function and altered innate immune defense), is of importance, to provide new diagnostic tools and therapeutic approaches. According to the literature influenza infection appears to prime the host airways for bacterial infection, whilst modifying and impairing immune responses in a number of ways. Viral induced immunosuppression can allow for a bacterial super infection, as host immune responses can be suppressed when immunologic cells are impaired during influenza infection and immune cell dysfunction can reduce the host’s ability to fight bacteria [14].
Typically, TSS is caused by S. aureus or streptococcal infections. Exotoxins secreted from Staphylococcus aureus or Streptococcus pyogenes might act as superantigens enhancing inflammation processes via cytokine storm release [5, 6]. However, the exact pathophysiological mechanism behind the presence of TSS induced by CoNS, remains largely unknown and warrants further investigation.
The true incidence of TSS by CoNS is an unexplored territory, and currently only few cases have been reported in the literature [Table 3]. Among them, a recently published case by Goda K et al. with TSS caused by a CoNS species (Staphylococcus simulans) after an episode of pneumococcal pneumonia associated with influenza [10]. Of interest, this case presented with high levels of inflammatory markers and cytokines (neopterin and IL-6), supporting the hypothesis of a cytokine storm release in CoNS TSS [10]. Similarly, Pomputius WF et al. reported a pediatric case of CoNS TSS due to S. epidermitis [11]. Although superantigen proteins were not isolated from the bloodstream of the child, a panel of four superantigen genes were finally detected in the plasma, suggesting that the CoNS found in urine, could be a causative agent inducing TSS.
To conclude, we present a rare adult case TSS caused by coagulase-negative staphylococci (CoNS). It remains to be further evaluated how TSS is induced by the CoNS infection, with several mechanisms being proposed, including the presence of superantigens and hyper inflammation induced by cytokine mediators.
Data availability (ADM)
Further patient’s data are available upon request to the Corresponding Author, Zoi Dorothea Pana, email: z.pana@euc.ac.cy, contact phone: +35,794,049,474.
Abbreviations
- CoNS:
-
Coagulase-negative staphylococcus
- CT:
-
Computed tomography
- MRSE:
-
Methicillin-resistant Staphylococcus – epidermidis
- S. simulans:
-
Staphylococcus simulans
- S. aureus:
-
Staphylococcus aureus
- PCR:
-
Polymerase chain rection
- TSS:
-
Toxic shock syndrome
- ICU:
-
Intensive Care Unit
- IVIG:
-
Intravenous Immunoglobulin
- WBC:
-
White blood cell count
- Plt:
-
Platelet count
- CRP:
-
C reactive protein
- CNS:
-
Central nervous system
References
Rynda-Apple A, Robinson KM, Alcorn JF. Influenza and bacterial superinfection: Illuminating the immunologic mechanisms of Disease. Infect Immun. 2015;83(10):3764–70.
Blyth CC, Webb SA, Kok J, Dwyer DE, van Hal SJ, Foo H, et al. ANZIC Influenza Investigators; COSI Microbiological Investigators. The impact of bacterial and viral co-infection in severe influenza. Influenza Other Respir Viruses. 2013;7(2):168–76.
Paget C, Trottein F. Mechanisms of bacterial superinfection post-influenza: a role for unconventional T cells. Front Immunol. 2019;10:336.
McCullers JA. The co-pathogenesis of influenza viruses with bacteria in the lung. Nat Rev Microbiol. 2014;12(4):252–62.
Michels R, Last K, Becker SL, Papan C. Update on coagulase-negative staphylococci-what the Clinician should know. Microorganisms. 2021;9(4):830.
Stach CS, Vu BG, Schlievert PM. Determining the presence of superantigens in coagulase negative staphylococci from humans. PLoS ONE. 2015;10:e0143341.
Madhusoodanan J, Seo KS, Remortel B, Park JY, Hwang SY, Fox LK, et al. An enterotoxin-bearing pathogenicity island in Staphylococcus epidermidis. J Bacteriol. 2011;193:1854–62.
Lina G, Fleer A, Etienne J, Greenland TB, Vandenesch F. Coagulase-negative staphylococci isolated from two cases of toxic shock syndrome lack superantigenic activity but induce cytokine production. FEMS Immunol Med Microbiol. 1996;13:81–6.
Crass BA, Bergdoll MS. Involvement of coagulase-negative staphylococci in toxic shock syndrome. J Clin Microbiol. 1986;23:43–5.
Goda K, Kenzaka T, Hoshijima M, Yachie A, Akita H. Toxic shock syndrome with a cytokine storm caused by Staphylococcus simulans: a case report. BMC Infect Dis. 2021;21(1):19.
Pomputius WF, Kilgore SH, Schlievert PM. Probable enterotoxin-associated toxic shock syndrome caused by Staphylococcus epidermidis. BMC Pediatr. 2023;23(1):108.
Centers for Disease Control and Prevention. Toxic shock syndrome (other than streptococcal) (TSS) 2011 case definition https://ndc.services.cdc.gov/case-definitions/toxic-shock-syndrome-2011/.
Smith AP, Lane LC, Zuniga IR, Moquin D, Vogel P, Smith A. Increased virus dissemination leads to enhanced lung injury but not inflammation during influenza-associated secondary bacterial infection. FEMS Microbes. 2022;3:xtac022.
Morris DE, Cleary DW, Clarke SC. Secondary bacterial Infections Associated with Influenza Pandemics. Front Microbiol. 2017;8:1041.
Acknowledgements
N/A (not applicable).
Funding
None.
Author information
Authors and Affiliations
Contributions
“C.A. and Z.D.P wrote the main manuscript text, A.I.,T.L., A.G, E.D., K.M.,C.A. were the physicians who treated the patient. All authors drafted and reviewed the manuscript.“
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
informed consent from the subject for publication of identifying information/images in an online open-access publication has been obtained; the draft has received approval from the hospital committee.
Consent for publication
informed consent from the subject for publication of identifying information/images in an online open-access publication has been obtained; the draft has received approval from the hospital committee.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Armeftis, C., Ioannou, A., Lazarou, T. et al. Staphylococcus epidermidis induced toxic shock syndrome (TSS) secondary to influenza infection. BMC Infect Dis 23, 583 (2023). https://doi.org/10.1186/s12879-023-08487-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08487-3