Abstract
Background
Enteric fever is an acute systemic infectious disease associated with substantial morbidity and mortality in low- and middle-income countries (LMIC), with a global burden of 14.3 million cases. Cases of enteric fever or paratyphoid fever, caused by Salmonella enterica serovar Paratyphi A (S. Para A) have been found to rise in many endemic and non-endemic countries. Drug resistance is relatively uncommon in S. Para A. Here we report a case of paratyphoid fever caused by ceftriaxone resistant S. Para A from Pakistan.
Case presentation
A 29-year-old female presented with a history of fever, headache, and shivering. Her blood culture revealed a S. Para A isolate (S7), which was resistant to ceftriaxone, cefixime, ampicillin and ciprofloxacin. She was prescribed oral Azithromycin for 10 days, which resulted in resolution of her symptoms.
Two other isolates of S. Para A (S1 and S4), resistant to fluoroquinolone were also selected for comparison. DST and whole genome sequencing was performed for all three isolates. Sequence analysis was performed for identification of drug resistance and phylogeny. Whole Genome Sequencing (WGS) of S7 revealed the presence of plasmids, IncX4 and IncFIB(K). blaCTX-M-15 and qnrS1 genes were found on IncFIB(K). The gyrA S83F mutation conferring fluoroquinolone resistance was also found present. Multi-locus sequence typing (MLST) showed the S7 isolate to belong to ST129. S1 and S4 had the gyrA S83Y and S83F mutations respectively.
Conclusions
We highlight the occurrence of plasmid-mediated ceftriaxone resistant strain of S. Para A. This is of significance as ceftriaxone is commonly used to treat paratyphoid fever and resistance in S. Para A is not known. Continuous epidemiological surveillance is required to monitor the transmission and spread of antimicrobial resistance (AMR) among Typhoidal Salmonellae. This will guide treatment options and preventive measures including the need for vaccination against S. Para A in the region.
Similar content being viewed by others
Background
Enteric fever (Typhoid and Paratyphoid fever) is an acute systemic infectious disease. It is associated with a global burden of 14·3 million cases, causing substantial morbidity and mortality (1). Since in low- and middle-income countries (LMIC), a rising trend of antimicrobial resistance is seen in Salmonella species, WHO has ranked it as a high priority organism requiring research and newer antibiotic development (https://www.who.int/publications/i/item/WHO-EMP-IAU-2017.12). Salmonella enterica serovar Paratyphi A (S. Para A) is ranked second as a causative agent of enteric fever, preceded only by Salmonella enterica serovar Typhi (S. Typhi). Enteric fever caused by S. Para A, or Paratyphoid fever was thought to be responsible for a comparatively smaller proportion of enteric fever cases [1]. However, since the 1980s both the incidence and relative frequency of Paratyphoid fever have risen in Nepal, Pakistan, and Thailand [2, 3]. Moreover, the populous nations of India and China have reported substantial numbers of S. Para A cases [4, 5]. Non-endemic countries like the United States report an increasing trend of Paratyphoid fever especially, amongst travelers from South Asia [6].
S. Para A resides in the human gut and its clinical manifestations are indistinguishable from Typhoid fever. Its genome is like that of S. Typhi, with the additional accumulation of 173 to 210 pseudo genes among its protein coding sequences [7]. Until recently, S. Para A was mostly observed to have a distinct prevalence rate and drug resistance pattern from that of S. Typhi [8]. For example, multidrug resistant (MDR) S. Typhi strains, are commonly isolated from many enteric fever endemic countries, while MDR S. Para A strains are either not yet reported from many enteric fever endemic countries like Bangladesh and Nepal [9, 10] or infrequently reported from some countries like Pakistan and India [11, 12]. Likewise, while ceftriaxone resistant S. Typhi strains have been commonly reported from Pakistan, this resistance has not been reported in S. Para A from Pakistan. In fact, our extensive literature search has revealed only one case report of ceftriaxone resistant S. Para A, published from United Kingdom in 2020. Ceftriaxone resistant S. Para A in that case was causing infective colitis in a traveler returning to England from Bangladesh [13].
Here, we report the first ceftriaxone resistant S. Para A, isolated from the blood culture of a clinically suspected case of paratyphoid fever or enteric fever.
Case presentation
On 1st June 2021, a set of blood culture bottle (BACT/ALERT® Culture Media, bioMérieux) was received at the Clinical Microbiology Laboratory of Aga Khan University Hospital (AKUH) Karachi, Pakistan. The patient was a 29-year-old female, resident of Karachi with no known comorbidity. On 3rd day of fever, headache, and shivering, she consulted her physician who requested blood culture. After positive blood culture result, she was prescribed oral Azithromycin for 10 days, her symptoms subsided with medications.
S. Para A (isolate S7) was identified using API® 20E (Analytical profile index-BioMérieux) and Salmonella poly O and factor 2 antisera (BD-difcoTM). Antimicrobial drug susceptibility testing was performed by Kirby-Bauer disk diffusion and VITEK 2® COMPACT SYSTEM (BioMérieux). Susceptibility results against ampicillin, ceftriaxone, cefixime, chloramphenicol, trimethoprim-sulfamethoxazole, ciprofloxacin, ofloxacin, azithromycin, imipenem, ertapenem and meropenem were interpreted using recent CLSI performance standards for Antimicrobial Susceptibility Testing (M100-Ed32).
Two additional S. Para A clinical isolates (S1 and S4) were randomly picked from the same batch of positive blood cultures and underwent same identification protocol like S. Para A (S7). Similarly, S1 and S4 isolates were tested against same antibiotics as S. Para A(S7) using similar susceptibility testing methods.
Whole genome sequencing (WGS) was performed on DNA extracted from S. Para A isolates S1, S4 and S7. Library preparation was performed using the Nextera XT DNA kit. Sequencing was performed on the Illumina MiniSeq system. FASTQ files of the samples were checked for quality using Fastqc v0.11.9 (https://github.com/s-andrews/FastQC) and were trimmed and assembled using Shovill v0.9.0 (https://github.com/tseemann/shovill). The assembly quality was checked using QUAST [14] using the reference genome S. Para A (NC_006511) [7]. Variant calling was performed using Freebayes v1.3.5 [15] and Snippy v4.6.0 (https://github.com/tseemann/snippy) and the variants were annotated using snpEFF v4.5.0 [16]. The AMR profiling was performed using rgi v5.1.1 [17] and staramr v0.7.2 [18] using CARD, Megares, AMRfinder databases.
S. Para A sequences (S1, S4 and S7) were submitted to NCBI SRA with accession numbers SRR16674692, SRR16674689 and SRR16674686, respectively. Genome sequences were compared with the S. Para A reference sequence accession number (NC_006511) [7], a sequence reported from a travel associated infective colitis caused by ESBL producing ceftriaxone resistant S. Para A, from stool sample of a traveler returning to England from Bangladesh in 2017 [13] and a S. Para A sequence from Bangladesh (SRR7209524), Fig. 1.
BRIG plot of S. Para A strains. The coverage map of three S. Para A sequences is shown as compared with the reference S. Para A strain (SRR7209524). Additional GC content and GC Skew features are displayed. The tool used to draw figure is BRIG tool (https://brig.sourceforge.net/)
Resistance genes were determined using ResFinder v4.0 software [19]. PlasmidFinder v2.1 [20] was used to detect the types of plasmids. The gene cassettes were identified using the prokka tool [21].
BLAST [22] pairwise alignment was performed to compare relatedness of plasmids between S7 IncFIB (Pakistan) and the Inc-MK238490 (Bangladesh) [13] (Fig. 2A). The plot was visualized using BRIG tool [23]. The Fig. 2B and C displayed with SnapGene (www.snapgene.com).
XDR plasmid in S. Para A isolate. A Pairwise alignment of S7 IncFIB(K) plasmid (blue ring) is shown against the S. Para A strain from Bangladesh with Inc-MK238490 (green ring) and E.coli plasmid CPO42900 (reference sequences, outer red ring). GC-skew is shown in inner ring, black line. The circular alignment is produced and visualized using BRIG tool. B expanded region (genes in red) indicating presence of betaCTX-M-1 associated with transposase Tn2 and Tn3. C Bangladesh strain plasmid Inc-MK238490 with betaCTX-M-1 cassette with Tn3 family genes. The plasmids are constructed using SnapGene tool (www.snapgene.com)
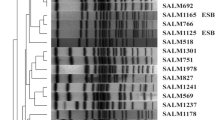
A phylogenetic tree was made using the variants generated using Snippy for sequences from S1, S4 and S7 along with the other available S. Para A sequences of strains reported from between 2014 and 2021 from countries of different regions: Cambodia [24], Canada [25], China [26], Bangladesh [27], Belgium (BioProject: PRJEB18573) and USA [7]. The tree was generated using Iqtree with (http://www.cibiv.at/software/iqtree) using substitution model GTR algorithm (Fig. 3). The tree was visualized using an interactive tree visualization tool itol [28].
Identification and assignment of species type for S. Para A (S1, S4, and S7) isolates were determined using Multi Locus Sequencing Typing MLST v2.19.0 [29].
Results
Antimicrobial susceptibility testing results of S1, S4 and S7 isolates are shown in Table 1.
Ceftriaxone MIC for S7 was > = 64 µg/ml and for SI and S4, it was < = 1 µg/ml. All three isolates (S1, S4 and S7) were susceptible to imipenem, ertapenem, meropenem and azithromycin.
We found consistent sequence coverage across the whole genome of all three isolates (S1, S4 and S7) (Fig. 2A).
S1 had the fluoroquinolone resistance conferring mutation S83Y in the gyrA gene whilst S4 and S7 had gyrA S83F. S7 isolate was found to have blaCTX-M-15 gene associated with Ceftriaxone resistance and the qnrS1 gene (Table 1). S7 isolate had two plasmids, IncX4 and IncFIB. blaCTX-M-15 and qnrS1 genes were found on IncFIB, (Fig. 2B).
We compared the IncFIB plasmid of S7 with the Inc-MK238490 plasmid of a MDR S. Para A isolate from Bangladesh [13] (Fig. 2C). Overall, there was less than 10% sequence similarity found between the plasmids from Pakistan (IncFIB) and Bangladesh (Inc-MK238490) strains. The Bangladeshi Inc-MK238490 plasmid had the blaCTX-M-15 and blaTEM-1B genes, the latter associated with Ampicillin resistance.
The blaCTX-M-15 gene in both the Pakistan and Bangladesh strains were associated with a transposon. The gene cassette ISEcp9 –blaCTX-M-15-hp-tnpA was present in the Bangladesh strain [13]. In S7 we found the blaCTX-M-15 gene to be associated with ISEc36-tnp3 (Fig. 2B and C).
Phylogenetic analysis of the Pakistani S. Para A isolates revealed that the S1 and S7 isolates were closely related to an isolate from Bangladesh identified in 2017 [13] (Fig. 3). Whilst the S4 isolate was related to an isolate identified from a 2010 community outbreak of paratyphoid fever in China [30]. We performed MLST analysis for the isolates which revealed that S1 and S7 belonged to ST129 while S4 belonged to ST85.
Discussion
To our knowledge this is the first report of extended-spectrum-β-lactamase (ESBL) positive S. Para A (S7) from a Paratyphoid fever case. This S7 isolate shows antimicrobial resistance determinants identified by both phenotypic and genotypic methods. The S7 isolate was also genomically aligned with S. Para A sequence from Bangladesh (SRR7209524) which also harboured blaCTX-M-15 containing plasmid conferring resistance to cephalosporin [13]. The overall blaCTX-M-15 containing plasmids similarity among S. Para A strains from Pakistan and Bangladesh was found low (< 10%). They were also different incompatibility groups, IncFIB in this study and Inc-MK238490 from the Bangladesh strain [13]. However, strains from both Pakistan and Bangladesh included blaCTX-M-15 gene with a transposon associated with it. The gene cassette ISEcp9 –CTX-M-15-hp-tnpA has been reported to be responsible for transmission of the ESBL resistance in the Bangladesh strain [13]. In our strains however we found the blaCTX-M-15 gene to be associated with ISEc36-tnp3. This data supports the role of transposons in the transfer of AMR genes between plasmids of different strains.
It is of interest that both the S7 isolate here, and the S. Para A isolate from Bangladesh (SRR70209524) belonged to the ST129 clade. It would be necessary to conduct experimental studies to investigate whether this was a coincidence or that ST129 may be more readily available to accept plasmids from ESBLs harboring blaCTX-M-15.
S. Para A has an established dissimilarity in the prevalence rate and drug resistance pattern from its peer organism S. Typhi [8]. In Pakistan, MDR S. Para A strains have shown a sustained resistance rate of 2.2% since 2009, while a high percentage of fluoroquinolone resistant S. Para A strains has been reported from this country [12]. The S7 isolate has shown phenotypic and genotypic resistant to ampicillin, fluoroquinolone, and ceftriaxone. Though this isolate was also carrying catA1 gene, however, phenotypically it appeared susceptible to chloramphenicol. Ceftriaxone resistance was conferred by plasmids IncFIB. This plasmid type has been shown to carry resistance genes in Enterobacteriaceae [31]. Resistance to fluoroquinolone may be conferred by either the presence of qnr genes or mutations in the qrdr (quinolone resistance determining region of gyrA genes. As such, the intermediate resistance to fluoroquinolone observed in strains S1 and S4 could be due to mutations in gyrA S83F. Mutations in the qrdr have been defined as codons 67–106 in gyrA. These genes encode for drug target enzymes, DNA gyrase and DNA topoisomerase IV, and therefore mutations in these genes are associated with fluoroquinolone resistance [32].
Our study highlights the emergence of rising drug resistance in S. Para A. Increased drug resistance in S. Typhi and S. Para A is observed globally and associated with spread through travelers [33]. Expanding ESBL resistance in S. Para A and other Typhoidal Salmonella will increase the pressure in empirical treatment of Typhoidal salmonellae with treatment providers resorting to expensive injectable such as, meropenem and the oral macrolide, Azithromycin. Overuse of azithromycin is already raising a threat for surge in its resistance through the COVID-19 pandemic [34]. Due to potential to spread by fecal oral route, increasing drug resistance in S. Para A is a public health concern. Given that the current Typhoid conjugate vaccine does not provide defense against paratyphoid fever, and the fact that S. Para A reveals a different AMR profile from its peer S. Typhi, enteric fever disease dynamics and usefulness of empirical therapy are likely to change soon. Therefore, gaining further knowledge about S. Para A is essential. Furthermore, there is a need to introduce S. Para A vaccine for the at-risk population.
Conclusion
This case report indicates paratyphoid fever (enteric fever) causing potential of plasmid-mediated ceftriaxone resistant strain of S. Para A. The presence and emergence of ESBL S. Para A in Pakistan indicates the importance of epidemiological surveillance to track and monitor antimicrobial resistance in this pathogen. The emergence of this resistant S. Para A indicates additional threat due to drug resistant Salmonella species and highlights the importance of public health preventive measures and enhanced vaccinations to prevent further spread.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Change history
23 May 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12879-023-08321-w
Abbreviations
- S. Para A:
-
Salmonella enterica Serovar Paratyphi A
- S. Typhi:
-
Salmonella enterica Serovar Typhi
- LMIC:
-
Low- and middle-income countries
- AMR:
-
Antimicrobial resistance
- MDR:
-
Multidrug resistant
- ESBL:
-
Extended-spectrum-β- lactamase
- MLST:
-
Multi-locus sequence typing
- AKUH:
-
Aga Khan University Hospital
- qrdr:
-
Quinolone resistance determining region
- HSP:
-
Health Security Partners
References
Typhoid GBD, Paratyphoid C. The global burden of typhoid and paratyphoid fevers: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Infect Dis. 2019;19(4):369–81.
Arndt MB, Mosites EM, Tian M, Forouzanfar MH, Mokhdad AH, Meller M, Ochiai RL, Walson JL. Estimating the burden of paratyphoid a in Asia and Africa. PLoS Negl Trop Dis. 2014;8(6): e2925.
Maharjan A, Dhungel B, Bastola A, Thapa Shrestha U, Adhikari N, Banjara MR, Lekhak B, Ghimire P, Rijal KR: Antimicrobial susceptibility pattern of salmonella spp. isolated from enteric fever patients in Nepal. Infect Dis Rep 2021, 13(2):388–400.
John J, Van Aart CJ, Grassly NC. The burden of typhoid and paratyphoid in India: systematic review and meta-analysis. PLoS Negl Trop Dis. 2016;10(4):e0004616.
Liu FF, Zhao SL, Chen Q, Chang ZR, Zhang J, Zheng YM, Luo L, Ran L, Liao QH. Surveillance data on typhoid fever and paratyphoid fever in 2015, China. Zhonghua Liu Xing Bing Xue Za Zhi. 2017;38(6):754–8.
Date KA, Newton AE, Medalla F, Blackstock A, Richardson L, McCullough A, Mintz ED, Mahon BE. Changing Patterns in Enteric Fever Incidence and Increasing Antibiotic Resistance of Enteric Fever Isolates in the United States, 2008–2012. Clin Infect Dis. 2016;63(3):322–9.
McClelland M, Sanderson KE, Clifton SW, Latreille P, Porwollik S, Sabo A, Meyer R, Bieri T, Ozersky P, McLellan M, et al. Comparison of genome degradation in Paratyphi A and Typhi, human-restricted serovars of Salmonella enterica that cause typhoid. Nat Genet. 2004;36(12):1268–74.
Neupane DP, Dulal HP, Song J: Enteric fever diagnosis: current challenges and future directions. Pathogens 2021, 10(4):410.
Saha S, Islam M, Saha S, Uddin MJ, Rahman H, Das RC, Hasan M, Amin MR, Hanif M, Shahidullah M et al: Designing comprehensive public health surveillance for enteric fever in endemic countries: importance of including different healthcare facilities. J Infect Dis 2018, 218(suppl_4):S227-S231.
Saha S, Sajib MSI, Garrett D, Qamar FN. Antimicrobial resistance in typhoidal salmonella: around the world in 3 days. Clin Infect Dis. 2020;71(Suppl 2):S91–5.
Yousafzai MT, Irfan S, Thobani RS, Kazi AM, Hotwani A, Memon AM, Iqbal K, Qazi SH, Saddal NS, Rahman N, et al. Burden of culture confirmed enteric fever cases in Karachi, Pakistan: Surveillance for Enteric fever in Asia Project (SEAP), 2016–2019. Clin Infect Dis. 2020;71(Suppl 3):S214–21.
Qamar FN, Azmatullah A, Kazi AM, Khan E, Zaidi AK. A three-year review of antimicrobial resistance of Salmonella enterica serovars Typhi and Paratyphi A in Pakistan. J Infect Dev Ctries. 2014;8(8):981–6.
Nair S, Day M, Godbole G, Saluja T, Langridge GC, Dallman TJ, Chattaway M. Genomic surveillance detects Salmonella enterica serovar Paratyphi A harbouring blaCTX-M-15 from a traveller returning from Bangladesh. PLoS One. 2020;15(1):e0228250.
Gurevich A, Saveliev V, Vyahhi N, Tesler G. QUAST: quality assessment tool for genome assemblies. Bioinformatics. 2013;29(8):1072–5.
Garrison E, Marth G: Haplotype-based variant detection from short-read sequencing. arXiv preprint arXiv:12073907 2012.
Cingolani P, Platts A, le Wang L, Coon M, Nguyen T, Wang L, Land SJ, Lu X, Ruden DM. A program for annotating and predicting the effects of single nucleotide polymorphisms, SnpEff: SNPs in the genome of Drosophila melanogaster strain w1118; iso-2; iso-3. Fly (Austin). 2012;6(2):80–92.
Alcock BP, Raphenya AR, Lau TTY, Tsang KK, Bouchard M, Edalatmand A, Huynh W, Nguyen AV, Cheng AA, Liu S, et al. CARD 2020: antibiotic resistome surveillance with the comprehensive antibiotic resistance database. Nucleic Acids Res. 2020;48(D1):D517–25.
Bharat A, Petkau A, Avery BP, Chen JC, Folster JP, Carson CA, Kearney A, Nadon C, Mabon P, Thiessen J et al: Correlation between phenotypic and in silico detection of antimicrobial resistance in salmonella enterica in Canada using staramr. Microorganisms 2022, 10(2):292.
Bortolaia V, Kaas RS, Ruppe E, Roberts MC, Schwarz S, Cattoir V, Philippon A, Allesoe RL, Rebelo AR, Florensa AF et al: ResFinder 4.0 for predictions of phenotypes from genotypes. J Antimicrob Chemother 2020, 75(12):3491–3500.
Carattoli A, Zankari E, Garcia-Fernandez A, Voldby Larsen M, Lund O, Villa L, Moller Aarestrup F, Hasman H. In silico detection and typing of plasmids using PlasmidFinder and plasmid multilocus sequence typing. Antimicrob Agents Chemother. 2014;58(7):3895–903.
Hossain ME, Rahman MZ, Islam MM, Hoque AF, Sumiya MK, Begum MN, Alam MM, Uddin KMM, Hassan MZ, Rahman M, et al. Pre COVID-19 molecular epidemiology of respiratory syncytial virus (RSV) among children in Bangladesh. Heliyon. 2022;8(10): e11043.
Altschul SF, Gish W, Miller W, Myers EW, Lipman DJ. Basic local alignment search tool. J Mol Biol. 1990;215(3):403–10.
Alikhan NF, Petty NK, Ben Zakour NL, Beatson SA. BLAST Ring Image Generator (BRIG): simple prokaryote genome comparisons. BMC Genomics. 2011;12:402.
Kuijpers LMF, Le Hello S, Fawal N, Fabre L, Tourdjman M, Dufour M, Sar D, Kham C, Phe T, Vlieghe E, et al. Genomic analysis of Salmonella enterica serotype Paratyphi A during an outbreak in Cambodia, 2013–2015. Microb Genom. 2016;2(11): e000092.
Andres D, Gohlke U, Broeker NK, Schulze S, Rabsch W, Heinemann U, Barbirz S, Seckler R. An essential serotype recognition pocket on phage P22 tailspike protein forces Salmonella enterica serovar Paratyphi A O-antigen fragments to bind as nonsolution conformers. Glycobiology. 2013;23(4):486–94.
Yan M, Li X, Liao Q, Li F, Zhang J, Kan B. The emergence and outbreak of multidrug-resistant typhoid fever in China. Emerg Microbes Infect. 2016;5(6): e62.
Tanmoy AM, Westeel E, De Bruyne K, Goris J, Rajoharison A, Sajib MSI, van Belkum A, Saha SK, Komurian-Pradel F, Endtz HP: Correction for Tanmoy et al., Salmonella enterica serovar typhi in Bangladesh: exploration of genomic diversity and antimicrobial resistance mBio 2021, 12(3):e0104421.
Letunic I, Bork P. Interactive Tree Of Life (iTOL) v5: an online tool for phylogenetic tree display and annotation. Nucleic Acids Res. 2021;49(W1):W293–6.
Jiang Y, Yu D, Wei Z, Shen P, Zhou Z, Yu Y. Complete nucleotide sequence of Klebsiella pneumoniae multidrug resistance plasmid pKP048, carrying blaKPC-2, blaDHA-1, qnrB4, and armA. Antimicrob Agents Chemother. 2010;54(9):3967–9.
Yan, M., Yang, B., Wang, Z., Wang, S., Zhang, X., Zhou, Y., Pang, B., Diao, B., Yang, R., Wu, S., Klena, J. D., & Kan, B. (2015). A Large-Scale Community-Based Outbreak of Paratyphoid Fever Caused by Hospital-Derived Transmission in Southern China. PLoS Neglect Trop Dis. 9(7): e0003859. https://doi.org/10.1371/journal.pntd.0003859
Oliveira EM, Beltrao EMB, Scavuzzi AML, Barros JF, Lopes ACS. High plasmid variability, and the presence of IncFIB, IncQ, IncA/C, IncHI1B, and IncL/M in clinical isolates of Klebsiella pneumoniae with bla KPC and bla NDM from patients at a public hospital in Brazil. Rev Soc Bras Med Trop. 2020;53: e20200397.
Hooper DC, Jacoby GA. Mechanisms of drug resistance: quinolone resistance. Ann N Y Acad Sci. 2015;1354(1):12–31.
Chattaway MA, Gentle A, Nair S, Tingley L, Day M, Mohamed I, Jenkins C, Godbole G: Phylogenomics and antimicrobial resistance of salmonella typhi and paratyphi A, B and C in England, 2016–2019. Microb Genom. 2021, 7(8):000633.
Atal S, Misra S, Balakrishnan S. Continued use of azithromycin for mild COVID-19 in India: Evidence and implications? J Family Med Prim Care. 2021;10(12):4341–4.
Acknowledgements
We acknowledge Juma Research Laboratory genomics core group and Clinical Microbiology laboratory staff of Aga Khan University Hospital, Karachi for their support.
Funding
This study was supported by the Health Security Partners (HSP)-USA, as part of their collaboration with the Department of Pathology and Laboratory Medicine, Aga Khan University, for laboratory capacity building and strengthening for antimicrobial resistance surveillance.
Author information
Authors and Affiliations
Contributions
SI planned study and performed phenotypic data collection of results while ZH, JA, SA & AK & NG conducted molecular analysis and bioinformatics. FQ contributed in provision of clinical information and approved the final manuscript. SI & ZH contributed in manuscript writing, while RH & SN, NG & FQ reviewed the script. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved from institutional ethical board review of Aga Khan University (ERC No: 2019–0410-4188).
Consent for publication
Written informed consent was obtained from study participant to publish this information.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been updated to correct an author name.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Irfan, S., Hasan, Z., Qamar, F. et al. Ceftriaxone resistant Salmonella enterica serovar Paratyphi A identified in a case of enteric fever: first case report from Pakistan. BMC Infect Dis 23, 267 (2023). https://doi.org/10.1186/s12879-023-08152-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08152-9