Abstract
Background
Indwelling urinary tract catheters (UTC) are a well-known risk factor for urinary tract infections (UTI). Because geriatric patients are at high risk of infection, an intervention with a focus on appropriate and minimal UTC use was introduced in 4 acute care geriatric wards.
Methods
Between 11/2018 and 1/2020, unit-based data on UTC use and nosocomial UTI was collected in accordance with the methods of the German national surveillance system KISS. From 6/2019 to 1/2020, a champion-led intervention was implemented which focused on: (i) feedback of surveillance data, (ii) education and training in aseptic UTC insertion and maintenance, (iii) HCW’s daily assessment of UTC necessity based on a checklist and (iv) timely removal of unnecessary UTCs. UTC use, incidence, and incidence densities for catheter-associated UTI (CAUTI) were calculated before and during the intervention. In addition, we analyzed adherence to a scheduled daily assessment of UTC necessity. Rate ratios (RR) with 95% confidence intervals (95%CI) were calculated. Differences based on the quality of checklist completion were evaluated using the Kruskal Wallis test.
Results
We analyzed the data of 3,564 patients with a total 53,954 patient days, 9,208 UTC days, and 61 CAUTI. Surveillance data showed a significant decrease in the pooled UTC utilization rate from 19.1/100 patient days to 15.2/100 patient days (RR = 0.80, 95%CI 0.77–0.83, p < 0.001). CAUTI per 100 patients dropped from 2.07 to 1.40 (RR = 0.68, 95%CI 0.41–1.12, p = 0.1279). Overall, 373 patients received a UTC during the intervention. Of those patients 351 patients had an UTC ≥ 2 days. The analysis of these patients showed that 186 patients (53%) received a checklist as part of their chart for daily evaluation of UTC necessity. 43 (23.1%) of the completed checklists were of good quality; 143 (76.9%) were of poor quality. Patients in the group whose checklists were of good quality had fewer UTC days (median 7 UTC days IQR (3–11)) than patients whose checklists were of poor quality (11 UTC days IQR (6–16), p = 0.001).
Conclusion
We conclude that a champion-led, surveillance-based intervention reduces the use of UTC among geriatric patients. Further research is needed to determine to what extent the use of checklists in daily medical UTC assessment affects the prevention of CAUTI. The fact that patients whose checklists were completed well had fewer UTC days should encourage a conscientious and thorough daily review of the need for UTC.
Similar content being viewed by others
Background
Nosocomial urinary tract infections (UTIs) are one of the most frequent healthcare-associated infections (HAI) in acute care hospitals and long-term care facilities [1]. UTIs result in an increase in both mortality and antibiotic consumption, especially in multimorbid geriatric patients [2,3,4,5]. Therefore, a reduction in UTIs not only decreases the harm to individual patients, it is also an element in confronting global antimicrobial resistance because it reduces antibiotic consumption [6].
Up to 70% of UTIs can be avoided by adhering to infection control and prevention (IPC) measures [7]. In addition to aseptic technique in urinary tract catheter (UTC) insertion and proper UTC maintenance, the use of UTCs should be restricted to the appropriate medical indications. Although indwelling UTCs are the primary risk factor for nosocomial UTIs, healthcare workers (HCW) are not always aware of the reasons a catheter is being used [8]. Inappropriate use of catheters has also been described in the literature [9].
All of this speaks to the need for greater awareness of the uses of UTC that are strictly indicated medically. In addition to attention to the indications, various IPC guidelines—including the German national IPC guidelines—recommend continuous assessment of UTC necessity in order to minimize patient risk of infection [10,11,12,13]. Several studies have shown the benefit of activities aimed at reducing UTC use and preventing catheter associated UTI (CAUTI) [14,15,16,17]. However, only a few of these interventions have focused on geriatric patients. German national reference data on HAI in non-intensive care units has shown high UTC utilization along with high CAUTI rates on geriatric wards [18]. Hence, our study of CAUTI prevention was conducted specifically in this setting. In order to reduce the risk of CAUTI among geriatric patients, a champion-led intervention study was performed in four acute care geriatric wards. The aim of this study was to provide a surveillance based intervention that would (i) strengthen HCWs’ competence in the prevention of CAUTI and (ii) improve UTC use and care. Because we are not aware of a similar study approach having been carried out in Germany, the feasibility of the project was also assessed.
Methods
Study design and setting
We introduced a single-center surveillance-based interventional quality improvement study with a pre-post design in four non-intensive care geriatric units with a total of about 2,900 admissions per year. All four wards were located in a secondary care teaching hospital with 443 acute care beds. Admission criteria for the four geriatric wards were \(\ge\)65 years of age and multimorbidity, where multimorbidity was defined as the simultaneous occurrence of three diseases or more.
Study intervention
Unit-based data on UTC use and CAUTI was collected from 11/2018 to 1/2020 using methods described in the KISS module “STATIONS-KISS” and in KISS definitions [19, 20]. In brief, device utilization rates and device-associated infection rates are monitored in non-intensive care wards and submitted annually to the German National Reference Center for Surveillance of Nosocomial Infections at Charité-Universitätsmedizin Berlin. The surveillance was performed by an internal medicine resident (LM) following a one-day introductory course at the National Reference Center.
After the conclusion of the first surveillance phase from 11/2018 to 5/2019, surveillance phase 2 began in 6/2019 and was completed in 1/2020. In surveillance phase 2, we implemented an intervention that focussed on (i) the provision of feedback on surveillance data; (ii) education and training of staff in aseptic UTC insertion and maintenance; (iii) the daily assessment of UTC necessity; and, (iv) the timely removal of UTCs judged to be unnecessary.
Intervention measures
Feedback on surveillance data
Feedback on ward-based surveillance data collected during surveillance phase 1 was provided to ward physicians and nursing staff at the beginning of phase 2 in order to explain surveillance methods, to discuss CAUTI rates, and to raise awareness of the necessity of CAUTI prevention.
The content of the feedback included data on UTC utilization and ward-based CAUTI rates. All physicians and nurses of the participating wards were invited to the feedback presentation. Nurses were represented by their respective ward managers (n = 4). In addition, the head physician and the hospital IPC specialist participated as well as all physicians present that day (n = 10). The presentation and discussion of surveillance data were included in an introductory lecture about the intervention.
Education and training in aseptic UTC insertion and maintenance
Education and training in aseptic UTC insertion and maintenance was offered to the nursing staff of each ward in a one-day interactive, theoretical and practical training session. It consisted of a two-hour simulation training session on UTC insertion and maintenance for all HCWs in the participating wards.
Teaching material was developed by LM and SH. It consisted of evidence-based recommendations with a special focus on the critical use of UTCs and the daily assessment of UTC necessity in accordance with national guidelines [11].
Daily assessment of UTC necessity
A checklist was developed to keep a daily record of the indications for each individual UTC. Thus, ongoing documentation of the daily assessment of UTC necessity was performed for every patient with a UTC. The following data was to be recorded on each patient’s checklist on a daily basis: date of UTC insertion, UTC indication, total UTC use in days, and the daily confirmation of UTC indication. The form was to be signed by nursing and medical staff on a daily basis. The checklist was placed in patient charts by nursing staff when a patient with an UTC was admitted to one of the four geriatric wards or once a patient received a UTC during their ward stay.
Timely removal of unnecessary UTCs
Finally, the UTC was removed by nursing staff if the indication was no longer present. At the same time, the physician’s oral or written order for removal was noted.
The intervention was intended for physicians and nursing staff on the participating wards and thus emphasized a team-based approach to CAUTI prevention.
The intervention was champion-led by the first author (LM), who initiated and performed the surveillance and teaching as well as creating and distributing the checklist.
The project was presented to and approved by the geriatric department and hospital IPC management.
Endpoints
The primary endpoints were changes in UTC use and CAUTI in the four participating wards. For this purpose, data was analyzed in accordance with KISS methods [19].
The secondary endpoint was adherence to a checklist, as defined in the quality of use of patients’ individual checklists.
Well-completed checklists were defined as checklists that included a documented UTC indication and at least 80% evidence of daily assessment. Poorly completed checklists were defined as checklists without at least 80% evidence of daily assessment.
Data collection
Data on patient days, UTC days, and CAUTIs was collected before and during the intervention.
Statistical analysis
UTC utilization rate was calculated as a ratio of UTC days per 100 patient days. CAUTI rates were calculated in accordance with KISS methods as the ratio of CAUTIs per 100 patients (incidence) and per 1000 patient days and/or per 1000 UTC days (incidence densities). Comparison of the UTC utilization rates, incidences, and incidence densities of CAUTI before and during the intervention was performed by calculating rate ratios (RR) with 95% confidence intervals (95%CI).
In a sub-analysis, CAUTI incidences and incidence densities were calculated according to the quality of checklists of patients who had a UTC for at least 2 days. The analysis of the checklists was restricted to this group of patients because device use during the 48 h preceding the onset of infection is required by the definition of a device-associated infection [19]. Rate ratios with 95%CI were calculated in order to investigate the effect of a well-completed checklist or no checklist on CAUTI compared to a poorly completed checklist. We tested how the number of UTC days differed between patients with a poorly completed, a well completed, or with no checklist using the Kruskal Wallis test.
All statistical tests were performed at an alpha level of 0.05. Two-tailed p-values and 95% confidence intervals are reported for all rate ratios.
Statistical analyses were conducted with the help of SPSS (IBM SPSS Statistics 27.0) and R software (version 4.0.3).
Ethical considerations
All data was collected in accordance with KISS methods and was obtained during routine surveillance as required by the German Protection against Infection Act (Infektionsschutzgesetz, IfSG). § 23 of the IfSG requires hospitals to systematically collect and analyze data on hospital-acquired infections (HAIs) [21]. Ethical approval and informed consent were thus not required.
Results
Overall, the study surveyed the data of 3,564 patients with 53,954 patient days, 9,208 UTC days, and 61 CAUTIs. As summarized in Table 1, we analyzed data from 1,640 patients with 34 CAUTIs in surveillance phase 1 and 1,924 patients with 27 CAUTIs during the intervention in surveillance phase 2.
Of the 1,924 patients analyzed during the intervention, 373 (19.4%) received a UTC. Further analysis of the 351 patients with a UTC ≥ 2 days showed that 186 patients received a checklist (53%). Of these checklists, the quality of 43 (23.1%) was good and of 143 (76.9%) was poor. The use of the checklist varied among the individual wards, with the percentage of good quality checklists ranging from 7 to 22%.
Non-use of the checklist varied between 23% and 65% (table in the supplement).
The pooled UTC use decreased significantly from the baseline 19.12 UTC days per 100 patient days in surveillance phase 1 to 15.24 UTC days per 100 patient days during the intervention period (p < 0.001).
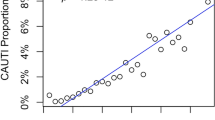
As regards the pooled infection rates, the rate of CAUTI in relation to device days decreased from 6.99 to 6.21 CAUTIs per 1000 UTC-days (p = 0.6492) which corresponds to a rate ratio of 0.89 (CI95% 0.53–1.47). CAUTIs per 100 patients decreased from 2.07 to 1.40 (p = 0.1279), which corresponds to a rate ratio of 0.68 (CI95% 0.41–1.12) (Table 1; Fig. 1).
As summarized in Table 2, median UTC use was highest in the group of patients with checklists that were poorly completed (11 UTC days, IQR 6–16), followed by the group which did not use a checklist (10 UTC days, IQR 7–16). The lowest UTC use was seen in patients with well completed checklists (7 UTC days, IQR 3–11). Correspondingly, the CAUTI rate per 100 patients was lowest in patients with well-completed checklists (4.65 CAUTI per 100 patients) and highest in patients with poorly-completed checklists (8.39 CAUTI per 100 patients). The group of patients for whom a checklist was not used had a UTI rate of 6.67 CAUTIs per 100 patients.
Discussion
The data shows that it was possible to achieve the aim of using devices critically with geriatric patients and this led to a significant reduction in UTC utilization. A reduction is best achieved when initial rates of use are relatively high. Participating wards had a baseline UTC utilization rate above the median but below the 75th percentile, and they were able to reduce their rate to below the median reference utilization rate in comparison to national reference data from 66 German geriatric wards which showed a median UTC use of 16.01/100 pd (IQR 12.9–20.2) [18].
This pronounced reduction could not be demonstrated for infection rates. Here the baseline level was also above the median and below the 75th percentile of national reference data. However, a reduction below the median did not occur. It should be taken into account that a pre-post-comparison of device-associated infection rates may mask the impact of a successful intervention since these rates are affected by reduced device utilization [22]. Therefore, we also analyzed CAUTIs in relation to patients and patient days, although this approach does not incorporate the optimal risk adjustment.
A reduction of almost one-third was observed in the incidence of CAUTIs per 100 patients, but this reduction was not significant, most likely because of the small sample size.
Demonstrating such a reduction with our baseline incidence would have required a sample size of 13,216 patients (6,608 per period).
There are several studies which have described a positive effect of focusing on the critical use of UTCs [16, 17, 23,24,25]. Thus, our results are in line with other research in the literature. They also include some additional findings: The use of the checklist varied among the wards while the percentage of checklists of good documentation quality was lower than that of checklists of poor quality. The stratified analysis of documentation quality demonstrated a better outcome for patients with well-completed checklists in comparison to patients with poorly completed checklists.
The association of high UTC utilization and high CAUTI rates in patients with poorly completed checklists should be further investigated. It is possible that the presence of the checklist reassured individual HCWs that something was being done to prevent CAUTI and that, as a result, those workers did not consider conscious engagement with the catheter necessary.
Interestingly, the group of patients with no checklist in their chart had lower CAUTI rates than patients with poorly completed daily documentation. Since the lack of a checklist for some patients was observable in all four wards, the decision not to keep a checklist must have been individual rather than ward-based. To what extent patient-related factors influenced such a decision could not be analyzed in our study.
Many authors describe the use of checklists or reminders as helpful for UTI prevention, but only a few have analyzed the extent of adherence. Thus far, Giles et al. have described documented indications for catheter insertion for the majority of their patients. However the percentage of reviews of the necessity of UTCs were far lower [16]. To what extent higher adherence can be achieved has not yet been clearly shown.
Successful nurse-driven or nurse-led interventions for UTI reduction have been described for the US and Australia. But these results must always be interpreted in connection with the organizational particularities of the respective health systems of those countries [16, 17].
Reynolds et al. described a 4-year sustained reduction in UTI rates achieved with a multifaceted strategy led by champions. However, the numbers and professions of those champions were not specified [26]. The intervention described here was also led by a champion—a resident with training in internal medicine who was highly motivated to prevent infection. This champion initiated and performed the surveillance and training as well as creating and implementing the checklist in the four wards. It was not possible to assess the extent to which other HCWs in the participating wards acted as local champions. Hence, in our study we speak of a single lead champion.
Champions play an essential role in implementation. However, Shaw et al. differentiate between project champions, who are associated with specific projects, and organizational change champions, who lead change for an entire organization [27, 28]. Damschroder et al. emphasize the importance of intrinsic motivation and enthusiasm in IPC for successful champions, and noted that their effectiveness is influenced by the quality of organizational networks [29]. In our view, this underscores a motivated champion’s positive influence on UTC utilization and the reduction of infection rates described in our study.
The gaps we identified in adherence to the checklist protocol were most likely due to the fact that the champion was predominantly a project champion rather than an organizational change champion.
The number of poorly completed and unused checklists might have been lower had there been more support at the organizational level, not only because hard-to-influence HCWs might be better reached by organizational change champions, but also because champions might take advantage of organizational support to increase the commitment of HCWs [30].
This study had a few limitations. Since it was surveillance-based at the ward-level, we were not able to analyze individual patient-based data. In addition, the activities and effects of the champion were not further analyzed as recommended very recently by Shea [30]. Because our study was primarily a feasibility study, we did not focus on follow-up and did not obtain data on the intervention’s sustainability.
Conclusion
In conclusion, our study shows clear potential for CAUTI prevention in non-ICU geriatric patients. Although at first sight, the intervention appeared quite easy, a checklist was not kept for every patient and checklists were not always well kept. Since our results indicate that thorough documentation results in a benefit for patient outcomes, a high rate of adherence to structured daily assessment of UTC necessity should be a goal in geriatric patient care. To what extent clinical champions can promote long-lasting implementation of CAUTI prevention in acute care hospitals must be studied further.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Suetens C, Latour K, Kärki T, Ricchizzi E, Kinross P, Moro ML et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Eurosurveillance 2018, 23(46):1800516.
Saint S. Clinical and economic consequences of nosocomial catheter-related bacteriuria. Am J Infect Control. 2000;28(1):68–75.
Tchouaket Nguemeleu E, Beogo I, Sia D, Kilpatrick K, Seguin C, Baillot A, et al. Economic analysis of healthcare-associated infection prevention and control interventions in medical and surgical units: systematic review using a discounting approach. J Hosp Infect. 2020;106(1):134–54.
Holroyd-Leduc JM, Sen S, Bertenthal D, Sands LP, Palmer RM, Kresevic DM, et al. The relationship of indwelling urinary catheters to death, length of hospital stay, functional decline, and nursing home admission in hospitalized older medical patients. J Am Geriatr Soc. 2007;55(2):227–33.
Polites SF, Habermann EB, Thomsen KM, Amr MA, Jenkins DH, Zietlow SP, et al. Urinary tract infection in elderly trauma patients: review of the Trauma Quality Improvement Program identifies the population at risk. J Trauma Acute Care Surg. 2014;77(6):952–9.
Naghavi M. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–55.
Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. 2011;32(2):101–14.
Saint S, Wiese J, Amory JK, Bernstein ML, Patel UD, Zemencuk JK, et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med. 2000;109(6):476–80.
Hu FW, Yang DC, Huang CC, Chen CH, Chang CM. Inappropriate use of urinary catheters among hospitalized elderly patients: clinician awareness is key. Geriatr Gerontol Int. 2015;15(12):1235–41.
Hooton TM, Diagnosis, Prevention, Treatment of Catheter-Associated Urinary Tract Infection in Adults. and : 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clinical Infectious Diseases, Volume 50, Issue 5, 1 March 2010, Pages 625–663 01 March 2010.
Kommission für Krankenhaushygiene und Infektionsprävention. Prävention und Kontrolle Katheter-assoziierter Harnwegsinfektionen: Empfehlung der Kommission für Krankenhaushygiene und Infektionsprävention (KRINKO) beim Robert Koch-Institut. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2015;58(6):641–50.
Lo E, Nicolle LE, Coffin SE, Gould C, Maragakis LL, Meddings J, et al. Strategies to Prevent Catheter-Associated urinary tract infections in Acute Care Hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(5):464–79.
Healthcare infection control practices advisory commitee. Guideline for prevention of catheter-associated urinary tract infections 2009. https://www.cdc.gov/infectioncontrol/pdf/guidelines/cauti-guidelines-H.pdf. Accessed 1 Dec 2022.
Meddings J, Rogers MA, Krein SL, Fakih MG, Olmsted RN, Saint S. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: an integrative review. BMJ Qual Saf. 2014;23(4):277–89.
Fakih MG, Pena ME, Shemes S, Rey J, Berriel-Cass D, Szpunar SM, et al. Effect of establishing guidelines on appropriate urinary catheter placement. Acad Emerg Med. 2010;17(3):337–40.
Giles M, Graham L, Ball J, King J, Watts W, Harris A, et al. Implementation of a multifaceted nurse-led intervention to reduce indwelling urinary catheter use in four australian hospitals: a pre- and postintervention study. J Clin Nurs. 2020;29(5–6):872–86.
Tyson AF, Campbell EF, Spangler LR, Ross SW, Reinke CE, Passaretti CL, et al. Implementation of a nurse-driven protocol for catheter removal to decrease Catheter-Associated urinary tract infection rate in a Surgical Trauma ICU. J Intensive Care Med. 2018;35(8):738–44.
Krankenhaus-Infektions-Surveillance-Systems (KISS). Modul STATIONS-KISS, Referenzdaten Berechnungszeitraum. Januar 2017 bis Dezember 2020.2021. https://www.nrz-hygiene.de/files/Referenzdaten/STATIONS/Infektionen/201701_202012_DeviceRef.pdf. Accessed 1 Dec 2022.
Krankenhaus-Infektions-Surveillance-System (KISS). Surveillance Device-assoziierter nosokomialer Infektionen auf Normalpflegestationen/ Nicht-Intensivstationen.2016. https://www.nrz-hygiene.de/files/Referenzdaten/STATIONS/Infektionen/201701_202012_DeviceRef.pdf. Accessed 1 Dec 2022.
Krankenhaus-Infektions-Surveillance-System (KISS). Definitionen nosokomialer Infektionen für die Surveillance im Krankenhaus-Infektions-Surveillance-System (KISS-Definitionen).2017. www.nrz-hygiene.de/files/KISS-Definitionen/KISS_Definitionen_E-Book_Neuauflage_06_2017.pdf. Accessed 1 Dec 2022.
Bundesamt für Justiz. Gesetz zur Verhütung und Bekämpfung von Infektionskrankheiten beim Menschen (Infektionsschutzgesetz - IfSG).2000. www.gesetze-im-internet.de/ifsg/BJNR104510000.html. Accessed 1 Dec 2022.
Wright MO, Kharasch M, Beaumont JL, Peterson LR, Robicsek A. Reporting catheter-associated urinary tract infections: denominator matters. Infect Control Hosp Epidemiol. 2011;32(7):635–40.
Saint S, Kaufman SR, Thompson M, Rogers MA, Chenoweth CE. A reminder reduces urinary catheterization in hospitalized patients. Jt Comm J Qual Patient Saf. 2005;31(8):455–62.
Au AG, Shurraw S, Hoang H, Wang S, Wang X. Effectiveness of a simple intervention for prevention of catheter-associated urinary tract infections on a medical hospital unit. J Infect Prev. 2020;21(6):221–7.
Nassikas NJ, Monteiro JFG, Pashnik B, Lynch J, Carino G, Levinson AT. Intensive care unit rounding checklists to reduce catheter-associated urinary tract infections. Infect Control Hosp Epidemiol. 2020;41(6):680–3.
Reynolds SS, Sova CD, Lewis SS, Smith BA, Wrenn RH, Turner NA et al. Sustained reduction in catheter-associated urinary tract infections using multi-faceted strategies led by champions: A quality improvement initiative.Infect Control Hosp Epidemiol2021:1–5.
Hendy J, Barlow J. The role of the organizational champion in achieving health system change. Soc Sci Med. 2012;74(3):348–55.
Shaw EK, Howard J, West DR, Crabtree BF, Nease DE Jr, Tutt B, et al. The role of the champion in primary care change efforts: from the State Networks of Colorado Ambulatory Practices and Partners (SNOCAP). J Am Board Fam Med. 2012;25(5):676–85.
Damschroder LJ, Banaszak-Holl J, Kowalski CP, Forman J, Saint S, Krein SL. The role of the champion in infection prevention: results from a multisite qualitative study. Qual Saf Health Care. 2009;18(6):434–40.
Shea CM. A conceptual model to guide research on the activities and effects of innovation champions.Implement Res Pract2021,2.
Acknowledgements
The authors acknowledge Gerald Brennan for editorial assistance.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
LM, DZM, SH and PG formulated the research question and conceived the intervention. LM introduced the surveillance and intervention. LM, SS and FS performed the data analysis. LM drafted the manuscript with the input of all other authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Only aggregated and anonymous data that were collected in accordance with § 23 of the German “Protection against Infection Act” were analyzed. Thus, ethical approval and informed consent were not required and institutional review boards were not consulted.
Consent to publish
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mrziglod, L., Saydan, S., Schwab, F. et al. Reducing urinary catheter use in geriatric patients - results of a single-center champion-led intervention. BMC Infect Dis 23, 94 (2023). https://doi.org/10.1186/s12879-023-08064-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08064-8