Abstract
Background
Candidemia is increasing in frequency and is associated with high mortality. We sought to determine the burden of illness, the population it affects and its resistance profile in our region.
Methods
The Calgary Zone (CZ) provides all care for residents of Calgary and surrounding communities (~ 1.69 million) via five tertiary hospitals each served by a common single laboratory for acute care microbiology. All adult patients in the CZ with at least one Candida spp.-positive blood culture between January 1, 2010, and December 31, 2018, were identified using microbiological data from Calgary Lab Services, the laboratory that processes > 95% of all blood culture samples in the CZ, were reviewed for the study.
Results
The overall annual incidence of candidemia among individuals living in the CZ was 3.8 per 100,000 persons (Median age 61 years (IQR 48–72) and 221/455 (47.4%) were female). C. albicans was the most common species (50.6%), followed by C. glabrata, (24.0%). No other species accounted for more than 7% of cases. Overall mortality at 30, 90, and 365 days was 32.2, 40.1, and 48.1% respectively. Mortality rate did not differ by Candida species. Of individuals who developed candidemia, more than 50% died within the next year. No new resistance pattern has emerged in the most common Candida species in Calgary, Alberta.
Conclusions
In Calgary, Alberta, the incidence of candidemia has not increased in the last decade. C. albicans was the most common species and it remains susceptible to fluconazole.
Similar content being viewed by others
Background
Candidemia is a common cause of hospital-acquired bloodstream infection, with ~ 22,660 cases of candidemia annually in the United States and an estimated overall annual incidence of 7.0 cases per 100,000 persons [1,2,3]. Increased medical devices, immunosuppression and broad-spectrum antimicrobials have increased the incidence [4]. Mortality can exceed 40%, with marginal improvement over the last decade despite novel antifungals [5,6,7,8]. Hospitalizations complicated by invasive candidiasis cost > $1 billion USD/year in the USA [9].
A shift from Candida albicans to Candida non-albicans spp. fungemia has increased infections resistant to first-line azoles with global emergence of Candida auris causing concerns regarding antifungal resistance and increased mortality [10,11,12]. The Infectious Diseases Society of America (IDSA) published its inaugural recommendations for treating candidiasis in 2000, followed by three updates, primarily to describe newer and less toxic systemic antifungals (i.e., echinocandins).
Current objectives were to characterize: (1) the burden of candidemia in Calgary; (2) those that develop candidemia; and (3) Candida antimicrobial resistance (AMR) from 2010 to 2018.
Methods
Study setting and data sources
The Calgary Zone (CZ) provides comprehensive medical and surgical care to 1.69 million individuals in Calgary and surrounding communities, in Alberta, Canada, except for acute heart, liver and lung surgical transplants. We report a 9-year population-based study of candidemia epidemiology. The CZ includes four medical centres: Foothills Medical Centre, Peter Lougheed Centre, Rockyview General Hospital, and South Health Campus. Patient characteristics and medical information were retrieved (Sunrise Clinical Manager, Discharge Abstract Database, National Ambulatory Care Reporting System, Provincial Registry and Pharmaceutical Information Network). All patients were assigned a unique code to ensure anonymity, data were stored on a secure University of Calgary (UofC) with double password protection and accessed only by study investigators. The Conjoint Health Research Ethics Board approved the study with a waiver for informed consent (REB18-1659).
Patients
All adults (age ≥ 18) in the CZ with at least one Candida spp.-positive blood culture from January 1, 2010, to December 31, 2018, were included, based on microbiological data from Calgary Lab Services, the laboratory that processes > 95% of all blood culture samples. The index blood culture and onset of candidemia was defined as the first positive blood culture. Data were merged on unique ID and candidemia characteristics (source of infection, duration, complications, treatments, etc.). Multiple episodes with the same Candida species were considered separate events if there was at least 30 days between occurrences and blood culture cleared between episodes. Duration of candidemia was defined as the interval from the last positive blood culture to the first negative culture. Clearance was documented when there was a negative blood culture for Candida not followed by further blood cultures containing it. Chart reviews ensured the first registered candidemia episode from January 2010 to March 2010 was unrelated to a previous event. Admission data and risk factors for candidemia were recorded. Electronic Medical Records (EMR) were reviewed for each patient by infectious disease clinicians (SBB, JCL and DBG). Community-onset candidemia which includes healthcare-associated and community-acquired candidemia was defined if the organism was isolated within 48 h after initial hospitalization and not attributable to prior hospitalization. Recurrence of infection was established based on review of available information from the EMR.
Detailed chart reviews were conducted, capturing patient demographics and comorbidities, disposition of hospitalization, biochemical and microbiology data at incident blood culture draw, investigations, metastatic phenomenon, antimicrobial and immunosuppressive usage, and clinical outcomes. For patients transferred to the CZ, postal code was used to verify CZ residence. The CZ includes four hospitals with one site acting as the centre for all transplantation within the zone consisting of hematological and renal transplantation only. Each of the hospitals is equipped with an intensive care unit.
Laboratory analyses
Blood cultures were incubated for 5 d in BacTAlert™ FA and FN blood culture bottles (BioMerieux, Montreal, Canada) [13]. From 2010 to 2014, on-site identification used germ tube testing, morphology on Cornmeal Blue Agar and Vitek 2 YST ID card (BioMérieux, Montreal, QC, Canada) or API-20C AUX System (BioMérieux, Montreal, QC, Canada) [14, 15]. Thereafter, identification was primarily matrix-assisted laser desorption/ionization Vitek-MS™ (BioMérieux, Montreal, QC, Canada), plus phenotypic identification and Vitek 2 YST ID cards when MALDI-TOF did not provide identification. Sensititre YeastOne Y-05 colorimetric broth microdilution panels (Trek Diagnostic Systems Inc, Cleveland, OH, USA) were used for susceptibility testing, following package insert and Clinical Laboratory Standard Institute (CLSI) M60 protocols with supplementation from Pfaller et al. if the Candida species lacked CLSI breakpoint or epidemiological cut-off value (ECV) [16,17,18]. For epidemiological cut-offs, Candida isolates were labelled as wild type (WT), or non-wild type (NWT) based on CLSI definition [17].
Statistical analyses
Regional dashboard data from Alberta.ca were used to determine the CZ population to calculate annual incidence rates [19]. Differences in the incidence of the six most common Candida species were tested using a Poisson regression model, with number of candidemia patients as the outcome variable and year as a continuous explanatory variable and annual total population size added as exposure.
Differences between hospital- and community-onset candidemia regarding occurrence of co-morbidities were tested using equality of proportions. A multilevel logistic regression model was used, with isolates classified susceptible or resistant. Hospital site was a fixed effect to correct for patients within a hospital who are potentially more alike in terms of antimicrobial susceptibility than patients between hospitals.
Normally distributed variables were reported as means with standard deviations (SD) whereas non-normally distributed data were reported as medians with inter-quartile ranges (IQR). All data manipulations and analyses used STATA (Stata Corp, 2015, Stata: release 16). Statistical significance was P ≤ 0.05.
Results
Incidence
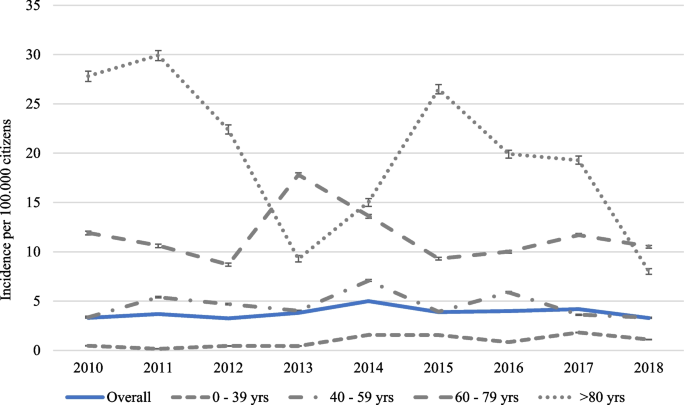
Overall annual incidence of candidemia among patients living in the CZ was 3.8 per 100,000 population, ranging from 3.2 per 100,000 in 2012 to 5.0 per 100,000 in 2014 (P < 0.001; Fig. 1). Incidence changed throughout the study but did not differ between start and end (P = 0.54). The annual incidence among patients between 0 and 39 years was generally low, ranging between 0.2 and 1.8 per 100,000, and increased during the study period (P < 0.01) (Fig. 1). The annual incidence among patients between 40 and 59 years was steadily low and ranged between 3.3 and 7.1 per 100,000. The annual incidence among patients between 60 and 79 years and > 80 years fluctuated more and was higher, ranging between 8.7 and 17.8 per 100,000 and 8.0–29.9 per 100,000, with no significant changes over the study period.
Patient demographics
In total, 455 individuals with 466 episodes of candidemia were analysed. Patients with multiple episodes had events separated by 692 days (IQR 403–852). Median age was 61 years (IQR 48–72), ranging from 19 to 100 years, and 47.4% of the patients were female (Table 1). Median hospital stay was 28 d (IQR: 14–55 d), ranging from 0 to 1470 d, with 53.7% getting ICU support. In total, 16.7% of patients were transferred to CZ from another hospital; based on postal code, 44 non-Calgary residents were excluded from incidence calculations. Most patients were discharged from the hospital (54.9%), 42.1% died before discharge and some left the hospital against medical advice (2.6%) or were transferred to another hospital (0.2%). Most (n = 366, 78.5%) patients were treated with antimicrobials 30 d before candidemia, approximately half (48.5%) had cardiovascular disease as a comorbidity and approximately one-quarter had diabetes, chronic liver disease, pulmonary disease, or cancer (Table 1).
Candidemia
Approximately 23.4% of Candida bloodstream infections were community acquired, with the remainder hospital acquired. Overall, patient demographics were similar between groups, although patients with hospital-acquired candidemia were more likely to have cardiovascular disease (51.3 vs. 39.5%; P = 0.03), specifically congestive heart failure (17.7 vs. 4.6%; P < 0.001) and arrhythmia (27.5 vs. 11.0%; P < 0.01), but less likely to have peripheral vascular disease (3.6 vs. 10.0%; P = 0.01). In addition, hospital-onset candidemia more often had cancer in the last year (25.8 vs. 14.7%; P = 0.02), were receiving parenteral nutrition (20.7 vs. 1.8%; P < 0.001) or received ≥ 10 mg prednisone equivalent of corticosteroids daily for the last 30 days (30.3 vs. 15.6%; P < 0.01)[20]. Asthma was more apparent in community-onset candidemia infections (9.2 vs. 3.9%; P = 0.03) (Table 1).
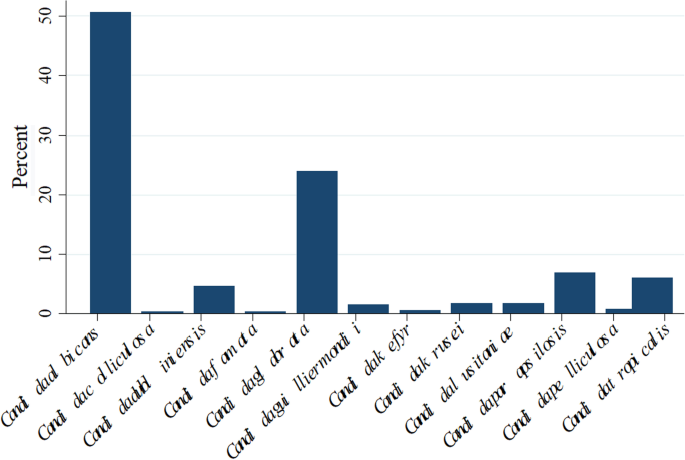
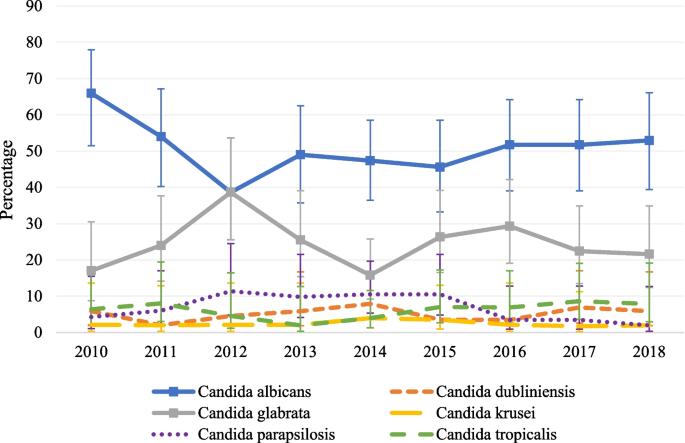
The most common isolated species were C. albicans (50.6%) and C. glabrata (24.0%) (Fig. 2). An infection with a second and different species of Candida isolated > 2 d after the first positive culture occurred in 5.8% of the cases. In 32% of these cases, patients got an infection with C. albicans and C. glabrata. No other trends were observed. The relative proportion of the six most common Candida species (C. albicans, C. glabrata, C. parapsilosis, C. dubliniensis, C. krusei and C. tropicalis) did not change over time, apart from a transient decrease in C. albicans between 2010 and 2012 (P = 0.02) and a significant increase in C. glabrata infections (P = 0.03). (Fig. 3).
Mortality
Forty-four (9.4%) of patients with candidemia died within 24 h after the index blood culture and were excluded from analyses. For the remaining 422 patients, all-cause mortality rate at 30 d, 90 d and 1 y post candidemia was 32.2% (95% CI: 27.7–36.7%), 40.1% (95% CI: 35.4–44.8%) and 48.1% (95% CI: 43.3–52.9%), respectively. The all-cause mortality rate at 30 d, 90 d and 1 y post candidemia was generally higher in the patient group with hospital acquired candidemia infections than the community-onset group (35.7 vs. 21.0%, P < 0.01; 42.6 vs. 32.0%, P = 0.06, and 51.9 vs. 36.0%, P < 0.01). When stratifying mortality by the three most common Candida species, the all-cause mortality rate at 30 d, 90 d and 1 year post candidemia did not differ from the overall rate. For C. albicans (n = 218 patients), mortality at 30 d, 90 d and 1 year were 32.1% (95% CI: 25.9–38.3%), 38.5% (95% CI: 32.0–45.0%) and 45.4% (95% CI: 38.8–52.0%), respectively. For C. glabrata (n = 106 patients) mortality at 30 d, 90 d and 1 year were 34.0% (95% CI: 25.0–43.0%), 43.4% (95% CI: 34.0–52.8%) and 55.7% (95% CI: 46.2–65.2%). Finally, for C. parapsilosis, mortality at 30 d, 90 d and 1 year were 26.5% (95% CI: 11.7–41.3%), 38.2% (95% CI: 21.9–54.5%) and 44.1% (95% CI: 27.4–60.8%).
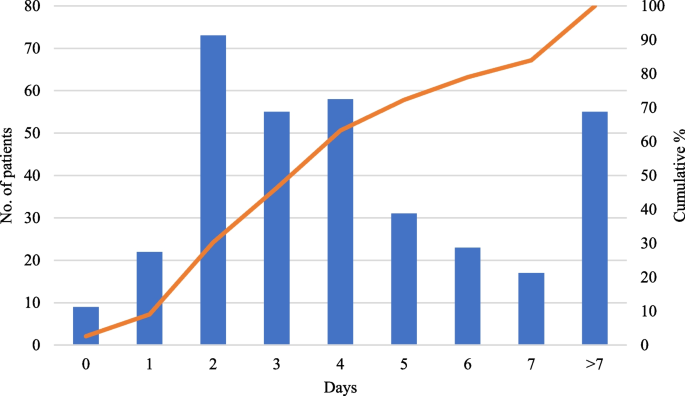
Documented blood culture clearance of Candida spp. from blood occurred in 343 patients, with a median duration of candidemia of 4 d (IQR 2–6 d). Furthermore, 84% of patients cleared their Candidemia in < 7 days (Fig. 4).
Average interval from hospital admission to candidemia diagnosis was 16 d (95% CI: 13–20 d) with a median of 8 d. Readmission within 1 y occurred in 102 patients (21.9%), but this was due to candidemia in only 5 patients (4.9%).
Nine (2.0%) patients had two or more distinct episodes of candidemia during the study period but were classified as unrelated. Most were admitted twice, and 2 were re-admitted 3 times. For these 9 patients, median interval from discharge to readmission was 599 d (IQR 403–852 d), ranging from 48 to 2,026 d.
Antifungal susceptibilities of Candida species causing candidemia
Susceptibility testing was performed for all isolates of C. albicans (n = 242), C. glabrata (n = 117), C. parapsilosis (n = 33) and C. tropicalis (n = 30). Resistance to common antifungals ranged from 0 to 2.5%, and percentage of non-wild types from 0.0 to 9.4% for C. albicans (Table 2). These percentages were slightly higher for C. glabrata (1.0–9.4% and 0.0–7.8%) (P < 0.01; P = 0.63; Table 3) and higher for C. tropicalis isolates ((0.0–31.0% and 0.0–52.9%) (P < 0.001; P < 0.001; Table 4)). No resistance was observed for C. parapsilosis (Table 5). No difference in percentages of susceptible dose dependent (SDD and resistant isolates was observed among the 4 hospitals, except C. glabrata isolates resistant for fluconazole decreased from 5.1 (95% CI: 1.9–10.8%) to 1.2% (95 CI: 0.0–46.9%) after removing one site from the equation (this site had much higher local resistance than the other three sites).
Discussion
Candidemia remains a significant cause of morbidity and mortality [21]; the incidence in the CZ did not change from 2010 to 2018, but it was higher than in 1999 to 2004. [4] In this study, there was a significant difference between mortality in community acquired candidemia and hospital acquired candidemia. These groups of patients differed with patients suffering from hospital acquired candidemia more likely having cancer, receiving parenteral nutrition or having been exposed to steroids. These markers of frailty may explain in part while this group’s mortality was higher. Parenteral nutrition and malignancy were found to be risk factors for candidemia from C. tropicalis in the past [21]. The overall incidence of Candida infections continues to be lower than in other parts of the world [22,23,24]. Candida albicans remains the most common species causing candidemia followed by C. glabrata.[4] However, the proportion of individuals with C. glabrata and its resistance to fluconazole remain relatively low [3, 25]. Furthermore, Alberta has one of the youngest populations in Canada, whereas areas with a higher median age have higher rates of Candidemia [26]. In our study, less recurrence of candidemia occurred compared to a recently published population-based US contemporary cohort [26].
Regarding the discrepancy between echinocandin resistance when comparing micafungin and caspofungin susceptibility profiles for C. glabrata and C. tropicalis, our laboratory stopped reporting caspofungin at the beginning of the last decade due to unreliability in intermediate or resistant results [18]. Thereafter, micafungin susceptibility was used as a surrogate [27]. The C. tropicalis isolates in our study had over 20% resistance to fluconazole. In our study, fluconazole resistance in C. tropicalis was higher than expected. This is consistent with the findings of a Spanish study [28]. In this cohort of patients with C. tropicalis candidemia, 23% of isolates were fluconazole resistance. Their finding and ours suggests possible horizontal transmission within a high-risk population. Resistance to azoles in other settings for this Candida species has been reported to be associated with over expression of ERG11 [29]. Other studies identified solid organ transplantation as a main risk factor for increased candidemia [30]. That acute solid organ transplant surgery and immediate post-operative recovery do not occur in the CZ may artificially lower the incidence. The transient change in proportion of C. albicans was attributed to noise.
Isolates of C. albicans, C. parapsilosis and C. glabrata within the CZ continue to be susceptible to fluconazole, although C. tropicalis which was not reliably susceptible to azoles. Preserved susceptibility of C. parapsilosis and C. glabrata to fluconazole is not reported in other regions, including the United States [31].
Unlike other studies, we did not exclude patients with more than 1 episode when those episodes were separate (demonstrated blood clearance with at least 30 d between episodes) [32]. We felt that the expertise of the infectious disease specialist would allow for proper determination if repeat episodes of candidemia occurred in the same patient were associated with a single episode or separate events. Regardless, the impact was minimal, as only 7 patients had > 1 candidemia episode.
Several limitations are acknowledged. No acute transplant surgical care within the CZ may underestimate the population incidence of candidemia. Incomplete data within the EMR did not allow for calculating a Charlson comorbidity index to adjust for the lack of acute transplant surgical care within the CZ.
The length of candidemia could not always be determined as follow up blood cultures to document clearance were not always collected in relation to their bloodstream infection event. Furthermore, some first negative blood cultures were collected later than recommended by clinical practice guidelines, potentially increasing the duration of the candidemia without altering severity of the infection [33]. However, in 87% of patients the interval from their last positive to their first negative culture was < 3 d, so the effect was likely small.
In summary, in the largest Canadian study on candidemia, incidence was higher than previously measured, but did not increase through the duration of the study. Short- and long-term mortality from candidemia continue to be high. In our study population, resistance to antifungal for C. albicans has not emerged.
Availability of data and materials
The anonymized data are stored securely on the University of Calgary cloud platform It can be made available through reasonable request to corresponding author.
References
Zaoutis TE, Argon J, Chu J, Berlin JA, Walsh TJ, Feudtner C. The epidemiology and attributable outcomes of candidemia in adults and children hospitalized in the United States: a propensity analysis. Clin Infect Dis. 2005;41:1232–9.
Pfaller MA, Diekema DJ, Jones RN, Sader HS, Fluit AC, Hollis RJ, et al. International surveillance of bloodstream infections due to Candida species: frequency of occurrence and in vitro susceptibilities to fluconazole, ravuconazole, and voriconazole of isolates collected from 1997 through 1999 in the SENTRY Antimicrobial Surv. J Clin Microbiol. 2001;39:3254–9.
Tsay SV, Mu Y, Williams S, Epson E, Nadle J, Bamberg WM, et al. Burden of Candidemia in the United States, 2017. Clin Infect Dis. 2020;e449–e453.
Laupland KB, Gregson DB, Church DL, Ross T, Elsayed S. Invasive Candida species infections: a 5 year population-based assessment. J Antimicrob Chemother. 2005;56:532–7.
Corzo-Leon DE, Alvarado-Matute T, Colombo AL, Cornejo-Juarez P, Cortes J, Echevarria JI, et al. Surveillance of Candida spp bloodstream infections: epidemiological trends and risk factors of death in two Mexican tertiary care hospitals. PLoS ONE. 2014;9: e97325.
Al-Rawahi GN, Roscoe DL. Ten-year review of candidemia in a Canadian tertiary care centre: predominance of non-albicans Candida species. Can J Infect Dis Med Microbiol. 2013;24:e65–8.
Raja NS. Epidemiology, risk factors, treatment and outcome of Candida bloodstream infections because of Candida albicans and Candida non-albicans in two district general hospitals in the United Kingdom. Int J Clin Pract. 2021;75: e13655.
MacPhail GLP, Taylor GD, Buchanan-Chell M, Ross C, Wilson S, Kureishi A. Epidemiology, treatment and outcome of candidemia: a five-year review at three Canadian hospitals. Mycoses. 2002;45:141–5.
Benedict K, Jackson BR, Chiller T, Beer KD. Estimation of direct healthcare costs of fungal diseases in the United States. Clin Infect Dis. 2019;68:1791–7.
Spivak ES, Hanson KE. Candida auris: an emerging fungal pathogen. J Clin Microbiol. 2018;56.
Kim EJ, Lee E, Kwak YG, Yoo HM, Choi JY, Kim SR, et al. Trends in the epidemiology of candidemia in intensive care units from 2006 to 2017: results from the Korean National Healthcare-Associated Infections Surveillance System. Front Med (Lausanne). 2020;7:606976–606976.
Horn DL, Neofytos D, Anaissie EJ, Fishman JA, Steinbach WJ, Olyaei AJ, et al. Epidemiology and outcomes of Candidemia in 2019 patients: data from the Prospective Antifungal Therapy Alliance Registry. Clin Infect Dis. 2009;48:1695–703.
Ericson EL, Klingspor L, Ullberg M, Özenci V. Clinical comparison of the Bactec Mycosis IC/F, BacT/Alert FA, and BacT/Alert FN blood culture vials for the detection of candidemia. Diagn Microbiol Infect Dis. 2012;73:153–6.
Garcia LS. Clinical microbiology procedures handbook. 3rd ed. Washington, D.C: ASM Press; 2010.
Leber AL. Clinical microbiology procedures handbook. 4th ed. Washington, DC: ASM Press; 2016.
Pfaller MA, Diekema DJ. Progress in antifungal susceptibility testing of Candida spp. by use of Clinical and Laboratory Standards Institute broth microdilution methods, 2010 to 2012. J Clin Microbiol. 2012;50:2846–56.
CLSI. Epidemiological cutoff values for antifungal susceptibility testing, 3rd edn. Clinical and Laboratory Standards Institute. 2020.
CLSI. Performance standards for antifungal susceptibility testing of yeasts, 2nd edn. Clinical and Laboratory Standards Institute. 2020.
Calgary—Population. 2022. https://regionaldashboard.alberta.ca/region/calgary/population/#/?from=2001&to=2019. Accessed 28 Aug 2022.
McCarty TP, White CM, Pappas PG. Candidemia and invasive Candidiasis. Infect Dis Clin N Am. 2021;35:389–413.
Muñoz P, Giannella M, Fanciulli C, Guinea J, Valerio M, Rojas L, et al. Candida tropicalis fungaemia: incidence, risk factors and mortality in a general hospital. Clin Microbiol Infect. 2011;17:1538–45.
Magill SS, O’Leary E, Janelle SJ, Thompson DL, Dumyati G, Nadle J, et al. Changes in prevalence of health care-associated infections in US hospitals. N Engl J Med. 2018;379:1732–44.
Koehler P, Stecher M, Cornely OA, Koehler D, Vehreschild MJGT, Bohlius J, et al. Morbidity and mortality of candidaemia in Europe: an epidemiologic meta-analysis. Clin Microbiol Infect. 2019;25:1200–12.
Tsay S, Williams S, Mu Y, Epson E, Johnston H, Farley MM, et al. 363. National Burden of Candidemia, United States, 2017. Open Forum Infect Dis. 2018;5(suppl1):S142–3.
Guinea J. Global trends in the distribution of Candida species causing candidemia. Clin Microbiol Infect. 2014;20:5–10.
Seagle EE, Jackson BR, Lockhart SR, Jenkins EN, Revis A, Farley MM, et al. Recurrent Candidemia: trends and risk factors among persons residing in 4 US States, 2011–2018. Open Forum Infect Dis. 2022;9:ofac545.
Pfaller MA, Messer SA, Diekema DJ, Jones RN, Castanheira M. Use of Micafungin as a surrogate marker to predict susceptibility and resistance to Caspofungin among 3,764 clinical isolates of Candida by use of CLSI methods and interpretive criteria. J Clin Microbiol. 2014;52:108.
Fernández-Ruiz M, Puig-Asensio M, Guinea J, Almirante B, Padilla B, Almela M, et al. Candida tropicalis bloodstream infection: incidence, risk factors and outcome in a population-based surveillance. J Infect. 2015;71:385–94.
Wang D, An N, Yang Y, Yang X, Fan Y, Feng J. Candida tropicalis distribution and drug resistance is correlated with ERG11 and UPC2 expression. Antimicrob Resist Infect Control. 2021;10:54.
Kim EJ, Lee E, Kwak YG, Yoo HM, Choi JY, Kim SR, et al. Trends in the epidemiology of Candidemia in intensive care units from 2006 to 2017: results from the Korean National Healthcare-Associated Infections Surveillance System. Front Med (Lausanne). 2020;7.
Toda M, Williams SR, Berkow EL, Farley MM, Harrison LH, Bonner L, et al. Population-based active surveillance for culture-confirmed Candidemia—four sites, United States, 2012–2016. MMWR Surveill Summ. 2019;68:1–17.
Cuervo G, Garcia-Vidal C, Puig-Asensio M, Merino P, Vena A, Martín-Peña A, et al. Usefulness of guideline recommendations for prognosis in patients with candidemia. Med Mycol. 2019;57:659–67.
Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, et al. Clinical practice guideline for the management of Candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:e1-50.
Acknowledgements
This study was presented virtually as a poster at the annual conference of ESCMID in July 2021.
Funding
This study was supported by the Industrial Research Chair in Infectious Diseases of Dairy Cattle, funded by Canada's Natural Sciences and Engineering Research Council (NSERC) Industrial Research Chair Program (Ottawa, ON, Canada), with industry contributions from Alberta Milk (Edmonton, AB, Canada), the Dairy Farmers of Canada (Ottawa, ON, Canada), Westgen Endowment Fund (Milner, BC, Canada), the BC Dairy Association (Burnaby, BC, Canada), Canadian Dairy Network (Guelph, ON, Canada), CanWest DHI (Guelph, ON, Canada), SaskMilk (Regina, SK, Canada), Dairy Farmers of Manitoba (Winnipeg, MB, Canada) and MSD Animal Health (Kirkland, QC, Canada).
Author information
Authors and Affiliations
Contributions
S.B.B., J.C.L., M.D.P., D.C., J.C., and D.B.G. participated in study design. S.B.B., J.C.L., A.K. and D.B.G. have participated in data collection. S.B.B., M.M.B., H.W.B. and D.B.G. participated in the writing of the manuscript. M.M.B. and S.B.B. participated in data analysis. S.B.., M.M.B., J.C.L., A.K., D.C., J.C., B.D., M.D.P., H.W.B., and D.B.G. participated in the review and editing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Conjoint Health Research Ethics Board approved the study protocols (REB18-1659). All methods were performed in accordance with relevant guidelines and regulations. The Conjoint Health Research Ethics Board approved the study with a waiver for informed consent (REB18-1659).
Consent for publication
Not applicable.
Competing interests
The authors confirm there are no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bourassa-Blanchette, S., Biesheuvel, M.M., Lam, J.C. et al. Incidence, susceptibility and outcomes of candidemia in adults living in Calgary, Alberta, Canada (2010–2018). BMC Infect Dis 23, 100 (2023). https://doi.org/10.1186/s12879-023-08050-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08050-0