Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic continues to evolve. Globally, COVID-19 continues to strain even the most resilient healthcare systems, with Omicron being the latest variant. We made a thorough search for literature describing the effects of the COVID-19 in a high human immunodeficiency virus (HIV)/tuberculosis (TB) burden district-level hospital setting. We found scanty literature.
Methods
A retrospective observational study was conducted at Khayelitsha District Hospital in Cape Town, South Africa (SA) over the period March 2020–December 2021. We included confirmed COVID-19 cases with HIV infection aged from 18 years and above. Analysis was performed to identify predictors of mortality or hospital discharge among people living with HIV (PLWH). Predictors investigated include CD4 count, antiretroviral therapy (ART), TB, non-communicable diseases, haematological, and biochemical parameters.
Findings
This cohort of PLWH with SARS-CoV-2 infection had a median (IQR) age of 46 (37–54) years, male sex distribution of 29.1%, and a median (IQR) CD4 count of 267 (141–457) cells/mm3. Of 255 patients, 195 (76%) patients were discharged, 60 (24%) patients died. One hundred and sixty-nine patients (88%) were on ART with 73(28%) patients having acquired immunodeficiency syndrome (AIDS). After multivariable analysis, smoking (risk ratio [RR]: 2.86 (1.75–4.69)), neutrophilia [RR]: 1.024 (1.01–1.03), and glycated haemoglobin A1 (HbA1c) [RR]: 1.01 (1.007–1.01) were associated with mortality.
Conclusion
The district hospital had a high COVID-19 mortality rate among PLWH. Easy-to-access biomarkers such as CRP, neutrophilia, and HbA1c may play a significant role in informing clinical management to prevent high mortality due to COVID-19 in PLWH at the district-level hospitals.
Similar content being viewed by others
Background
Globally, COVID-19 continues to test even the resilient healthcare systems, with the Omicron being the latest variant in circulation. As of March 25th, 2022, the World Health Organization (WHO) had reported over 476 million confirmed cases of COVID-19, including over 6 million deaths, and approximately 11 billion vaccine doses had been administered [1]. South Africa, a middle-income country, is experiencing epidemics of noncommunicable diseases and chronic infectious diseases such as the human immunodeficiency virus (HIV) and tuberculosis (TB). Around eight million of South Africa's 60 million people are HIV-positive, accounting for one-fifth of all HIV-positive people worldwide [2, 3]. A high proportion of people newly diagnosed in South Africa are at an advanced stage of HIV infection (defined as a CD4 count < 200 cells/mm3), by which point the immune system is extremely compromised [3, 4]. Lastly, South Africa recorded 0.7% of TB prevalence for all ages, among them 301,000 are new cases of TB [5].
A systematic review including twenty-two studies conducted in developed and low and middle countries showed that HIV remains a significant risk factor for SARS-CoV-2 infection and is linked to a higher risk of death from COVID-19 [6]. Similarly, a meta-analysis found that active TB was more common in COVID-19/HIV co-infected people than in COVID-19 infected people [7]. On the other hand, COVID-19 risk was high among current HIV/TB co-infected cases [7]. According to one study, patients with SARS-CoV-2 infection who also had HIV and TB had altered T-cell functions and were at higher risk of developing severe disease [8]. Furthermore, COVID-19 could be accelerated in HIV patients with compromised immunity [7, 9]. SARS-CoV-2 and HIV may both decrease lymphocyte and CD4 counts. Corticosteroids given as management for moderate to severe disease for SARS-CoV-2 may predispose to TB [7, 10]. Co-infection with SARS-CoV-2 and tuberculosis may exacerbate the pathologies associated with each pathogen [11]. Co-infection of macrophages can increase the production of pro- and anti-inflammatory cytokines, playing a significant role in pathogenesis of COVID-19 [11]. COVID-19 pneumonia, on the other hand, may hasten the progression of tuberculosis [12, 13]. The combination of a weakened virus-induced cytokine response caused by a severe/dysfunctional immune system and in vitro activity of certain antiretroviral drugs (tenofovir and lopinavir-ritonavir) on coronaviruses is thought to be associated with a reduction in the severity COVID-19 in PLWH [14,15,16]. However, PLWH were 30% more likely to die after admission to hospital with COVID-19, regardless of age, gender, severity at presentation, or co-morbidities [17]. Diabetes, high blood pressure, and male sex were all associated with an increased risk of death [18]. These comorbidities are caused by ART-related inflammation and ongoing immune dysregulation, which may influence COVID-19 disease severity, the durability of protective antiviral responses, and vaccine responsiveness [19,20,21,22]. According to a recent non-peer reviewed systematic review, COVID-19 vaccines had lower immunogenicity and antigenicity among PLWH, than among HIV negative people [23]. Furthermore, PLWH require more attention during the COVID-19 pandemic because the emergence of Omicron in Southern Africa has raised the question of whether this heavily mutated variant is the result of the HIV pandemic, a common cause of immunodeficiency in the region [3].
South Africa has a dual healthcare system with both public and privately funded facilities. The publicly funded district healthcare system serves approximately 84% of the population [24]. The district-level healthcare system, which is often understaffed, along with the primary healthcare system, are the primary points of contact for COVID-19 patients. Experiences from district-level hospitals with high HIV/TB burdens provide a unique opportunity to study the effects of the COVID-19 pandemic at the 'grass roots' level, which will inform the success or failure of public health interventions. The purpose of this study was to describe the clinical features of COVID-19 patients in a district hospital setting in a population with a high TB/HIV prevalence.
Methods
Study design
This was a retrospective observational study describing the epidemiological and clinical characteristics of COVID-19 patients admitted at Khayelitsha District Hospital, Cape Town, South Africa from March 2020–December 2021.
Case definition and management
A COVID-19 case was defined as PLWH with a positive antigen or reverse transcriptase polymerase chain reaction (RT-PCR) assay (Abbott Panbio Covid-19 antigen test or Cepheid Xpert Xpress CoV-2 plus test) for SARS-CoV-2 who were admitted to hospital. For those diagnosed with HIV, ELISA (BIOMERIEUX MINI VIDAS duo kit) test was performed on all patient during admissions if HIV status was not known. In terms of management and treatment, all patients were given oxygen and corticosteroid therapy. The management pillars were based on the recovery trial results, which showed that COVID-19 patients who were oxygen dependent and on corticosteroid therapy had a better outcome than those who were not on corticosteroid therapy. Because the clinical and radiological findings were consistent with hypoxemic pneumonia, all patients were started on empiric bacterial treatment with Ceftriaxone and Azithromycin in accordance with national and international guidelines for community acquired pneumonia. Once COVID-19 was confirmed by antigen testing or RT-PCR, empiric antibiotic therapy was thereafter immediately discontinued.
Study population
We included all consecutive COVID-19 cases with HIV infection, 18 years and older who required hospital admission from March 2020 until December 2021. The main indication for hospitalization was anyone with COVID-19 pneumonia requiring oxygen therapy. Patients were prospectively followed up until completed hospital course (either discharge, transfer to tertiary or field hospital or death) at censoring. A total of 255 PLWH were included in this study.
Setting
Khayelitsha District Hospital, located in Mandela Park, Khayelitsha, is a 330-bed district hospital that opened in 2012. Khayelitsha township is Southeast of Cape Town (Fig. 1). Most of the population (98.6%) is black African [25]. Khayelitsha was created by the apartheid government via the forced removals of the Group Areas Act. It is isolated, located on sand dunes, and has a substantial risk of flooding. It is entirely residential, with no designated commercial or industrial areas [26]. Most of the population (55.6%) lives in informal housing [27]. Khayelitsha has South Africa's highest concentration of poverty and unemployment [27]. Furthermore, with 37.0% TB burden and 47.6% HIV/TB co-infection, Khayelitsha has the worst health indicators in the Cape Town metropolitan area [28]. Similarly, Khayelitsha has the highest rates of mortality for stroke, hypertension, and diabetes mellitus [29, 30]. Overpopulation, poverty, trauma, mental health, communicable, and noncommunicable diseases have all posed significant challenges to Khayelitsha Hospital's ability to serve the community. No fewer than ten nearby primary care clinics refer patients to the hospital. The population of Khayelitsha is estimated to be close to 500 000 people [31], but this is a gross underestimation due to the community's continued growth. In this population, 51.1% are females, 48.8% are between the ages of 25 and 65, only 4.9% completed high school, and 30.7% finished secondary school [27]. The unemployment rate is estimated to be 38.32% [27]. The first case of COVID-19 in a South African township occurred in Khayelitsha. Overtime medical admissions at Khayelitsha District Hospital have risen steadily over the last five years, averaging 5500 per year with a mortality rate of less than 10%.
Data collection
The patients’ demographic, clinical, baseline laboratory results and outcome data were collected from digital application-based registries. Additional data were captured from electronic medical records. Furthermore, the presence of comorbidities including HIV/AIDS hypertension, diabetes, overweight or obesity (defined as a body mass index (BMI > 25 or > 30 kg/m2 respectively) or as documented by treating clinicians as the BMI was not captured. Other comorbidities were cardiac disease, chronic kidney disease, and active or previous history of TB were also included in the data collection process. Baseline arterial blood gas and laboratory values including severity indices were captured. These included the partial pressure of arterial oxygen to fraction of inspired oxygen (P/F Ratio), the white cell count (WCC), the neutrophil to lymphocyte ratio (N/L Ratio), serum creatinine (Cr), HbA1c and the CRP and CD4 cell counts. Viral load measurements were captured if they were performed up to a year prior to admission. The main outcome of the study was death or discharge. Patients whose outcome data was unknown were excluded from the analyses. Data were captured retrospectively based on clinical notes at the bedside, which were securely stored electronically, and clinical data were entered remotely onto a Research Electronic Data Capture (REDCap®) database; laboratory results were imported into the database. Data were checked by the ‘data entry supervisor.’
Ethical approval
Ethical approval for the study was obtained from the Stellenbosch University health research ethics committee (Ethics Reference Number: N20/05/020_COVID-19).
Statistical analysis
Continuous variables were expressed as median with inter-quartile range for skewed data. Categorical variables were expressed using frequencies and percentages. A multivariable model was developed for demographics, comorbidities, clinical symptoms, haematological, and biochemical parameters using variables strongly associated with mortality or survival outcomes at univariable analysis. The comparison between mortality and survival used the Pearson χ2 test or Fisher exact test where appropriate for categorical variables, and the Wilcoxon's rank-sum test for continuous variables. Robust Poisson regression was used to assess significant associations between demographic, laboratory results, and mortality. Factors associated with death at p < 0.15 in unadjusted univariable robust Poisson regression were included in a multivariable model to identify predictor variables associated with death. Due to the high mortality, around 24%, the logistic regression overestimated the effect measure with large standard errors resulting in wide confidence intervals, therefore robust Poisson regression was used. Adjusted risk ratios and their 95% CIs were used as a measure of association. Receiver Operating Characteristic curve (ROC) analysis was performed to evaluate the diagnostic performance of various haematological and biochemical parameters to discriminate between severe cases in terms of survival and non-survival. Schoenfeld residuals and cox proportional hazards test were used to assess the proportional hazards assumption [32]. Kaplan-Meir survival curve was plotted, and the log-rank test was used to compare the two groups [32]. All statistical analyses were performed using Stata (V.16, Stata Corp, College Station, Texas, USA) and R (V, 4.1.0, R Core Team) with R Studio (V.1.3, R Studio Team) statistical software.
Results
Characteristics of PLWH with SARS-COV-2
A total of 255 PLWH were admitted during the first and the second waves. The cohort was comprised mainly of females (70.9%) and mostly above 50 years old (38.8%), with 55.2% (n = 32) of all patients who died being 50 years and older (Table 1). Among PLWH, the main pre-existing co-morbidities were hypertension (43.1%), diabetes mellitus (29.4%), chronic kidney disease (7.1%), TB (12.9%), and acute kidney injury (16.9%) (Table 1). The presenting clinical signs and symptoms suggestive of COVID-19 included fever (38.8%), cough (75.7%), sore throat (11.0%), and myalgia (22.4%) (Table 1). Most of this PLWH cohort (88.5%) were on ARV therapy. Among them, 36.9% of this cohort had severe immunosuppression with CD4 < 200mm3 with only 21% having a CD4 ≥ 500 mm3 (Table 1). The median oxygen saturation and PaO2 were 93% (86–97) and 8 kPa (6.8–9.9), respectively (Table 1). Higher median CRP was observed among those who died 20.4 (12.4–28.5) as compared to those discharged 13.9 (7.0–20.7) characterised this PLWH cohort and, high median (IQR) HbA1c was a predictor of mortality with 12% (10.35–13.35%) (Table 1). The case fatality rate in the study population was 23.5% (60/255). Around sixty-seven percent (150/225) had known HIV viral load and seventy-eight (117/150) percent had undetectable HIV viral load (< 50 copies/ml).
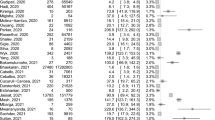
Association of demographic, haematological, and biochemical parameters with mortality among PLWH with SARS-CoV-2 infection
Table 2 shows the association between demographic, haematological, and biochemical parameters with survival among PLWH. Creatinine (1.001, 95% CI: 1.001–1.002, p < 0.001), Neutrophils (1.02, 95% CI: 1.01–1.03; p < 0.001), HbA1c (1.01, 95% CI: 1.007–1.010; p < 0.001), and CRP (1.003, 95% CI: 1.001–1.005, p < 0.001) were significantly associated with the risk of mortality. In multivariable analysis smoking, neutrophils, HbA1c and CRP were all significantly associated with increased risk of mortality (aRR 4.17: 1.50–10.01); (aRR: 1.03, 95% CI: 1.02–1.05; p < 0.001); (aRR: 1.01, 95% CI: 1.001–1.02; p = 0.021); (aRR; 1.002, 95% CI: 1.002–1.01; p < 0.032).
ROC curves and cut-offs
As the adjusted RR was significant for neutrophils and CRP at the borderline, we determined the optimal cut-offs to predict non-survival and test performance of these two parameters using ROC curves. ROC curves were drawn with sensitivity as the horizontal coordinate and the 1‑specificity as the vertical coordinate to predict COVID-19 severity and mortality among PLWH admitted to the hospital. The proposed optimum cut-off points for neutrophils derived from ROC analysis was ≥ 5.6 × 109/L with sensitivity = 76% and specificity = 56% (Table 3 and Fig. 2). An optimal cut-off of 202 mg/L rendered 52% sensitivity and 74% specificity for the CRP (Table 3 and Fig. 3). The area under the ROC curves (AUC) for the neutrophils and CRP were 0.66 and 0.65, respectively (Table 3). However, the performance of both was suboptimal to use as a predictive marker on their own. The combination of the two variables and their predictive value on the roc curve changed slightly to AUC = 0.67.
Kaplan–Meier survival estimates between males and females
The rate of death seemed to be higher among male patients during the whole duration of the hospitalization. However, Poisson regression analysis was used to compare male and female mortality, no significant difference was found (p = 0.160) (Fig. 4). The median stay was 7 (IQR: 3–12) days for females compared to 5 (IQR: 3–9.5) days for males. The overall median stay was 6 (IQR: 3–10) days. (Fig. 4). The plots of the scaled Schoenfeld residuals of each covariate against log-time were used to determine whether the proportional hazards assumption was violated (Fig. 5). The Schoenfeld residuals test revealed that a proportional hazard assumption had the same effect on male and female survival rates (p = 0.3905) (Fig. 5).
Discussion
This retrospective cohort study of 255 PLWH with SARS-CoV-2 infection focused on hospitalized individuals at a district hospital in Cape Town. Most of these patients were stable on ART and over one-third of them died. The median (IQR) age was 46 (37–54) years, with 70.9% of the population being female. PLWH who died were older than 50 years old, females, smokers, had acute kidney injury, CD4 less than 200 mm3, hypoxemic, high CRP, and HbA1c. Creatinine, Neutrophils, HbA1c, and CRP were significantly associated with the risk of mortality in univariable analysis. Smoking, neutrophils, HbA1c, and CRP were all significantly associated with an increased risk of mortality in a multivariable analysis. CRP and neutrophil performance were both suboptimal for use as survival predictors. The high mortality experienced among PLWH was consistent with a systematic review and meta-analysis of twenty-two studies involving 20,982,498 PLWH, which found that HIV was associated with a significantly higher risk of SARS-CoV-2 infection (RR 1.24, 95 percent CI 1.05–1.46) [6]. The overall pooled RR of COVID-19 mortality associated with HIV was 1.78 (95%CI 1.21–2.60), implying that HIV-positive patients have an 80% increased risk of death when compared to people who do not have HIV/AIDS [6]. Similarly, a review revealed that the RR of severe COVID-19 in PLWH was significant only in Africa (RR = 1.14, 95% CI = 1.05–1.24), while the relative risk of mortality was 1.5 (95% CI = 1.45–2.03) globally [33]. Although the RR of severe COVID-19 in PLWH appeared to be lower, the studies included in this review were conducted in often well-resourced and skilled tertiary, academic, and intensive care unit (ICU) hospital settings. The high COVID-19 mortality rate among PLWH should be considered in the context of the devastation brought on by the COVID-19 pandemic in a limited resource district hospital which is already overwhelmed by the high burden of HIV, TB, and other non-communicable diseases. In addition to this, the low CD4 count, high AIDS rate, and a high prevalence of multiple co-morbidities among PLWH with COVID-19, seem to have a key role in the high COVID-19 mortality in a district hospital setting. A recent study conducted among PLWH in Cape Town revealed that PLWH with CD4 count < 200 cells/µl were associated with COVID-19 death (aHR vs people living without HIV, 2.36 [95% CI, 1.47–3.78]; aHR vs PLWH with CD4 count ≥ 350 cells/µl, 1.97 [95% CI, 1.14–3.40]) [34]. Compared with HIV disease stage 1 (CD4 counts > 500 cells/ml), hospitalization rates were 29% higher for stages 2 (CD4 counts 200–499 cells/ml) and 69% higher for stage 4 CD4 counts < 200 cells/ml) [35]. The unadjusted hazard ratio of COVID-19 death was 1.07 (95% CI 0.88–1.32) for HIV-positive vs. HIV-negative, and 2.14 (95% CI 1.70–2.20) after adjustment for age, sex, and other comorbidities [34]. This finding was consistent with our findings, as CD4 counts of less than 200 cells/ml were associated with COVID-19 among PLWH in unadjusted RR. The interplay between the inverse relationship between the CD4 count, HIV viral load, the access and adherence to ARV therapy play a crucial role in the determinant of severity of HIV infection and associated outcomes.
As this study was conducted in a high HIV/TB setting, emphasis is also placed on the interactions between COVID-19, HIV, and TB. This cohort found 12.9% cases of TB coinfection with COVID-19 among PLWH. However, the records did not specify whether these cases were active or had previous TB. Knowing that a study performed in an urban township of Cape Town observed a very high (88.0%) latent TB infection (LTBI) prevalence rate among PLWH [36] and SARS-CoV-2 infection decreases TB–specific CD4 + T cell response [8], many concerns have been raised about the possibility that COVID-19 could reactivate latent TB in a high TB-endemic setting such as Khayelitsha district. The reactivation of TB could be explained by cytokines and chemokines dysregulation, higher consumption of CD4 + and CD8 + T-cells, decrease in regulatory T-cells, and an altered innate immune environment leading to a cytokine storm and worsen tissue damage [37,38,39]. A study showed poor outcome in mortality rate among COVID-19/HIV/TB co-infection compared to COVID-19/TB [7]. Even though, our study found no significant link between COVID-19 mortality and HIV/TB cases, a large cohort study conducted in Cape Town found an association between COVID-19 mortality and previous and active TB [34]. Our findings should be interpreted in the context of inadequate TB screening in COVID-19 patients admitted to the district hospital.
Our study also found out that raised neutrophil count, CRP, HbA1c, and smoking were associated with worse outcomes after confounding adjustment. This is substantial as those biomarkers may play a vital role in preventing worse outcomes among COVID-19 in PLWH. A multivariable analysis showed that raised neutrophil count was an independent risk factor for mortality. This finding is similar to the previous study which revealed that a higher neutrophil count in COVID-19 patients was found to be associated with a higher mortality rate among PLWH with SARS-CoV-2 infection [40]. This could be explained by emergency release of granulocyte colony-stimulating factor with activation of immature neutrophils, neutrophil maturation, neutrophil degranulation, and release of neutrophil extracellular traps (NETs) [41, 42]. Neutrophil activation and degranulation result in release of neutrophil-activation markers including resistin, lipocalin-2, hepatocyte growth factor and interleukin-8 which causes significant collateral damage. The immune response of natural killer cells and T lymphocytes contributes to the formation of NETs and the activation of the complement system (C5 and C3) [42]. The result is the development of microvascular thrombosis, which leads to organ damage with an increased risk of severe COVID-19 and mortality [41, 42]. The early elevation of activated immature neutrophils, G-CSF and neutrophil-activation markers were suggested as early predictors of severe COVID-19 infection and increased mortality. Additionally, alteration to gene expression of neutrophils with a prominence of immature neutrophils markers was found in severe COVID-19 patients [43]. While access to these tests is not feasible in limited-resource countries the use of neutrophil count could be used as an affordable predictor variable of COVID-19 severity and mortality among PLWH. Importantly, our analysis revealed a significantly higher CRP in the non-survivor group compared to the survivor group. The CRP is an acute phase reactant which functions as a reliable biomarker and is recommended as a predictor of COVID-19 severity and mortality. Our findings were in the line with studies including PLWH and SARS-COV-2, conducted in the same settings which showed significantly high CRP levels among non-survivors [8, 40]. The cut-offHbA1c level of ≥ 6.5% is defined as diabetes mellitus. A study revealed that high HbA1c level is associated with inflammation, hypercoagulability, and low SaO2 in COVID-19 patients, and the mortality rate is higher in patients with diabetes mellitus [44, 45]. In our study, HbA1c was high in both discharged and death cases and the difference in HGT was not statistically significant between the two groups. The plausible explanation for the high HbA1c among COVID-19 cases with HIV could be more severe inflammatory process and more intense coagulation disorder associated with poor prognosis [45]. Another explanation could be the high HbA1c found in public sector primary health care facilities in Cape Town as a study showed 78.9% of type 2 diabetes mellitus patients had HbA1c outside of the target range [46]. As high HbA1c may not be a reliable biomarker in this context, our findings were focused on the neutrophils and CRP. Even though, the performance of both was suboptimal to use as a prediction marker, high neutrophils and CRP are consistent with previous studies showing higher diagnostic accuracy and AUC of ROC analysis [47, 48]. Lastly, our study found that smoking was an independent factor of mortality PLWH with SARS-CoV-2 infection. A systematic review of fifty‐seven studies found that current smokers are at reduced risk of SARS-CoV-2 infection, while former smokers appeared to be at increased risk of hospitalization, increased disease severity and mortality from COVID-19 [49]. We could not find a plausible explanation for this association. However, a study conducted on smoking status found that the response rate was low among current smoking (10%) compared to 58.8% among former smokers [50]. This could overestimate the effect of smoking status on COVID-19 outcome. Even though our study did not identify current and former smoking status, the association between smoking and COVID-19 mortality among PLWH should be taken with caution.
This study has several strengths. This is the first study to our knowledge conducted in a South African district-level hospital involving COVID-19 patients with HIV infection. Based on the study findings, COVID-19 management among PLWH at the district-level may face multiple challenges due to limited resources. As primary healthcare systems are often poorly funded, overcrowded, short-staffed, and are unable to provide efficient care. This study has provided an overview of COVID-19 severity and mortality risk factors among vulnerable and specific population of PLWH in district-level hospital. Additionally, significant COVID-19 challenges faced by the facility included the lack of infrastructure within the facility with a daily bed occupancy rate to deal with the separation of COVID-19 patients from Persons Under Investigation (PUIs) and general medical admissions. This study showed that easily available biomarkers in a district hospital setting are associated with COVID-19 mortality. These biomarkers could be used by clinicians at district-level hospitals to risk stratify and motivate for higher level of care at their tertiary referral hospitals. This study had several limitations among which is its retrospective design nature. The retrospective cohort study design limited our ability to gather data about factors that may influence the risk of mortality such as the HIV viral load, ART regimens, active and previous TB, estimated glomerular filtration rate (eGFR), and smoking status. Another study flaw was that transferred cases were not followed up with the Western Cape Provincial Health Data Centre (PHDC) to learn about their outcomes. This was the source of missing and incomplete data. The other limitation of the study might be that it is a single centre study but also underpowered due to sample size used, hence our results might be limited to the population of Khayelitsha and not generalized to other similar populations.
Conclusion
This study showed that the mortality rate of COVID-19 patients co-infected with HIV was high at district hospital level. An increase in neutrophils, HbA1c, and CRP were all significantly associated with risk of mortality. As such COVID-19 diagnosis and management among PLWH at the district-level should include easily accessible, reliable, and affordable assessment for these biomarkers to support the front-line clinicians for an effective risk stratification of patients at an increased of poor outcome and subsequent early transfer to tertiary level hospital for advanced care and minimise loss of life in such patients.
Availability of data and materials
All data are available upon request from the corresponding author of the study.
Abbreviations
- AIDS:
-
Acquired immunodeficiency syndrome
- ARDS:
-
Acute respiratory distress syndrome
- ART:
-
Antiretroviral therapy
- ARV:
-
Antiretroviral
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- CDC:
-
Centers for diseases control and prevention
- CD4 count:
-
Cluster of differentiation 4
- CO2:
-
Partial pressure of carbon dioxide
- COVID-19:
-
Coronavirus disease 2019
- Cr:
-
Serum creatinine
- eGFR:
-
Estimated glomerular filtration rate
- ELISA:
-
Enzyme-linked immunoassay
- FiO2:
-
Fraction of inspired oxygen
- ICU:
-
CRP: C-reactive protein
- HbA1c:
-
Glycated haemoglobin
- HGT:
-
Hemo Glucose test
- HIV:
-
Human immunodeficiency virus
- ICU:
-
Intensive care unit
- LTBI:
-
Latent TB infection
- NET:
-
Neutrophil extracellular traps
- N/L Ratio:
-
Neutrophil to lymphocyte ratio
- PCT:
-
Procalcitonin
- P/F Ratio:
-
Fraction of inspired oxygen ratio
- PCR:
-
Polymerase chain reaction
- pH:
-
Potential hydrogen
- PLWH:
-
People living with HIV
- PUIs:
-
Persons Under Investigation
- ROC:
-
Operating characteristic curve
- SA:
-
South Africa
- SANAS:
-
South African National Accreditation Services
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- TB:
-
Tuberculosis
- WCC:
-
White cell count
- WHO:
-
World Health Organization
References
WHO. WHO Coronavirus (COVID-19) Dashboard-Overview, 2022. https://covid19.who.int/
UNAIDS. South Africa. https://www.unaids.org/en/regionscountries/countries/southafrica
Freer J, Mudaly V. HIV, and covid-19 in South Africa. BMJ. 2022;376: e069807.
Carmona S, Bor J, Nattey C, et al. Persistent high burden of advanced HIV disease among patients seeking care in South Africa’s national HIV program: data from a nationwide laboratory cohort. Clin Infect Dis. 2018;66(suppl 2):S111–7.
National Department of Health. The First National TB Prevalence Survey|South Africa, 2018. https://www.samrc.ac.za/media-release/first-south-african-national-tb-prevalence-survey-gives-clearer-picture-epidemic
Ssentongo P, Heilbrunn ES, Ssentongo AE, Advani S, Chinchilli VM, Nunez JJ, Du P. Epidemiology, and outcomes of COVID-19 in HIV-infected individuals: a systematic review and meta-analysis. Sci Rep. 2021;11(1):6283.
Tamuzi JL, Ayele BT, Shumba CS, et al. Implications of COVID-19 in high burden countries for HIV/TB: a systematic review of evidence. BMC Infect Dis. 2020;20(1):744.
Riou C, du Bruyn E, Stek C, et al. Relationship of SARS-CoV-2-specific CD4 response to COVID-19 severity and impact of HIV-1 and tuberculosis coinfection. J Clin Invest. 2021;131(12): e149125.
Soriano V, Barreiro P. Impact of new coronavirus epidemics on HIV-infected patients. AIDS Rev. 2020;22(1):57–8.
Liu W, Fontanet A, Zhang PH, et al. Pulmonary tuberculosis and SARS. China Emerg Infect Dis. 2006;12(4):707–9.
Tapela K, Ochieng’ Olwal C, Quaye O. Parallels in the pathogenesis of SARS-CoV-2 and M. tuberculosis: a synergistic or antagonistic alliance? Future Microbiol. 2020;15:1691–5.
Tadolini M, Codecasa LR, García-García JM, et al. Active tuberculosis, sequelae, and COVID-19 co-infection: first cohort of 49 cases. Eur Respir J. 2020;56(1):2001398.
Wilkinson RJ. Tuberculosis and type 2 diabetes mellitus: an inflammatory danger signal in the time of coronavirus disease 2019. Clin Infect Dis. 2021;72(1):79–81. https://doi.org/10.1093/cid/ciaa747.
Laurence J. Why aren’t people living with hiv at higher risk for developing severe coronavirus disease 2019 (COVID-19)? AIDS Patient Care STDS. 2020;34(6):247–8.
Del Amo J, Polo R, Moreno S, Dı’az A, Martı’nez E, Arribas JR, et al. Antiretrovirals and risk of COVID-19 diagnosis and hospitalization in HIV-Positive persons. Epidemiol. 2020;31:e49–51.
Mascolo S, Romanelli A, Carleo MA, Esposito V. Could HIV infection alter the clinical course of SARS-CoV-2 infection? When less is better. J Med Virol. 2020;92(10):1777–8.
WHO. Clinical features and prognostic factors of COVID-19 in people living with HIV hospitalized with suspected or confirmed SARS-CoV-2 infection, 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-Clinical-HIV-2021.1
Bertagnolio S, Thwin S, Silva R, Ford N, Baggaley R, Vitoria M, Jassat W, Doherty M. Clinical characteristics, and prognostic factors in people living with HIV hospitalized with COVID-19: findings from the WHO Global Clinical Platform. In: 11th International AIDS Society Conference on HIV Science, 2021; pp. 18–21.
Deeks SG, Phillips AN. HIV infection, antiretroviral treatment, ageing, and non-AIDS related morbidity. BMJ. 2009;338: a3172.
Pallikkuth S, Parmigiani A, Silva SY, et al. Impaired peripheral blood T-follicular helper cell function in HIV-infected nonresponders to the 2009 H1N1/09 vaccine. Blood. 2012;120(5):985–93.
Moir S, Fauci AS. B-cell responses to HIV infection. Immunol Rev. 2017;275(1):33–48.
Alrubayyi A, Gea-Mallorquí E, Touizer E, et al. Characterization of humoral and SARS-CoV-2 specific T cell responses in people living with HIV. Nat Commun. 2021;12(1):5839.
Tamuzi JL, Muyaya LM, Mitra A, Nyasulu P. Systematic review and meta-analysis of COVID-19 vaccines safety, tolerability, and efficacy among HIV-infected patients. https://doi.org/10.1101/2022.01.11.22269049v1
Naidoo S. The South African national health insurance: a revolution in health-care delivery! J Public Health (Oxf). 2012;34(1):149–50.
City of Cape Town. 2011 Census Suburb Khayelitsha. Strategic development information and GIS Department (SDI&GIS), Cape Town, 2013. http://www.capetown.gov.za/en/stats/2011CensusSuburbs/2011_Census_CT_Suburb_Khayelitsha_Profile.
Maylam P. The rise and decline of urban apartheid in South Africa. Afr Aff. 1990;89(354):57–84.
City of Cape Town. Census Suburb Khayelitsha-2011, 2013. https://resource.capetown.gov.za/documentcentre/Documents/Maps%20and%20statistics/2011_Census_CT_Suburb_Khayelitsha_Profile.pdf
Mahtab S, Coetzee D. Influence of HIV, and other risk factors on tuberculosis. S Afr Med J. 2017;107(5):428–34.
Groenewald P, Bradshaw D, Daniels J, Zinyakatira N, Matzopoulos R, Bourne D, Shaikh N, Naledi T. Local-level mortality surveillance in resource-limited settings: a case study of Cape Town highlights disparities in health. Bull World Health Organ. 2010;88(6):444–51.
Smit W, de Lannoy A, Dover RV, Lambert EV, Levitt N, Watson V. Making unhealthy places: The built environment and non-communicable diseases in Khayelitsha. Cape Town Health Place. 2016;39:196–203.
Western Cape Government. Population data, 2020. https://www.westerncape.gov.za/assets/departments/health/h_102_2020_covid-19_population_data.pdf
Lalla U, Koegelenberg CFN, Allwood BW, Sigwadhi LN, Irusen EM, Zemlin AE, Masha TE, Erasmus RT, Chapanduka ZC, Prozesky H, Taljaard J, Parker A, Decloedt EH, Retief F, Jalavu TP, Ngah VD, Yalew A, Tamuzi JL, Baines N, McAllister M, Zumla A, Nyasulu PS. Comparison of patients with severe COVID-19 admitted to an intensive care unit in South Africa during the first and second wave of the COVID-19 pandemic. Afr J Thorac Crit Care Med. 2021. https://doi.org/10.7196/AJTCCM.2021.v27i4.185.
Oyelade T, Alqahtani JS, Hjazi AM, Li A, Kamila A, Raya RP. Global and regional prevalence and outcomes of COVID-19 in people living with HIV: a systematic review and meta-analysis. Trop Med Infect Dis. 2022;7(2):22.
Western Cape Department of Health in collaboration with the National Institute for Communicable Diseases, South Africa. Risk Factors for Coronavirus Disease 2019 (COVID-19) Death in a Population Cohort Study from the Western Cape Province, South Africa [published correction appears in Clin Infect Dis. 2022 Mar 17:]. Clin Infect Dis. 2021;73(7): e2005-e2015.
Tesoriero JM, Swain CE, Pierce JL, et al. COVID-19 Outcomes Among Persons Living with or Without Diagnosed HIV Infection in New York State. JAMA Netw Open. 2021;4(2): e2037069.
Wood R, Lawn SD, Johnstone-Robertson S, Bekker LG. Tuberculosis control has failed in South Africa–time to reappraise strategy. S Afr Med J. 2011;101(2):111–4. https://doi.org/10.7196/samj.4587.
Grifoni A, Weiskopf D, Ramirez SI, Mateus J, Dan JM, Moderbacher CR, Rawlings SA, Sutherland A, Premkumar L, Jadi RS, Marrama D, de Silva AM, Frazier A, Carlin AF, Greenbaum JA, Peters B, Krammer F, Smith DM, Crotty S, Sette A. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. 2020;181(7):1489-1501.e15.
Rydyznski Moderbacher C, Ramirez SI, Dan JM, Grifoni A, Hastie KM, Weiskopf D, Belanger S, Abbott RK, Kim C, Choi J, Kato Y, Crotty EG, Kim C, Rawlings SA, Mateus J, Tse LPV, Frazier A, Baric R, Peters B, Greenbaum J, Ollmann Saphire E, Smith DM, Sette A, Crotty S. Antigen-specific adaptive immunity to SARS-CoV-2 in acute COVID-19 and associations with age and disease severity. Cell. 2020;183(4):996-1012.e19.
Tan LY, Komarasamy TV, Rmt BV. Hyperinflammatory immune response and COVID-19: a double-edged sword. Front Immunol. 2021;12: 742941.
Parker A, Koegelenberg CFN, Moolla MS, et al. High HIV prevalence in an early cohort of hospital admissions with COVID-19 in Cape Town. South Africa S Afr Med J. 2020;110(10):982–7.
Meizlish ML, Pine AB, Bishai JD, et al. A neutrophil activation signature predicts critical illness and mortality in COVID-19. Blood Adv. 2021;5(5):1164–77.
Nappi F, Giacinto O, Ellouze O, et al. Association between COVID-19 diagnosis and coronary artery thrombosis: a narrative review. Biomedicines. 2022;10(3):702.
Aschenbrenner AC, Mouktaroudi M, Krämer B, et al. Disease severity-specific neutrophil signatures in blood transcriptomes stratify COVID-19 patients. Genome Med. 2021;13(1):7.
Wang Z, Du Z, Zhu F. Glycosylated hemoglobin is associated with systemic inflammation, hypercoagulability, and prognosis of COVID-19 patients. Diabetes Res Clin Pract. 2020;164: 108214.
Unluguzel Ustun G, Keskin A, Aci R, Arslanbek Erdem M, Ari M. Association between Hb A1c and Severity of COVID-19 Patients. Hemoglobin. 2021;45(2):124–8.
Monanabela KB, van Huyssteen M, Coetzee R. Describing medicine therapy management of type 2 diabetes mellitus at primary health care facilities in Cape Town. Health SA. 2019;24:1051.
Xu JB, Xu C, Zhang RB, Wu M, Pan CK, Li XJ, Wang Q, Zeng FF, Zhu S. Associations of procalcitonin, C-reaction protein and neutrophil-to-lymphocyte ratio with mortality in hospitalized COVID-19 patients in China. Sci Rep. 2020;10(1):15058.
Xiao LN, Ran X, Zhong YX, Li SS. Clinical value of blood markers to assess the severity of coronavirus disease 2019. BMC Infect Dis. 2021;21(1):921.
Simons D, Shahab L, Brown J, Perski O. The association of smoking status with SARS-CoV-2 infection, hospitalization, and mortality from COVID-19: a living rapid evidence review with Bayesian meta-analyses (version 7). Addiction. 2021;116(6):1319–68.
Merkely B, Szabó AJ, Kosztin A, Berényi E, Sebestyén A, Lengyel C, et al. Novel coronavirus epidemic in the Hungarian population, a cross-sectional nationwide survey to support the exit policy in Hungary. GeroScience. 2020;42:1063–74.
Acknowledgements
None.
Funding
We received grant support for aspects of this work from the National Institutes of Health Grant number: U01 AI069924.
Author information
Authors and Affiliations
Contributions
ATM and PSN initiated and supervised the study project. ATM, LNS, VN, and AY collected and managed the data. LNS and AY conducted the data analysis and interpreted the results. JLT prepared Fig. 1. ATM, PSN, AEZ, ZCC, VN, LNS, AY, and JLT drafted the manuscript. ATM, DS, NE, NS, NB, NS, SG, LNS, AEZ, ZCC, VN, AY, TJ, IA, JLT, TN, YT, MAD, RE, PSN reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for the study was obtained from the Stellenbosch University health research ethics committee (Ethics Reference Number: N20/05/020_COVID-19). Informed consent was obtained from all subjects and/or their legal guardian(s). All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
No conflict of interest declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mnguni, A.T., Schietekat, D., Ebrahim, N. et al. The clinical and epidemiological characteristics of a series of patients living with HIV admitted for COVID-19 in a district hospital. BMC Infect Dis 23, 123 (2023). https://doi.org/10.1186/s12879-023-08004-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08004-6