Abstract
Introduction
Neisseria meningitidis (Nm) is a major cause of meningitis and septicemia. Most people are infected with latent infections or are carriers. We aimed to estimate the carriage prevalence of Nm in China.
Methods
We did a systematic review of published work to assess the prevalence of meningococcal carriage in China. The quality assessment was conducted by the risk of bias tool according to Damian Hoy’s study. We estimated pooled proportions of carriage and its 95% confidence interval (95% CI) using fixed effect model for studies with low heterogeneity and random effect model for studies with moderate or high heterogeneity. Subgroup analyses were also conducted by region and age group.
Results
In total, 115 studies were included. The quality evaluation grades of all included documents were medium or high grade. The weighted proportion of carriage was 2.86% (95% CI: 2.25–3.47%, I2: 97.7%, p = 0). The carriage prevalence of Nm varied between provinces, ranged from 0.00% (95% CI: 0.00–0.66%) to 15.50% (95% CI: 14.01–16.99%). Persons aged 15 years and older had the highest carriage 4.38% (95% CI: 3.15–5.62%, I2: 95.4%, p < 0.0001), and children under 6 years of age had the lowest carriage 1.01% (95% CI: 0.59–1.43%, I2: 74.4%, p < 0.0001). In positive carriers, serogroup B (41.62%, 95% CI: 35.25–48.00%, I2: 98.6%, p = 0) took up the highest proportion, and serogroup X (0.02%, 95% CI: 0.00–0.09%, I2: 0.00%, p = 1) accounted for the lowest proportion.
Conclusion
The meningococcal carriage in China was estimated low and varied by region and age group. Understanding the epidemiology and transmission dynamics of meningococcal infection in insidious spreaders is essential for optimizing the meningococcal immunization strategies of the country.
Similar content being viewed by others
Introduction
Neisseria meningitidis (Nm), a gram-negative bacterium that colonizes 10% of the human nasopharynx and spreads through the respiratory droplets of infected people, can cause invasive meningococcal disease (IMD), such as meningitis and septicemia [1, 2]. According to the structure and characteristics of capsular polysaccharides, Nm strains are divided into 12 serogroups (A, B, C, W, X, Y, Z, E, H, I, K, L) and non-groupable serogroups [3]. It is generally believed that six groups (Nm A, B, C, W, Y and X) are the main causes of IMD and that non-groupable Nm is not pathogenic.
Globally, the incidence and mortality of meningococcal disease have continued to decrease since 1990, although differences in age and geographic distribution remained [4, 5]. In 2020, the incidence was 0.56 per 100,000 population in Spain and 0.17 per 100,000 population in Brazil [5]. During 2015–2019, the incidence rate of meningococcal disease in China was 0.078 per million persons, and the case fatality rate was 11.82% [6]. The reported cases of meningitis in China are mainly people aged 10–19 years, accounting for 34.15% (111/325) of the total reported cases of meningococcal disease, followed by people aged 1–9 years, accounting for 29.54% (96/325) [7].
Invasive cases are relatively rare in meningococcal infected cases while most cases are asymptomatic [8]. The phenomenon of asymptomatic colonization in the upper respiratory tract mucosa is known as carriage [2]. The colonization of Nm in the nasopharynx is the initial step in IMD development [9]. The meningococcus of the patient is usually obtained through close contact with carriers rather than patients [10]. Estimates of carriage prevalence are important for studying the dynamics of carriage and disease and for understanding the potential effect of control programs, such as vaccination, on the transmission of meningococci.
In the African meningitis belt, the carriage prevalence of Nm ranged from 0.595% in infants to 1.94% at age 10 [11]. In European countries, the highest carriage prevalence was 23.7% in 19-year old [8]. In the Americas, the prevalence among adolescents and young adults, especially university students and males, was higher than that of other populations [12]. These indicate that differences exist between regions and age groups. The overall carriage prevalence of Nm between 2000 and 2013 in China was 2.7% (95%CI: 2.0–3.5%), but the regional distribution and age distribution was unclear [13]. Understanding the distribution of meningococcal carriage in regions and age groups is critical to understanding the spread of Neisseria meningitidis.
Knowing the carriage prevalence can understand the dynamics of the spread of bacteria in the population, which is the important evidence for evaluating, planning, and implementing intervention measures, such as vaccine immunization. Currently, the meningococcal vaccines marketed in China include Group A meningococcal polysaccharide vaccine (MPV-A), Group A and group C meningococcal polysaccharide vaccine (MPV-AC), Group A, C, Y, and W135 meningococcal polysaccharide vaccine (MPV-ACWY), Group A and group C meningococcal polysaccharide conjugate vaccine (MPCV-AC), Group A and group C meningococcal polysaccharide conjugate and Haemophilus type b conjugate combined vaccine (MPCV-AC-Hib) [14, 15]. There is evidence that meningococcal polysaccharide conjugate vaccines (MPCVs) can reduce nasopharyngeal meningococcal bacteria carriage and have the ability to induce herd protection [16, 17]. There is no group B meningococcal vaccine in China. American CDC’s Advisory Committee on Immunization Practices (ACIP) recommends to vaccinate the quadrivalent meningococcal conjugate vaccine (MenACWY) for teenagers aged 11 or 12 years, and to boost immunization at the age of 16 [18]. Knowing the carriage prevalence of Nm can indirectly indicate the IMD prevalence. Meanwhile, understanding the difference in the carriage prevalence of different age groups can help to adjust the immunization strategy.
We conducted this systematic review and meta-analysis to evaluate the meningococcal carriage prevalence in China and to learn the distribution of Nm and serogroup proportions in positive carriers. Learning the regions and age groups with high level of carriage is important for understanding the transmission dynamics and determination of target population for vaccination. It is of significance for the development of new vaccines, such us serogroup B vaccines, to find out the serogroup with the highest proportion in positive carriers.
Methods
Search strategy and data sources
This review was conducted in accordance with the PRISMA 2020 statement [19] (Additional file 1: Table S1) to identify articles reporting the carriage of Nm in different provinces in China published between 1st January 2005 and 30th April 2022. We searched five databases [China national knowledge infrastructure (CNKI), Wanfang Data Knowledge Service Platform (Wanfang), China Science and Technology Journal Database (VIP), China Biology Medicine disc (CBMdisc) and PubMed] using the following medical subject headings (MeSH) and text words: “Cerebrospinal meningitis”, “Meningococcal meningitis”, “Meningococcal Infections”, “Meningitis”, “Neisseria meningitidis”, “Neisseria”, “Meningococcal”, and “carriage”.
Inclusion and exclusion criteria
Studies were considered for inclusion if they met the following criteria: (1) the studies reported pharyngeal carriage of all meningococcal serogroups from different provinces in China; (2) the subjects of these studies must be healthy populations; (3) the studies were peer-reviewed and published between 1st January 2005 (when MPV-AC was included in the national immunization program) and 30th April 2022; (4) the studies were published in English or Chinese.
Studies were ineligible for inclusion if they met the following items: (1) case reports, case–control reports, outbreak investigations, reviews and other meta-analyses; (2) Studies that reported carriage among cases or close contacts of cases; (3) Studies that only reported the carriage prevalence of a single serogroup of meningococci; (4) studies with incomplete data; (5). Studies that reported the evaluation of the effect of antibiotics or post-chemical prophylaxis research results; (6) Duplicate studies including the same samples.
Data extraction and classification
Study selection (including screening titles and abstracts and assessment through full text review) and data collection were independently conducted by two authors (YMM and XJ). If disagreement occurred, we sought for the recommendation of the third researcher (SZJ). The data extracted from eligible studies included the following aspects: title, first author, publication year, region, research time, sampling methods, lab methods, the number of age groups, the number of carriers and sample size. Provinces were classified into seven geographical regions [20], i.e. northeast (Heilongjiang, Jilin and Liaoning), north (Beijing, Hebei, Inner Mongolia and Shanxi), east (Anhui, Fujian, Jiangsu, Jiangxi and Shandong), south (Guangdong, Guangxi and Hainan), central (Henan, Hubei and Hunan), northwest (Gansu, Ningxia, Qinghai, Shaanxi and Xinjiang), and southwest (Guizhou, Sichuan and Yunnan). Due to the different methods of age groupings reported in different literatures, the median age of each age group in the literature was used for the age grouping of subgroup analysis. The reported age groups of study participants were divided into three groups, i.e. 0–6 years, 7–14 years, and ≥ 15 years, since children aged 0–6 years are required to be vaccinated in the National Immunization Schedule.
Quality assessment
The quality assessment of the included studies was independently conducted by two reviewers (YMM and XJ). The risk of bias tool was used to assess the quality of selected studies according to Damian Hoy’s study, including external validity (Items 1 to 4) and internal validity (Items 6 to 10) [21]. Items included the sampling frame of the sample, the sampling methods, the nonresponse bias, the case definition, the data collected, lab method, and data source. Each question answered “yes” received one point, while the “no” answer for each question received zero. In addition, each question answered “unknown” got 0.5 points. The risk of bias was classified as high (0–5 score), medium (5.5–8 score) and low (8.5–10 score).
Statistical analyses
All statistical analyses were performed in R software (version 4.1.2, Auckland University, USA). We used the metaprop function in the meta package to pool proportions of included studies. Subgroup analyses were conducted by province, region and age group. The Higgins I2 test was used to measure heterogeneity between studies. Heterogeneity was classified as low (0 < I2 ≤ 50%), moderate (50% < I2 ≤ 75%) and high (75% < I2 ≤ 100%). A fixed effect model was performed for studies with low heterogeneity, while a random effect model was used for studies with moderate or high heterogeneity. Funnel plots and Egger’s test were used to evaluate possible publication bias. If publication bias exists, the trim-and-fill method was performed to evaluate the impact of publication bias on the results. Sensitivity analysis was performed to assess the stability of the results by calculating the combined carriages and 95% CIs after excluding each selected study.
Results
Study screening
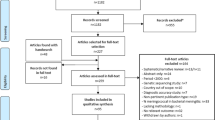
Overall, 2845 records were identified from five databases based on the search strategy. After removing 1370 duplicated records, 1475 studies remained. 1316 records were excluded after screening the titles and abstracts, i.e., 293 records not relevant to Nm, 2 duplicated studies, and 1021 studies associated with Nm but not carriage. In the full text screening process, 159 studies were screened, and 44 studies excluded, i.e., 25 duplicated studies, 4 studies published before 2005, and 15 studies carriage data not reportable. Overall, 115 studies reporting the carriage of Nm in different provinces of China were included in the systematic review and meta-analysis (Fig. 1).
Characterization and quality assessments of included studies
Among the 115 included studies, 114 studies reporting the carriage prevalence of Nm of 28 provinces in China were included regional subgroup analysis (Table 1). 66 studies were cross sectional, 48 were serial cross sectional, and one study was a combination of cross sectional and longitudinal. 57 studies reported on the carrying status of meningococci in different age groups using different grouping methods. 55 studies reported the carriage prevalence with different sampling methods: cluster sampling, cluster stratified random sampling, random sampling, multistage stratified random Sampling, simple random sampling, stratified cluster sampling and stratified random sampling. 104 studies used the isolation and culture of meningococcus as the identification standard, and 10 of them also used PCR as the identification standard.
Most (85.22%, 98/115) included studies received a medium score of the quality assessment (Additional file 1: Fig. S1). No study received a high risk-of bias score. The target population of 115 studies was not well representative of the national population. Most (97.39%, 112/115) studies did not cover a sufficient period of time (≥ 1 year) to account for seasonal variation and 58.26% (67/115) of the included studies did not report whether they used random sampling.
Carriage prevalence by region
The overall carriage prevalence of Nm of all 115 studies was 2.86% (95% CI: 2.25–3.47%, I2: 97.7%, p = 0) with random effect model. In the results of subgroup analysis by province (Fig. 2), the meningococcal carriage rate ranged from 0.00% (95% CI: 0.00–0.66%) in Jilin in northeast China to 15.50% (95% CI: 14.01–16.99%) in Xinjiang in northwest China. In the results of subgroup analysis by region (Table 2), the meningococcal carriage prevalence ranged from 1.65% (95% CI: 1.10–2.20%) in Southwest China to 4.48% (95% CI: 0.91–8.05%) in Northwest China.
Carriage prevalence by age
The age group data were divided into 3 age groups according to the different age groupings of each study (Table 3). Random effect mode was used to generate the weighted carriage rate of each age group. As shown in Table 2, the highest carriage was 4.38% (95% CI: 3.15–5.62%) in age group ≥ 15 years old, and the lowest carriage was 1.01% (95% CI: 0.59–1.43%) in 0–6 years age group.
The proportion of N. meningitidis serogroups in positive cases
As shown in Table 4, random effect model was used to calculated the proportion of Nm serogroups, except NmX and NmY, in positive cases of carriage studies. The proportion of meningococcal serogroup in positive cases ranges from 0.02% (0.00–0.09%) of serogroup X to 41.62% (35.25–48.00%) of serogroup B.
Publication bias and sensitivity analysis
We used funnel plots and Egger’s linear regression to assess the publication bias of all included studies. The result of the funnel plot, which was asymmetric (Fig. 3A), and the P value of Egger’s test (Fig. 3B, P < 0.0001) illustrated the presence of publication bias. The weighted mean carriage rate was 0.91% (95%CI: 0.18–1.64%, Q = 9937.12, p = 0, I2 = 98.4%, 95% CI of I2: 98.3–98.5%) after adding 45 studies by the trim-and-fill method (Fig. 3C). The results of the sensitivity analysis (Additional file 1: Fig. S2) illustrated that the combined carriages and 95% CIs after excluding each selected study did not show much change. The results of the meta-analysis were stable and steady.
Discussion
At present, this is the first systematic review and meta-analysis to describe the regional distribution and age distribution of meningococcal carriage prevalence in healthy people in China. We estimated the overall carriage rate to be 2.85% (95% CI: 2.24–46%), which is lower than that reported in Cuba (31.9%), America (24%) and Brazil (21.5%) [12]. Limited nasopharyngeal swab sampling collection and insufficient laboratory testing capacity in different regions may contribute to the low carriage prevalence of Nm. The transportation of samples may also affect the carriage prevalence of Nm.
More than half of the studies were retrieved from East and North China, with the largest number of studies from Fujian Province of East China. A part (8.06%) of the research subjects were from rural areas [71, 83, 95, 102, 106, 113, 116, 119, 122, 136]. The majority of the study subjects included people of all ages, and only 2 were conducted on primary and middle school students [93, 95]. During 2006 and 2014, the provinces with the most cases of meningitis in China included Anhui (cases = 159) and Jiangsu (cases = 70) provinces in East China and Hebei Province (cases = 61) in North China [137]. Between 2015 and 2019, there were still many cases of meningitis reported in Hebei in North China while cases in Southwest and Northeast were fewer than that of other regions [6]. In a study analyzing the results of surveillance of meningococcal disease in China in 2009, 9743 subjects in eight provinces or cities were tested, and the carriage rate was 0.94% (92/9743), in which Hebei in North China was the province with the highest carriage rate [138].
According to the results of the age subgroup analysis, the meningococcal carriage rates of age group 7–14 and the age group ≥ 15 years old were higher than those of children (0–6 years). In the African meningitis belt, the carriage prevalence of individuals aged 5–19 years were significantly higher than that of other age groups [11]. Since 2010, the meningococcal serogroup A conjugate vaccine (MenAfriVac) has been introduced in 26 countries of the African meningitis belt for individuals aged 1–29 years [139]. In European countries, the carriage prevalence increased from 4.5% in infants to a peak of 23.7% in 19-year-old adolescents and then decreased in adulthood to 7.8% in adults aged 50 [8]. This demonstrates the success of the immunization program of meningococcal serogroup C conjugate (MCC) for children under 18 in UK [140]. In China, the basic immunization population of the five meningococcal vaccines that have been marketed are children aged 0–6 [141]. It is important to improve vaccine strategies to determine whether it is necessary to booster immunization with meningococcal meningitis vaccines among people aged ≥ 7 years.
In our study, the highest and lowest proportion of N. meningitidis serogroups in positive meningococcal carriers was NmB with 41.62% (35.25–48.00%) and NmX with 0.02% (0.00–0.09%). Globally, serogroup B was the foremost cause of invasive meningococcal disease in America, Europe, and the western Pacific [142, 143]. At present, vaccines marked in China includes NmA, NmC, NmW and NmY vaccines except NmB vaccines [14, 15]. It is urgent for the development of serogroup B vaccines.
The results of the funnel plot and trim-and-fill method indicate that there is publication bias in this study. As 114 studies were regional and small-scale studies, the target population of these studies was not well representative of the national population (Additional file 1: Fig. S1). This review includes only published studies without unpublished literature whose results may be not significant.
A limitation of this review is that there is no unified standard on sample collection and laboratory testing methods, which can cause bias that impacts the results of meta-analysis. Inconsistent diagnostic methods and a lack of diagnostic kits may lead to underestimation or misinformation of the data reported in the study.
Understanding the carriage prevalence of Nm in generalizable populations contributes to providing evidence for further improvement of meningococcal vaccine and vaccination strategies. This is important for the prevention of meningitis and development of vaccines in China in the future.
Conclusion
In summary, the meningococcal carriage in China was estimated low and varied by region and age group. Based on our findings, we suggest that the surveillance on epidemic cerebrospinal meningitis among generalizable populations in each province and region in China should be enhanced. The age distribution of meningococcal carriage highlights the importance of monitoring and booster immunization among teenagers aged ≥ 7 years.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- Nm :
-
Neisseria meningitidis
- IMD:
-
Invasive meningococcal disease
- CNKI:
-
China national knowledge infrastructure
- Wanfang:
-
Wanfang Data Knowledge Service Platform
- VIP:
-
China Science and Technology Journal Database
- CBMdisc:
-
China Biology Medicine disc
- MeSH:
-
Medical subject headings
- MPV-A:
-
Group A meningococcal polysaccharide vaccine
- MPV-AC:
-
Group A and group C meningococcal polysaccharide vaccine
- MPV-ACWY:
-
Group A, C, Y, and W135 meningococcal polysaccharide vaccine
- MPCV-AC:
-
Group A and group C meningococcal polysaccharide conjugate vaccine
- MPCV-AC-Hib:
-
Group A and group C meningococcal polysaccharide conjugate and Haemophilus type b conjugate combined vaccine
References
Tefera Z, Mekonnen F, Tiruneh M, Belachew T. Carriage rate of Neisseria meningitidis, antibiotic susceptibility pattern and associated risk factors among primary school children in Gondar town, Northwest Ethiopia. BMC Infect Dis. 2020;20(1):358. https://doi.org/10.1186/s12879-020-05080-w.
Yazdankhah SP, Caugant DA. Neisseria meningitidis: an overview of the carriage state. J Med Microbiol. 2004;53(Pt 9):821–32. https://doi.org/10.1099/jmm.0.45529-0.
Peterson ME, Li Y, Shanks H, Mile R, Nair H, Kyaw MH, Meningococcal CG. Serogroup-specific meningococcal carriage by age group: a systematic review and meta-analysis. BMJ Open. 2019;9(4): e024343. https://doi.org/10.1136/bmjopen-2018-024343.
Collaborators GBDM. Global, regional, and national burden of meningitis, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(12):1061–82. https://doi.org/10.1016/S1474-4422(18)30387-9.
Alderson MR, Arkwright PD, Bai X, Black S, Borrow R, Caugant DA, Dinleyici EC, Harrison LH, Lucidarme J, McNamara LA, et al. Surveillance and control of meningococcal disease in the COVID-19 era: a global meningococcal initiative review. J Infect. 2022;84(3):289–96. https://doi.org/10.1016/j.jinf.2021.11.016.
Li JH, Wu D, Wen N, Zheng H, Shi W, Xu L, Shao ZJ, Yin ZD, Li YX. Serogroup distribution of meningococcal meningitis in China, 2015–2019. Chin J Vaccines Immun. 2020;26(03):241–4.
Li JH, Wu D, Yin ZD, Li YX. Analysis of epidemic characteristics for meningococcal meningitis in China during 2015–2017. Chin J Prev Med. 2019;02:159–63. https://doi.org/10.3760/cma.j.issn.0253⁃9624.2019.02.007.
Christensen H, May M, Bowen L, Hickman M, Trotter CL. Meningococcal carriage by age: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10(12):853–61. https://doi.org/10.1016/s1473-3099(10)70251-6.
Soriano-Gabarro M, Wolter J, Hogea C, Vyse A. Carriage of Neisseria meningitidis in Europe: a review of studies undertaken in the region. Expert Rev Anti Infect Ther. 2011;9(9):761–74. https://doi.org/10.1586/eri.11.89.
Serra L, Presa J, Christensen H, Trotter C. Carriage of Neisseria meningitidis in low and middle income countries of the Americas and Asia: a review of the literature. Infect Dis Therapy. 2020;9(2):209–40. https://doi.org/10.1007/s40121-020-00291-9.
Cooper LV, Kristiansen PA, Christensen H, Karachaliou A, Trotter CL. Meningococcal carriage by age in the African meningitis belt: a systematic review and meta-analysis. Epidemiol Infect. 2019;147: e228. https://doi.org/10.1017/S0950268819001134.
Santos-Neto JF, Ferreira VM, Feitosa CA, Martinez-Silveira MS, Campos LC. Carriage prevalence of Neisseria meningitidis in the Americas in the 21st century: a systematic review. Braz J Infect Dis. 2019;23(4):254–67. https://doi.org/10.1016/j.bjid.2019.06.006.
Zhang Y, Wei D, Guo X, Han M, Yuan L, Kyaw MH. Burden of Neisseria meningitidis infections in China: a systematic review and meta-analysis. J Glob Health. 2016;6(2): 020409. https://doi.org/10.7189/jogh.06.020409.
Association CPM. Efficacy, safety, and cost⁃effectiveness of meningococcal vaccines. Chin J Prev Med. 2019;25(01):102-108+114.
China NHCotPsRo. Immunization schedules and instructions for vaccines of the national immunization program (2021 version). Chin J Viral Dis. 2021;2021:241–5. https://doi.org/10.16505/j.2095-0136.2021.0021.
Pizza M, Bekkat-Berkani R, Rappuoli R. Vaccines against meningococcal diseases. Microorganisms. 2020. https://doi.org/10.3390/microorganisms8101521.
McMillan M, Chandrakumar A, Wang HLR, Clarke M, Sullivan TR, Andrews RM, Ramsay M, Marshall HS. Effectiveness of meningococcal vaccines at reducing invasive meningococcal disease and pharyngeal Neisseria meningitidis carriage: a systematic review and meta-analysis. Clin Infect Dis. 2021;73(3):E609–19. https://doi.org/10.1093/cid/ciaa1733.
Mbaeyi SA, Bozio CH, Duffy J, Rubin LG, Hariri S, Stephens DS, MacNeil JR. Meningococcal vaccination: recommendations of the Advisory Committee on Immunization Practices, United States, 2020. MMWR Recomm Rep. 2020;69(9):1–41. https://doi.org/10.15585/mmwr.rr6909a1.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71. https://doi.org/10.1136/bmj.n71.
Ye Z, Zeng G, Yang H, Li J, Tang K, Wang G, Wang S, Yu Y, Wang Y, Zhang T, et al. The status and characteristics of urinary stone composition in China. BJU Int. 2020;125(6):801–9. https://doi.org/10.1111/bju.14765.
Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, Baker P, Smith E, Buchbinder R. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–9. https://doi.org/10.1016/j.jclinepi.2011.11.014.
Lan YY, Jiang XC, Lu XY. Analysis on epidemiological features of patients with epidemic cerebrospinal meningitis in Quzhou from 1985 to 2010. Chin Prev Med. 2012;13(05):377–9. https://doi.org/10.16506/j.1009-6639.2012.05.018.
Ding RC. Investigation on the level of meningococcal immunity and bacteria-carrying status of healthy people in Yunxi District from 2011 to 2012. Chin J of PHM. 2013;29(03):374–5.
Liang XM, Cao JD, Luo XJ, Sun BJ. The analysis of healthy people suffering from cerebrospinal meningitis in Yi Liang County in 2014. China’s Rural Health. 2018;04:34.
Zhang HF, Liu YY, Li SF, Chang XL, Zhang DW, Wu FY, Ren LH, Lin Z. Surveillance report of Neisseria meningitidis carrying and antibody levels in healthy people in Kezuozhong Banner, Tongliao City. J Dis Monit Control. 2010;4(12):658.
Hu WJ, Wang RZ, Wang YQ, Zhang SB. Neisseria meningitidis carriage prevalence and serogroup distribution among a healthy population of Shaanxi province. J Pract Med. 2020;36(06):796–800.
Wang YQ, Zhang SB, Wang RZ, Kou GP, Gao T, Hou TJ, Wang ZG. A carriage survey of Neisseria meningitidis among a healthy population in Guanzhong region, Shaanxi province. Chin J Vaccines Immun. 2017;23(04):375–8.
Yang TT, Wang XF, Chang SY, Guang M, Wang H, Yang HX. Analysis of epidemic cerebrospinal meningitis in healthy people in Shanxi Province from 2016 to 2017. Chin Rem Clin. 2019;19(10):1619–20.
Lai HL, Wang H, Hu QB, Cao CY, Liao LH. An investigation on meningococcal meningitis group A, group C antibody level and the pathogen rate of partly healthy population in Longyan City. J Dis Monit Control. 2011;5(09):521–2.
Zhang JL, Gu LN. Surveillance and analysis of immune level and carrier rate of epidemic meningitis in healthy population in Lianyungang City from 2014 to 2016. Pract Prev Med. 2019;26(09):1126–8.
He XP. Surveillance and Analysis of Antibody Level and Carrier Status of Meningococcal Healthy Population in Jiangyou City. World Health Digest Med Period. 2013;4:98–9. https://doi.org/10.3969/j.issn.1672-5085.2013.04.086.
Liu ZY, Nie W, Liu LZ, Hu GC, Shan XY, Bai AY. Monitoring results and analysis of Neisseria meningitides carrying status among healthy population in Jinan from 2008 to 2015. Chin J Health Lab Tec. 2016;26(23):3436–40.
Wang YT, Jia ZY, He BH, Ma HS, Wang Q, Jiang X, Qian ZY, Liu XL, Chen SL, Sun YQ. Analysis of Neisseria meningitidis carriage situation among healthy population in Hebei Province from 2006 to 2013. Chin J Vaccines Immun. 2015;21(05):506-510+518.
Liu ZW, Jin YH, Zeng Z. Investigation on immune level against epidemic cerebrospinal meningitis and carrier status among healthy population in Hefei. J Med Pest Control. 2017;33(07):726–9. https://doi.org/10.7629/yxdwfz201707005.
Deng HY, Sun LY, Zeng XX, Wang SL, Huang CH, Fu ZW, Yan XJ, He J, Pan TT, Li WH, et al. Survey of Neisseria meningitiis-carrying rate and detection of antibody level in Hainan in 2006. China Trop Med. 2010;10(11):1365–6. https://doi.org/10.13604/j.cnki.46-1064/r.2010.11.009.
Cui M, Xu JX, Cai YS, Fu CX, Li MX, Zhang CH, Li KB, Wang M. Level of immunity against epidemic cerebrospinal meningitis and the carrier status among healthy population in 2009–2011 in Guangzhou. J Trop Med. 2013;13(08):1015–7.
Wu XH, Lin M, Quan Y, Fang JS, Liang DB, Qin WW, Qiu XQ. Reaserch on bacteria carrying antibody level and control strategy for epidemic cerebrospinal meningitis in Guangxi. Chin J Sch Health. 2010;03:337–9. https://doi.org/10.16835/j.cnki.1000-9817.2010.03.035.
Qiu DS, Zhang YD, Tan CJ. Investigation and analysis of carrier rate for Neisseria meningitides among healthy population from 2013 to 2014 in Gaomi City. Chin J Hosp Stat. 2016;23(01):35–7.
Jiang WP, Bi C. Investigation of meningococcal antibody level and bacteria carrying situation in healthy population in Danyang City. Jiangsu J Prev Med. 2014;25(03):56–7.
Chu HN, Wei F, Zhao GL, Wang W, Li QL, Li Q. Surveillance on the rate of the healthy carrier from 2013 to 2014 of epidemic Neisseria meningitis (NM) in Chengde city. J Med Pest Control. 2016;32(05):494–6. https://doi.org/10.7629/yxdwfz201605008.
Zhou YH. Investigation on the infection rate and immune level of epidemic cerebrospinal meningitis among healthy people in Wujin District of Changzhou in 2011. Jiangsu J Prev Med. 2012;23(05):55–6.
Jia B, Zhang N, Shi Q, Chen TJ, Chu P. Analysis on the status of meningococcal infection among healthy people from 2009 to 2013 in Chaoyang District. Beijing Pract Prev Med. 2016;23(5):614–615+627.
Niu HC, Wu Y, Shu GL, Gao JX. Analysis of presence status, serotype distribution and antibiotic susceptibility of Neisseria meningitidis among healthy residents in Changping district of Beijing, 2016. Jiangsu J Prev Med. 2018;29(2):131–4.
He F, Yang HM, Li GM, Zhu BQ, Zhang Y, Jiang HL, Yuan M, Jiang Y, Lv J. Neisseria meningitidis carriage and risk factors among teenagers in Suizhou city in China. Epidemiol Infect. 2020;148: e227. https://doi.org/10.1017/s0950268820002113.
Xue WH, Pang ZL, Zhang Y, Liu ZL, Zhao MQ. Analysis of the surveillance results of meningomyelitis among healthy population in Pingshan in 2015. Chin J Health Lab Tec. 2016;26(07):1020-1021+1024.
Zheng QX, Zhang HT, Sun H, Gao P, Dong M. The condition of Neisseria meningitidis of the non-epidemic season among healthy people during 2015–2017 in Dongcheng district, Beijing. Cap J PubIic Health. 2019;13(04):189–91.
Geng L, Sun RC, He BH, Zhang HX, Jia ZY, Wang YT, Sun YQ. Analysis of Neisseria meningitidis carriage situation among healthy population in Hebei Xinji City from 2015 to 2016. J Med Pest Control. 2017;33(11):1182–4. https://doi.org/10.7629/yxdwfz201711019.
Liao YH, Lin W, Cao CY, Chen JX, Guo ZZ, He Y. Surveillance on epidemic cerebrospinal meningitis among the healthy population, Longyan city, 2014–2016. Prev Med Trib. 2017;23(07):476-558–9.
Xie FQ, Li QW, Luo CC, Lin ZY, Chen AP. Analysis on carrying rate of Neisseria meningitis and antibody level of epidemic cerebrospinal meningitis among the healthy population in epidemic period in two cities, Fujian Province, 2011. Prev Med Trib. 2016;22(04):260–2. https://doi.org/10.16406/j.pmt.issn.1672-9153.2016.04.007.
Hu YF, Lu YP, Zhang BQ. Investigation on carrier status of epidemic miningitis virus and immune level among healthy people in Pingnan County in 2009. Prev Med Trib. 2011;17(01):39-40+43.
Liang SG, Wang BY. Investigation on antibody level against epidemic cerebrospinal meningitis and carriage rate of Neisseria meningitidis among healthy population in Harbin in 2009. Chin Foreign Med Res. 2011;9(13):126–8. https://doi.org/10.14033/j.cnki.cfmr.2011.13.084.
Yan YF, Zhao LP, Guo NN, Ma YX, Li YX, Li RF, Deng J, Huang L. Germ-carrying rate of epidemic cerebrospinal meningitis and molecular typing of bacteria among healthy population in Handan City, 2009–2015. Pract Prey Med. 2018. https://doi.org/10.3969/j.issn.1006-3110.2018.02.023.
Tang XL. Investigation on germ-carrying situation on Neisseria meningitidis (Nm) of health populations in Qinghai Province in 2007. Mod Prev Med. 2010;37(03):555–6.
Wang ML, Qu WJ, Sai JY, Liu Y, Liu T. Analysis of Neisseria meningitidis carrier monitoring data in healthy people in Wendeng City, 2007–2010. Prev Med Trib. 2011;17(07):654+657. https://doi.org/10.16406/j.pmt.issn.1672-9153.2011.07.030.
Wang ZJ, Wang JT, Zheng LF, Zheng JB. Investigation and analysis of meningococcal disease in healthy people in Wen County from 2004 to 2008. Henan J Prev Med. 2010;21(04):277–8. https://doi.org/10.13515/j.cnki.hnjpm.2010.04.035.
Qi YM, Gao YH, Lu JR, Wang CD, Pang ZQ. Monitoring results of epidemic cerebrospinal meningitis pathogen among healthy population in Cangzhou from 2000–2013. Occup Health. 2014. https://doi.org/10.13329/j.cnki.zyyjk.2014.16.039.
Luan L, Zhan YH, Zhang MH, Bi C, Zhu YH, Zhang J, Zheng BF, Chen T. Epidemiological analysis of the meningococcal disease in Suzhou City during 1992–2012. Mod Prev Med. 2014;41(12):2113-2115+2118.
Hao CX, Yuan H, Luo LZ, Li YC, Zhu XP, Liu LG. Results of surveillance of Group A、C、Y and W135 of epidemic cerebrospinal meningitis in Hejiang County of Sichuan Province in 2008. China Trop Med. 2010;10(02):165–6. https://doi.org/10.13604/j.cnki.46-1064/r.2010.02.037.
Gao JZ, He F, Wu LQ, Song XJ, Liu HB, Zhang YT, Yang HM, Lv J. Epidemiological characteristics of epidemic cerebrospinal meningitis from 1971 to 2018 and trend of Neisseria meningitidis in Shiyan City. Int J Lab Med. 2019;40(23):2858–63. https://doi.org/10.3969/j.issn.1673-4130.2019.23.010.
Lan RW, Liu MZ, Deng LL, Xu L, Mao WC, Yu HF, Wen DL, Wu L, Zeng LY, Meng NX, et al. Neisseria meningitidis carriage prevalence and serogroup distribution among a healthy population. Chin J Vaccines Immun. 2014;20(05):438–41.
Wang YF, Zhang YY. Monitoring report of meningococcal meningitis in Jiaxiang County in 2012. Zongheyixue. 2013;10(19):154–5. https://doi.org/10.3969/j.issn.1674-4985.2013.19.075.
Liu Q, Seng MH, Li MY, Guo YH, Xu J. Surveillance and analysis of epidemic cerebrospinal meningitis in Henan Province from 2010 to 2011. China Health Care Nutr. 2013;23(10):6133–4. https://doi.org/10.3969/j.issn.1004-7484(x).2013.10.685.
Ye XF, Liu CT, Zhao ST, Zhang L, Zhu Q, Ren G. Laboratory surveillance result analysis of epidemic cerebrospinal meningitis (EMC) in Guizhou Province. Open J Nat Sci. 2017;5(01):73–8. https://doi.org/10.12677/ojns.2017.51011.
Yuan L, Lin ZY, Wang ZM, Wen CJ, Cao CY, Yang ZQ, Zhang BQ. The surveillance of meningococcal infection and antibody levels in Fujian Province in 2009. Strait J Prev Med. 2012;18(01):29–31.
Yuan HZ, Cai BL, Li YC, Liu J, Chen QY. Epidemiological analysis of epidemic cerebrospinal meningitis in Dongguan City from 2008 to 2010. South China J Prev Med. 2012;38(6):39–40, 43.
Xiao D, Yang SH, Han YN. Analysis of epidemiological surveillance results of epidemic cerebrospinal meningitis in Dalian from 1996 to 2010. J Dis Monit Control. 2011;5(11):655–7.
Cheng FY. Analysis of the incidence of meningococcal meningitis and monitoring results in Feidong County, Anhui Province in 2009. Anhui Med J. 2012;33(06):739–40.
Sun X, Liu YB, Xu Y, Wang ZG, Tang FY. Analysis of epidemic characteristics and antibody level of epidemic cerebrospinal meningitis in Jiangsu province during 2014–2015. Mod Prev Med. 2018;45(14):2510-2512+2520.
Liu HT, Zhuang GL, Wang ZY, Song JH, Zhou B. Analysis of Neisseria meningitidis carrier rate among healthy people during 2013–2015 in Mentougou district. Beijing Cap J Public Health. 2016;10(2):78–9.
Xu SX. Analysis of the carrier and antibody levels of Neisseria meningitidis in some healthy people in Luanping County in 2012. Prev Med Trib. 2013;19(06):447–8. https://doi.org/10.16406/j.pmt.issn.1672-9153.2013.06.033.
Lu LR, Wnag CD, Yang Y, Dong XJ, Li XZ, Dai GJ. Status of epidemic cerebrospinal meningitis in rural areas of Xianxian County, 2012. J Prev Med Inf. 2013;29(09):755–7.
Li MS, Lin XJ, Wang M, Lv JJ, Zhang Y, Fu ZY, Xiao ZK, Xu Q, Song LZ. Analysis on pathogen surveillance data of epidemic cerebrospinal meningitis in Shandong Province, 2008–2009. Prev Med Trib. 2010;16(09):835–7. https://doi.org/10.16406/j.pmt.issn.1672-9153.2010.09.028.
Deng X, Yao PP, He HQ, Yan R, Tang XW, Zhou Y, Fu J, Xie SY. Epidemiological characteristics of meningococcal meningitis and changing trend of serogroups of Neisseria meningitidis in Zhejiang, 2006–2017. Dis Surveil. 2018;33(07):547–51.
Chen LJ, Cui WJ, Feng JG, Xu L, Chen YM, Huang H, Tang JH. Surveillance of epidemic cerebrospinal meningitis in Shaoguan City, 2006–2008. J Occup Health Damage. 2012;27(03):160–2.
Yan XP, Zeng YQ, Liu GR, Li YC, Luo LZ. Carriage of Neisseria meningitidis and immunity level among healthy population in Jiajiang County, 2006–2008. J Prev Med Inf. 2010;26(4):276–9.
Yuan H, Luo LZ, Li YC, Hao CX, Tang XY, Lv Q, Liu LG, Zhu XP. Surveillance of epidemic cerebrospinal meningitis in Sichuan Province, 2005 to 2008. J Prev Med Inf. 2010;26(05):340–3.
Wu JJ, Song KJ, Zhang T, Yang H, Zhao JY, Wu CC, Zhang J. Epidemiological characteristics of meningococcal meningitis and changing trend of serogroups of Neisseria meningitidis in Jinan, 1991–2018. Mod Prev Med. 2020;47(19):3598-3601+3606.
Wang Y, Fu RH, Gu SY, Han Y. Analysis for surveillance on epidemic cereborspinal meningitis in Liaoning Province during 1950 to 2013. Chin J Public Health Eng. 2016;15(06):582–3.
Chen SX. Study on the prevalence trend of new meningococcal Y and W135 groups 2013.
Li QW, Yuan WH, Zheng EH, Yuan L, Lin ZY, Chen AP. Monitoring and analysis of epidemic cerebrospinal meningitis infection rate and antibody level in healthy population in Fujian province in 2012. Chin J Health Lab Tec. 2014;24(02):244–6.
Yang XF. Surveillance of Neisseria meningitides carrier incidence in Changsha population. Pract Prev Med. 2007;03:732–3.
Fu XQ, Yin JW, Gao Y. Analysis of survey results of meningococcal pathogens in healthy people in Yunnan Province in 2005. Pract Prev Med. 2006;13(2):341–2. https://doi.org/10.3969/j.issn.1006-3110.2006.02.052.
Yang TP. The monitoring analysis of groups of healthy people suffering from cerebrospinal meningitis in Wengyuan County in 2006. Chin Prim Health Care. 2007;21(7):40–1. https://doi.org/10.3969/j.issn.1001-568X.2007.07.018.
Li XC, Li Y, Zhang HC, Lin GK, Chen HY, Zhang LY, Hong CJ, Wang LH. Surveillance analysis of epidemic cerebrospinal meningitis in Wenzhou. Dis Surveil. 2007;06:390-391+404.
Fan YS, Zhang LS, Wang JH. Survey of N meningitidis carrier in healthy confluence of Tangshan. Chin J Health Lab Technol. 2008;04:690–1.
Guo F, Liu XH, Jiang B, Peng B, Huang XM, Wang YG, Nie SF. Analysis on the surveillanee results of epidemic cerebrospinal meningitis in the healthy people in Suizhou city from 2001 to 2006. Chin J Dis Control Prev. 2007;11(5):482–4. https://doi.org/10.3969/j.issn.1674-3679.2007.05.012.
Shi SJ, Xu QY, He ZQ. Surveillance of antibody levels and carrying rate of epidemic meningitis of group A and group C of healthy people in Suzhou City in 2005. J Med Pest Control. 2006;22(2):106–8. https://doi.org/10.3969/j.issn.1003-6245.2006.02.014.
Zhang SX. Epidemiological survey on the distribution of epidemic cerebrospinal meningitis in Shenyang. China Mod Med. 2009;07:136.
Chen Y, Wang YC. Surveillance and analysis of epidemic cerebrospinal meningitis in Shenyang City in 2005. Modern Preventive Medicine. 2007;34(4):855,861. https://doi.org/10.3969/j.issn.1003-8507.2007.04.080.
Wen QW, Duan YX, Ju CY. Situation of taking Neisseria meningitidis in health population in Shenzhen. J Prev Med Inf. 2006;05:527–9.
Ju CY, Huang WF, Yu MH, Liu HJ, Duan YX. Survey of prevalence of Neisseria meningitidis in heathy population in Shenzhen City in 2005 and 2006. China Trop Med. 2008;8(1):80–1. https://doi.org/10.3969/j.issn.1009-9727.2008.01.044.
Li GH, Gao XF, Zhang QX, Zuo SJ, Hao RE. Investigation and analysis on the status of epidemic cerebrospinal meningitis in healthy people in Shanxi Province in 2005. Chin Rem Clin. 2006;6(9):696. https://doi.org/10.3969/j.issn.1671-2560.2006.09.018.
Zhang JM, Jin WE, Ye CH. Situation of carrier rate of Neisseria meningitides in school healthy population in Quzhou City during 2003–2008. Chin J Health Lab Technol. 2009;19(7):1647-1648,1669.
Jia YJ. Investigation on the carrier and antibody levels of Neisseria meningitidis in healthy people in Qinghai Province. Chin J Vaccines Immun. 2008;05:460.
Yang Y, Liang JL, Ju CY, Su HW, Chen ZQ, Gan ZL, Liu HC. Investigation on the germ-carrying status of epidemic meningitis among health rural students in primary and middle school of Luzhou. Mod Prev Med. 2008;12:2347–9.
Cao CY, Chen QJ, He Y, Lin ZY, Yuan L. Analysis on the status of meningococcal bacteria and immune level in some healthy people in Longyan City in 2006 and 2007. Strait J Prev Med. 2009;03:45–6.
Yang M, Yuan H, Liu XQ, Ding S, Xu JM, Xu XQ, Shao ZJ, Cui ZG, Xu L, Diao BW. Investigation on carriage of Neisseria meningitidis and analysis of serogroup C strains by PFGE in Jiangxi Province, 2005. Chin J Vaccines Immun. 2007;03:200–2.
Liu XQ, Yuan H, Yang M, Xie Y, Xu XQ, Liao YJ. Prevalence of epidemic cerebrospinal meningitis in Jiangxi Province. Chin J Public Health. 2009;25(8):907–8. https://doi.org/10.3321/j.issn:1001-0580.2009.08.051.
Zhong ZL, Yu LG. Investigation of carrying status and immune level of meningitides in health population in Lishui County of Jiangsu Province. Occup and Health. 2008;24(16):1671–3. https://doi.org/10.3969/j.issn.1004-1257.2008.16.037.
Lu W. Investigation on immune level and carrier status of epidemic meningitis in healthy population. World Health Digest Med Period. 2008;5(4):521–2.
Lv J, Liu L, Sun J, Cheng JF, Lin FR, Wu HX. Analysis of the surveillance of epidemic cerebrospinal meningitis in Hubei, 2000–2005. J Pub Health Prev Med. 2006;17(4):41–4. https://doi.org/10.3969/j.issn.1006-2483.2006.04.015.
Qian ZY, Ma HS, Sun YQ, Zhen SJ, Li YP, Jiang X, Wang YT, Liu HB. Surveillance and analysis of bacteria carrying in healthy population with epidemic cerebrospinal meningitis from 2007 to 2008 in Hebei. Hebei Med J. 2009;31(14):1819–20. https://doi.org/10.3969/j.issn.1002-7386.2009.14.069.
Wang XP, Jin YH, Wang H. Investigation of the infection rate and antibody level on epidemic cerebrospinal meningitis in the epidemic prophase and metaphase in healthy people in Hefei. Chin J Vaccines Immun. 2007;13(6):548–51. https://doi.org/10.3969/j.issn.1006-916X.2007.06.010.
Yan XJ, Sun LY, Zeng ZC, Fu ZW, Deng HY, Chen SM. Survey of distribution of epidemic cerebrospinal meningitis bacterium and the population immunity level in Hainan Province. China Trop Med. 2006;6(2):244–5. https://doi.org/10.3969/j.issn.1009-9727.2006.02.017.
Song T, He JF, Liu MZ. Epidemic analysis on meningococcal meningitis prevalence status and control effect in Guangdong Province in 2005. Chin J Vaccines Immun. 2007;03:203–5.
Zhao LF, Xi JL. Analysis of monitoring results of meningococcal disease and immune level among healthy people in Guyuan City Ningxia. Med J. 2007;12:1155.
Yang JY, Yang SM, Zhang GY, Yu DS, Yang JJ, Zhao XH. Analysis of the surveillance results of the population carrying bacteria in the peak season of meningitis in 2005. Health Vocat Educ. 2005;23(23):82–3. https://doi.org/10.3969/j.issn.1671-1246.2005.23.057.
Lin P, Pan ZY, Liu H. An investigation on the infection rate and immune level of epidemic cerebrospinal meningitis among healthy people in Fuzhou. Dis Surveil. 2007;08:536.
Yang HK, Zhang LP, Liu MZ. Analysis of surveillance results of meningococcal meningitis among healthy people in Dongguan in 2005. Chin J Health Lab Technol. 2006;01:76–7.
Luo SH, Zhang LP, Huang SZ, Li JQ. Analysis of surveillance results of meningococcal meningitis in Dongguan from 2004 to 2005. Chin J Health Lab Technol. 2006;06:701–2.
Teng Y. Analysis of serum surveillance of meningococcal meningitis among healthy people in Dehui City in 2008. Chin J Public Health Eng. 2009;S1:20–1.
Zou YG, Chen JW, Li TP, Luo XJ, Wu CL, Peng JJ, Dai DF. Investigation on antibody level against epidemic cerebrospinal meningitis and carriage rate of Neisseria meningitidis among healthy population in Qidong County in 2008. Pract Prev Med. 2009;02:410–1.
Gu HY, Chen BY, Chu XJ. Surveillance of epidemic cerebrospinal meningitis in Langfang City, Hebei Province in 2008. J Trop Dis Parasitol. 2009;02:103–4. https://doi.org/10.3969/j.issn.1672-2302.2009.02.017.
Wu XH, Lin M, Quan Y, Fang JS, Wang ML, Qin WW. Study on healthy carrier and antibody level for meningococcal meningitis in Guangxi, 2008. Appl Prev Med. 2009;06:331–4.
Wang WJ, Kuang SS, Han ZM, Liu YM, You CQ, Gou N, Zhou GH, Zhou S, Zhao SM. Investigation on antibody level and carriage rate of Neisseria meningitidis in healthy population before epidemic period in Chongqing. Prog Microbiol Immunol. 2008;03:29–33. https://doi.org/10.13309/j.cnki.pmi.2008.03.015.
Sun YQ, Ma HS, Zhen SJ, Jiang X, Qian ZY, Li YP, Liu HB, Wang YT. AnaIysis of epidemic cerebrospinal meningitis surveillance in Hebei province in 2007. Dis Surveil. 2008;23(10):634–6. https://doi.org/10.3784/j.issn.1003-9961.2008.10.015.
Huang RN. Analysis on Neisseria meningitidis carriage status of residents in health population in Chengdu District. Strait J Prev Med. 2009;04:13–5.
Cong QM, Tang SH, Zhang JB, Sun Q, Xiao HC. Investigation on the carrying status of Neisseria meningitidis in some healthy people in Weihai City from 2007 to 2008. Prev Med Trib. 2009;09:911. https://doi.org/10.16406/j.pmt.issn.1672-9153.2009.09.031.
Yin JW, Gao Y, Fu XQ, Zhou YM, Yang JB, Gu WP. Investigation on the status of meningococcal disease in healthy people in some areas of Yunnan Province in 2006. J Prev Med Inf. 2007;03:362–3.
Ren LH, Liu YY, Wu FY, Chang XL, Yang HM. Investigation on Neisseria meningitidis and the level of immune antibody among healthy population in Tongliao City in 2006. Prev Med Trib. 2008;01:57–8.
Gong Y, Luo XC, Zhao Q, Cai SW, Zhong GX. Investigation on the level of meningococcal antibody and the rate of infection among healthy people in Sanming City in 2006. Strait J Prev Med. 2009;15(5):33.
Wang J, Yan LQ. Surveillance analyses on epidemic cerebrospinal meningitis of Zhongwei city of Ningxia in 2006. Chin Health Lab Technol. 2007;03:495–6.
Xiao ZK, Song LZ, Li MS, Wang M, Zhang L, Xu Q, Xu AQ. Epidemiological analysis for epidemic cerebrospinal meningitis in Shandong Province from 2006 to 2008. Prev Med Trib. 2009;09:805-806+836. https://doi.org/10.16406/j.pmt.issn.1672-9153.2009.09.027.
Luo XC, Luo LM, Gong Y, Luo HH, Cai SW, Zhao Q. Analysis of surveillance results of epidemic cerebrospinal meningitis in Sanming City in 2005. Chin J Health Lab Technol. 2006;04:451–2.
Li X, Wu CP, Bai L. Investigation on antibody level and epidemic cerebrospinal meningitis in Inner Mongolia 2005. Prev Med Trib. 2007;13(10):883–4. https://doi.org/10.3969/j.issn.1672-9153.2007.10.008.
Wang H, Zhang XL, Yang YL. Investigation and analysis of Neisseria meningitides infection status of residents in Hefei District. Anhui Prev Med. 2007;13(1):17–8.
You L, Tian KC, Yao GH, Nie W, Zou ZT. Investigation on the status of healthy population carrying bacterial pathogens of epidemic cerebrospinal meningitis in Guizhou Province in 2005. Dis Surveil. 2006;21(3):120–2. https://doi.org/10.3784/j.issn.1003-9961.2006.03.005.
Liu MZ, Yang HK, Liao GD, Huang ZS, Xu L, Deng XL, Tan HL, Chen JD, Song T. Investigation on antibody level against epidemic cerebrospinal meningitis and carriage rate of neisseria meningitidis in healthy population in Guangdong Province. Chin J Health Lab Technol. 2007;17(2):325-326,338. https://doi.org/10.3969/j.issn.1004-8685.2007.02.057.
Zhang Y, Li MS, Liu GF, Lin XJ, Feng L, Xu AQ, Zhang L. Analysis of Neisseria meningitidis carriage characteristics among healthy population in Shandong province from 2008 to 2020. Chin J Prev Med. 2021;55(08):973–7. https://doi.org/10.3760/cma.j.cn112150-20210412-00358.
Luo JJ, Lv J, Li TT, Xiao J. Analysis of the monitoring results of Neisseria meningitidis carrier rate among healthy people in Hubei Province from 2013 to 2018. Appl Prev Med. 2021;27(02):180-182+184.
Xie N, Fu WH, Zhu BQ, Wang TM, Chen T, Hanaxi Z, Xu L, Shao ZJ, Cui Y. Epidemiological and etiologic characteristics of Meningococcal meningitis in Xinjiang Uygur Autonomous Region, 1960–2019. Chin J Epidemiol. 2021;42(6):1037–43.
Zhou XH, Zhang GQ, Fei YH. Surveillance on bacterial carrier and immune level of epidemic cerebrospinal meningitis among healthy people in Lianshui County in 2018. Anhui J Prev Med. 2021;27(3):238-240,252. https://doi.org/10.19837/j.cnki.ahyf.2021.03.017.
Jiang M, Zhao JJ, Cheng X, Liu JS. Investigation on antibody and carrier rate of epidemic meningitis A and C in Lianshui County. Prev Med. 2021;33(10):1053–6. https://doi.org/10.19485/j.cnki.issn2096-5087.2021.10.020.
Chen C, Ren Y, Guo N, Zheng Y, Li YZ, Tang C, Tan YZ, Li JC, Wang XF, Cun W, et al. Investigation on carrying status of Neisseria meningitidis in healthy population in Baoshan City, Yunnan Province, China. Chin J Biol. 2021;34(05):571–4. https://doi.org/10.13200/j.cnki.cjb.003337.
Zhang Y, Deng X, Jiang Y, Zhang J, Zhan L, Mei L, Lu H, Yao P, He H. The epidemiology of meningococcal disease and carriage, genotypic characteristics and antibiotic resistance of Neisseria meningitidis Isolates in Zhejiang Province, China, 2011–2021. Front Microbiol. 2021;12: 801196. https://doi.org/10.3389/fmicb.2021.801196.
Lu JR, Wang CD, Bi HJ, Li XZ. Test results analysis of epidemic cerebrospinal meningitis carrier in Cangzhou Area from 2008–2011. Occup Health. 2012;28(21):2–3. https://doi.org/10.13329/j.cnki.zyyjk.2012.21.041.
Li JH, Li YX, Wu D, Ning GJ, Shao ZJ, Yin ZD. Epidemiological characteristics of meningococcal meningitis and switching trend of serogroups of Neisseria meningitidis in China, 2006–2014. Chin J Vaccines Immun. 2015;21(05):481–5.
Li JH, Li YX, Shao ZJ, Zhou HJ, Ning GJ, Yin ZD, Luo HM, Liang XF. Surveillance of meningococcal disease in China, 2009. Dis Surveil. 2010;25(10):770-773+780.
Jaca A, Wiyeh AB, Sambala EZ, Wiysonge CS. The burden of meningococcal meningitis in the African Meningitis Belt, from 2009 to 2014: a trend analysis. Pan Afr Med J. 2021;39:57. https://doi.org/10.11604/pamj.2021.39.57.17629.
Trotter CL, Maiden MCJ. Meningococcal vaccines and herd immunity: lessons learned from serogroup C conjugate vaccination programs. Expert Rev Vaccines. 2009;8(7):851–61. https://doi.org/10.1586/Erv.09.48.
Chinese PMA. Experts’ consensus on immunization with meningococcal vaccines in China. Chin J Vaccines Immun. 2019;25(01):96–101.
Purmohamad A, Abasi E, Azimi T, Hosseini S, Safari H, Nasiri MJ, Imani Fooladi AA. Global estimate of Neisseria meningitidis serogroups proportion in invasive meningococcal disease: a systematic review and meta-analysis. Microb Pathog. 2019;134: 103571. https://doi.org/10.1016/j.micpath.2019.103571.
Peterson ME, Li Y, Bita A, Moureau A, Nair H, Kyaw MH, Meningococcal Surveillance G, Abad R, Bailey F, Garcia IF, et al. Meningococcal serogroups and surveillance: a systematic review and survey. J Glob Health. 2019;9(1): 010409. https://doi.org/10.7189/jogh.09.010409.
Acknowledgements
Not applicable.
Funding
This study was funded by the Sanming Project of Medicine in Shenzhen (SZSM201803081) and Beijing Municipal Natural Science Foundation (L212011), including all costs associated with the development and publishing of the manuscript.
Author information
Authors and Affiliations
Contributions
YMM and XJ are joint first authors. YMM: studies screening and selection, data collection, data analysis and interpretation, manuscript writing. XJ: studies screening and selection, data collection. YJX: the conception and design of the study, search strategy making. SZJ: revision of the article, final approval of submitted version, guarantor of the study. All authors critically revised the article, read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declares that there is no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
PRISMA checklist. Fig S1. Quality assessment of the included studies. Fig S2. Forest plot of sensitivity analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yue, M., Xu, J., Yu, J. et al. Carriage prevalence of Neisseria meningitidis in China, 2005–2022: a systematic review and meta-analysis. BMC Infect Dis 22, 594 (2022). https://doi.org/10.1186/s12879-022-07586-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07586-x