Abstract
Background
There remain gaps in quantifying mortality risk among individuals co-infected with chronic hepatitis B (HBV) and human immunodeficiency virus (HIV) in sub-Saharan African contexts. Among a cohort of HIV-positive individuals in Rwanda, we estimate the difference in time-to mortality between HBV-positive (HIV/HBV co-infected) and HBV-negative (HIV mono-infected) individuals.
Methods
Using a dataset of HIV-infected adults screened for hepatitis B surface antigen (HBsAg) from January to June 2016 in Rwanda, we performed time-to-event analysis from the date of HBsAg results until death or end of study (31 December 2019). We used the Kaplan–Meier method to estimate probability of survival over time and Cox proportional hazard models to adjust for other factors associated with mortality.
Results
Of 21,105 available entries, 18,459 (87.5%) met the inclusion criteria. Mean age was 42.3 years (SD = 11.4) and 394 (2.1%) died during follow-up (mortality rate = 45.7 per 100,000 person-months, 95% confidence interval (CI) 41.4–50.4) Mortality rate ratio for co-infection was 1.7, 95% CI 1.1–2.6, however, Cox regression analysis did not show any association with mortality between compared groups. The adjusted analysis of covariates stratified by co-infection status showed that males, residing outside of the capital Kigali, drinking alcohol, WHO-HIV-clinical stage 3 and 4 were associated with increased mortality in this HIV cohort.
Conclusions
HBV infection does not significantly influence mortality among HIV-infected individuals in Rwanda. The current cohort is likely to have survived a period of high-risk exposure to HBV and HIV mortality and limited health care until their diagnosis.
Similar content being viewed by others
Background
Globally in 2020, 820,000 individuals died from chronic hepatitis B virus infection (HBV), compared to 680,000 people dying from HIV disease [1], and approximately 2.6 million HIV-infected individuals are co-infected with HBV [2]. Although HIV and HBV can share similar transmission routes [3], the contribution of transmission routes to infection burden may differ by geographical region [2]. For example, studies in East Africa have shown that scarification and blood transfusions are important risk factors for HBV transmission [4] and that HBV is often acquired at a younger age (before 5 years) compared to other regions in Africa. In contrast, HIV transmission in East Africa is driven by heterosexual sex in adulthood [2]. Low levels of HIV transmission among younger age groups can be explained by the recent introduction of antivirals in Africa [5] for prevention of mother-to-child transmission. The pathophysiology of HBV and the duration of the infection in East Africa, is an important factor to suspect a different risk of mortality that is assumed to be different of that in developed countries where, advanced health infrastructure for vaccination, screening and treatment make HBV acquisition in adulthood through sex and injecting drug use [6].
Several studies have found reduced survival [7,8,9,10] of HBV and HIV co-infected individuals, while other large studies [11,12,13] found no effect. These discrepancies, along with the potential lack of generalizability of previous studies for the eastern African population, raise reasonable question on the effect of HIV–HBV co-infection on mortality risk, warranting local-level investigation for more targeted policy guidance.
We conducted this study in Rwanda, an East African country where identification of people with HBV–HIV co-infection began in 2016 after a long period of uncertainty about co-infection and its impact on population mortality. Building on the previous work by Umutesi et al. (2021), we focus on HIV-infected people, and take into account the introduction of universal, early and immediate antiretroviral therapy (ART) [14] that raised ART coverage to 97.5% in Rwanda [15], and the prioritization of TDF as a first-line treatment [16]. There is little evidence of the effect of HBV on mortality in HIV-infected individuals, particularly in large cohorts with routine HIV care, routine free HIV/HBV testing, high antiretroviral treatment coverage and in the context of a differential HBV transmission route [2]. Using a large HIV-infected individual cohort in sub Saharan Africa, we examined the association between chronic HBV infection and HIV mortality among HIV-infected individuals.
Methods
Study design, population and settings
In this retrospective cohort study, we use data derived from a nationwide cohort of 117,258 HIV-infected adults (15 years and above) screened for hepatitis B surface antigens (HBsAg) during a vaccination and screening campaign in 2016 (the characteristics of this population is presented in Additional file 2: Appendix S2). The set-up, process and other details of this campaign have been described by Umutesi et al. [17]. In addition, a national electronic medical record (EMR) registry was used to supplement individual clinical, immunological and treatment data. The information on the Rwanda EMR has been published in earlier studies [18, 19]. The study period was from 1 January 2016 to 31 December 2019, included 21,105 records from populations with available HBV test results available between January and February 2016, and have been registered in one of the 340 HIV clinics with an EMR system in 2016.
Data processing and data collection
Data were collected using a predefined list of variables. This was developed and approved by the study committee after consultation of the literature on factors affecting survival of HIV-infected individuals. The unique patient identifier in the HBV vaccination and screening database and in the national EMR database for HIV-infected patients were matched, as the EMR did not contain HBV results. The HBV vaccination and screening database showed that as of 31 January 2016, HBV results were available for 59 health facilities and only 40 sites had EMR backups. To include all provinces, urban and rural district hospitals and health centers, we extended the period to 29 February 2016, and 62 of the 71 facilities including six district hospitals and 56 health centers were included and were visited to manually complete missing data, which resulted in 21,105 records for analysis. We considered these data sufficient to cover residence and geographic characteristics. Health care personnel involved in recording patient data received constant supervision and mentoring to ensure high quality data. In addition, data found to be incomplete or inconsistent were cross-checked on-site with patient files and patient registers. The principles of data protection and good scientific practice were strictly followed, both in Rwanda and in Germany, where the analysis was conducted and ethics committees in both countries approved the study (No. 958/RNEC/2019 and Nr.8604_BO_K_2019).
Measurement and outcome definitions
We assessed all-cause mortality, defined as death from any cause during the study period, as medically recorded in the EMR. The follow-up period was disaggregated into months from 1 January 2016 to 31 December 2019. Two groups were compared: HBsAg-positive participants, defined as co-infected with HBV and HIV, and HBsAg-negative participants, defined as HIV mono-infected individuals. Independent variables included age, disaggregated into four groups: 15–34, 35–54, 55–64 and 65+, sex categorized as less than and more than 7 years. Province of residence, TDF or non-TDF-based regimen defined as the last registered antiretroviral treatment containing TDF or not otherwise, HIV clinical staging according to WHO guidelines [20]. Diabetes, history of tuberculosis, duration of HIV treatment and time since HIV testing which were classified into two categories: less than 7 years and 7 years and over. Adherence to treatment measured as good when recorded as 95% and above and low when recorded as below 95% [21]. Biological factors, such as CD4 cell count at HBsAg testing binarized into low when below 350 cells/mm3 and high when 350 cells/mm3. HIV viral load (VL) at HBsAg testing considered to be undetectable when below 1000 copies/ml and detectable when above 1000 copies/ml [22]. Socio-behavioral factors, such as smoking history and alcohol use, were also assessed as binary yes/no information.
Statistical analysis
For each variable analyzed, we computed the prevalence of HBsAg and the mortality rate. Each participant was followed from the date of HBsAg test result and censored at death or at administrative censoring on December 31, 2019. Missing variables (> 5%) were not analyzed unless the variable is considered an important factor of mortality in HIV infected individuals. Data on transfer-out and lost to follow-up were considered as incomplete as there was no further information provided and were removed from the main analysis. However, we described them separately by co-infection category for different covariates to assess whether they might have had any impact on our results, and the results have been presented in Additional file 3: Appendix S3. In addition, individuals with no HBsAg results and individuals with positive hepatitis C virus (HCV) antibody results were removed to avoid confounding and because chronic HCV infections could not be determined. We calculated mortality rates by dividing the number of deaths by the person-months of follow-up and survival time (in months) by subtracting the date of HBsAg testing results from the date of death for both co-infected and mono-infected individuals. We used a non-parametric Kaplan–Meier survival modeling [23] to visualize overall survival experience of the entire cohort, stratified by chronic HBV co-infection status, and then by selected covariates known to be associated with mortality. In addition to visualization, we tested the difference between the survival curves by comparing the survival probability of the covariates using the log-rank test (given an equal chance at each time point). We used the Cox proportional hazards model to estimate multivariable adjusted hazard ratios (or ratios of mortality rates between study groups) and their 95% confidence intervals (CIs). To allow a flexible and a wide effect model, during variable selection for model inclusion, we considered variables that had a p-value of 0.10 and below in unadjusted regression models and all possible interactions. Modeling was performed using stepwise backwards deletion, assessing the magnitude of change in effect of the covariates for variable retention. Adjustments were made for sex, age, province of residence, smoking habit, alcohol use, CD4 cells levels, HIV VL copies, TDF based regimen, ART adherence, WHO clinical staging of HIV/AIDS, tuberculosis, time from HIV testing and time from ART initiation. The proportional hazard assumption of the risk function was tested using the Schoenfeld test [24]. We presented unadjusted and adjusted hazard ratios and their 95% CIs and assessed the statistical significance with a two-sided alpha of 0.05.
Results
Flow diagram of the study participants
Figure 1 shows that of a total of 117,258 HIV-infected individuals who participated in the 2017 vaccination and screening campaign, 21,105 from 62 health facilities met the study criteria and were therefore included in the study, with the details of their selection explained earlier in “Methods” section.
Characteristics of study participants
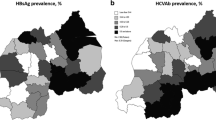
The study population were followed from the date of HBsAg results to death or end of the study period. Table 1 presents the characteristics of the study population using median and interquartile range (IQR) or mean and standard deviation (SD) for continuous covariates, or as frequencies and percentages for categorical data and differences in distribution among co-infected and mono-infected were assessed using the Pearson Chi-square test [25]. The study population had a mean age of 42.3 years (SD 11.4) and 65.1% were women. The prevalence of HBV infection by groups is shown in Additional file 1: Appendix S1.
Mortality rates by characteristics of the study population
The overall mortality rate was 45.7 per 100,000 person-months, with co-infected individuals, men and the oldest age group of 65 years and above experiencing a higher mortality rate as presented in Table 2.
Survival experience of participants according to hepatitis B co-infection
The Kaplan Meier curve (Fig. 2) shows the estimated survival probabilities by infection category during the follow-up period predominated by co-infected individuals.
Using log-rank test, crude analysis shows a statistically significant difference in the probability of survival between HIV mono-infected individuals and HIV/HBV co-infected individuals (p = 0.0117) as shown in Fig. 2.
Multiple Cox regression analysis
The median time to mortality was 47.4 months (range 1.5–47.7 months). Table 3 shows the results of the univariate and multiple survival model. Crude analysis shows a statistically significant association of co-infection and time to mortality. All covariates included in the analysis-co-infection status, sex, age, residence, alcohol use, WHO-HIV stages, years since initiation of ART, smoking, history of tuberculosis, and TDF use-were statistically significant, except for TDF use, and were included in the Cox regression model. However, the adjusted analysis failed to identify an association with time to mortality between co-infected and mono-infected groups: adjusted hazard ratio (aHR) of 0.84 and a 95% CI of 0.52–1.36. Multiple Cox regression analysis of covariates stratified by co-infection status shows that among 18,216 (94.9%) observations retained for multiple Cox regression analysis, sex, and age, province of residence, drinking alcohol, WHO clinical staging of HIV/AIDS and time from ART initiation were predictive mortality in both crude and adjusted analysis. For example, compared to females, and holding other covariates constant, males had a 1.39 times higher aHR and the difference was statistically significant. Compared to people residing in the capital city, Kigali, those residing in the northern, southern and western province had a higher aHR. Our results show that individuals who initiated ART at least 7 years prior to their HBV diagnosis had lower mortality compared to those on ART for lesser than 7 years, Table 3.
Discussion
Our results show that chronic HBV co-infection is not associated with time to mortality in HIV-infected individuals in Rwanda. We consider the following are reasons for minimal effect of HBV–HIV co-infection on increased mortality. First, by the end of 2007, about 10 years before participants in the current study could be tested for HBV, 80% of eligible HIV-positive Rwandans were on ART [26] a primary reason for a possible reduction in overall HIV-related mortality in Rwanda. We further note that 17,947/18,459 (97.2%) of our study population were on highly active antiretroviral therapy (HAART), and of these 13,339 (72.3%) were on a TDF-based regimen. In fact, TDF has been used in first-line ART in Rwanda since 2009 and various research studies have shown that it reduces HBV replication [27], thereby improving HIV outcomes, including mortality. Second, 100% of our population was on Lamividine (also known as 3TC, Epivir), another drug that reduces HBV replication [28]. Third, we consider our study population to be individuals who have succeeded or survived a past where the risk of infection and mortality was higher due to poor health infrastructure and insufficient knowledge of HIV and HBV in the population. In fact, African populations have carried a huge proportion of HBV infection for decades [29] and it is therefore indisputable that chronic HBV is a major risk factor for mortality in untreated individuals [30], and anti-HBV drugs have recently been introduced in African countries [31]. Consultation with traditional healers in the past is another reason that may increase the progression of the disease and the many deaths of HBV chronically infected individuals. Fourth, we suspect differences in mortality can be observed over longer periods of follow-up beyond the follow-up time after HBV diagnosis allowed by our study. Finally, our population displayed good clinical control of HIV infection as measured by CD4 cell counts, HIV RNA load, adherence to antiretroviral therapy, comorbidities including TB and WHO-HIV clinical stage. Nevertheless, a meta-analysis of studies conducted before the introduction of HAART found an increase in mortality among HBV–HIV co-infected individuals compared to mono-infected individuals [7]. However, all studies included in the review were from developed countries in Europe and the United States, and no studies were conducted in Africa. In contrast, a cohort study of HIV-infected persons enrolled between 1984 and 2003 in Greece found no impact of HBV co-infection on all-cause mortality. In another recent study conducted by Thornton [10], an increase in all-cause mortality following HBV and HIV co-infection was found in England. Higher mortality among co-infected individuals in developed countries may not translate to higher mortality in developing countries since the demographic distribution of co-infected individuals and access to prevention and treatment services between the two contexts is importantly different. For example, co-infected individuals from developed countries are more likely to be intravenous drug users and men who have sex with men, with potential differences in adherence to treatment contributing to higher mortality [10].
Although the prevalence of HBV/HIV co-infection is estimated to be over 28.4% in some African countries [32], a number of mortality studies have been conducted on specific populations. For example, a clinical trial conducted in Côte d’Ivoire by Kouamé in 2021 focused on people with low CD4 cell counts and found a higher impact of HIV and HBV co-infection on mortality [9]. However, in countries or regions where HAART is universal, this risk could be reduced, as in the case of an HIV clinic in Nigeria in 2014, where the study occurred before the implementation of TDF and HAART was a protective factor against mortality risk [12]. In the same vein, in countries where HAART was introduced in 1990s, such as in Europe [33], the effect of chronic HBV on liver-related mortality has been demonstrated but without any impact on progression to AIDS, immunological or virological response to HAART [34]. These scenarios could apply to Rwanda where, in 2020, 97.5% of HIV-infected persons were on HAART [15].
Independently to HBV co-infection status, our study showed that other factors increased the risk of mortality in HIV-infected persons, including being male. However, this finding is not consistently described in the literature where some have described a higher risk of mortality in women [35] while others a higher mortality risk among men [36, 37]. The increased case mortality risk in HIV-infected men may be related to a later diagnosis [38], later clinic attendance or lack of adherence to ART, as has been shown to be common among men in sub-Saharan Africa [39]. Age over 55 years versus 15–24 years and WHO-HIV stages 3 and 4 were predictive of mortality, which may be related to long-term HIV infection with more severe signs and symptoms or other comorbidities that, in turn, tend to increase with age [40]. The province of residence was also associated with the time to mortality, where residing in southern, northern and western province as compared to capital Kigali were highly associated with time to mortality. Previous studies have shown a higher risk of infection in provinces bordering neighboring countries [41] and a higher case fatality rate is likely. Other reasons could be related to health services centralized in Kigali and the increased likelihood of consulting traditional healers in certain peripheral regions of the county. Another predictor of mortality was alcohol consumption and its increased effect on liver disease was demonstrated [42, 43]. Finally, one co-variate, time since starting treatment, showed that taking ART for at least 7 years was associated with a lower risk of mortality, suggesting the effectiveness of ART [44].
Limitations of our study include a relatively short follow-up period that does not allow detection of a difference in mortality between the co-infected groups, because the development of cirrhosis and hepatocellular carcinoma (HCC) is too slow in patients on TDF [45]. Also the lack of quantification of the risk of HCCand liver-related mortality. As the data could not allow us to follow the study participants from the age of onset of HBV infection and that the immortal time bias is possible, we recommend further analysis to interpret the hazard ratio by age of acquisition of infection. We believe that prolonged duration between infection and diagnosis, an artefact of lack of prior health infrastructure, meaning a substantial proportion of this population died prior to the time diagnosis was offered and could not be included in our study. It is therefore unlikely that our results show a lethal effect of hepatitis B in the study population. We recognize the limitation of not being able to assess the actual survival time of those lost to follow-up, and lack of information on the completeness of EMR mortality data and other supporting sources, which may lead to reporting bias and thus conservative interpretation of the results of this study. Finally, considering that HBV viral load activity at the start of ART may also influence the difference in mortality [46, 47], we acknowledge that the lack of HBV DNA testing may limit our results.
Data availability
The data used during this study are not publicly available due to data protection regulation in Rwanda and Germany. However, upon reasonable request, the data can be obtained from the corresponding author: Justine.umutesi@helmholtz-hzi.de.
References
World Health Organization. Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021. Geneva: WHO Press; 2021.
Kourtis AP, et al. HIV-HBV coinfection-a global challenge. N Engl J Med. 2012;1:1–5.
World Health Organization. HIV and hepatitis B co-infection. Geneva: World Health Organization; 2009. p. 1–43.
Kafeero HM, Ndagire D, Ocama P, Kudamba A, Walusansa A, Sendagire H. Prevalence and predictors of hepatitis B virus (HBV) infection in east Africa: evidence from a systematic review and meta-analysis of epidemiological studies published from 2005 to 2020. Arch Public Health. 2021;79(1):1–19.
UNAIDS. Start free stay free AIDS free—2017 progress report. 2017;84. https://www.unaids.org/sites/default/files/media_asset/JC2923_SFSFAF_2017progressreport_en.pdf. Accessed 6 Nov 2020.
MacLachlan JH, Cowie BC. Hepatitis B virus epidemiology. Cold Spring Harb Perspect Med. 2015;5(5):1–12.
Nikolopoulos GK, Paraskevis D, Hatzitheodorou E, Moschidis Z, Sypsa V, Zavitsanos X, et al. Impact of hepatitis B virus infection on the progression of AIDS and mortality in HIV-infected individuals: a cohort study and meta-analysis. Clin Infect Dis. 2009;48(12):1763–71.
McGovern BH. The epidemiology, natural history and prevention of hepatitis B: implications of HIV coinfection. Antivir Ther. 2007;12(Suppl 3):H3-13.
Kouamé GM, Gabillard D, Moh R, Badje A, Ntakpé JB, Emième A, et al. Higher risk of mortality in HIV-HBV co-infected patients from sub-Saharan Africa is observed at lower CD4+ cell counts. Antivir Ther. 2021;26:25–33.
Thornton AC, Jose S, Bhagani S, Chadwick D, Dunn D, Gilson R, et al. Hepatitis B, hepatitis C, and mortality among HIV-positive individuals. AIDS. 2017;31(18):2525–32.
Zhang F, Zhu H, Wu Y, Dou Z, Zhang Y, Kleinman N, et al. HIV, hepatitis B virus, and hepatitis C virus co-infection in patients in the China National Free Antiretroviral Treatment Program, 2010–12: a retrospective observational cohort study. HHS Public Access. 2018;14(11):1065–72.
Ladep NG. Hepatitis B co-infection is associated with poorer survival of HIV-infected patients on highly active antiretroviral therapy in West Africa. J AIDS Clin Res. 2013. https://doi.org/10.4172/2155-6113.S3-006.
Chen M, Wong WW, Law MG, Kiertiburanakul S, Yunihastuti E, Merati TP, et al. Hepatitis B and C co-infection in HIV patients from the TREAT Asia HIV observational database: analysis of risk factors and survival. PLoS ONE. 2016;11(3):1–17.
Nsanzimana S, Remera E, Ribakare M, Burns T, Dludlu S, Mills EJ, et al. Phased implementation of spaced clinic visits for stable HIV-positive patients in Rwanda to support Treat All. J Int AIDS Soc. 2017;20:20–7. https://doi.org/10.7448/IAS.20.1.21635.
RBC. Rwanda population-based HIV impact assessment RPHIA 2018–2019. 2019.
Rwanda M of health. National guidelines for prevention and management of HIV and STIs edition 2016. 2016.
Umutesi J, Simmons B, Makuza JD, Dushimiyimana D, Mbituyumuremyi A, Uwimana JM, et al. Prevalence of hepatitis B and C infection in persons living with HIV enrolled in care in Rwanda. BMC Infect Dis. 2017;17(1):1–7.
Nsanzimana S, Semakula M, Ndahindwa V, Remera E, Sebuhoro D, Uwizihiwe JP, et al. Retention in care and virological failure among adult HIV + patients on second-line ART in Rwanda : a national representative study. BMC Infect Dis. 2019;2:1–9.
Amoroso CL, Akimana B, Wise B, Sf H. Using electronic medical records for HIV care in rural Rwanda. In: Medinfo. 2010;337–41.
World Health Organization (WHO). Interim WHO clinical staging of HIV/AIDS and HIV/AIDS case definitions for surveillance, African region. Geneva: World Health Organization; 2005. p. 513–4.
Chalker J, Andualem T, Tadeg H, Gitau L, Ntaganira J, Obua C, et al. Developing standard methods to monitor adherence to antiretroviral medicines and treatment defaulting in resource-poor settings. Essent Med Monit. 2019;1:4–8.
WHO. What’s new in treatment monitoring: viral load and CD4 testing. HIV Treat care. 2017;(update):8624–8.
Kleinbaum DG, Klein M. Statistics for biology and health. In: Survival analysis, a self-learning text. 3rd edition. Media. 2010.
Sooriyarachchi WWMA, Sooriyarachchi MR, Abeysekera. Use of Schoenfeld’s global test to test the proportional hazards assumption in the Cox proportiona. J Nat Sci Found. 2009;37(1).
Wooldridge JM. Introductory econometrics: a modern approach. 5th ed. Boston: Cengage Learning; 2012. p. 127–8.
Nsanzimana S, Kanters S, Remera E, Forrest JI, Binagwaho A, Condo J, et al. HIV care continuum in Rwanda: a cross-sectional analysis of the national programme. Lancet HIV. 2015;2(5):e208–15. https://doi.org/10.1016/S2352-3018(15)00024-7.
Huang AJ, Núñez M. Outcomes in HIV/HBV-coinfected patients in the tenofovir era are greatly affected by immune suppression. J Int Assoc Provid AIDS Care. 2015;14(4):360–8.
Dore GJ, Cooper DA, Barrett C, Goh LE, Thakrar B, Atkins M. Dual efficacy of lamivudine treatment in human immunodeficiency virus/hepatitis B virus-coinfected persons in a randomized, controlled study (CAESAR). J Infect Dis. 1999;180(3):607–13.
Zampino R, Boemio A, Sagnelli C, Alessio L, Adinolfi LE, Sagnelli E, et al. Hepatitis B virus burden in developing countries. World J Gastroenterol. 2015;21(42):11941–53.
Lee HW, Kim SU, Park JY, Baatarkhuu O, Kim DY, Ahn SH, et al. Prognosis of untreated minimally active chronic hepatitis B patients in comparison with virological responders by antivirals. Clin Transl Gastroenterol. 2019;10(6):1–6.
Desalegn H, Aberra H, Berhe N, Mekasha B, Stene-Johansen K, Krarup H, et al. Treatment of chronic hepatitis B in sub-Saharan Africa: 1-year results of a pilot program in Ethiopia. BMC Med. 2018;16(1):1–10.
Stabinski L, O’Connor S, Barnhart M, Kahn RJ, Hamm TE. Prevalence of HIV and hepatitis B virus co-infection in Sub-Saharan Africa and the potential impact and program feasibility of Hepatitis B surface antigen screening in resource-limited settings. J Acquir Immune Defic Syndr. 2015;68:S274–85.
World Health Organization. HIV/AIDS in Europe. Moving from death sentence to chronic disease management. Geneva: WHO; 2006. p. 188.
Konopnicki D, Mocroft A, De Wit S, Antunes F, Ledergerber B, Katlama C, et al. Hepatitis B and HIV: prevalence, AIDS progression, response to highly active antiretroviral therapy and increased mortality in the EuroSIDA cohort. AIDS. 2005;19(6):593–601.
Burchell AN, Raboud J, Donelle J, Loutfy MR, Rourke SB, Rogers T, et al. Cause-specific mortality among HIV-infected people in Ontario, 1995–2014: a population-based retrospective cohort study. CMAJ Open. 2019;7(1):E1-7.
Kerkhoff AD, Sikombe K, Eshun-Wilson I, Sikazwe I, Glidden DV, Pry JM, et al. Mortality estimates by age and sex among persons living with HIV after ART initiation in Zambia using electronic medical records supplemented with tracing a sample of lost patients: a cohort study. PLoS Med. 2020;17(5):1–21. https://doi.org/10.1371/journal.pmed.1003107.
Druyts E, Dybul M, Kanters S, Nachega J, Birungi J, Ford N, et al. Male sex and the risk of mortality among individuals enrolled in antiretroviral therapy programs in Africa: a systematic review and meta-analysis. AIDS. 2013;27(3):417–25.
Tang H, Mao Y, Tang W, Han J, Xu J, Li J. “Late for testing, early for antiretroviral therapy, less likely to die”: results from a large HIV cohort study in China, 2006–2014. BMC Infect Dis. 2018;18(1):1–13.
Mills EJ, Beyrer C, Birungi J, Dybul MR. Engaging men in prevention and care for HIV/AIDS in Africa. PLoS Med. 2012;9(2):1–4.
Konrad BP, DarleneTaylor JM, et al. Age-specific mortality patterns in HIV-infected individuals: a comparative analysis of African community study data. AIDS. 2007;21(SUPPL. 6):87–96.
Umutesi J, Klett-Tammen C, Nsanzimana S, Krause G, Ott JJ. Cross-sectional study of chronic hepatitis B virus infection in Rwandan high-risk groups: unexpected findings on prevalence and its determinants. BMJ Open. 2021;11(12):e054039.
Sorenson SB. Gender disparities in injury mortality: consistent, persistent, and larger than you’d think. Am J Public Health. 2011;101(SUPPL. 1):353–8.
Xi B, Veeranki SP, Zhao M, Ma C, Yan Y, Mi J. Relationship of alcohol consumption to all-cause, cardiovascular, and cancer-related mortality in U.S. adults. J Am Coll Cardiol. 2017;70(8):913–22.
Nsanzimana S, Remera E, Kanters S, Chan K, Forrest JI, Ford N, et al. Life expectancy among HIV-positive patients in Rwanda: a retrospective observational cohort study. Lancet Glob Health. 2015;3(3):e169–77.
Zhang P, Liu Q, Yuan M, Wang L. Tenofovir disoproxil fumarate reduce incidence of HCC development in CHB-patients with compensated cirrhosis. Infect Agent Cancer. 2018;13(1):1–5.
Kouame GM, Boyd A, Moh R, Badje A, Gabillard D, Ouattara E, et al. Higher mortality despite early antiretroviral therapy in human immunodeficiency virus and hepatitis B virus (HBV)-coinfected patients with high HBV replication. Clin Infect Dis. 2018;66(1):112–20.
Velen K, Charalambous S, Innes C. Chronic hepatitis B increases mortality and complexity among HIV-co-infected patients in South Africa: a cohort study. HIV Med. 2019;17(9):702–7.
Acknowledgements
We thank Mr. Eric Remera for data collection and anonymization and Dr. Michael Penkunas for linguistic verification of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. There was no specific funding for the conduct of this work. However, the DAAD under Rwandan—German Ph.D. Programme offered a study scholarship to the first author of this study, and the RBC provided the study data.
Author information
Authors and Affiliations
Contributions
JU, GK, and JJO initiated the project and elaborated the project protocol, including study variables and ethics-related approvals. JU wrote the manuscript, managed and analyzed the data. PV contributed to the improvement of the draft with a focus on the statistical part. CYL carefully reviewed the document. SN helped obtain the data used and ethical clearance in Rwanda and revised the manuscript with a focus on local parameters. All authors actively contributed to the writing, proofreading. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participants
This study was conducted in accordance with the Declaration of Helsinki, with the utmost respect for the study participants. Prior to data collection during the screening campaign, oral consent was sought from participants and the Rwandan National Ethics Committee approved the waiver for written informed consent. In addition, we obtained the data anonymously to ensure that no participant would be harmed by not being contacted directly, all information about individual persons was removed, with a high degree of assurance that individual information would not be linked. Before the analysis, the following institutions have approved the study: (1) Rwanda National Council for Science and Technology (No 139/NCST.2019), Rwanda, (2) Rwanda National Ethics Committee (No. 958/RNEC/2019), Rwanda (3) Ethical commission at Hannover Medical School (Nr.8604_BO_K_2019), Germany.
Consent to publication
Not applicable.
Competing interests
There is no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix S1.
HBsAg prevalence by characteristics of the study population.
Additional file 2: Appendix S2.
Comparing characteristics of all HIV infected screened in 2016 and the current study population.
Additional file 3: Appendix S3.
Characteristics of individuals lost to follow up by co-infection categories.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Umutesi, J., Nsanzimana, S., Yingkai Liu, C. et al. Long-term effect of chronic hepatitis B on mortality in HIV-infected persons in a differential HBV transmission setting. BMC Infect Dis 22, 500 (2022). https://doi.org/10.1186/s12879-022-07477-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07477-1