Abstract
Background
In older adult patients, bloodstream infections cause significant mortality. However, data on long-term prognosis in very elderly patients are scarce. This study aims to assess 1-year mortality from bacteraemia in very elderly patients.
Methods
Retrospective cohort study in inpatients aged 80 years or older and suspected of having sepsis. Patients with (n = 336) and without (n = 336) confirmed bacteraemia were matched for age, sex, and date of culture, and their characteristics were compared. All-cause mortality and risk of death were assessed using the adjusted hazard ratio (aHR).
Results
Compared to controls, cases showed a higher 1-year mortality (34.8% vs. 45.2%) and mortality rate (0.46 vs. 0.69 deaths per person-year). Multivariable analysis showed significant risk of 1-year mortality in patients with bacteraemia (aHR: 1.31, 95% confidence interval [CI] 1.03–1.67), quick Sepsis Related Organ Failure Assessment (qSOFA) score of 2 or more (aHR: 2.71, 95% CI 2.05–3.57), and age of 90 years or older (aHR 1.53, 95% CI 1.17–1.99).
Conclusions
In elderly patients suspected of sepsis, bacteraemia is associated with a poor prognosis and higher long-term mortality. Other factors related to excess mortality were age over 90 years and a qSOFA score of 2 or more.
Similar content being viewed by others
Background
Bacteraemia is a major cause of mortality in high-income countries, despite advances in therapeutic strategies. Furthermore, its incidence is increasing with the proportion of very elderly people in the population [1,2,3], in whom infectious disease outcomes also tend to be more severe. This is due to multiple factors, including increased comorbidities and decreased functional reserve, with patients over the age of 80 years being the most likely to develop organ dysfunction [4,5,6].
Identifying mortality predictors in elderly patients with bacteraemia is especially important for their follow-up. Although predictors of short-term excess mortality are relatively well established, few studies provide information regarding long-term survival [7,8,9]. Moreover, patient-related factors, such as the level of organ dysfunction, could impact survival even more than bacteraemia, confounding results in survival studies in this population. The quick Sequential Organ Failure Assessment (qSOFA) has been useful in detecting suspected cases of sepsis associated with higher mortality, especially in elderly patients [10,11,12]; however, its behaviour as a long-term prognostic marker is not well known.
This study aims to compare 1-year mortality in hospitalised patients older than 80 years with and without bacteraemia and to evaluate its association with qSOFA and other clinical and laboratory data that could act as confounders.
Methods
Study setting
The study involved 672 patients admitted to the General University Hospital of Alicante (Spain), an acute care centre with 750 beds that cares for a population of 265,000 inhabitants. This is an observational study of paired retrospective cohorts (1:1), in which we reviewed the results of blood cultures performed on patients older than 80 years admitted to any hospital service between January 2016 and December 2017. The sample size necessary to obtain an adjusted hazard ratio (HR) different from 1 with respect to mortality between positive and negative blood culture was calculated. To do this, a pilot study was conducted with 20 people with a negative culture and 20 others with a positive culture, in which an HR of 1.3 and a mortality rate of 68% were obtained. With these values, setting the type I error at 5%, the type II error at 20%, and the exposure ratio at 1:1, at least 671 patients were needed.
Study cohort
Patients who met at least two of the Systemic Inflammatory Response Syndrome (SIRS) criteria (fever > 38.0 °C or hypothermia < 36.0 °C, tachycardia > 90 beats/minute, tachypnea > 20 breaths/minute, leukocytosis [leukocytes > 12 × 109/l] or leucopenia [< 4 × 109/l]) were suspected of sepsis. At times, antibiotics were prescribed before blood culture. Blood cultures were obtained, processed, and interpreted according to the recommendations of the Spanish Society of Infectious Diseases and Clinical Microbiology (SIDCM—SEIMC) [13]. At least two bottles of haemoculture were obtained for patients (Becton Dickinson BACTEC FX blood culture system). Bacteraemia was defined as the isolation of pathogenic bacteria in the blood culture. The pathogen was identified by both traditional microbiological techniques (Gram culture and antibiogram by microdilution; Walk Away, Beckman, USA) and new techniques (MALDI-TOF; Bruker, Germany) from a blood culture. Potentially contaminating microorganisms, such as coagulase negative staphylococci, Streptococcus from the viridans group, Propionibacterium acnes or Clostridium perfringens, were included only when they were detected in at least two blood cultures [13].
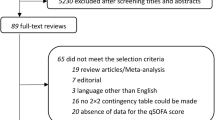
The cohort of patients with bacteraemia has been described previously [14]. Briefly, the exposed cohort was selected retrospectively from a database provided by the Microbiology Service at the General University Hospital of Alicante, which contained the 5792 blood cultures carried out between 2016 and 2017 in patients over 80 years of age. Patients with both community-acquired and nosocomial bacteraemia were included, while those with previous bacteraemia or unavailable clinical histories, along with cultures showing microorganisms considered to be contaminants, were excluded. In the end, 336 patients with a positive blood culture were randomly selected (Fig. 1).
All controls were selected from the same database as the cases, and they were matched for sex, age, date of blood culture, and origin of infection. If there were no equivalent controls according to these characteristics, those of the same gender and of the closest age were chosen. Controls that developed a subsequent episode of bacteraemia were included, while those with at least one previous episode were excluded. Until all the cases and controls were selected, it was unknown whether they had died at the time of the study. No data are available on how many of them had a diagnosis of infection at discharge.
Data source
Data were collected using the unique patient identifier assigned by the Valencian Health Agency to all residents of the Valencian Community. Clinical, laboratory, and epidemiological data were obtained from each patient’s electronic health record (EHR) using the Orion Clinic v11.0 computer programme (Valencian Health Agency, Spain). The Population Information System (Generalitat Valenciana, Spain) was used to collect the date of death from any cause as well as the date of loss to follow-up. Data were stored in a Microsoft Excel v16.0 spreadsheet (Microsoft, USA).
Variables and definitions
We collected variables registered in the EHR on the day of the blood culture. The main variable of the study was the time to event, where the event was death from any cause. Patients were classified according to their age (80–89 years vs. ≥ 90 years). Dichotomous variables for systolic blood pressure, respiratory rate, and level of consciousness were created to match the criteria of the qSOFA scale [11]: hypotension, systolic blood pressure ≤ 100 mmHg; tachypnoea, ≥ to 22 breaths per minute; and low level of consciousness, Glasgow Coma Scale < 15. Patients who met two or more qSOFA criteria were considered at high risk of organ failure. Kidney injury (KI) was defined as an estimated glomerular filtration rate (eGFR) less than 60 mL/min; hypernatremia, as a plasma sodium concentration greater than 145 mEq/L; and hyponatremia, as a concentration less than 135 mEq/L. The variables included in the study were renal function and natremia, since the relevant role of these variables as risk factors for mortality in patients with infections has been seen in other studies [15, 16]. Other variables such as lactate or albumin were not included since they are not routinely collected.
Survival was calculated from the date of the blood culture to the date of death from any cause, with a maximum follow-up time of 365 days. Using the same procedure, a 30-day survival study was also performed.
Statistical analysis
The Kaplan–Meier method was used to perform the survival analysis and generate a graphical representation of the survival curves. Cox regression was used for the univariable and multivariable analysis; results are expressed as HR and adjusted HR (aHR), with their 95% confidence intervals (CIs). In all tests, p values of less than 0.05 were considered significant. The software used for statistical analysis was SPSS for Windows, v22.0 (IBM, USA).
Ethics approval
The study was approved by the General University Hospital of Alicante Research Ethics Committee (CEIm PI2018/105). Analysis was performed on de-identified, aggregated patient level data, and no individual informed consent was obtained. The need for written informed consent was explicitly waived from the participants. Research was performed in accordance with the Helsinki Declaration.
Results
Sample description
Table 1 shows the characteristics of the sample. There were 370 women (65.1%); 516 (76.8%) were aged 80 to 89 years, while the other 156 (23.2%) were aged 90 years or more. The mean age was 86 years in patients both with and without bacteraemia. Hypotension was more frequent in cases compared to controls (24.3% vs. 16.1% p = 0.010), as was a qSOFA score of 2 or more (21.7% vs. 12.8% p = 0.003). KI was quite prevalent in both groups but more so in patients with (75%) vs. without (66.3%) bacteraemia (p=0.03). The most frequently isolated microorganism in patients with positive blood culture was Escherichia coli (43.2%), followed by Enterococcus spp. (12.4%) and Klebsiella spp. (10.4%). Regarding the source of bacteraemia, the urinary tract (44.3% of cases), lower respiratory tract (20.8%), and bile duct (9.3%) were the most frequent origins.
Mortality study
Table 2 shows 1-month and 1-year mortality. At 1 year, 269 of the 672 patients (40%) had died. In patients with bacteraemia, mortality was 45%, with an incidence rate of 0.69 deaths per person-year. In the case of patients with negative blood culture, it was 35% and the incidence rate was 0.46 per person-year. The observed mortality was also higher in patients aged over 90 years (51.3% vs. 36.6% p < 0.001), patients with a qSOFA ≥ 2 (68.1% vs. 34.2% p < 0.001), and with hypernatremia (56.7% vs. 38.4% p = 0.009).
One-year survival
The survival functions for both cohorts, obtained by the Kaplan–Meyer method, are represented in Fig. 2 (log-rank p = 0.004). Bacteraemia was significantly associated with mortality (HR = 1.42, log-rank p = 0.004) in the univariable analysis (see Table 3), as was age over 90 years (HR = 1.56, p = 0.001) and hypernatremia (HR = 1.94, p < 0.001). The association of the greatest magnitude was a qSOFA score of 2 or more (HR = 2.98, p < 0.001).
In the multivariable analysis, bacteraemia remained an independent risk factor for 1-year mortality (aHR 1.31, p = 0.029). Patients over the age of 90 years (aHR 1.53, p = 0.002) and with a qSOFA score ≥ 2 (aHR = 2.71 p < 0.001) also carried a higher risk. After adjusting the data for potential confounders, no statistically significant differences were found for hypernatremia. Figure 3 shows the survival curve in patients classified according to their qSOFA score.
Discussion
The results of the present study show how the alteration of certain variables is associated with a worse prognosis in elderly patients with suspected sepsis, although its impact on short- and long-term mortality differs. Specifically, we found that the risk of death in the first year in patients with a positive blood culture is 31% higher than those with a negative blood culture. Moreover, patients over the age of 90 have about 50% higher risk than those aged 80–89 years; and a qSOFA score of 2 or more was associated with a 171% increase in 1-year mortality.
Bacteraemia has a notable social and health impact due to its frequency and associated mortality, especially in the elderly population. Thus, the identification of prognostic factors when faced with clinical suspicion acquires special relevance in these patients. In this study, we hypothesised that a positive blood culture could have less prognostic impact than other variables such as age, clinical severity, or other laboratory findings. However, we found that bacteraemia is associated with a higher mortality in both the short and long term in very elderly patients. One-month mortality in patients with bacteraemia was 21.4%, a similar figure to that obtained in other studies, such as the one carried out by Søgaard et al. in 2008 [9]. To the best of our knowledge, ours is the first study comparing long-term mortality specifically in elderly patients using hospital controls; other authors, such as Nielsen et al. [17], reported similar mortality in this subgroup in 2015 (53% vs. 45% in this study), although with risk ratios that were 40 times higher (compared to our 31%) since they used healthy population controls.
Age has been widely described in the literature as a poor prognostic factor in patients with bacteraemia. Different authors have found 21–35% higher short- and long-term mortality in patients older than 80 years with respect to the rest of the geriatric population [5, 18,19,20], and Nielsen et al. [17] suggested that age may be a more important risk factor for mortality than bacteraemia itself, since the higher risks of mortality (compared to controls) were described in young patients without comorbidities. There are no studies comparing the risk in patients aged 80–89 years vs. 90 years or older, but our data show a 50% higher risk of death in the older group, both at 30 days and 1 year. This value is strikingly higher than the 35% described for those over 80 years of age, probably due to the greater number of comorbidities and higher rates of institutionalisation, as well as the lower functional reserve of the oldest patients [6].
The results suggest a higher frequency of qSOFA scores over 2 in patients with a positive blood culture, as well as a strong association with mortality, with a three-fold greater risk of death in the first month and a two-fold higher risk in the first year. Although our figures seem to indicate that qSOFA is the best predictor of mortality among the studied variables, literature on the prognostic validity of the scale is controversial. In this study, 30-day mortality was 45.7%, higher than in other studies in the elderly population, where figures ranged from 24 to 33%; In those studies, the qSOFA yielded a lower prognostic validity [12, 21, 22]. A recent systematic review [23] attributed the variability of results to the different populations studied and to differences in the interpretation of the scale’s variables, especially “altered mental state”. For this reason, a standardised definition is necessary for future studies, especially in patients with dementia and other underlying neurological disorders, very common in elderly patients.
Moreover, diagnosing bloodstream infections and sepsis in the elderly is challenging, as the expected clinical presentation of infections is often lacking or altered due to impaired ability to communicate, underlying conditions, and previous alterations in laboratory markers. Sometimes, doctors do not suspect sepsis until it is fully established.
Studies on the long-term prognosis following bacteraemia infection are scarce, and barely any data are available in elderly patients. This study provides useful information on the prognosis of bacteraemia in very elderly patients.
However, it has some limitations. First, its retrospective nature entails an inherent risk of selection or misclassification bias. Secondly, several variables were not considered, such as lactate, albumin, comorbidities, immunity status, prescribed antibiotic treatment, cause of death, or quality of life after bacteraemia. Third, the EHR had no information on frailty status, a physiological condition characterised by a decreased reserve to stressors [24]. Reliable, easy-to-use, and validated instruments are available, such as the Clinical Frailty Scale [25,26,27,28,29], and this scale has been shown to correlate with outcomes for several pathologies in multicentre studies [25,26,27,28,29]. Unfortunately, this variable was not available to us. Fourthly, delirium is associated with higher mortality, and it is one of the most consequential geriatric syndromes, especially in septic patients, but it was not considered in our study despite its potential influence on mortality. Fifthly, appropriate empirical antibiotic treatment and implementation of resuscitation bundles are a strategy for preventing mortality due to bloodstream infection, but in our study this was not recorded. Finally, it is an observational study from a single centre, which could limit the generalisability of our results.
Conclusions
Based on our data, bacteraemia is associated with a poor prognosis and higher long-term mortality in elderly (≥ 80 years) patients. This infection remains a serious and life-threatening clinical entity. In elderly patients, optimising long-term outcomes in survivors hinges on high suspicion, early diagnosis and treatment of bloodstream infections and sepsis, and awareness of the need for multidisciplinary care, preferably involving geriatricians.
Bacteraemia should not be considered a benign process, so it is necessary to adopt measures to prevent death in the near term as well as to minimise the functional damage that can condition mortality later on. Other factors related to excess mortality were age over 90 years and a qSOFA score of 2 or more. On these last two points, little information is available, so future studies are needed.
It is important to design a multicentre prospective study on sepsis in the elderly population, including an appropriate antibiotic and implementation of resuscitation bundles, but also to optimise care of these patients, addressing risk factors like delirium and providing the elderly with the best possible care to improve short- and long-term outcomes.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- CEIm:
-
General University Hospital of Alicante Research Ethics Committee
- SIDCM–SEIMC:
-
Spanish Society of Infectious Diseases and Clinical Microbiology
- eGFR:
-
Estimated glomerular filtration rate
- EHR:
-
Electronic health record
- HR:
-
Hazard ratio
- aHR:
-
Adjusted hazard ratio
- CI:
-
Confidence interval
- qSOFA:
-
Quick Sequential Organ Failure Assessment
- Brpm:
-
Breaths per minute
References
Girard TD, Ely EW. Bacteremia and sepsis in older adults. Clin Geriatr Med. 2007;23:633–47.
Goto M, Al-Hasan MN. Overall burden of bloodstream infection and nosocomial bloodstream infection in North America and Europe. Clin Microbiol Infect. 2013;19:501–9.
Søgaard M, Nørgaard M, Dethlefsen C, Schønheyder HC. Temporal changes in the incidence and 30-day mortality associated with bacteremia in hospitalized patients from 1992 through 2006: a population-based cohort study. Clin Infect Dis. 2011;52:61–9.
Lee CC, Chen SY, Chang IJ, Chen SC, Wu SC. Comparison of clinical manifestations and outcome of community-acquired bloodstream infections among the oldest old, elderly, and adult patients. Medicine (Baltimore). 2007;86:138–44.
Blot S, Cankurtaran M, Petrovic M, Vandijck D, Lizy C, Decruyenaere J, et al. Epidemiology and outcome of nosocomial bloodstream infection in elderly critically ill patients: a comparison between middle-aged, old, and very old patients. Crit Care Med. 2009;37:1634–41.
Bassetti M, Righi E, Del Giacomo P, Sartor A, Ansaldi F, Trucchi C, et al. Predictors of mortality with Staphylococcus aureus bacteremia in elderly adults. J Am Geriatr Soc. 2018;66:1284–9.
McNamara JF, Righi E, Wright H, Hartel GF, Harris PNA, Paterson DL. Long-term morbidity and mortality following bloodstream infection: a systematic literature review. J Infect. 2018;77:1–8.
Big C, Malani PN. Staphylococcus aureus bloodstream infections in older adults: clinical outcomes and risk factors for in-hospital mortality. J Am Geriatr Soc. 2010;58:300–5.
Søgaard M, Schønheyder HC, Riis A, Sørensen HT, Nørgaard M. Short-term mortality in relation to age and comorbidity in older adults with community-acquired bacteremia: a population-based cohort study. J Am Geriatr Soc. 2008;56:1593–600.
Minejima E, Delayo V, Lou M, Ny P, Nieberg P, She RC, Wong-Beringer A. Utility of qSOFA score in identifying patients at risk for poor outcome in Staphylococcus aureus bacteremia. BMC Infect Dis. 2019;19:149.
Burnham JP, Kollef MH. qSOFA score: predictive validity in Enterobacteriaceae bloodstream infections. J Crit Care. 2018;43:143–7.
Ramos JGR, da Hora PR, Teixeira MB, Gobatto ALN, Coutinho RVDS, et al. Prognostic ability of quick-SOFA across different age groups of patients with suspected infection outside the intensive care unit: a cohort study. J Crit Care. 2018;47:178–84.
Loza Fernández de Bobadilla E, Planes Reig A, Rodríguez Creixems M. Cercenado E, Cantón R. Procedimientos en Microbiología Clínica: Recomendaciones de la Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica. 2003. Available at: https://www.seimc.org/contenidos/documentoscientificos/procedimientosmicrobiologia/seimc-procedimientomicrobiologia3a.pdf.
Ramos-Rincón JM, Fernández-Gil A, Merino E, et al. The quick Sepsis-related Organ Failure Assessment (qSOFA) is a good predictor of in-hospital mortality in very elderly patients with bloodstream infections: a retrospective observational study. Sci Rep. 2019;9:15075.
Suh SH, Kim CS, Choi JS, Bae EH, Ma SK, Kim SW. Acute kidney injury in patients with sepsis and septic shock: risk factors and clinical outcomes. Yonsei Med J. 2013;54:965–72.
Tsipotis E, Price LL, Jaber BL, Madias NE. Hospital-associated hypernatremia spectrum and clinical outcomes in an unselected cohort. Am J Med. 2018;131:72–82.
Nielsen SL, Lassen AT, Gradel KO, Jensen TG, Kolmos HJ, Hallas J, Pedersen C. Bacteremia is associated with excess long-term mortality: a 12-year population-based cohort study. J Infect. 2015;70:111–26.
Rebelo M, Pereira B, Lima J, Decq-Mota J, Vieira JD, Costa JN. Predictors of in-hospital mortality in elderly patients with bacteraemia admitted to an Internal Medicine ward. Int Arch Med. 2011;4:33.
Artero A, Inglada L, Gómez-Belda A, Capdevila JA, Diez LF, Arca A, et al. The clinical impact of bacteremia on outcomes in elderly patients with pyelonephritis or urinary sepsis: a prospective multicenter study. PLoS One. 2018;13:e0191066.
Retamar P, López-Prieto MD, Rodríguez-López F, de Cueto M, García MV, González-Galan V, Del Arco A, SAEI/SAMPAC/REIPI Bacteremia Group. Predictors of early mortality in very elderly patients with bacteremia: a prospective multicenter cohort. Int J Infect Dis. 2014;26:83–7.
Yañez MC, Salido Mota M, Fuentes Ferrer M, Julián-Jiménez A, Piñera P, Llopis F, Gamazo Del Rio J, et al. Grupo de Infecciones de la Sociedad Española de Medicinade Urgencias y Emergencias (INFURG-SEMES) [Comparison of different strategiesfor short-term death prediction in the infected older patient]. Rev Esp Quimioter. 2019;32:156–64.
González Del Castillo J, Julian-Jiménez A, González Martínez F, Álvarez-Manzanares J, Piñera P, Navarro-Bustos C, et al. Infectious Disease Group of the Spanish Emergency Medicine Society Prognostic accuracy of SIRS criteria, qSOFA score and GYM score for 30-day-mortality in older non-severely dependent infected patients attended in the emergency department. Eur J Clin Microbiol Infect Dis. 2017;36:2361–9.
Lo RSL, Leung LY, Brabrand M, Yeung CY, Chan SY, Lam CCY, Hung KKC, Graham CA. qSOFA is a poor predictor of short-term mortality in all patients: a systematic review of 410,000 patients. J Clin Med. 2019;8:8.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–95.
Guidet B, de Lange DW, Boumendil A, Leaver S, Watson X, Boulanger C, VIP2 study group, et al. The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med. 2020;46:57–69.
Flaatten H, De Lange DW, Morandi A, Andersen FH, Artigas A, Bertolini G, VIP1 study group, et al. The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years). Intensive Care Med. 2017;43:1820–8.
Ibarz M, Boumendil A, Haas LEM, Irazabal M, Flaatten H, de Lange DW, VIP1 study, et al. Sepsis at ICU admission does not decrease 30-day survival in very old patients: a post-hoc analysis of the VIP1 multinational cohort study. Ann Intensive Care. 2020;10:56.
Flaatten H, Guidet B, Andersen FH, Artigas A, Cecconi M, Boumendil A, VIP2 study group, et al. Reliability of the clinical frailty scale in very elderly ICU patients: a prospective European study. Ann Intensive Care. 2021;11:22.
Haas LEM, Boumendil A, Flaatten H, Guidet B, Ibarz M, Jung C, VIP2 study group, et al. Frailty is associated with long-term outcome in patients with sepsis who are over 80 years old: results from an observational study in 241 European ICUs. Age Ageing. 2021;50:1719–27.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific Grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
RHQ carried out the data collection, performed the statistical analysis and drafted the manuscript. AFG helped to collect the data. JCRD and AG provided inpatient’s data from the microbiology service’s data base. VB, EM, RSM, BV and JMRR conceived the study and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Study was approved by the General University Hospital of Alicante Research Ethics Committee (CEIm PI2018 / 105). According to Spanish legislation (BOE-A-2020-14960) and European Legislation (REGULATION (EU) No 536/2014), informed consent is not necessary for this study. Given its observational design, the prerequisites are limited to the favourable opinion of the Research Ethics Committee of the health centre complying with the Personal Data Protection Law (BOE-A -2018-16673) and the real conditions of clinical practice.
Consent for publication
All authors read and approved the final manuscript.
Competing interests
The authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hernández-Quiles, R., Merino-Lucas, E., Boix, V. et al. Bacteraemia and quick Sepsis Related Organ Failure Assessment (qSOFA) are independent risk factors for long-term mortality in very elderly patients with suspected infection: retrospective cohort study. BMC Infect Dis 22, 248 (2022). https://doi.org/10.1186/s12879-022-07242-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07242-4