Abstract
Background
Drug-resistant tuberculosis (TB) continues to be a public health threat. There are few studies on transmission and genotyping of MDR-TB family households in China. This study aimed to investigate transmission of multidrug-resistant tuberculosis (MDR-TB) within family households by deletion-targeted multiplex polymerase chain reaction (DTM-PCR), mycobacterial interspersed repetitive unit variable number tandem repeats (MIRU-VNTR) genotyping.
Methods
Among 993 MDR-TB patients registered from Wuhan Institute for Tuberculosis Control, drug resistance and the time interval between the index patients and secondary patients were analyzed in 49 MDR-TB patients from 23 families, in which 22 MDR-TB strains from 11 families who had matched strains were genotyped by DTM-PCR and standard 24-loci MIRU-VNTR genotyping method.
Results
The time interval between the index patients and the secondary patients ranged from half a month to 110 months. Thirteen secondary patients developed active MDR-TB within two years and accounted for 50% (13/26) of all secondary patients. Among eleven pairs of MDR-TB families, six pairs had identical genotypes, the cluster rate was 54.5% (12/22); three pairs had a single MIRU-VNTR locus variation. If a single MIRU-VNTR locus variation was tolerated in the cluster definition, the cluster rate raised to 81.8% (18/22).
Conclusions
The family households of MDR-TB patients are at risk for infection of MDR-TB. To reduce transmission, MDR-TB patients should be diagnosed earlier and promptly treated in an effective manner, meanwhile, the close family contacts should be screened for TB infection.
Similar content being viewed by others

Background
Drug-resistant tuberculosis (TB) continues to be a public health threat. Worldwide in 2019, close to half a million people developed rifampicin-resistant TB (RR-TB), of which 78% had multidrug-resistant TB (MDR-TB). China ranked the second (14%) among the countries with the largest share of the global burden of MDR-TB [1]. MDR-TB is transmitted through air droplets like drug-susceptible tuberculosis. The high-risk groups most vulnerable to the spread of MDR-TB are close family contacts. Data show that MDR-TB close contacts are often multidrug-resistant when they develop active TB [2, 3]. Among immunocompromised people, the highest risk of developing TB within the first two years after exposure is about 5%-10%, after which the risk is significantly reduced. In the areas with high burden of TB, above half of family members are infected with the same bacterial strain [4]. The WHO “Guidelines for the programmatic management of drug-resistant tuberculosis” recommends that the investigation of MDR-TB contacts should be given priority; close contacts of MDR-TB should be followed up for at least 2 years.
Genotyping of Mycobacterium tuberculosis (MTB) strains is important to effectively guide outbreak investigations, define transmission dynamics and assist global epidemiological surveillance of the disease [5]. Owing to its shorter turnaround and simple numerical nomenclature system, mycobacterial interspersed repetitive unit variable number tandem repeats (MIRU-VNTR) genotyping, which is based on 24 standardized loci has replaced IS6110 DNA fingerprinting over the last decade as a gold standard among classical strain typing methods for many applications [5]. In addition, the deletion-targeted multiplex polymerase chain reaction (DTM-PCR), which is also faster and easier to perform, has been considered as a good alternative method to Spoligotyping to identify Mycobacterium tuberculosis Beijing strains. The Beijing genotype is predominant among MDR-TB strain in China [6, 7].
Literature analysis revealed studies on transmission and genotyping of MDR-TB family close contacts in China is scarce and limited with case reports [8, 9]. In the current study, we collected data on 993 MDR-TB patients from Wuhan Institute for Tuberculosis Control, a site for National MDR Tuberculosis Prevent and Control Management Demonstration Zone under MDR-TB Prevention and Control Project between January 1, 2007 and March 31, 2018. forty-nine MDR-TB family members were finally chosen for analysis wherein, their drug resistance patterns, and transmission was analysed using DTM-PCR and 24-loci MIRU-VNTR genotyping methods.
Methods
Ethics statement
The study was approved by the Medicine Ethics Committee of Wuhan Pulmonary Hospital. All the patients provided informed consent before participation in this study. Ethics in accordance with the Helsinki Declaration on the participation of human subjects in medical research were respected.
Patients
From January 1, 2007 to March 31, 2018, 993 MDR-TB patients were enrolled in the Wuhan MDR-TB Prevention and Control Project, among them 49 MDR-TB family members representing 23 families (There were two cases in 20 families, and there three cases in three families) were included for analysis in this study.
Diagnosis of MDR-TB
Sputum specimens were decontaminated with a 2–fourfold volume of 4% NaOH, liquefied at room temperature for 20 min. The processed specimens were inoculated on to Lowenstein-Jensen (L-J) based solid medium for isolation of Mycobacteria. Drug susceptibility testing was performed by using the proportion method on Lowenstein-Jensen (L-J) medium. The following drug critical concentrations were used: isoniazid (INH): 0.2 μg/mL, rifampicin (RFP): 40.0 μg/mL, streptomycin (SM): 4.0 μg/mL, ethambutol (EMB): 2.0 μg/mL, ofloxacin (OFX): 2.0 μg/mL, kanamycin (KM): 20.0 μg/mL. MDR-TB is defined as resistance to at least isoniazid and rifampicin in vitro[10].
Discovery of a secondary case
MDR-TB patient diagnosis and treatment information was inputted into the China Disease Prevention and Control Information System Tuberculosis Special Report System. Wuhan Institute for Tuberculosis Control set up a MDR-TB clinic, which assigned one doctor and one nurse to be responsible for establishing the medical record information of MDR-TB patients. During the two years of treatment and management, they conducted interviews and screenings for close contacts in MDR-TB families. The case information of close contact in MDR-TB families was collected, such as whether there were cough, fever, night sweat and other symptoms. Sputum specimens from patients with cough, strong TST positive and abnormal chest X-rays were collected for smears and culture.
Relevant definitions
Index case The first MDR-TB patient diagnosed in the family, according to the date of collection of the first culture -positive specimen.
Secondary case The MDR-TB patient diagnosed subsequently in the same family.
MDR-TB close family contact People living in the same family, or people who spend several hours a day with the MDR-TB patient in the same room.
The DTM-PCR typing method
Genomic DNA of the isolate was extracted according to the bacterial genomic DNA extraction kit provided by Daan Gene Biology Co., Ltd.
The method reported from Khosravi et al. [11] was used for DTM-PCR typing of all strains. W-Beijing family strains generally lack the RD105 region during the evolution process, while non-Beijing family strains still retain this region. Therefore, W-Beijing family strains can be identified by detecting the deletion of RD105.
MIRU-VNTR genotyping
MIRU-VNTR genotyping based on standard 24 loci [12] was performed to determine genetic relationships among isolates in this study. The 24 loci include MIRU02, Mtub04, ETRC, MIRU04, MIRU40, MIRU10, MIRU16, Mtub21, MIRU20, QUB11b, ETRA, Mtub29, Mtub30, ETRB, MIRU23, MIRU24, MIRU26, MIRU27, Mtub34, MIRU31, Mtub39, QUB26, QUB4156, and MIRU39. The primers were synthesized by Sangon Biotech (Shanghai) Co., Ltd. Each locus amplification reaction was performed in a total volume of 20 μl consisting of 10 μl 2 × Taq PCR MasterMix (CWBIO), 2 μl 2 μmol/L each primer, 1 μl DNA lysate and 5 μl ddH2O. The PCR products were analyzed in a 1.5 ~ 2% agarose gel using a 100 bp DNA ladder as the molecular weight standard. Positive and negative controls were included in each PCR reaction, as H37Rv and H2O, respectively. The number of tandem repeats was calculated based on the length of the repeat and flank sequences for each locus. The 24-digit profiles were compared using https://www.miru-vntrplus.org. The unweighted pair-group method with arithmetic mean (UPGMA) was used to construct the MIRU minimum tree.
Statistical processing
Excel 2013 software was used to manage data. SPSS21.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The demographic and clinical features of patients were assessed by univariate descriptive analysis.
Results
Inclusion and demographics of study subjects
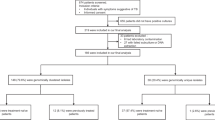
From January 1, 2007 to March 31, 2018, there were 993 MDR-TB patients enrolled in the Wuhan MDR-TB Prevention and Control Project, of which 49 were MDR-TB family members, and they were distributed in 23 families. Forty-nine MDR-TB cases from twenty-three families were included in our study. Twenty-two matched strains from eleven families were typed on DTM-PCR and MIRU-VNTR genotyping (Fig. 1).
Among the 49 MDR-TB patients, there were twenty-nine males and twenty females. Their age ranged from 15 to 72 years old. They were distributed in 23 families, and 40 patients came from 20 families which had two cases per family (one index case and one secondary case); nine patients came from three families, which had three cases per family (one index case and two secondary cases); There were 23 index cases and 26 secondary cases. Among the 26 secondary family cases, there were 15 males, accounting for 57.7%; 11 females, accounting for 42.3%; Their ages ranged from 15 to 68 years old. Among twenty-six secondary cases, six secondary cases had diabetes mellitus type 2 (T2DM) (Table 1).
The relationship between index cases and secondary cases
Thirty cases were parent–child relationship (57.7%), twelve cases were husband and wife relationship (23.1%), six cases were sibling relationship (11.5%), and four cases were relative relationship (7.7%) (Table 1).
Onset time of secondary cases
The time interval between the onset of the secondary case and the index case was 0.5–110 months, of which thirteen cases occurred within two years, accounting for 50.0%; eight cases occurred at an interval of 3–4 years, accounting for 30.8%; four cases occurred at an interval of 5 years, accounting for 15.4%; one case occurred more than nine years apart, accounting for 3.8%.
The phenotypic susceptibility results of the secondary cases and the index cases
The phenotypic susceptibility results of the secondary cases and the index cases were consistent in thirteen cases, accounting for 50%, and the phenotypic susceptibility results were inconsistent in thirteen cases, accounting for 50%.
The results of DTM-PCR and 24-loci MIRU-VNTR genotyping
DTM-PCR typing of twenty-two strains of Mycobacterium tuberculosis from eleven pairs of families showed that twenty-one strains belonged to Beijing genotype, and only one strain (A12-1) belonged to non-Beijing genotype.
We performed 24-loci MIRU-VNTR genotyping on twenty-two strains of Mycobacterium tuberculosis from eleven pairs of matched families, and UPMGA method was used to draw the minimum classification tree, as shown in Fig. 2. The genotyping results of six pairs of families were consistent. Three pairs of families (A5, A6, A17) had one locus difference in genotyping results. One pair of families (A19) has four loci differences, and one pair of families (A12) had 12 loci differences.
Discussion
MDR-TB is a heavy burden on tuberculosis control due to the variety of treatment drugs, long treatment course, high incidence of adverse reactions, and high treatment costs. It may lead to adverse treatment outcomes or deaths to patients, and bring great damage to patients' physical and mental health and their family. Close family contacts are high-risk groups of transmission [13]. A second case or more than one case of MDR-TB in a family will cause great psychological and family financial harm. The proportion of patients with catastrophic family expenditures due to MDR-TB is up to 78% [14]. Follow-up of close contacts of MDR-TB families can identify and treat MDR-TB patients in a timely manner, effectively saving more lives and reducing transmission within the family.
Like ordinary tuberculosis, transmission of MDR-TB is mainly short-range droplet transmission. Because there is no better isolation and protection measures in contact time and space for the family living in the same household, MDR-TB is easier to spread. A previous study reported transmission from close family contacts of smear-positive pulmonary tuberculosis patients in China [15], but few reports were available about the transmission of MDR-TB from close family contacts. Studies from the other countries reported that the incidence of MDR-TB was higher among close family contacts of MDR-TB patients [16, 17].
If there are two or more secondary MDR-TB cases in close family contacts, it is called an outbreak [18]. An outbreak of seven and four MDR-TB cases in close family contacts has been documented Turkey [18] and Taiwan, China [9]. This study collected the cluster incidence of MDR-TB in 23 families and showed that there were three outbreaks of MDR-TB in the three families. This study showed that among the transmission of MDR-TB in family members, the highest transmission rate occurred between parents and children (57.7%), followed by transmission between couples (23.1%), indicating the risk of transmission between parents and children and between couples is high. The risk of transmission between siblings is relatively low, suggesting that MDR-TB transmission is related to close family contact. It has been reported [19] that the risk of onset is the highest within two years of MDR-TB exposure. The results of this study showed that the shortest time interval between the onset of the secondary case and the index case was half a month and the longest interval was 110 months. Fifty percent of the secondary cases had the onset within two years, and 80.8% of the secondary cases had the onset within three years. The results suggested that the follow-up of close contacts of MDR-TB for three years can detect 80% of secondary cases early, then early isolation and treatment can reduce transmission.
Many factors are involved in influencing for the occurrence of MDR-TB. MDR-TB patients can cause great transmission before, during and after the treatment period to potentially harm the surrounding population. Gao Qian et al. [20] believed that transmission is the main cause of high rates of drug resistance to TB in China. A study in Peru [21] showed that 64.3% (27/42) of the secondary cases had the same phenotypic susceptibility results as the index case, and 50% of the secondary cases in this study were consistent with the index case, indicating that there might be intra-family transmission. The phenotypic susceptibility results of 50% of the secondary cases were inconsistent with those of the index cases. There might be two situations: one was that the secondary cases were infected through other routes and were not transmitted within the family; the other was the transmission within families due to the inconsistent stability of drug sensitivity tests for different anti-tuberculosis drugs. INH and RFP have the highest stability [22], while other anti-tuberculosis drugs such as EMB, SM, KM and OFX have poor stability and poor reproducibility, resulting in the same susceptibility results of INH and RFP among family cases, but the drug susceptibility results of other anti-tuberculosis drugs are not consistent.
Diabetes mellites is correlated with increased susceptibility to and disease progression of tuberculosis [23]. Our results showed that six of twenty-six secondary cases had diabetes mellitus type 2 (T2DM), for which the time intervals were 0.5, 10, 46, 41, 45, 110 months respectively. Among them, two cases were diagnosed within one year, four cases were diagnosed after more than three years. This indicated MDR-TB household contacts with diabetes might be susceptible to tuberculosis and should be early screened and followed up for TB infection.
The MIRU-VNTR typing method is a simple and rapid method for Mycobacterium tuberculosis genotyping, and also an important tool for TB molecular epidemiology study, which can be used to explore the transmission mechanism of tuberculosis, contact investigation and homology investigation. There were few reports on the genotyping of transmission in MDR-TB families, but most of which were case reports [8, 9]. We used the standard 24-loci MIRU-VNTR genotyping in twenty-two MDR-TB patients, and twelve (54.5%) had exactly the same genotype, and three cases differed in only one locus. If defined as clusters within one locus, intra-family transmission increased to eighteen cases (81.8%), which was basically consistent with the results of family transmission of tuberculosis reported by Augustynowicz-Kopec et al. [24]. As MIRU-VNTR assays discriminate genotypic differences during the transmission process, some loci may be variable during transmission [25]. Cavany SM's genotype among matched tuberculosis close contacts was 79% homologous, which also suggested higher contact transmission [26]. Although there were identical phenotypic drug susceptible test results in two familial strains, the more extensive differences in them precluded intra-family transmission of MDR-TB. Patients from those families could have developed MDR-TB as a result of transmission from outside the household.
The traditional opinion is that bacterial resistance will reduce bacterial fitness, which manifests itself in a lower risk of transmission of resistant organisms [27, 28]. Some studies indicated some resistance mutations reduce growth rates or virulence [29, 30], others argued that some mutations had little or variable impact [31]. Even when mutations do confer fitness costs, subsequent ‘compensatory’ mutations can overcome fitness deficits associated to drug resistance, setting the basis for the spread of DR-TB [32, 33]. Although the transmission of MDR-TB and sensitive tuberculosis are controversial, some authors believed that there was no difference between the transmission of MDR-TB and sensitive tuberculosis at population level [34]. Our results further confirmed that the close family contacts of MDR-TB patients had a higher transmission rate. Personal protection, education, and screening should be carried out in accordance with regulations for close contacts of MDR-TB patients to reduce transmission.
There are several limitations in our study. First of all, in twenty-three matched families, we only collected and genotyped eleven pairs of MTB strains from eleven families, the other samples were not included due to strain loss or death. Second, due to lack of investigation of family contacts of MDR-TB patients, it was impossible to analyze the incidence of MDR-TB in close family contacts. Finally, the lack of investigation in contact networks outside the patient households was a limitation of the current work.
Conclusions
This study indicates that the family households of MDR-TB patients are at risk for infection of MDR-TB. To reduce transmission, MDR-TB patients should be diagnosed earlier and promptly treated effectively, meanwhile the family contacts should be screened for TB infection and be followed up at least two years.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- DNA:
-
Deoxyribonucleic acid
- DTM-PCR:
-
Deletion-targeted multiplex polymerase chain reaction
- EMB:
-
Ethambutol
- INH:
-
Isoniazid
- IS6110:
-
Insert sequence 6110
- KM:
-
Kanamycin
- MDR-TB:
-
Multidrug-resistant tuberculosis
- MIRU-VNTR:
-
Mycobacterial interspersed repetitive unit variable number tandem repeats
- MTB:
-
Mycobacterium tuberculosis
- OFX:
-
Ofloxacin
- RFP:
-
Rifampicin
- RR-TB:
-
Rifampicin-resistant tuberculosis
- SM:
-
Streptomycin
- TB:
-
Tuberculosis
- TST:
-
Tuberculin skin test
- T2DM:
-
Diabetes mellitus type 2
- UPGMA:
-
The unweighted pair-group method with arithmetic mean
- WHO:
-
World Health Organization
References
World Health Organization. Global Tuberculosis Report 2020. Geneva: World Health Organization; 2020.
Becerra MC, Appleton SC, Franke MF, Chalco K, Arteaga F, Bayona J, Murray M, Atwood SS, Mitnick CD. Tuberculosis burden in households of patients with multidrug-resistant and extensively drug-resistant tuberculosis: a retrospective cohort study. Lancet. 2011;377(9760):147–52.
Shadrach BJ, Kumar S, Deokar K, Singh GV, Hariharan, Goel R. A study of multidrug resistant tuberculosis among symptomatic household contacts of MDR-TB patients. Indian J Tuberc. 2021;68(1):25–31.
Conceição EC, Guimarães A, Lopes ML, Furlaneto IP, Rodrigues YC, da Conceição ML, Barros WA, Cardoso NC, Sharma A, Lima L, et al. Analysis of potential household transmission events of tuberculosis in the city of Belem, Brazil. Tuberculosis (Edinb). 2018;113:125–9.
Merker M, Kohl TA, Niemann S, Supply P. The evolution of strain typing in the Mycobacterium tuberculosis complex. Adv Exp Med Biol. 2017;1019:43–78.
Luo D, Chen Q, Xiong G, Peng Y, Liu T, Chen X, Zeng L, Chen K. Prevalence and molecular characterization of multidrug-resistant M. tuberculosis in Jiangxi province, China. Sci Rep. 2019;9(1):7315.
Zhang Z, Lu J, Liu M, Wang Y, Qu G, Li H, Wang J, Pang Y, Liu C, Zhao Y. Genotyping and molecular characteristics of multidrug-resistant Mycobacterium tuberculosis isolates from China. J Infect. 2015;70(4):335–45.
Yan LP, Qin LH, Zhang Q, Sun H, Han M, Xiao HP. Transmission of extensively drug-resistant and multidrug resistant Mycobacterium tuberculosis in families identified by genotyping. Chin Med J (Engl). 2013;126(3):521–5.
Tang TQ, Fu SC, Chen YH, Chien ST, Lee JJ, Lin CB. Outbreak of multidrug-resistant tuberculosis in an aboriginal family in eastern Taiwan. Ci Ji Yi Xue Za Zhi. 2016;28(1):29–32.
Aziz MA, Wright A, Laszlo A, De Muynck A, Portaels F, Van Deun A, Wells C, Nunn P, Blanc L, Raviglione M, et al. Epidemiology of antituberculosis drug resistance (the Global Project on Anti-tuberculosis Drug Resistance Surveillance): an updated analysis. Lancet. 2006;368(9553):2142–54.
Khosravi AD, Goodarzi H, Alavi SM, Akhond MR. Application of deletion- targeted multiplex PCR technique for detection of Mycobacterium tuberculosis Beijing strains in samples from tuberculosis patients. Iran J Microbiol. 2014;6(5):330–4.
Supply P, Allix C, Lesjean S, Cardoso-Oelemann M, Rusch-Gerdes S, Willery E, Savine E, de Haas P, van Deutekom H, Roring S, et al. Proposal for standardization of optimized mycobacterial interspersed repetitive unit-variable-number tandem repeat typing of Mycobacterium tuberculosis. J Clin Microbiol. 2006;44(12):4498–510.
Baliashvili D, Kempker RR, Blumberg HM, Kuchukhidze G, Merabishvili T, Aslanikashvili A, Magee MJ. A population-based tuberculosis contact investigation in the country of Georgia. Public Health Action. 2018;8(3):110–7.
Mullerpattan JB, Udwadia ZZ, Banka RA, Ganatra SR, Udwadia ZF. Catastrophic costs of treating drug resistant TB patients in a tertiary care hospital in India. Indian J Tuberc. 2019;66(1):87–91.
Guo J, Yang M, Wu Z, Shen X, Wang Y, Zhao G. High incidence and low case detection rate among contacts of tuberculosis cases in Shanghai, China. BMC Infect Dis. 2019;19(1):320.
Vella V, Racalbuto V, Guerra R, Marra C, Moll A, Mhlanga Z, Maluleke M, Mhlope H, Margot B, Friedland G, et al. Household contact investigation of multidrug-resistant and extensively drug-resistant tuberculosis in a high HIV prevalence setting. Int J Tuberc Lung Dis. 2011;15(9):1170–5.
Javaid A, Khan MA, Khan MA, Mehreen S, Basit A, Khan RA, Ihtesham M, Ullah I, Khan A, Ullah U. Screening outcomes of household contacts of multidrug-resistant tuberculosis patients in Peshawar, Pakistan. Asian Pac J Trop Med. 2016;9(9):909–12.
Iliaz S, Caglar E, Koksalan OK, Chousein EG. An outbreak of multidrug-resistant tuberculosis among a family. Indian J Tuberc. 2016;63(2):130–2.
Moore DA. What can we offer to 3 million MDRTB household contacts in 2016? BMC Med. 2016;14:64.
Yang C, Luo T, Shen X, Wu J, Gan M, Xu P, Wu Z, Lin S, Tian J, Liu Q, et al. Transmission of multidrug-resistant Mycobacterium tuberculosis in Shanghai, China: a retrospective observational study using whole-genome sequencing and epidemiological investigation. Lancet Infect Dis. 2017;17(3):275–84.
Grandjean L, Crossa A, Gilman RH, Herrera C, Bonilla C, Jave O, Cabrera JL, Martin L, Escombe AR, Moore DA. Tuberculosis in household contacts of multidrug-resistant tuberculosis patients. Int J Tuberc Lung Dis. 2011;15(9):1164–9.
Kim SJ. Drug-susceptibility testing in tuberculosis: methods and reliability of results. Eur Respir J. 2005;25(3):564–9.
Menon S, Rossi R, Nshimyumukiza L, Wusiman A, Zdraveska N, Eldin MS. Convergence of a diabetes mellitus, protein energy malnutrition, and TB epidemic: the neglected elderly population. BMC Infect Dis. 2016;16:361.
Augustynowicz-Kopec E, Jagielski T, Kozinska M, Kremer K, van Soolingen D, Bielecki J, Zwolska Z. Transmission of tuberculosis within family-households. J Infect. 2012;64(6):596–608.
Jeon S, Lim N, Park S, Park M, Kim S. Comparison of PFGE, IS6110-RFLP, and 24-Locus MIRU-VNTR for molecular epidemiologic typing of Mycobacterium tuberculosis isolates with known epidemic connections. J Microbiol Biotechnol. 2018;28(2):338–46.
Cavany SM, Vynnycky E, Sumner T, Macdonald N, Thomas HL, White J, White RG, Maguire H, Anderson C. Transmission events revealed in tuberculosis contact investigations in London. Sci Rep. 2018;8(1):6676.
Espinal MA, Dye C. Can DOTS control multidrug-resistant tuberculosis? Lancet. 2005;365(9466):1206–9.
Gygli SM, Borrell S, Trauner A, Gagneux S. Antimicrobial resistance in Mycobacterium tuberculosis: mechanistic and evolutionary perspectives. FEMS Microbiol Rev. 2017;41(3):354–73.
Nieto RL, Mehaffy C, Creissen E, Troudt J, Troy A, Bielefeldt-Ohmann H, Burgos M, Izzo A, Dobos KM. Virulence of Mycobacterium tuberculosis after acquisition of isoniazid resistance: individual nature of katG mutants and the possible role of AhpC. PLoS ONE. 2016;11(11):e0166807.
Mariam DH, Mengistu Y, Hoffner SE, Andersson DI. Effect of rpoB mutations conferring rifampin resistance on fitness of Mycobacterium tuberculosis. Antimicrob Agents Chemother. 2004;48(4):1289–94.
Casali N, Nikolayevskyy V, Balabanova Y, Harris SR, Ignatyeva O, Kontsevaya I, Corander J, Bryant J, Parkhill J, Nejentsev S, et al. Evolution and transmission of drug-resistant tuberculosis in a Russian population. Nat Genet. 2014;46(3):279–86.
Nguyen QH, Contamin L, Nguyen TVA, Banuls AL. Insights into the processes that drive the evolution of drug resistance in Mycobacterium tuberculosis. Evol Appl. 2018;11(9):1498–511.
Brandis G, Pietsch F, Alemayehu R, Hughes D. Comprehensive phenotypic characterization of rifampicin resistance mutations in Salmonella provides insight into the evolution of resistance in Mycobacterium tuberculosis. J Antimicrob Chemother. 2015;70(3):680–5.
Becerra MC, Huang CC, Lecca L, Bayona J, Contreras C, Calderon R, Yataco R, Galea J, Zhang Z, Atwood S, et al. Transmissibility and potential for disease progression of drug resistant Mycobacterium tuberculosis: prospective cohort study. BMJ. 2019;367:5894.
Acknowledgements
We are grateful to all the participants involved in this study.
Funding
This work was supported by China TB Control Program of Global Fund (CHN-S10-G14-T), The Science and Technology Program Of The Health and Family Planning Commission of Wuhan Municipality (WG15A04, WG13A04, WG20A03), The Science and Technology Program of Hubei Provincial Health Commission (WJ2021M026).
Author information
Authors and Affiliations
Contributions
JC, LFC, QHD and MLZ were the primary researchers, conceived and designed the study. JC, LFC, MZ, GW, YYR, CJ, QHD and MLZ performed data collection, DST, amplification and gel-electrophoresis, interpreted results and helped draft the manuscript. JC, LFC and QHD performed the statistical analysis. JC, LFC, CJ, QHD and MLZ wrote the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Medicine Ethics Committee of Wuhan Pulmonary Hospital. All the patients provided informed consent before participation in this study. Ethics in accordance with the Helsinki Declaration on the participation of human subjects in medical research were respected.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, J., Chen, L., Zhou, M. et al. Transmission of multidrug-resistant tuberculosis within family households by DTM-PCR and MIRU-VNTR genotyping. BMC Infect Dis 22, 192 (2022). https://doi.org/10.1186/s12879-022-07188-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07188-7




