Abstract
Background
Maternal immunization confers passive immunity to the fetus by transplacental antibody transfer. Infants may be better protected against pertussis if the mother received a diphtheriae, tetanus and acellular pertussis (Tdap) vaccination in the second trimester of pregnancy compared to the third trimester. This study evaluates IgG antibody concentrations in term and preterm infants at birth and 2 months after birth after maternal Tdap-vaccination between 200 and 240 w of gestation vs third trimester Tdap-vaccination. Further aims are assessing the determinants that underlie acceptance of second trimester maternal Tdap-vaccination as well as the tolerability of vaccination.
Methods
This prospective cohort study consists of two parts. In the acceptance part, pregnant women complete a questionnaire on determinants that underlie acceptance of a second trimester Tdap-vaccination, which is offered subsequently between 200 and 240 w of gestation. Vaccinated women complete an additional questionnaire on vaccination tolerability. Vaccinated women may also participate in the immunogenicity part, in which blood is drawn from mother at delivery and from infant at birth and 2 months after birth. Women are also eligible for the immunogenicity part if they received a Tdap-vaccination between 200 and 240 w of gestation via the national immunization program and get hospitalized for an imminent preterm delivery. Blood sampling continues until 60 term and 60 preterm mother-infant-pairs have been included. Pertussis-specific IgG antibody concentrations are determined in serum using a fluorescent bead-based multiplex immunoassay. For term infants, non-inferiority in IgG antibody concentrations against pertussis toxin (anti-PT) will be assessed referred to a historical control group in which mothers were Tdap-vaccinated between 300 and 320 w of gestation. For preterm infants, non-inferiority of anti-PT IgG concentrations is referred to as 85% of infants having ≥ 20 international units/mL at 2 months after birth.
Discussion
This study investigates acceptance, tolerability and immunogenicity regarding maternal Tdap-immunization between 200 and 240 w of gestation. Its results provide insight into the effects of second trimester Tdap-vaccination on IgG antibody concentrations in term and preterm infants before primary infant vaccinations. Results on acceptance and tolerability guide antenatal care providers in communication with pregnant women and maintain the safety of second trimester Tdap-vaccination.
Trial registration: EU Clinical Trials Register, 2018-002976-41, retrospectively registered 24 July 2019, https://www.clinicaltrialsregister.eu/ctr-search/search?query=2018-002976-41.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Pertussis is a respiratory infectious disease caused mainly by Bordetella pertussis. Especially young infants are at increased risk of severe complications, hospitalization and sometimes even death [1]. Infant vaccinations against pertussis started around 1950 with steady high coverage, leading to lower incidences [2, 3]. However, in the nineties of the previous century, pertussis re-emerged in many countries, including the Netherlands [4]. Incidences in all ages increased with epidemic peaks every 3–4 years (Fig. 1) [5].
Number of pertussis notifications per 100,000 per age category in 2005–2019 [31]
The Netherlands implemented several changes in the national immunization program in response to the increase. In 1999, the first pertussis containing vaccination was scheduled at 2 months (m) instead of 3 m. Late in 2001, an acellular pertussis component was added to the preschool diphtheria, tetanus and poliomyelitis booster dose at 4 years (y) of age and from 2005 onwards, the primary infant pertussis vaccinations also contained an acellular pertussis component instead of whole cell pertussis. However, surveillance data show that the incidence in young infants did not decrease following these changes (Fig. 1) [5]. In fact, an increase within this vulnerable age group was observed during every epidemic peak [2]. Adolescents and adults are likely a source of transmission to young infants [6].
In 2011, increased incidence rates of reported pertussis cases were followed by a large outbreak in 2012 in the Netherlands and surrounding countries, including England [7]. In response to an increasing number of pertussis related deaths, the English government decided to offer a maternal pertussis vaccination by means of a tetanus, diphtheria, acellular pertussis and poliomyelitis (Tdap-IPV) vaccine to all pregnant women during the third trimester. Maternal vaccination induces protection of young, not yet (fully) vaccinated infants. It confers passive immunity to the fetus by transplacental antibody transfer, which starts around 17 weeks (w) of gestational age (GA) and peaks in the third trimester [8]. After birth, maternal antibodies wane rapidly over time [9].
The uptake in England ranged around 70% and observational data showed a high vaccine effectiveness without any important safety concerns [9, 10]. To date, over 25 countries recommend maternal pertussis immunization with reassuring effectiveness and safety data. In December 2015, the Health Council of the Netherlands advised to offer a pertussis vaccination to all pregnant women in their third trimester [11]. In July 2018, the Ministry of Health, Welfare and Sports, decided to follow the advice of a maternal pertussis vaccination program. First vaccinations were offered mid December 2019.
Most countries offer third trimester Tdap-vaccination because of its benefits for newborns in general. However, preterm infants are less protected by third trimester Tdap-vaccination due to too short time intervals between vaccination and delivery. This was demonstrated in data from England, showing that preterm infants were overrepresented in pertussis hospitalizations and with an increase from 9.8 to 12.1% in the share of preterm infants after the introduction of third trimester Tdap-vaccination [12]. A similar overrepresentation of preterm infants among pertussis hospitalizations is shown in Norway (10.0% vs 5.2%) [13] and in the Netherlands (11.8% vs 7.8%) [14]. To offer women more opportunities for vaccination, England widened the interval for maternal Tdap-vaccination to the second trimester [15], resulting in an increase of the vaccination coverage of about 15% [16]. The overrepresentation of pertussis in preterm infants in England reduced strongly since widening this interval [17]. Switzerland also recommends vaccination from second trimester onwards and showed that infants of second trimester vaccinated mothers had higher antibody levels at birth than infants of third trimester vaccinated mothers [18]. Importantly, they also showed that preterm infants of second trimester vaccinated mothers had higher pertussis antibody levels at birth than preterm infants of third trimester vaccinated mothers [19]. By contrast, Winter et al. demonstrated that third trimester Tdap-vaccination was more effective in preventing clinical pertussis than vaccination earlier during pregnancy (85% vs 64%) [20]. However, both studies used different endpoints, i.e. Eberhardt et al. used immunogenicity as outcome measure, while Winter et al. used effectiveness as outcome measure. In the Netherlands, Tdap-vaccines are offered to pregnant women from 22 w GA onwards and administered via youth public healthcare services. Studies show that women in their second trimester are less willing to accept the vaccination compared to women later throughout gestation [21, 22]. However, these studies were performed without current knowledge that preterm infants are worse off than term infants following third trimester pertussis vaccination.
We set up this study of pregnant women and their infants to fill the knowledge gap on the effects of second trimester maternal Tdap-vaccination for the prevention of pertussis in term and preterm infants. In a prospective study that is divided into two study parts, i.e. acceptance and immunogenicity, we aim to assess the determinants that underlie acceptance of Tdap-vaccination in the second trimester of pregnancy and how second trimester Tdap-vaccination induces maternal antibody levels in term and preterm infants before primary vaccinations. Furthermore, we aim to assess tolerability of a maternal Tdap-vaccination.
Methods/design
Study design and objectives
This study is conducted as a prospective cohort study of pregnant women, with follow-up of their infants up to 2 m of age. It is divided into two parts. In the acceptance part, determinants that underlie acceptance of second trimester Tdap-vaccination are assessed using a questionnaire, as followed up by the tolerability after vaccination. In the immunogenicity part, pertussis-specific IgG antibody concentrations are determined in term and preterm infants at birth and 2 m after birth if the mother accepted the vaccination between 200 and 240 w GA.
Primary objectives
Immunogenicity part
-
To evaluate non-inferiority of anti-Pertussis Toxin (PT) IgG antibodies in term infants at 2 m of age born of mothers who received a Tdap-vaccination between 200 and 240 w GA, compared to a reference anti-PT IgG at 2 m of age in a historical control group of term infants born of mothers who were vaccinated between 300 and 320 w GA in the period January 2014 to February 2016.
-
To evaluate non-inferiority of anti-PT IgG in preterm infants at 2 m of age born of mothers who received a Tdap-vaccination between 200 and 240 w GA, as referred to at least 85% of preterm infants having anti-PT IgG concentrations ≥ 20 international units (IU)/mL as used in many immunogenicity studies.
Secondary objectives
Acceptance part
-
To assess pregnant women’s social cognitive determinants and underlying beliefs on maternal Tdap-vaccination between 200 and 240 w GA and distinguish results among women who are pregnant for the first time, women who were pregnant before, and in both groups, women with and without a known increased risk of preterm delivery.
-
To assess the correlation between social cognitive determinants and underlying beliefs and actual behavior, i.e. acceptance of a maternal Tdap-vaccination between 200 and 240 w GA.
-
To compare social cognitive determinants and underlying beliefs of maternal Tdap-vaccination between 200 and 240 w GA with those of third trimester maternal vaccination.
Tolerability (extension of the acceptance part)
-
To assess tolerability of the maternal Tdap-vaccination, administered to pregnant women between 200 and 240 w GA.
-
To assess possible adverse pregnancy outcomes of maternal Tdap-vaccination between 200 and 240 w GA.
Immunogenicity part
-
To compare pertussis specific IgG concentrations at 2 m of age (i.e. before the primary infant vaccinations) between term and preterm infants.
-
To compare the decay in pertussis-specific maternal IgG concentrations in the first 2 m after birth between term and preterm infants.
-
To compare pertussis-specific IgG concentrations at delivery between mothers who delivered term and preterm.
-
To compare pertussis-specific IgG concentrations in mothers who received second trimester Tdap-vaccination and a group that received third trimester vaccination.
-
To determine levels of pertussis-specific IgG transferred from the mother to the neonate relative to the interval from vaccination to delivery, if possible depending on the variation in interval.
Study population and setting
The study population consists of pregnant women who receive primary, secondary or tertiary antenatal care. Participants are included by their antenatal care provider and followed-up prospectively in both the acceptance and immunogenicity study parts. By including women in secondary and tertiary care, we aim to oversample women with an increased risk for preterm delivery, e.g. women with multiple pregnancy, history of preterm delivery, cervical conization in the medical history and uterus anomaly.
In order to be eligible to participate in this study, women must be 18 y or older, pregnant, and in relation to the immunogenicity part of the study, both parents (or mother and legal guardian) must be willing to adhere to the protocol and perform all planned visits and sample collections for themselves and their newborn child. Women who meet any of the following criteria are excluded from participation in the immunogenicity part of this study: history of having received a pertussis containing vaccination in the past 2 years; known or suspected serious underlying condition that can interfere with the results of the study such as but not limited to cancer, autoimmune disease, immunodeficiency, seizure disorder or significant psychiatric illness; receipt of any high-dose (≥ 20 mg of prednisone daily or equivalent) daily corticosteroids within 2 weeks of study entry (inhaled or other local steroids are acceptable) with exception of corticosteroids to enhance maturation of fetal lungs in case of imminent early delivery; receipt of other immune modulating medication, for instance biologicals; receipt of blood products or immunoglobulins, within 3 months of study entry (rhesus negative women who receive anti-rhesus (D) immunoglobulin will not be excluded from the study); presence of bleeding disorder; having experienced a previous severe adverse reaction to any vaccine; receipt of any vaccine(s) within 2 weeks of study vaccine (except influenza vaccine which may be given concomitantly); all mothers who give birth before 240 w GA.
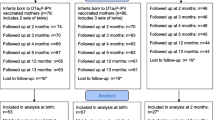
Recruitment and follow-up
In the acceptance part, women complete an online questionnaire on the determinants of acceptance of second trimester Tdap-vaccination. The vaccine is offered between 200 and 240 w GA and administered by their antenatal care provider if accepted. Vaccinated women complete a second questionnaire on the tolerability of vaccination. They are also eligible for participation in the immunogenicity study part. In this part, a blood sample from the mother and infant (cord blood) is drawn at delivery and a second sample from the infant at 2 m of age, i.e. before the first infant vaccination. Study samples are stored at the laboratory of the National Institute for Public Health and the Environment. Recruitment continues until blood samples are drawn from 60 term and 60 preterm mother-infant-pairs.
During the recruitment phase, two alternative recruitment routes were added to increase inclusion speed for both study parts (Fig. 2). The alternative acceptance route focuses on recruitment of women for the acceptance part via midwives in primary care facilities. The alternative immunogenicity route focuses on faster recruitment of preterm infants via secondary and tertiary antenatal care.
Alternative acceptance route
After completing the questionnaire on the determinants that underlie acceptance of second trimester Tdap-vaccination, midwifes inform pregnant women about the possibility of getting a Tdap-vaccination via youth public healthcare services. Vaccination status is requested retrospectively via the national immunization registry. The vaccine is not administered by the antenatal care provider in this route.
Alternative immunogenicity route
Antenatal care providers in hospitals ask consent for sampling cord blood and finger-stick-blood if a women gets hospitalized for an imminent preterm delivery and proves that she received a Tdap-vaccination between 200 and 240 w GA via the national immunization program. In case of an unclear answer, vaccination status is requested retrospectively via the national immunization registry. Further study procedures for blood sampling are identical to those in in the immunogenicity part.
Questionnaires
Acceptance
The online questionnaire focuses on behavioral determinants and beliefs that underlie acceptance of a second trimester Tdap-vaccination. It consists of about sixty questions and statements assessing demographics, social cognitive determinants, underlying beliefs, past experiences, women’s information desires and considerations regarding information provision and implementation of maternal Tdap-vaccination. A Dutch version of the questionnaire is provided in Additional file 1: Appendix 1.
Tolerability
This questionnaire contains questions about the onset of local reactions and solicited systemic adverse events (AE) within 1 week post-vaccination. Local reactions include swelling, redness, and pain at the injection site. Systemic AEs include fever, headache, tiredness, nausea, vomiting, diarrhea, dizziness, loss of appetite, stiffness of muscles and joints, itch, abnormal sweating, skin rash, swollen lymph nodes, sore throat, upper airway infection, coughing, fainting, and influenza-like illness. The questionnaire also includes questions about solicited systemic events at baseline, i.e. in the week pre-vaccination. Time interval and duration of symptoms are collected, as well as the use of analgesics, medical intervention, and absence from work and/or other activities. A Dutch version of the survey is provided in Additional file 2: Appendix 2.
Blood sample collection infant and mother (heel or finger stick)
For IgG testing using the X-map Luminex technology, a maximum of 2 mL infant cord blood is used. Furthermore, a maximum of 300 µl blood samples of the mother at birth and of the infants at 2 m of age is collected by heel or finger stick. Samples are tested for IgG antibody concentrations against pertussis antigens, diphtheria and tetanus. Antibody concentrations will be assessed in serum using a fluorescent bead-based multiplex immunoassay [23].
Defining prematurity
We define preterm infants as infants born before 350 w GA, although normally the cut-off for prematurity is set before 370 w GA. We assume that for preterm infants born between 350 and 360 w GA second or third trimester maternal Tdap-vaccination will generally allow enough time for sufficient transfer of antibodies. We will use the same definition for term infants as used in the historical control group, i.e. ≥ 370 w GA.
Investigational product
Boostrix is a suspension for injection in a prefilled syringe containing diphtheria, tetanus and acellular pertussis vaccine (adsorbed, reduced antigen content). The Boostrix vaccine will be given as a single 0.5 mL intramuscular injection, in the deltoid muscle of the upper arm between 200 and 240 w GA. For subjects who are ill or have a moderate or high fever (rectal temperature of > 38.0 °C), vaccination will be postponed until the symptoms of illness and the fever have disappeared. Pregnant women in the historical cohort [24] received the same vaccine investigational product.
Sample size calculation for immunogenicity part
To reach non-inferiority in term infants, the lower limit of the 95% confidence interval (CI) of the geometric mean concentration (GMC) after second trimester vaccination divided by the GMC after third trimester vaccination must be ≥ 0.5, with a one-sided 2.5% significance level and 80% power. As the GMC of anti-PT IgG in the historical control group (n = 58) was 26.1 IU/mL (95% CI 19.5–35.0), we need to include 53 term infants in the study. Taking into account 10% drop out or failed blood sampling, 58 term infants suffice.
Furthermore, non-inferiority in preterm infants is defined as 85% of infants with an anti-PT IgG above the 20 IU/mL at 2 m of age. This cut-off is used in many immunogenicity studies. With 10% precision, we need to include 49 blood samples from preterm mother-infant-pairs. Taking into account 10% drop-out or failed blood sampling, 54 preterm infants suffice. Due to the probability of multiple pregnancies in the preterm infant group and the likeliness of correlation between twins and triplets, preterm mother-infant-pairs are included and counted as one after multiple birth.
Statistical analyses
Acceptance part
Items targeting social cognitive determinants and beliefs are measured on 7-point Likert scales. Items with the same underlying theoretical construct will be averaged into one single construct in case internal consistency is sufficient (Cronbach’s alpha α > 0.60 or Pearson correlation coefficient r > 0.50). Spearman’s correlation test will be used to explore univariate associations for attitude with social cognitive determinants, underlying beliefs and possible barriers and facilitators. We will control for the false discovery rate in multiple testing according to the Benjamini–Hochberg procedure. Next, variables with the largest predictive value for women’s attitude towards pertussis vaccination during pregnancy will be determined by random forest analysis. We will compare results with a similar study which assessed the determinants of acceptance of third trimester maternal vaccination, to distinguish determinants on the acceptance of maternal Tdap-vaccination in second versus third trimester of pregnancy [25].
Tolerability (extension of the acceptance part)
The percentage and 95% CI of pregnant women experiencing adverse events (AE) within 1 week after Tdap-vaccination are described by type and severity of the AE. Using binary generalized mixed models (GLMM), the association between the occurrence of symptoms in the week before and the week after vaccination will be analyzed. Proportions of absence from work and/or other activities, and medical intervention within 7 days after vaccination will be calculated together with 95% CI as well as the association of these items before and after vaccination using GLMM.
Immunogenicity part
For term and preterm infants, GMCs and 95% CIs will be calculated for IgG antibodies against three pertussis antigens in the vaccine (PT, filamentous hemagglutinin (FHA), pertactin (Prn)), tetanus and diphtheria in mothers and infants at delivery, and for infants at 2 m of age, before the start of infant vaccination. Differences in GMCs between the two groups will be analyzed with a t-test. All reported p-values are 2-sided, p-values ≥ 0.05 are considered significant.
The decay in IgG antibody concentrations against PT, Prn, FHA, tetanus and diphtheria from birth until 2 m of age will be analyzed with a paired t-test that compares GMCs at birth and at 2 m of age, for term and preterm infants separately. The ratio between maternal GMCs and infant GMCs at birth will be calculated for term and preterm infants separately and stratified for time interval between vaccination and delivery.
For term infants, we will compare the results with another maternal Tdap-vaccination trial in which pregnant women received a Tdap-vaccination between 300 and 320 w GA. Anti-PT IgG concentrations of the 58 term infants from the comparator trial were also measured at 2 m of age.
Discussion
General implications of results
This prospective cohort study will investigate the acceptance, tolerability and immunogenicity regarding maternal Tdap-vaccination between 200 and 240 w GA. Its results will provide valuable insights into anti-PT IgG antibody concentrations in term and preterm infants before primary infant vaccinations and how the vaccination schedule of these infants may be optimized in response to second trimester Tdap-vaccination. Determinants and beliefs that underlie pregnant women’s acceptance of second trimester Tdap-vaccination may guide antenatal care providers in the communication and recommendation of vaccinating early throughout gestation. Furthermore, assessing local reactions and solicited systemic adverse events following second trimester Tdap-vaccination will aid in communication about its safety profile.
Changes in the Dutch vaccination schedule may be considered if non-inferiority of anti-PT IgG antibodies in preterm infants at 2 m is addressed. Currently in the Netherlands, a Tdap-vaccination during pregnancy replaces the first infant vaccination for term infants who may then be vaccinated at 3, 5 and 11 m with a DTaP-IPV-Hib-HepB vaccine. Preterm infants are excluded from this reduced schedule and receive an extra vaccination at 2 m of age. GMCs of preterm infants at 2 m of age may inform us whether such a reduced schedule is also feasible for (late) preterm infants if they relate to GMCs at corresponding ages in term infants. For term infants, non-inferiority of anti-PT IgG antibody concentrations after second trimester Tdap-vaccination informs us that anti-PT IgG antibodies may still be higher at 2 m of age, compared to third trimester Tdap-vaccination. Since more than 93% of all annual births in the Netherlands are born after 370 w GA [26], the results of this study may provide reassurance for pregnant women to obtain the maternal Tdap-vaccination at the earliest opportunity throughout gestation, i.e. at 22 w GA in the Netherlands.
Strengths
This is the first time that anti-PT IgG concentrations are investigated in term and preterm infants up to 2 m of age in response to second trimester Tdap-vaccination. The prospective study design with measurements at birth and 2 m of age allows us to assess the velocity of antibody decay before primary infant vaccinations. Drawing blood samples from mother-infant-pairs at delivery provides additional insight in the rate of placental antibody transfer corrected for gestation. Combining these aspects in immunogenicity with the acceptance part into a single study design results in efficient follow-up of women participating in both study parts and also complete the questionnaire on tolerability.
To our knowledge, behavioral determinants and beliefs that underlie maternal Tdap-vaccination acceptance have not yet been assessed specific for administering the vaccine in the second trimester of pregnancy. The use of multiple recruitment routes allows us to assess acceptance in women in primary care facilities and hospitals, thus reaching both healthy pregnant women and women with an increased risk of preterm delivery. The results may ultimately be used for communication early in pregnancy, especially when the risk of preterm delivery is addressed.
Limitations
Assessing antibodies in term mother-infant-pairs based on a historical comparator results in performing analyses at different timepoints, which might affect pertussis antibody responses. However, the differences between these cohorts are limited to the time interval of Tdap-vaccination throughout gestation in both studies. Remaining study procedures, e.g. recruitment, data management and the used investigational product, are similar and performed by the same research institute and laboratory.
Since a maternal Tdap-vaccine could be obtained free of charge via study participation, pregnant women with high intention of acceptance may introduce selection bias due to high willingness of participation. After December 2019 when the vaccination is offered within the National Immunization Program for which no money is charged, women may still be likely to participate in this study for obtaining the vaccine from their antenatal care provider, instead of making an appointment for vaccination at a youth public healthcare service. Altogether, the results of second trimester Tdap-acceptance among pregnant women may be estimated more optimistic than in real life.
The results of our study are limited to a follow-up time of 2 m after birth. Maternal antibodies are known to interfere with term infants’ immune responses after primary vaccination series, which is known as blunting [24, 27,28,29]. The likeliness of a reduced immune response after primary vaccinations is not assessed in infants born of mothers who received second trimester maternal Tdap-vaccination and remains implicated for future research.
Availability of data and materials
The anonymized datasets generated during the current study will be made available from the corresponding author on reasonable request.
Abbreviations
- AE:
-
Adverse event
- CI:
-
Confidence interval
- FHA:
-
Filamentous hemagglutinin
- GA:
-
Gestational age
- GMC:
-
Geometric mean concentration
- IU:
-
International units
- m:
-
Months
- Prn:
-
Pertactin
- PT:
-
Pertussis toxin
- Tdap:
-
Tetanus, diphtheriae, acellular pertussis
- w:
-
Weeks
- y:
-
Years
References
Vegelin AL, van Vught AJ, Wolfs TF, Kimpen JL, Geelen SP. Pertussis in young infants. Ned Tijdschr Geneeskd. 1998;142(49):2657–60.
Schurink-van't Klooster TM. The National Immunisation Programme in the Netherlands; surveillance and developments in 2015–2016. Bilthoven: National Institute for Public Health and the Environment; 2016. Report No.: 2016-0141.
van Wijhe M, McDonald SA, de Melker HE, Postma MJ, Wallinga J. Effect of vaccination programmes on mortality burden among children and young adults in the Netherlands during the 20th century: a historical analysis. Lancet Infect Dis. 2016;16(5):592–8.
de Melker HE, Schellekens JFP, Neppelenbroek SE, Mooi FR, Rumke HC, Conyn-van Spaendonck MAE. Reemergence of pertussis in the highly vaccinated population of the Netherlands: observations on surveillance data. Emerg Infect Dis. 2000;6(4):348–57.
van der Maas NAT, Mooi FR, de Greeff SC, Berbers GAM, Conyn-Spaendonck MAE, de Melker HE. Pertussis in the Netherlands, is the current vaccination strategy sufficient to reduce disease burden in young infants? Vaccine. 2013;31(41):4541–7.
de Greeff SC, Mooi FR, Westerhof A, Verbakel JM, Peeters MF, Heuvelman CJ, et al. Pertussis disease burden in the household: how to protect young infants. Clin Infect Dis. 2010;50(10):1339–45.
whooping cough vaccination; coverage may be widened. Br Med J (Clin Res Ed). 2012;345(7868):E5201.
Malek A, Sager R, Kuhn P, Nicolaides KH, Schneider H. Evolution of maternofetal transport of immunoglobulins during human pregnancy. Am J Reprod Immunol. 1996;36(5):248–55.
Amirthalingam G, Campbell H, Ribeiro S, Fry AM, Ramsay M, Miller CA, et al. sustained effectiveness of the maternal pertussis immunization program in England 3 years following introduction. CID. 2016;63(suppl_4):S236-43.
Donegan K, King B, Bryan P. Safety of pertussis vaccination in pregnant women in UK: observational study. BMJ. 2014;349:g4219.
Gezondheidsraad. Vaccinatie tegen kinkhoest: doel en strategie. Den Haag: Gezondheidsraad; 2015.
Byrne L, Campbell H, Andrews N, Ribeiro S, Amirthalingam G. Hospitalisation of preterm infants with pertussis in the context of a maternal vaccination programme in England. Arch Dis Child. 2017;103(3):224–9.
Riise OR, Laake I, Vestrheim D, Flem E, Moster D, Riise Bergsaker MA, et al. Risk of pertussis in relation to degree of prematurity in children less than 2 years of age. Pediatr Infect Dis J. 2017;36(5):e151–6.
van der Maas NAT, Sanders EAM, Versteegh FGA, Baauw A, Westerhof A, de Melker HE. Pertussis hospitalizations among term and preterm infants: clinical course and vaccine effectiveness. BMC Infect Dis. 2019;19(1):919.
Amirthalingam G, Brown CS, Campbell H, Chand MA, Fry NK. New Public Health England guidelines for managing pertussis in England. J Infect. 2017;74(2):202–4.
Pertussis vaccination programme for pregnant women update: vaccine coverage in England, April to June 2018. Public Health England; 2018.
Tessier E, Campbell H, Ribeiro S, Fry NK, Brown C, Stowe J, et al. Impact of extending the timing of maternal pertussis vaccination on hospitalized infant pertussis in England, 2014–2018. Clin Infect Dis. 2020. https://doi.org/10.1093/cid/ciaa836.
Eberhardt CS, Blanchard-Rohner G, Lemaitre B, Boukrid M, Combescure C, Othenin-Girard V, et al. Maternal immunization earlier in pregnancy maximizes antibody transfer and expected infant seropositivity against pertussis. Clin Infect Dis. 2016;62(7):829–36.
Eberhardt CS, Blanchard-Rohner G, Lemaitre B, Combescure C, Othenin-Girard V, Chilin A, et al. Pertussis antibody transfer to preterm neonates after second-versus third-trimester maternal immunization. Clin Infect Dis. 2017;64(8):1129–32.
Winter K, Nickell S, Powell M, Harriman K. Effectiveness of prenatal versus postpartum tetanus, diphtheria, and acellular pertussis vaccination in preventing infant pertussis. Clin Infect Dis. 2017;64(1):3–8.
van Lier A, Steens A, Ferreira JA, van der Maas NA, de Melker HE. Acceptance of vaccination during pregnancy: experience with 2009 influenza A (H1N1) in the Netherlands. Vaccine. 2012;30(18):2892–9.
Healy CM, Rench MA, Montesinos DP, Ng N, Swaim LS. Knowledge and attitiudes of pregnant women and their providers towards recommendations for immunization during pregnancy. Vaccine. 2015;33(41):5445–51.
van Gageldonk PG, van Schaijk FG, van der Klis FR, Berbers GA. Development and validation of a multiplex immunoassay for the simultaneous determination of serum antibodies to Bordetella pertussis, diphtheria and tetanus. J Immunol Methods. 2008;335(1–2):79–89.
Barug D, Pronk I, van Houten MA, Versteegh FGA, Knol MJ, van de Kassteele J, et al. Maternal pertussis vaccination and its effects on the immune response of infants aged up to 12 months in the Netherlands: an open-label, parallel, randomised controlled trial. Lancet Infect Dis. 2019;19(4):392–401.
Anraad C, Lehmann BA, Visser O, van Empelen P, Paulussen TGW, Ruiter RAC, et al. Social-psychological determinants of maternal pertussis vaccination acceptance during pregnancy among women in the Netherlands. Vaccine. 2020;38(40):6254–66.
Peristat: Perined; 2019. Available from: https://www.peristat.nl/.
Ladhani SN, Andrews NJ, Southern J, Jones CE, Amirthalingam G, Waight PA, et al. Antibody responses after primary immunization in infants born to women receiving a pertussis-containing vaccine during pregnancy: single arm observational study with a historical comparator. Clin Infect Dis. 2015;61(11):1637–44.
Hardy-Fairbanks AJ, Pan SJ, Decker MD, Johnson DR, Greenberg DP, Kirkland KB, et al. Immune responses in infants whose mothers received Tdap vaccine during pregnancy. Pediatr Infect Dis J. 2013;32(11):1257–60.
Abu Raya B, Edwards KM, Scheifele DW, Halperin SA. Pertussis and influenza immunisation during pregnancy: a landscape review. Lancet Infect Dis. 2017;17(7):e209–22.
General grant conditions: ZonMW. Available from: https://www.zonmw.nl/en/news-and-funding/funding/grant-conditions-and-finances/.
Schurink-van't Klooster TM, de Melker HE. The National Immunisation Programme in the Netherlands—Surveillance en Developments in 2019–2020. 2020.
Acknowledgements
We are grateful to all instances that provide participant recruitment and perform study procedures, in particular the investigators of the obstetrics and/or neonatology departments in participating hospitals: the University Medical Center in Utrecht, the Radboud University Medical Center in Nijmegen, the Erasmus University Medical Center in Rotterdam, the Gelre Hospital in Apeldoorn, the Maasstad Hospital in Rotterdam, the Spaarne Hospital in Haarlem, the Beatrix Hospital in Gorinchem, the Rivierenland Hospital in Tiel and the Diakonessenhuis Hospital in Utrecht.
Funding
This study is funded by a peer-reviewed, competitive grant from the Netherlands Organization for Health Research and Development (ZonMW Netherlands, Registration Number 522004008). General grant conditions are described on the ZonMW website [30].
Author information
Authors and Affiliations
Contributions
MI, MB, HdM, NR, ES and NvdM designed the study. MI coordinates study procedures, e.g. preparations, logistics, and acquisition in primary care facilities and hospitals under supervision of MB and NvdM. HdM maintains progress of participant recruitment and completion of the study within the predefined goals. MI wrote the manuscript. MB, HdM, NR, ES and NvdM critically revised subsequent versions. All authors agreed to be personally accountable for their own contribution. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Central Committee on Research Involving Human Subjects in the Netherlands (Registration Number: NL66966.000.18). All participants provide written informed consent for participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix 1.
Questionnaire on determinants that underlie acceptance of early maternal pertussis immunization (in Dutch).
Additional file 2: Appendix 2.
Questionnaire on local reactions and solicited systemic adverse events before and after vaccination (in Dutch).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Immink, M.M., Bekker, M.N., de Melker, H.E. et al. Study protocol of the PIMPI-project, a cohort study on acceptance, tolerability and immunogenicity of second trimester maternal pertussis immunization in relation to term and preterm infants. BMC Infect Dis 21, 897 (2021). https://doi.org/10.1186/s12879-021-06559-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-021-06559-w