Abstract
Background
The efficacy of lockdown in containing the COVID-19 pandemic has been reported in different studies. However, the impact on sociodemographic characteristics of individuals infected with SARS-CoV-2 has not been evaluated. The aim of this study was to describe the changes in sociodemographic characteristics of patients hospitalized for COVID-19 and to compare the transmission risk factors of COVID-19 before and during lockdown in France.
Methods
An observational retrospective study was conducted in a University Hospital in Paris, France. Data from patients hospitalized for COVID-19 in the Infectious Diseases Department between February 26 and May 11, 2020 were collected. The study population was divided into 2 groups: group A of patients infected before lockdown, and group B of patients infected during lockdown, considering a maximum incubation period of 14 days. Sociodemographic characteristics and transmission risk factors were compared between the 2 groups using Student’s t-test for continuous variables and Chi-2 test or Fisher exact test for categorical variables.
Results
Three hundred eighty-three patients were included in the study, 305 (79.6%) in group A and 78 (20.4%) in group B. Patients in group A were significantly younger (60.0 versus (vs) 66.5 years (p = 0.03)). The professionally active population was larger in group A (44.3% vs 24.4%). There were significantly more non-French-speaking people in group B (16.7% vs 6.6%, p < 0.01). Most patients from group A had individual accommodation (92.8% vs 74.4%, p < 0.01). Contact with a relative was the main transmission risk factor in both groups (24.6% vs 33.3%, p = 0.16). Recent travel and large gathering were found only in group A. The proportion of people living in disadvantaged conditions, such as homeless people or people living in social housing, was significantly higher in group B (11.5% vs 4.3%, p = 0.03) as was the proportion of institutionalized individuals (14.1% vs 3.0%, p < 0.01).
Conclusions
In this study conducted in patients hospitalized for COVID-19 in Paris, France, the likelihood of being infected despite the lockdown was higher for people who do not speak French, live in social housing, are homeless or institutionalized. Targeted measures have to be implemented to protect these populations.
Similar content being viewed by others
Background
The COVID-19 pandemic is an unprecedented public health challenge. In the past century, dramatic changes in demographics, urbanization and globalization have facilitated the spread of infectious diseases across countries and continents. In a matter of weeks, the COVID-19 pandemic devastated communities worldwide, requiring a multinational governmental, healthcare system and public health response [1].
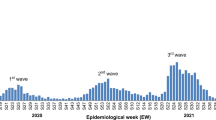
The outbreak of COVID-19 was declared as a global pandemic on March 11, 2020 and by May 30, 2020, about 6 million positive cases were registered worldwide [2]. As in many countries facing the pandemic, restrictive measures were progressively implemented in France from February 2020, such as a ban on public gatherings in enclosed spaces, closure of nurseries, schools and universities, physical distancing, and the use of face masks. Due to the continuously increasing incidence despite all the above measures and in order to help the healthcare system cope with the ever higher number of patients, the French Government declared, on March 17, a general population lockdown, as well as travel restrictions in the European Union and border closure of the Schengen area. The entire French population was in strict lockdown until May 11.
The efficacy of lockdown in containing the pandemic has been predicted by mathematical modeling [3]. Lockdown has also been reported to reduce the number of new cases in countries that implemented it [4] and to decrease the spread of COVID-19 in areas where there was general lockdown of the entire population, such as Wuhan in China and Asian countries [5]. The efficacy of lockdown is especially noticed around 10 days from its implementation and continues to grow until 3 weeks [4].
However, the impact of lockdown on the sociodemographic characteristics of individuals infected with SARS-CoV-2 has not been well evaluated. It is known that socioeconomic position is a determinant of infectious diseases [6]. The more disadvantaged people are probably more likely to present with main risk factors for developing COVID-19. Therefore, it is capital to consider socioeconomic characteristics to identify the high-risk groups for transmission of COVID-19, especially during the lockdown [6].
The aim of this study was to describe the changes in sociodemographic characteristics of patients hospitalized for COVID-19 in a University Hospital in Paris and to compare the transmission risk factors of COVID-19 before and during lockdown in France.
Methods
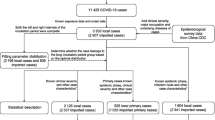
Study design and population
In this observational, retrospective, single-center study, we included all confirmed cases of COVID-19 between February 26 and May 11, 2020 admitted to the Infectious Diseases Department of Bichat-Claude Bernard University Hospital in Paris, France. All enrolled patients were diagnosed by positive reverse-transcription polymerase chain reaction for SARS-CoV-2 and/or typical chest computerized tomography characteristics. The study population was divided into 2 groups: group A of patients infected before lockdown, and group B of patients considered to be infected during lockdown. A maximum incubation period of 14 days was considered as suggested by previous studies [7, 8]. Therefore, group A consisted of patients with onset of infection between February 26 and March 31, 2020. Group B consisted of patients complaining of initial signs from April, 1 until May 11, 2020.
Outcomes and variables
The sociodemographic characteristics of patients hospitalized for COVID-19 before and during lockdown and the change in transmission risk factors between the 2 groups were collected. Sociodemographic data included age, gender, nationality, spoken language, occupation, healthcare insurance, type of household, and number of household members.
The potential transmission risk groups were assessed for each patient and classified in 8 categories as follows: (1) travel in an endemic international zone or in a cluster zone in France (city of Mulhouse, Oise department, Morbihan department); (2) unusual recent large gathering; (3) profession considered at risk (healthcare worker, caregiver, or public transport agent); (4) recent contact with a relative at high risk of infection (such as healthcare worker), presenting signs of infection or with confirmed COVID-19; (5) disadvantaged conditions (collective housing and homeless people); (6) nosocomial exposure (hospitalization and hemodialysis session); (7) institutionalized (elderly people and disabled persons); (8) not belonging to these transmission risk groups. Patients could belong to multiple transmission risk groups.
Data collection and analysis
Data collection was done using computerized medical records (Orbis® software). We retrospectively analysed the medical charts records of every patient during hospitalization.
A standardized and anonymized questionnaire was used in order to screen the charts and verify the diagnosis based on the inclusion criteria, the onset of infection and to collect the different sociodemographic characteristics and potential transmission risk factors in every patient; the questionnaire was filled and revised by two medical physicians for validation.
Statistical analyses were performed using Stata Version 12.0. Continuous variables were described by median and interquartile ranges, whereas categorical variables were represented by numbers and percentages. Student’s t-test was used to compare continuous variables. The Chi-2 test or Fisher exact test was used to compare categorical variables according to the distribution and headcounts of variables. A p-value < 0.05 was considered statistically significant.
Results
Sociodemographic characteristics of patients and transmission risk groups before and during lockdown are reported in Table 1. Sociodemographic characteristics and transmission risk factors before and during lockdown.
Sociodemographic characteristics
Three hundred and eighty-three patients were included in the study, 305 (79.6%) in group A and 78 (20.4%) in group B. Patients in group A were significantly younger, with a median age of 60.0 years old (IQR 39–81) versus (vs) 66.5 years old (IQR 43–90) in group B (p = 0.03). Occupation was significantly different between the 2 groups (p < 0.01). The professionally active population was indeed larger in group A (44.3% vs 24.4%), while the percentage of retirees was higher in group B (46.2% vs 32.8%). However, unemployed people were equally distributed in the 2 groups (13.1% vs 14.1%). Patients were mainly of French nationality, 61.6 and 59.0% in groups A and B, respectively. The proportion of French, European, and non-European citizens was equally distributed in the 2 groups (p = 0.65). However, there were significantly more non-French-speaking people in group B compared to group A (16.7% vs 6.6%, p < 0.01). Regarding housing, most patients (92.8%) from group A had individual accommodation vs 74.4% in group B, whereas there were more people living in social housing (6.4% vs 3.3%), homeless people (5.1% vs 1.0%), and institutionalized individuals (14.1% vs 3.0%) in group B (p < 0.01). Healthcare coverage was not significantly different between the two groups, with 5.9 and 7.7% of the population with no health insurance in groups A and B, respectively (p = 0.60).
Transmission risk groups
Contact with a relative as defined above was the predominant factor reported regardless of the period of infection (24.6% vs 33.3%, p = 0.16). Recent travel was only found in group A (9.8% vs 0.0%, p < 0.01), as was attendance at a recent large gathering (3.3% vs 0.0%, p = 0.22). The proportion of people with a profession considered at risk was equally distributed in the 2 groups (11.1% vs 9.0%, p = 0.79). In group B, the proportion of people living in disadvantaged conditions was significantly higher (11.5% vs 4.3%, p = 0.03) as was the proportion of institutionalized patients (14.1% vs 3.0%, p < 0.01). The nosocomial infection rate was the same in the 2 groups (11.5 and 11.5%, p = 0.99). Not belonging to a transmission risk group was more frequent in group A (39.3% vs 20.5%, p < 0.01).
Discussion
In this study, lockdown effectively reduced the number of new infections, with 80% of hospitalized patients being infected before its implementation. The same result has been observed in other countries both in Asia and Europe [5, 9] and reflects a high level of adherence to lockdown in these populations. A recent observation comparing countries from all over the world demonstrated a significant reduction in COVID-19 new cases in countries that implemented a general lockdown comparing to those that did not [4]. In our study, the protective effect of lockdown was particularly notable in younger, professionally active people living in individual accommodation, probably because of the major effect of lockdown on their day-to-day life.
However, our results indicate that some populations remained at risk of infection despite lockdown. First, ethnic minorities represented one-third of the patients hospitalized with COVID-19 in both periods and individuals not speaking French were at higher risk of infection during lockdown. In fact, pandemics rarely affect all people in a uniform way such as in the Black Death in the fourteenth century in which the highest number of deaths was observed among the poorest populations. Inequitable conditions and response to COVID-19 are also being seen in many countries [10]. Previous studies in the United-Kingdom have reported a higher risk of COVID-19 infection in black and Asian people than in white people [11, 12]. Ethnic minorities may have limited access to information from health authorities and less knowledge about the disease. This misinformation and miscommunication may lead ignorance of government health warning and thus to inappropriate behaviors [10, 13, 14]. Second, people living in social housing and homeless people were more likely to be infected during lockdown. A higher risk of infection in more deprived areas has also been reported in previous studies [11, 12]. A seroprevalence study conducted by Médecins Sans Frontières in food distribution sites, emergency shelters, and workers’ residences in Paris and its suburbs in June 2020 revealed that COVID-19 seropositivity reached 52%, with a strong association with overcrowding [15]. The limited access to COVID-19 screening tests and health services affects more profoundly the poorest populations especially during times of crisis [10]. In many studies, social features of health such as poverty, homelessness and ethnicity are proven to have considerable effect on COVID-19 transmission and outcomes. A higher risk of viral transmission is noted in homeless families because of their crowded living spaces and the absence of efficient social distancing in this disadvantaged conditions [10, 14, 16, 17].
In addition, individuals infected during lockdown were older and included more retirees and institutionalized persons. This population is more dependent and requires constant care, leading to a risk of infection by caregivers [18]. Implementation of social distancing is challenging in crowded long-term care facilities with shared common areas and low preparedness for infection control [19]. Therefore, long-term care facilities should monitor actively and rapidly isolate potentially infected patients as well as healthcare workers and limit access to visitors during the escalating COVID-19 outbreak among their vulnerable patients [20].
In our study, the number of individuals without any identified risk factor for transmission was high, and even higher before lockdown, when the virus was circulating and the general population was unaware of its route of transmission.
Our patients were mostly infected by a relative before and during lockdown. Mathematical modeling of the effect of lockdown in Italy showed that even with strict adherence to lockdown, transmission will still occur within households [3]. Physical distancing is hardly applicable at home, especially in large households but a rapidly respected quarantine at home by the index patient is still useful to prevent COVID-19 transmission within a household [21].
The risk of infection associated with traveling was reduced by travel restrictions and border closures, and that associated with public meetings and events was reduced by a ban on mass gatherings. Nosocomial and workplace infections remained stable over the two periods, other measures such as the use of personal protective equipment having been implemented before lockdown.
This study identifies specific vulnerable populations at high risk of COVID-19 despite lockdown. However, our results should be interpreted with caution given the retrospective design of the study and may not be similar in other settings.
Conclusion
The lockdown in France effectively contained the COVID-19 outbreak. However, ethnic minorities, vulnerable populations, the elderly, and institutionalized people remained at risk of infection during lockdown. Specific and targeted public health measures have to be implemented to prevent the spread of COVID-19 in these populations. The efficacy of lockdown should also be viewed in light of the collateral effect of prolonged lockdown which may exacerbate socioeconomic inequalities and increase poverty.
Availability of data and materials
The dataset used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- COVID-19:
-
Coronavirus Disease-19
- SARS-CoV-2:
-
Severe Acute Respiratory Syndrome-Coronavirus-2
- Vs:
-
versus
References
Roberts JD, Tehrani SO. Environments, behaviors, and inequalities: reflecting on the impacts of the influenza and coronavirus pandemics in the United States. Int J Environ Res Public Health. 2020;17(12):4484. https://doi.org/10.3390/ijerph17124484.
Adil MT, Rahman R, Whitelaw D, Jain V, Al-Taan O, Rashid F, et al. SARS-CoV-2 and the pandemic of COVID-19. Postgrad Med J. 2021;97(1144):110–6. https://doi.org/10.1136/postgradmedj-2020-138386.
Sjödin H, Wilder-Smith A, Osman S, Farooq Z, Rocklöv J. Only strict quarantine measures can curb the coronavirus disease (COVID-19) outbreak in Italy, 2020. Euro Surveill Bull Eur Sur Mal Transm Eur Commun Dis Bull. 2020;25(13).
Alfano V, Ercolano S. The efficacy of lockdown against COVID-19: a cross-country panel analysis. Appl Health Econ Health Policy. 2020;18(4):509–17. https://doi.org/10.1007/s40258-020-00596-3.
Lau H, Khosrawipour V, Kocbach P, Mikolajczyk A, Schubert J, Bania J, et al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med. 2020;27(3).
Khalatbari-Soltani S, Cumming RG, Delpierre C, Kelly-Irving M. Importance of collecting data on socioeconomic determinants from the early stage of the COVID-19 outbreak onwards. J Epidemiol Community Health. 2020:jech-2020-214297.
Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382(13):1199–207. https://doi.org/10.1056/NEJMoa2001316.
Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172(9):577–82. https://doi.org/10.7326/M20-0504.
Moris D, Schizas D. Lockdown during COVID-19: the Greek success. Vivo Athens Greece. 2020;34(3 Suppl):1695–9.
Ahmed F, Ahmed N, Pissarides C, Stiglitz J. Why inequality could spread COVID-19. Lancet Public Health. 2020;5(5):e240. https://doi.org/10.1016/S2468-2667(20)30085-2.
de Lusignan S, Dorward J, Correa A, Jones N, Akinyemi O, Amirthalingam G, et al. Risk factors for SARS-CoV-2 among patients in the Oxford Royal College of general practitioners research and surveillance Centre primary care network: a cross-sectional study. Lancet Infect Dis. 2020;15.
Niedzwiedz CL, O’Donnell CA, Jani BD, Demou E, Ho FK, Celis-Morales C, et al. Ethnic and socioeconomic differences in SARS-CoV-2 infection: prospective cohort study using UK Biobank. BMC Med. 2020;18(1):160.
Alsan M, Stantcheva S, Yang D, Cutler D. Disparities in Coronavirus 2019 Reported Incidence, Knowledge, and Behavior Among US Adults. JAMA Netw Open. 2020;3(6):e2012403.
Coetzee BJ, Kagee A. Structural barriers to adhering to health behaviours in the context of the COVID-19 crisis: considerations for low- and middle-income countries. Glob Public Health. 2020;11:1–10.
Roederer T, Mollo B, Vincent C, Nikolay B, Llosa AE, Nesbitt R, et al. Seroprevalence and risk factors of exposure to COVID-19 in homeless people in Paris, France: a cross-sectional study. Lancet Public Health. 2021;6(4):e202–9. https://doi.org/10.1016/S2468-2667(21)00001-3.
Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med. 2020;8(7):659–61. https://doi.org/10.1016/S2213-2600(20)30234-4.
Tsai J, Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Health. 2020;5(4):e186–7. https://doi.org/10.1016/S2468-2667(20)30053-0.
Grabowski DC, Mor V. Nursing home Care in Crisis in the wake of COVID-19. JAMA. 2020.
Lai C-C, Wang J-H, Ko W-C, Yen M-Y, Lu M-C, Lee C-M, et al. COVID-19 in long-term care facilities: an upcoming threat that cannot be ignored. J Microbiol Immunol Infect Wei Mian Yu Gan Ran Za Zhi. 2020;53(3):444–6. https://doi.org/10.1016/j.jmii.2020.04.008.
McMichael TM, Currie DW, Clark S, Pogosjans S, Kay M, Schwartz NG, et al. Epidemiology of Covid-19 in a long-term Care Facility in King County, Washington. N Engl J Med. 2020;382(21):2005–11. https://doi.org/10.1056/NEJMoa2005412.
Li W, Zhang B, Lu J, Liu S, Chang Z, Peng C, et al. Characteristics of household transmission of COVID-19. Clin Infect Dis Off Publ Infect Dis Soc Am. 2020;71(8):1943–6. https://doi.org/10.1093/cid/ciaa450.
Acknowledgements
We thank all the healthcare workers who have participated to this work.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
Author 1 (M.R) participated in the planning of the study, carried out data collection and drafted the manuscript. Author 2 (D.LP) participated in the planning of the study, carried out data analysis and participated in the writing of the manuscript. Author 3 (A.B) participated in the data collection, reviewing and editing of the manuscript. Author 4 (S.I), author 5 (M.P), author 6 (N.P), author 7 (H.T) and author 8 (FX.L) participated in the writing, reviewing and editing of the manuscript. Author 9 (Y.Y) participated in the planning of the study, the writing, reviewing and editing of the manuscript. Author 10 (L.D) carried out the planning of the study and participated in the data collection and analysis as well as the writing, reviewing and editing of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ‘Comité d’Evaluation de l’Ethique des projets de Recherche Biomédicale (CEERB) Paris Nord’ (Institutional Review Board -IRB 00006477- of HUPNVS, Paris 7 University, AP-HP) has reviewed and approved the research project including access to medical records and data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rahi, M., Le Pluart, D., Beaudet, A. et al. Sociodemographic characteristics and transmission risk factors in patients hospitalized for COVID-19 before and during the lockdown in France. BMC Infect Dis 21, 812 (2021). https://doi.org/10.1186/s12879-021-06419-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-021-06419-7