Abstract
Background
Cryptococcal antigen (CrAg) screening with fluconazole prophylaxis has been shown to prevent cryptococcal meningitis and mortality for people living with HIV (PLWH) with CD4 < 100 cells/mm3. While cryptococcal meningitis occurs in individuals with CD4 100–200 cells/mm3, there is limited evidence that CrAg screening predicts cryptococcal meningitis or mortality among this group with moderate immunosuppression. Current IDSA and WHO clinical guidelines recommend restricting CrAg screening to PLWH with CD4 < 100 cells/mm3.
Methods
We conducted a prospective cohort study of PLWH 18+ years who had not initiated ART in South Africa. We followed participants for 14 months to determine onset of cryptococcal meningitis or all-cause mortality. At study completion, we retrospectively tested stored serum samples for CrAg using an enzyme immunoassay (EIA). We calculated CD4-stratified incidence rates of outcomes and used Cox proportional hazards to measure associations between CrAg positivity and outcomes.
Results
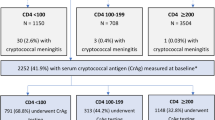
We enrolled 2383 PLWH, and 1309 participants had serum samples tested by CrAg EIA. The median CD4 was 317 cells/mm3 (interquartile range: 173–491 cells/mm3). By CD4 count at baseline, there were 209 individuals with a CD4 count of 100–200 cells/mm3 and available CrAg test results. Of these, four (1.9%) tested positive. Two of four (IR: 58.8 per 100 person-years) CrAg+ participants and 11 of 205 (IR: 5.6 per 100 person-years) CrAg- participants developed cryptococcal meningitis or died for an overall rate of death or cryptococcal meningitis that was 10.0-times higher for those who were CrAg+ (95% confidence interval: 2.2–45.3). Among those with CD4 < 100 cell/mm3 and CrAg EIA test results (N = 179), ten (5.6%) participants tested CrAg+. Among this group, seven of ten (IR: 137.6 per 100 person-years) CrAg+ participants and 26 of 169 (IR: 17.8 per 100 person-years) CrAg- participants developed cryptococcal meningitis or died, for a rate of death or cryptococcal meningitis that was 6.3-times higher for those who were CrAg+ (95% confidence interval: 2.7–14.6).
Conclusions
Although few PLWH with moderate immunosuppression screened CrAg positive, a positive CrAg test was predictive of increased risk of cryptococcal meningitis or death. Similar to those with a CD4 < 100 cell/mm3, systematic CrAg screening may reduce morbidity and mortality in PLWH with CD4 100–200 cells/mm3.
Similar content being viewed by others
Background
Despite a global increase in access to antiretroviral therapy (ART), cryptococcal meningitis continues to be a significant cause of morbidity and mortality among people living with HIV (PLWH) [1]. The majority of cryptococcal meningitis cases occur in low- and middle-income countries, particularly in sub-Saharan Africa [2]. Serum screening for cryptococcal antigen (CrAg) and subsequent prophylaxis for those who screen positive limits the burden of disease by preventing the progression from cryptococcal antigenemia to cryptococcal meningitis or death [1, 3]. Asymptomatic cryptococcal antigenemia is also associated with early all-cause mortality in PLWH in sub-Saharan Africa [4].
According to current World Health Organization (WHO) and Infectious Disease Society of America (IDSA) guidelines, screening for CrAg is reserved for PLWH who have a CD4 count less than 100 cells/mm3 [1, 5]. However, the WHO also states that screening may be considered at a higher CD4 threshold of < 200 cells/mm3, without specifying the specific circumstances in which to increase the threshold for CrAg screening [1].
South Africa is one of many countries in sub-Saharan Africa that now incorporates CrAg screening into its national HIV guidelines for people with CD4 < 100 cells/mm3 [6]. A previous meta-analysis established a pooled CrAg positivity prevalence of 2.0% for PLWH with CD4 100–200 cells/mm3 [7], and recent data from sub-Saharan Africa suggests that at least 9% of cases of cryptococcal meningitis present in individuals with CD4 > 100 cells/mm3 [8, 9]. We sought to characterize the association of CrAg positivity by the standard of care serum enzyme immunoassay (EIA) with cryptococcal meningitis or death among PLWH with CD4 100–200 cells/mm3.
Methods
Study design
We enrolled adults seeking HIV testing who presented to the iThembalabantu People’s Hope Clinic, which provides free HIV care for over 10,000 residents of the Umlazi township in KwaZulu-Natal, South Africa. The study included participants who were ART-naïve, newly diagnosed with HIV, English or Zulu speaking, and older than 17 years of age. The full design of the parent study has been previously described [10]. We excluded participants who were pregnant as well as participants who had received antifungal therapy in the previous three months. We obtained study approval by the University of Washington’s Institutional Review Board and the University of KwaZulu-Natal’s Medical Research Ethics Committee.
Data collection
At the time of enrollment, participants received rapid HIV testing. HIV-infected participants met with a research nurse, who obtained serum samples and completed a medical history and symptom questionnaire. Blood samples were obtained, CD4 count was tested using FACSCalibur flow cytometry at an offsite laboratory, and serum samples were stored. HIV testing and follow up treatment was in accordance with South African ART treatment guidelines [11]. Participants also underwent the WHO 4-symptom screen for tuberculosis (TB). Upon the completion of a 12-month follow-up period, we retrospectively tested stored serum samples for CrAg using the ALPHA CrAg EIA test system developed by Immy Diagnostics (Norman, Oklahoma, USA).
Outcomes
We followed participants for 12 months following HIV diagnosis, and collected data at regular intervals. Our primary outcomes of interest were all-cause mortality, cryptococcal meningitis, and a combined outcome of mortality or cryptococcal meningitis. For participants lost to follow-up, we searched the national South African death registry to obtain mortality outcomes. Outcomes that occurred up to 14 months following enrollment were included and any outcomes ascertained after 14 months were excluded from the analysis.
Data analysis
We calculated the incidence of study outcomes and assessed the relationship between serum CrAg positivity (positive compared to negative or indeterminate) and outcomes using a time-to-events analysis (Cox proportional-hazards regression and Kaplan-Meier). Incidence rates (IR) were calculated as the number of outcomes divided by the person-time at risk (person-years) up to 14 months after enrollment, accounting for loss to follow-up. Analyses were stratified by CD4 count at enrollment (< 100 or 100–200 cells/mm3).
Results
In total, we enrolled 2383 adults from September 2013 to November 2017 (Table 1). The majority (57.6%) of participants were female, and the mean age was 33.1 years (standard deviation: 9.3 years). 54.6% of participants did not complete high school, and 43% of participants were employed. Of the 2360 participants who reported income data, 75.6% had a monthly income of less than 2000 South African rand per month (<USD $150/month).
The median CD4 count was 317 cells/mm3 (interquartile range: 173–491 cells/mm3). Three hundred and twenty-five participants (13.6%) had CD4 < 100 cells/mm3, 354 (14.9%) participants had CD4 100–200 cells/mm3, and 1656 participants (69.5%) had CD4 > 200 cells/mm3. CD4 data were not available for 48 participants. Five participants had previously tested positive for CrAg, and three of these five participants previously received treatment with fluconazole.
At enrollment, participants frequently reported symptoms associated with cryptococcal meningitis, including fatigue (43.4%), headache for greater than 24 h (25.5%), fever (24.5%), neck stiffness (16.2%), difficulty walking (13.1%), vision changes (9.3%), and seizure within the last seven days (1.0%). Thirty-six participants (1.5%) had received fluconazole preventative therapy at one-year follow-up.
Serum EIA testing was only available from November 2013 to August 2016, and thus not all participants were able to receive serum EIA testing. In total, 1309 participants (54.9%) received EIA testing, and of those 15 (1.1%) were CrAg positive. Participants who did not receive EIA testing still received other point-of-care CrAg screening in accordance with the larger study protocol. There were no statistically significant differences in age, gender, or CD4 count between the group that received EIA testing and the group that did not. CrAg testing was positive in one participant with CD4 > 200 cells/mm3, four participants with CD4 100–200 cells/mm3, and ten participants with CD4 < 100 cells/mm3.
Among participants with CD4 < 100 cells/mm3 (N = 179), four of ten (IR: 64.7 per 100 person-years) CrAg positive participants and 26 of 169 (IR: 19.7 per 100 person-years) CrAg negative participants died, and four of ten (IR: 78.6 per 100 person-years) CrAg positive participants and 1 of 169 (IR: 0.7 per 100 person-years) CrAg negative participants developed cryptococcal meningitis. In aggregate, seven of ten (IR: 137.6 per 100 person-years) CrAg positive participants and 26 of 169 (IR: 17.8 per 100 person-years) CrAg negative participants died or developed cryptococcal meningitis (Fig. 1). In this group, CrAg positivity was strongly associated with increased risk of meningitis or death (HR: 6.3, 95% confidence interval [CI]: 2.7–14.6, p < 0.001) (Table 2).
In those with CD4 100–200 cells/mm3 (N = 209), two of four (IR: 58.8 per 100 person-years) CrAg positive participants and 11 of 205 (IR: 5.6 per 100 person-years) CrAg negative participants died, and none developed cryptococcal meningitis. In aggregate, two of four (IR: 58.8 per 100 person-years) CrAg positive participants and 11 of 205 (IR: 5.6 per 100 person-years) CrAg negative participants died or developed cryptococcal meningitis. CrAg positivity was associated with an increased hazard of death or cryptococcal meningitis (HR 10.0, CI: 2.2–45.3, p = 0.003).
Discussion
In this cohort of PLWH in sub-Saharan Africa, serum CrAg positivity was associated with increased risk of death or cryptococcal meningitis among participants with CD4 100–200 cells/mm3 as well as those with CD4 < 100 cells/mm3. The prevalence of CrAg positivity among those with CD4 100–200 cells/mm3 was 1.9%, which is consistent with prior studies [7]. There was one participant who was CrAg positive who had CD4 > 200 cells/mm3. This participant did not die or develop cryptococcal meningitis.
Our findings build on previous studies, which have individually reported the prevalence of CrAg and cryptococcal meningitis or death for PLWH with CD4 100–200 cells/mm3, but not their association. One study located in Uganda previously found that 9% of cryptococcal meningitis cases in PLWH presented in patients with a CD4 > 100 cells/mm3 [9], and another study from South Africa found a prevalence of 12.5% in this group [8].
While PLWH with CD4 < 100 cells/mm3 who are CrAg positive are most likely to have adverse outcomes, our results suggest CrAg screening may be beneficial for PLWH who have CD4 100–200 cells/mm3. Many participants reported symptoms suggestive of cryptococcal meningitis, such as neck stiffness, vision changes, and persistent headache; testing for serum CrAg could better characterize the pre-test probability of cryptococcal meningitis in patients presenting with relatively non-specific symptoms. Given that we only identified one CrAg positive participant with CD4 > 200 cells/mm3 who did not die or develop cryptococcal meningitis, we did not find any evidence to support raising the screening threshold to CD4 > 200 cells/mm3 in this setting.
Laboratory-based lateral flow assay (LFA) CrAg screening for PLWH with CD4 < 100 cells/mm3 has been shown to be life-saving and cost-effective when implemented in Uganda and South Africa [12, 13]. Despite a relatively low CrAg prevalence in PLWH with CD4 100–200 cells/mm3, using a low-cost screening test and prophylactic fluconazole would likely be cost-effective when compared to the high costs of cryptococcal meningitis and/or mortality. A sensitivity analysis of CrAg screening in PLWH with CD4 < 100 cells/mm3 demonstrated that CrAg screening was cost-effective as long as the CrAg prevalence remained greater than .5% [13]. Future studies should seek to evaluate the effect of fluconazole therapy in PLWH with CD4 100–200 cells/mm3, and model the costs associated with raising the CrAg screening threshold.
Our study took place in South Africa, a country with a high incidence of meningitis [6]. This likely affected the yield of screening in our cohort. Increasing the threshold for CrAg screening to 200 cells/mm3 may be less appropriate in regions with a lower incidence of cryptococcal meningitis, but more research is needed in different geographical areas.
Our study is limited by the small number of CrAg positive participants and person-time in which to assess outcomes. We used a combined outcome of death or confirmed cryptococcal meningitis in our study, although we suspect many of the deaths identified through searching the national registry could have been due to death from cryptococcal meningitis despite the participants not presenting for further evaluation. PLWH are at increased risk of multiple opportunistic infections, not just cryptococcal meningitis. In particular, KwaZulu-Natal has a high rate of TB and HIV/TB co-infection [14]. While we did assess TB symptoms at the time of enrollment, we were unable to reliably assess for development of TB-related mortality. Overall, our study findings are limited by the inability to confirm cause of death in all participants. In selecting the gold standard for our study, we opted to use the serum EIA test based on its proven accuracy for CrAg screening.
Conclusions
In the subset of newly identified PLWH with a CD4 100–200 cells/mm3 in South Africa, serum CrAg positivity was observed in almost 2% of participants, and a positive CrAg result was strongly associated with an increased risk of cryptococcal meningitis or death during a 12-month follow-up period. Raising the threshold for CrAg screening to 200 cells/mm3 could help reduce morbidity and mortality in PLWH in cryptococcus-endemic regions.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ART:
-
Antiretroviral Therapy
- CI:
-
Confidence Interval
- CrAg:
-
Cryptococcal antigen
- EIA:
-
Enzyme Immunoassay
- HIV:
-
Human immunodeficiency virus
- HR:
-
Hazard Ratio
- IDSA:
-
Infectious Diseases Society of America
- IR:
-
Incidence Rate
- LFA:
-
Lateral flow assay
- PLWH:
-
People living with HIV
- TB:
-
Tuberculosis
- USD:
-
United States Dollar
- WHO:
-
World Health Organization
References
Diagnosis THE, Cryptococcal MOF, Adults DINH. The Diagnosis, Prevention and Management of Cryptococcal Disease in Hiv-Infected Adults, Adolescents and Children Supplement To the 2016 Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing Hiv Infection 2018.
Stover J, Low A, Larke N, Drouin O, B-Lajoie M-R, Gavriilidis G, et al. Incidence of opportunistic infections and the impact of antiretroviral therapy among HIV-infected adults in Low- and middle-income countries: a systematic review and meta-analysis. Clin Infect Dis. 2016;62(12):1595–603.
Temfack E, Bigna JJ, Luma HN, Spijker R, Meintjes G, Jarvis JN, et al. Impact of routine Cryptococcal antigen screening and targeted preemptive fluconazole therapy in antiretroviral-naive human immunodeficiency virus-infected adults with CD4 cell counts <100/muL: a systematic review and meta-analysis. Clin Infect Dis. 2019 Feb;68(4):688–98.
Liechty CA, Solberg P, Were W, Ekwaru JP, Ransom RL, Weidle PJ, et al. Asymptomatic serum cryptococcal antigenemia and early mortality during antiretroviral therapy in rural Uganda. Tropical Med Int Health. 2007 Aug;12(8):929–35.
Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2010 Feb;50(3):291–322.
Rajasingham R, Smith RM, Park BJ, Jarvis JN, Govender NP, Chiller TM, et al. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis [Internet]. 2017/05/05. 2017 Aug;17(8):873–881. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28483415.
Ford N, Shubber Z, Jarvis JN, Chiller T, Greene G, Migone C, et al. CD4 cell count threshold for Cryptococcal antigen screening of HIV-infected individuals: a systematic review and meta-analysis. Clin Infect Dis. 2018;66(Suppl 2):S152–9.
Ndayishimiye E, Ross AJ. An audit of the screen-and-treat intervention to reduce cryptococcal meningitis in HIV-positive patients with low CD4 count. African J Prim Heal Care Fam Med. 2018;10(1):1–7.
Tugume L, Rhein J, Hullsiek KH, Mpoza E, Kiggundu R, Ssebambulidde K, et al. HIV-associated Cryptococcal meningitis occurring at relatively higher CD4 counts. J Infect Dis. 2019 Feb;219(6):877–83.
Drain PK, Hong T, Krows M, Govere S, Thulare H, Wallis CL, et al. Validation of clinic-based cryptococcal antigen lateral flow assay screening in HIV-infected adults in South Africa. Sci Rep. 2019 Feb;9(1):2687.
Meintjes G, Moorhouse MA, Carmona S, Davies N, Dlamini S, van Vuuren C, et al. Adult antiretroviral therapy guidelines 2017. S Afr J HIV Med. 2017;18(1):1–24.
Rajasingham R, Meya DB, Greene GS, Jordan A, Nakawuka M, Chiller TM, et al. Evaluation of a national cryptococcal antigen screening program for HIV-infected patients in Uganda: a cost-effectiveness modeling analysis. PLoS One. 2019;14(1):e0210105.
Jarvis JN, Harrison TS, Lawn SD, Meintjes G, Wood R, Cleary S. Cost effectiveness of cryptococcal antigen screening as a strategy to prevent HIV-associated cryptococcal meningitis in South Africa. PLoS One. 2013;8(7):e69288.
Massyn N, Peer N, English R, Padarath A, Barron P, Day editors C. District health barometer 2015/16. Durban Heal Syst Trust 2016;
Acknowledgements
The authors would like to thank the members of the Drain TB/HIV Research Lab for their mentorship and editing support.
Funding
This work was supported by the Infectious Disease Society of America Education & Research Foundation and National Foundation for Infectious Diseases (PKD); Massachusetts General Hospital Executive Committee on Research (PKD); the Harvard University Center for AIDS Research [P30 AI060354] (PKD); and the National Institute of Allergy and Infectious Diseases [K23 AI108293] (PKD). The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health or other funding agencies. The funding bodies had no role in the design of the study, collection, analysis, and interpretation of data, or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
JW drafted and edited the manuscript. SG1 performed the primary data analyses. SG1 and PD provided substantial editing support for the manuscript. SG2, MM, CW supervised data collection and reporting, read and edited the manuscript. CC read and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All study participants provided written informed consent in English or Zulu. The study was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee (BF052/13) and the University of Washington Institutional Review Board (49563).
Consent for publication
Participants’ written consent for publication was obtained at the time of study enrollment.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wykowski, J., Galagan, S.R., Govere, S. et al. Cryptococcal antigenemia is associated with meningitis or death in HIV-infected adults with CD4 100–200 cells/mm3. BMC Infect Dis 20, 61 (2020). https://doi.org/10.1186/s12879-020-4798-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-020-4798-1