Abstract
Background
Invasive meningococcal disease (IMD) presenting with meningitis causes significant mortality and morbidity. Suppurative complications of serogroup B meningococcal sepsis are rare and necessitate urgent multidisciplinary management to mitigate long-term morbidity or mortality.
Case presentation
We present a rare case of invasive meningococcal disease in a 28-month old boy complicated by multiple abscess formation within a pre-existing antenatal left middle cerebral artery territory infarct. Past history was also notable for cerebral palsy with right hemiplegia, global developmental delay and West syndrome (infantile spasms). Two craniotomies were performed to achieve source control and prolonged antimicrobial therapy was necessary. The patient was successfully discharged following extensive multidisciplinary rehabilitation.
Conclusions
Longstanding areas of encephalomalacia in the left MCA distribution may have facilitated the development of multiple meningococcal serogroup B abscess cavities in the posterior left frontal, left parietal and left temporal lobes following an initial period of cerebritis and meningitis. A combination of chronic cerebral hypoperfusion and some degree of pre-existing necrosis in these areas, may also have facilitated growth of Neisseria meningitidis, leading ultimately to extensive cerebral abscess formation following haematogenous seeding during meningococcemia. In this case report we review similar cases of cerebral abscess or subdural empyema complicating serogroup B meningococcal meningitis.
Similar content being viewed by others
Background
Neisseria meningitidis is an opportunist Gram-negative pathogen and commensal of the nasopharynx and upper respiratory tract. Transmission is via aerosol, droplets or direct contact with infected respiratory secretions. The prevalence of asymptomatic carriage of all serotypes of N. meningitidis increases with age, from 5% in childhood to 20% in late teenage years [1]. There are 13 antigenically distinct serogroups of meningococci and most disease-associated strains belong to serogroups A, B, C, X, Y or W135. The incidence of meningococcal disease varies worldwide but is estimated at 0.3–3 cases per 100,000 in Europe and North America, with a predominance of serogroups B and C. Overall, the incidence of meningococcal disease continues to decline in countries where vaccines targeting serogroups C and more recently B, have been introduced [2].
Invasive meningococcal disease (IMD) presenting with meningitis causes significant mortality, with a 10% case fatality rate in the very young, and morbidity in up to 20% of survivors, predominantly neurological sequelae (seizures, cognitive impairment), visual and/or auditory impairment and amputation of necrotic digits and/or limbs [3]. By contrast, acute suppurative complications of N. meningitidis meningitis occur in less than 1% of cases and are rarely reported [4, 5]. We report the successful treatment of multiple cerebral abscesses associated with serogroup B meningococcal meningitis in a young infant with a prior cerebral infarct and complex medical history. The overall aims of presenting this case report are to increase awareness of the increased risk of cerebral complications of meningococcal sepsis in patients with previous intracerebral neurovascular events and to demonstrate the role of advances in molecular diagnostics, permitting PCR detection of N. meningitidis DNA despite preceding antimicrobial therapy.
Case presentation
A 28-month old boy presented with a 24-h history of lethargy, pyrexia, mottled peripheries and decreased responsiveness. Past history was notable for antenatal left middle cerebral artery (MCA) infarct, cerebral palsy with right hemiplegia, global developmental delay and West syndrome (infantile spasms). He was up-to-date with vaccinations. Epilepsy was poorly controlled with up to 30 seizures per day despite maintenance clobazam, lacosamide, sodium valproate and levetiracetam treatment.
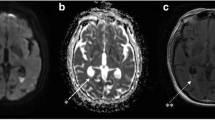
On examination he had neck stiffness and was haemodynamically unstable with persistent tachycardia and hypotension. He was coagulopathic (platelets 94 × 10 [6]/L, INR 2.5, fibrinogen 4.03 g/L, prothrombin time 16.8 s), with elevated white cell count (WCC) 28.9 × 10 [6]/L, neutrophilia (25.8 × 10 [6]/L), normal lymphocyte count (8.5 × 10 [6]/L) and c-reactive protein (CRP) 276 mg/L. He was transferred to the intensive care unit (day 0) where he required intubation, ventilation, fluid resuscitation and inotropic support. He was treated with intravenous (IV) ceftriaxone, vancomycin and aciclovir. Polymerase chain reaction (PCR) identified human metapneumovirus, parainfluenza type-3 and adenovirus in a nasal swab. Lumbar puncture demonstrated a macroscopic yellow appearance: WCC 142 (predominantly polymorphonuclear); glucose, 1.6 mmol/L; and protein, 5.46 g/L. No organisms were seen on Gram stain. Blood and cerebrospinal fluid (CSF) were culture negative (taken on antimicrobials) but PCR positive for N. meningitidis serogroup B. Antimicrobial treatment was rationalised to cefotaxime monotherapy. He subsequently became more encephalopathic with persistent pyrexia associated with rising blood WCC and CRP. Brain computed tomogram (CT) and magnetic resonance imaging (MRI) demonstrated multiple abscesses in the left MCA territory, cystic encephalomalacia of posterior left frontal, left parietal and left temporal lobes, and left hemispheric pial enhancement (Fig. 1a). Empiric treatment for cerebral abscess with IV meropenem, vancomycin and fluconazole was commenced.
a: Axial contrast-enhanced CT day 10 of illness reveals an extensive area of cystic encephalomalacia in the left middle cerebral artery territory with marginal enhancement. Pial enhancement is evident of the entire left cerebral hemisphere. There is longstanding ex vacuo dilatation of the left lateral ventricle and new mass effect with shift of the anterior falx to the right. b: Axial contrast-enhanced T1 MRI on day 21 after two neurosurgical interventions. The extensive left craniotomy, evacuation and debridement of the infected encephalomalacic tissue is evident with pronounced pial and leptomeningeal enhancement of the left cerebral hemisphere. There is discontinuity of the dura with overlying extradural fluid and air. An extra-ventricular drain tip is located in the anterior left lateral ventricle
A frameless stereotactic-guided endoscopic fenestration, drainage and washout of the cerebral abscesses was performed and a left external ventricular drain was sited (day 10). Further deterioration in neurological status necessitated an extensive fronto-temporal-parietal craniotomy with evacuation and debridement of residual collections and infected encephalomalacial tissue (day 16). Intraoperative fluid and parenchymal tissue was culture negative but PCR positive for N. meningitidis serogroup B and antimicrobial therapy was rationalised to meropenem monotherapy. A second craniotomy was performed for evacuation of a left frontal lobe abscess in the context of persistent swinging pyrexia (day 18). Intravenous linezolid was added for the treatment of a surgical site infection in the left parietal region, associated with a toxic shock-like syndrome. Intra-operative specimens were culture negative. The patient returned to theatre for repeat burrhole drainage of an intracerebral collection (day 20; Fig. 1b demonstrates clinical status post-operatively day 21). Intraoperative specimens were culture-negative again and were not sent for PCR analysis. He was discharged from ICU for extensive multidisciplinary rehabilitation (day 23). The patient was discharged home on day 40 to complete a further 6-weeks IV ceftriaxone. On outpatient follow-up, he is back to his baseline functioning status with no evidence of new neurological or auditory sequelae. Unfortunately, his seizures, which had disappeared in the immediate post-operative period, have since returned to their usual frequency.
Discussion & Conclusions
The present case is an example of a rare meningococcal complication with a positive outcome. Following the introduction of N. meningitidis serogroup C conjugate (MenC) vaccine in 2000, meningococcal B disease has been the predominant cause of IMD in Ireland [7]. In 2015, the age specific incidence rate (ASIR) for meningococcal B disease in children aged between 1 and 4 years was 3.87/100,000 with a case fatality rate of less than 5% [8]. Our patient was non-immune as vaccination against meningococcal serogroup B would not have been offered to his age-cohort at the time of his presentation.
His complex pre-admission intracerebral neuropathology likely increased the risk of meningococcal abscess formation. We hypothesise that areas of encephalomalacia in the left MCA distribution (Fig. 1a, b) may have facilitated the development of multiple meningococcal serogroup B abscess cavities in the posterior left frontal, left parietal and left temporal lobes following an initial period of cerebritis and meningitis. A combination of chronic cerebral hypoperfusion and some degree of pre-existing necrosis in these areas, may also have facilitated growth of N. meningitidis, leading ultimately to extensive cerebral abscess formation following haematogenous seeding during meningococcemia. West syndrome is not known to confer an increased risk of meningitis [9].
Similar cases of cerebral abscess or subdural empyema complicating serogroup B meningococcal meningitis are rare (Additional file 1). Rothbaum et al. reported successful antimicrobial treatment and surgical drainage of cerebral abscess in an area of left temporal lobe hypoperfusion in a previously healthy 5-month old with serogroup B meningococcal septic shock [5]. And more recently, multiple cerebral abscesses were reported in association with serogroup B meningococcal meningitis in a five-day old neonate in India [6].
With regard to learning outcomes from the present case, we remain vigilant to the increased risk of cerebral complications of meningococcal sepsis in all children, but particularly those with previous intracerebral neurovascular events, and note again that diagnosis was facilitated by advances in molecular microbiology permitting PCR detection of N. meningitidis DNA despite 16 days of preceding antimicrobial therapy [8]. A previous study from this centre, reviewing 266 cases of adult and paediatric IMD over 8 years (2001-2008), demonstrated that 63% of cases of meningococcal blood stream infection and 69% of cases of meningitis were diagnosed by PCR alone, emphasising the necessity for clinicians to utilise rapid PCR testing where IMD is suspected, to reduce mortality and morbidity [10]. We also continue to promote meningococcal vaccination as a public health initiative.
Availability of data and materials
No additional data are available.
Abbreviations
- CRP:
-
C-reactive protein
- CSF:
-
Cerebrospinal fluid
- CT:
-
Computed tomogram
- IMD:
-
Invasive meningococcal disease
- IV:
-
Intravenous
- MCA:
-
Middle cerebral artery
- MRI:
-
Magnetic resonance imaging
- PCR:
-
Polymerase chain reaction
- WCC:
-
White cell count
References
Christensen H, May M, Bowen L, Hickman M, Trotter CL. Meningococcal carriage by age: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10:853–61.
Dwilow R, Fanella S. Invasive meningococcal disease in the 21st century – an update for the clinician 2015. Curr Neurol Neurosci Rep. 2015;15:2.
Bilukha OO, Rosenstein N; Natonal Center for Infectious Diseases, Centers for Disease Control and Prevention (CDC). Prevention and control of meningococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2005;54(RR-7):1–21.
Rothbaum E, Nicholson O, Prince A. Cerebral abscess associated with meningococcal meningitis. Pediatr Infect Dis J. 2006;25(8):754–6.
Ray S, Riordan A, Tawil M, Mallucci C, Jauhari P, Solomon T, Kneen R. Subdural empyema caused by Neisseria meningitidis: a case report and review of the literature. Pediatr Infect Dis J. 2016;35(10):1156–9.
Basani L, Aepala R. Neisseria Meningitidis causing multiple cerebral abscesses in early neonatal period: case report and review of literature. J Clin Diagn Res. 2017;11(7):SD01–3.
Maoldomhnaigh.C Ó, Drew RJ, Gavin P, Cafferkey M, Butler KM. Invasive meningococcal disease in children in Ireland, 2001–2011. Arch Dis Child. 2016;101:1125–9.
Irish National Immunisation Guidelines. Chapter 13. Updated September 2016. Available at: https://www.hse.ie/eng/health/immunisation/hcpinfo/guidelines/chapter13.pdf. Accessed: 13.06.2018.
Wheless JW, Gibson PA, Rosbeck KL, Hardin M, O'Dell C, Whittemore V, Pellock JM. Infantile spasms (West syndrome): update and resources for pediatricians and providers to share with parents. BMC Pediatr. 2012;25(12):108.
Drew RJ. Ó Maoldomhnaigh C, Gavin PJ, O' Sullivan N, Butler KM, Cafferkey M. the impact of meningococcal polymerase chain reaction testing on laboratory confirmation of invasive meningococcal disease. Pediatr Infect Dis J. 2012;31(3):316–8.
Acknowledgements
The authors thank the staff of the Microbiology Laboratory at Temple Street Children’s University Hospital, Dublin 1, Ireland and the Irish Meningitis and Sepsis Reference Laboratory (IMSRL), Temple Street Children’s University Hospital, Dublin 1, Ireland. Special thanks also to Deirdre Butler, secretary to the Department of Infectious Diseases, Temple Street Children’s University Hospital, Dublin 1, Ireland, for her invaluable administrative support.
Funding
No funding source received.
Author information
Authors and Affiliations
Contributions
All authors contributed to this work, read and approved the manuscript. COC, AC, JC, CH, and PJG wrote the manuscript; ET provided radiology images and provided valuable feedback. COC, AC, ET, JC, CH, and PJG were directly involved in the care of the patient.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Yes, signed parental consent was obtained. Available on request.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1: Table S1.
Previous published papers describing meningococcal abscess formation
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
O’Connor, C., Collins, A., Twomey, E. et al. A case report of multiple cerebral abscess formation complicating serogroup B Neisseria meningitidis meningitis. BMC Infect Dis 19, 863 (2019). https://doi.org/10.1186/s12879-019-4509-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-019-4509-y