Abstract
Background
Streptococcus pneumoniae is a commensal of the human upper respiratory tract and a major cause of morbidity and mortality worldwide. This paper presents the distribution of serotypes and antimicrobial resistance in commensal S. pneumoniae strains cultured from healthy carriers older than four years of age in nine European countries.
Methods
Nasal swabs from healthy persons (age between 4 and 107 years old) were obtained by general practitioners from each country from November 2010 to August 2011. Swabs were cultured for S. pneumoniae using a standardized protocol. Antibiotic resistance was determined for isolated S. pneumoniae by broth microdilution. Capsular sequencing typing was used to identify serotypes, followed by serotype-specific PCR assays in case of ambiguous results.
Results
Thirty-two thousand one hundred sixty-one nasal swabs were collected from which 937 S. pneumoniae were isolated. A large variation in serotype distribution and antimicrobial resistant serotypes across the participating countries was observed. Pneumococcal vaccination was associated with a higher risk of pneumococcal colonization and antimicrobial resistance independently of country and vaccine used, either conjugate vaccine or PPV 23).
Conclusions
Serotype 11A was the most common in carriage followed by serotypes 23A and 19A. The serotypes showing the highest resistance to penicillin were 14 followed by 19A. Serotype 15A showed the highest proportion of multidrug resistance.
Similar content being viewed by others
Background
Streptococcus pneumoniae (pneumococcus) is a commensal of the human upper respiratory tract [1] and a major cause of morbidity and mortality worldwide. Pneumococcal disease has various manifestations including otitis media, pneumonia, septicemia and meningitis [2]. Incidence of the disease is highest at extremities of life: in very young children and in the elderly. Based on capsular polysaccharide chemistry and immunogenicity, over 90 distinct capsular types (serotypes) have been identified so far [3].
Two types of pneumococcal vaccines are commercially available: a pneumococcal polysaccharide vaccine (PPV) and pneumococcal conjugate vaccines (PCVs). Currently used PPV (Pneumovax 23) was first introduced in 1983 and by targeting 23 pneumococcal serotypes (1, 2, 3, 4, 5, 6B, 7F, 8, 9 N, 9 V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19A, 19F, 20, 22F, 23F, 33F) has valency broader than any PCV. However, unlike PCVs, PPV is not effective in very young children. Three different PCV’s are in use. The seven-valent vaccine (Prevnar, PCV7) was introduced in 2000, followed in 2009 by ten-valent (Synflorix, PCV10) and in 2010 by thirteen-valent (Prevenar13, PCV13) vaccines. PCV7 comprises serotypes 4, 6B, 9 V, 14, 18C, 19F and 23F, PCV10 includes additional serotypes 1, 5 and 7F, and PCV13 contains extra serotypes 3, 6A and 19A.
The introduction of PCVs into infant immunization programs has led to a major decrease in vaccine serotype (VT) disease in vaccinated children but to a various degree also resulted in herd effects across whole populations [4]. These indirect effects in unvaccinated individuals were caused by reduction of VT strain carriage in young children who are the main reservoir and main transmitters of pneumococci [5, 6]. PCVs may also contribute to a decrease in overall incidence of antimicrobial resistant pneumococcal disease [7]. This effect was augmented by the fact that VT strains were usually more resistant to antibiotics compared to non-vaccine (NVT) strains [7]. However, long term benefits of PCVs were eroded by the emergence of (multidrug-resistant) NVTs in carriage and in disease, the so called vaccine-induced serotype replacement [8].
There are differences in the timing of vaccine introduction, vaccination policies and vaccine coverage among countries that implemented PPV and PCVs into their National Immunization Programs (NIPs) [9]. This could result in differences in direct and herd effects, in serotype replacement and in resistance to anti-pneumococcal drugs in strains circulating in carriage and causing disease. By the end of 2012, 26 of the 53 countries of the European region vaccinated infants with PCVs in their NIPs [9]. In 2011, the PCVs coverage in infants’ vaccination (after administration of a minimum of 3 doses of vaccine by the age of 2 years) was more than 90% in these 26 European countries [9]. To our knowledge, there are no studies that evaluated the serotype distribution in commensal pneumococcal populations and its relationship with antimicrobial resistance across European countries as well as the impact of pneumococcal vaccination in a multicentre surveillance on pneumococcal carriage.
In this report, we assessed serotypes and resistance to antimicrobial agents of S. pneumoniae strains cultured from healthy carriers older than four years of age in nine European countries that differed in the timing of pneumococcal vaccines introduction, vaccines schedule and coverage, vaccines used (PCVs and PPV) and presence of catch-up campaigns. Results were analysed for impact of pneumococcal vaccination (immunization status) on individual person level and for effects that could be linked to differences in pneumococcal vaccination programs.
Methods
Study design
S. pneumoniae strains were cultured from samples collected from November 2010 to August 2011, as a part of the ‘The Appropriateness of prescribing antimicrobial agents in primary health care in Europe with respect to antimicrobial resistance’ (APRES) study as described by van Bijnen et al. [10]. Briefly, general practitioners (GP) from Austria, Belgium, Croatia, France Hungary, Spain, Sweden, the Netherlands and the United Kingdom (9 countries, 20 GPs per country), were each asked to provide nasal swabs from 200 healthy persons (with no history of antibiotic therapy or hospitalization in the previous three months), older than 4 years (except for UK, where for ethical reasons patients were older than 18 years). Within 48 h after collection swabs were transported to each national laboratory for further processing, with the exception of samples collected in France that were all sent to the Dutch national laboratory at Maastricht University Medical Centre (MUMC). On arrival to diagnostic labs, samples were cultured for S. pneumoniae using a standardized protocol [10]. Putative S. pneumoniae isolates from all participating countries were sent to the MUMC in skimmed milk at -80 °C for further analysis.
All participants provided written informed participatory consent and in the case of children aged less than 16, their parents or guardians provided written informed participatory consent on their behalf. All methods were approved by named institutional committee and were performed in accordance with relevant guidelines and regulations.
Capsular sequence typing (CST)
CST was performed in the National Institute for Public Health and the Environment, Bilthoven, The Netherlands as previously described by Elberse et al. [11]. Briefly, culture of S. pneumoniae in Brain Heart Infusion broth with 0,5% yeast extract, incubated overnight at 37 °C and 5% CO2, was heated at 95 °C for 10 min and used as a DNA template in PCR to amplify a fragment of the capsular wzh gene. Amplicons were sequenced by BaseClear BV, Leiden, The Netherlands. Sequences generated were assembled, edited and trimmed using Bionumerics v6.1 (Applied Maths, Sint-Maartens-Latem, Belgium) and assigned a capsular sequence type (CT) using the CST database (https://www.rivm.nl/mpf/typingtool/spn/). CT is a composite assignment, in which the first part represents the serotype assessed by conventional serotyping (Quellung) followed by the number representing a consecutive wzh allele identified among strains of a given serotype [11]. When an allele not yet recorded in CST database was found, serotype of an isolate was determined by Quellung method at the Netherlands National Reference Laboratory for Bacterial Meningitis (NRBM), Amsterdam, the Netherlands.
For statistical analysis feasibility, isolates were grouped by serotype and not by individual CTs. For CTs associated with a single serotype (61 of the 79 CST types found in this study), grouping was based on the first part of the CST assignment. For CTs represented by multiple serotypes, particularly those concerning vaccine serotypes, additional PCR and/or PCR-sequencing assays were performed as follows. For CTs representing serogroup 6 isolates, distinction between 6A/B and 6C/D was made using primers specific for wciNbeta, after which 6A and 6B were distinguished by PCR sequencing of wciP as described [12]. For CTs 15B-01, 15C-01, 22F-01, 23F-01, and 24F-01, the appropriate serotype-specific primers from the protocol of the CDC for multiplex PCR serotype deduction (http://www.cdc.gov/streplab/pcr.html) were used in single PCR. For isolates of CT 34–01, PCR-sequencing of the wzg gene was performed to distinguish between serotype 17 and 34 isolates. Finally, distinction between CT 25F-02-associated serotypes 25A/F and 38 was achieved by PCR-amplification of the wcyV gene. When no gene was amplified with the used primers and no CST could not be assigned, isolates were considered as not typable. Primers used for these additional PCR assays are shown in Additional file 1: Table S5.
Antimicrobial susceptibility
All isolates were tested for susceptibility to ceftazidime, clarithromycin, clindamycin, penicillin, tetracycline and trimethoprim-sulfamethoxazole. Minimal inhibitory concentrations of these drugs were assessed by broth microdilution method in accordance with EUCAST guidelines and EUCAST epidemiological cut-offs were applied as breakpoints [13]. Multidrug resistance was defined as resistance to three or more classes of antimicrobial agents.
Data analysis
In order to study the effect of vaccination on pneumococcal carriage and antimicrobial resistance, a multilevel logistic regression was performed. To account for non-random clustering of our data at family level and to control whether age and gender affects pneumococcal carriage prevalence, a 3-level multilevel logistic regression model (country, GP and patient) was estimated using MLWIN software package. Statistical analysis was performed using the PASW software package 19.0, with p-value < 0.05 considered statistically significant.
Results
Participants and bacterial strains
Table 1 shows the demographic background of the participating individuals. In total, 31,625 individuals were recruited, varying from 3969 in Spain to 3025 in Belgium. The proportion of males ranged between 39.9% in Croatia and 45.6% in Belgium. Working in the healthcare sector ranged between 2.2% in Hungary to 16.5% in Sweden and working in nursery between 1% in Croatia to 4.1% in Sweden. Living with children < 5 years of age was between 10.1% in Belgium and 16.1% in Sweden. Among all participants, 937 were identified as pneumococcal carriers and ranged between170 in France to 36 in UK.
Pneumococcal vaccination policy in the participating countries
Seven of the nine participating countries had introduced a pneumococcal conjugate vaccine in their NIP before November 2010 (Additional file 1: Table S1a) and used PCV7 during one (Sweden) to six years (Austria) prior to study onset. The exceptions were Croatia and Spain, two countries that only have risk-based pneumococcal vaccination programs. France was the only country with vaccination of risk group patients in the NIP in addition to infants. In Austria, Belgium, France and Sweden, PCV13 and PPV23 were used in adults and in risk populations (Additional file 1: Table S1b). In the Netherlands and Spain, only PPV23 was used in adult and on risk-based immunization. In Hungary, no recommendations were in place for vaccination of elderly and risk patients (Additional file 1: Table S1b).
Vaccination status among participants
Among all participants, 10.3% (n = 3316) were vaccinated, 79.0% (n = 25,404) were not, and 10.7% (n = 3441) had an unknown vaccination status. Among carriers, Spain had the highest percentage of vaccinated individuals (30.5%) and Croatia the lowest (0.7%) (Table 2). In all countries except Austria and Belgium, participants between 4 and 9 years old were more frequently vaccinated than those older than 10 years (p < 0.0001; Additional file 1: Table S2).
Serotype carriage in the participating countries
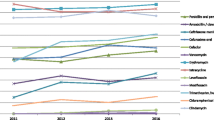
Serotype 11A was the most common in carriage in the study population (n = 60) followed by serotypes 23A (n = 58), 19A (n = 52), 3 (n = 51), 6C (n = 44) and 23B (n = 39). All these serotypes were considered as non-PCV types since none was targeted by either PCV7 or PCV10 used in the study populations at the time of sample collection. These serotypes were followed by 19F (n = 38) and 23F (n = 37), targeted by all commercially available pneumococcal vaccines. Serotype 23F was the most frequent among S. pneumoniae carriage isolates in Croatia (n = 15 of 134, 11.2%) one of two countries without PCVs in NIP. Serotype 23F was along with serotype 11A (n = 11 of 103, 10.7% each) also most common in carriage in Sweden, country with shortest PCV immunization program at the time the study was conducted (Additional file 1: Table S1a and b). Serotype 6C was the most common in the Netherlands (n = 11 of 129, 8.5%) and Spain (n = 11 of 167, 6.6%). Serotype 3 (n = 6, 14.0%), 15A (n = 6, 12.8%), 11A (n = 18, 10.6%) and 10A (n = 5, 13.9%) were the most common in Austria, Belgium, France and UK, respectively. Serotypes 23A and 15 B/C (n = 9, 7.8%) were the most common in Hungary (Table 3 and Additional file 1: Table S3).
Serotypes 17F and 22F, both targeted by PPV23 vaccine, were significantly associated with age older than 10 years (p = 0.03 and p = 0.01, respectively). Serotype 23F (PCV7 serotype) was significantly associated with age 4–9 years (p = 0.01). Other serotypes were not associated with any age category (Additional file 1: Table S4).
Vaccination effect on pneumococcal colonization and serotypes
Among the pneumococcal carriers (all serotypes considered), 115 were vaccinated and 727 were not vaccinated, while the vaccination status was unknown for 95 individuals.
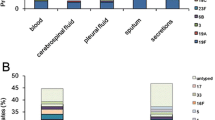
Table 4 shows the effect of pneumococcal vaccination on pneumococcal carriage. Being vaccinated was associated with a higher risk of pneumococcal colonization. None of the variables i.e. vaccine regimen, the presence of a catch-up campaign, the year of the vaccine implementation, the vaccine type, or the extent of vaccination program had separately a significant effect on pneumococcal colonization. Of 937 pneumococcal strains cultured from carriers, 170 (18.1%) were of PCV10 types. Of these 149 (15.9% of the total number of strains) were of PCV7. There were significantly fewer carriers of PCV10 serotypes among vaccinated (11 of 115, 9,6%) compared to non-vaccinated individuals (138 of 727, 19.0%), p = 0.01 (Table 5). These findings in combination with Table 4 suggest that vaccinated individuals have more chance to be colonized by non-vaccine serotypes.
Table 6 shows the antimicrobial resistance per serotypes. The highest resistance proportion to ceftazidime and penicillin was noticed among serotype 14 strains (13 of 16, 81.3%). Serotype 14 was the most frequent serotype showing resistance to penicillin, followed by serotype 19A and 15A. Among serotypes with more than 10 isolates, paediatric serotypes (6B, 9 V, 14, 19F and 23F) were more resistant to antimicrobial agents than non-paediatric serotypes (1, 3, 4, 7F). The serotypes presenting the highest proportion of multidrug resistance were 15A followed by 19A and 14. Serotypes 6C, 23B, 15A, 19A, 6A and 19F were significantly more prevalent whereas serotypes 22F, 23A, 3 and 14 were significantly less prevalent in the multidrug resistant fraction compared to the total study collection (Table 6).
Vaccination effect on antimicrobial resistance carriage
Table 7 shows the effect of vaccination on carriage of antimicrobial resistant pneumococcal isolates. Being vaccinated enhanced carriage of isolates resistant to at least one of the tested antimicrobial agents (model 1, OR = 0.60, p = 0.03). After adding different vaccination program characteristics (vaccine dose, conduction of catch-up campaign, period since vaccine was implemented, vaccine type and extent of vaccination program) separately, none of these could explain alone the vaccination effect (models 2–6).
Discussion
In this report, we assessed serotypes and resistance to antimicrobial agents of S. pneumoniae strains cultured from healthy carriers older than four years of age in nine European countries that differed in the timing of pneumococcal vaccines introduction. A large variation was found in serotype distribution in the participating countries and we observed difference in antimicrobial resistance including multidrug resistance, among these serotypes. The major finding was that pneumococcal vaccination was associated with a high risk of non PCV10 serotypes carriage.
This study was carried out on a large and well documented population, covering different age groups. To eliminate intra-laboratory variations, all methods were conducted in a central laboratory per method (susceptibility testing in MUMC, molecular serotyping in RIVM and conventional serotyping using Quellung method in NRBM). These points allowed us to accurately address the goals of this study. However, drawbacks were differences in numbers of strains collected and tested per country with significantly fewer strains from UK, Austria and Belgium (p < 0.0001) compared to any other participating sites. This could limit the generalization of our findings to the entire population in those countries. Possible explanation for differences in prevalence of carriage could be differences in age of sampled individuals (e.g. no minors under age of 18 years were sampled in UK) or in patterns of social contacts with very young children: carriage rates in parents of young children are reported to be few-fold higher compared to childless adults [14].
This study cannot be used to assess the spread and antimicrobial resistance in S. pneumoniae among non-vaccinated persons. This would require a longitudinal study. Furthermore, many factors determine carriage and resistance (e.g. antibiotic use was exclusion criterium in this study, seasonal variations in pneumococcal carriage), so one needs to be careful with drawing general conclusion based on these results.
For feasibility and costs considerations, capsular sequence typing was used in the primary method of serotyping. When highly frequent or vaccine CST’s could not be differentiated, additional PCR’s were performed. Conventional serotyping with type-specific sera was performed only when results generated with the CST method were equivocal. Our results support CST as a method alternative to the conventional Quellung serotyping in epidemiological studies.
PCV-7 was licensed in Europe in 2001. Higher valency vaccines were introduced since then (PCV-10 and PCV-13 in 2009 and 2010, respectively). If our results represented the effects of any vaccine in the studied population, these should be likely indirect (herd) effects of PCV7, and without any contribution of PCV13 since this vaccine was implemented after our study onset.
The most frequent serotypes among the carriage isolates were 11A, 19A, 3, 6C, 23A and 23B. All these serotypes were PPV vaccine or non-vaccine types. The most prevalent PCV7 vaccine type was 19F. These results might be explained by a replacement in the serotypes carriage. Our results are in concordance with an earlier report have reporting the predominance of non-vaccine serotypes, among which serotype 11A, in 336 paediatric patients in Ireland [15].
In contrast to previous carriage studies [16,17,18] which reported a decrease in pneumococcal carriage after vaccine implementation, our analyses show a higher risk of pneumococcal colonization upon vaccination. Most of the studies dealing with the effect of vaccination on pneumococcal carriage were conducted in vaccinated children and within few years after vaccination [19,20,21,22,23,24] . This reflects probably the immediate immunity and indirect effect of vaccination on the population. Our findings might be explained by the emergence of non-vaccine serotypes that co-circulated but were suppressed by vaccine serotypes. Another possible explanation could be that the protective effect of vaccination against pneumococcal carriage might decrease over time, allowing a re-emergence of vaccine serotypes in vaccinated patients. These results are supported by Principi et al., [25] who found that pneumococcal prevalence was higher in vaccinated individuals than in unvaccinated ones in a study enrolling 2076 children and adolescents from Italy.
Our results have shown that pneumococcal vaccination was associated with an increase in the prevalence of pneumococcal antimicrobial resistance. This may be explained by the fact that a vaccination might facilitate the introduction of new pneumococcal serotypes which are more resistant to antimicrobial agents [26] due to the replacement of vaccine serotypes [27].
A large variation in serotype distribution as well as in antimicrobial resistant serotypes was observed in the participating countries. In some countries, some serotypes were associated to resistance (19A and 14 resistance penicillin and ceftazidime). This might be due to differences in antimicrobial agents use between the participating countries [28], clonal spread of resistant microorganisms and antimicrobial cross-resistance between members of antimicrobial agents classes. This variation might justify the necessity of implementation of guidelines on antimicrobial agents use at country level.
Serotype 19A, a PCV-13 vaccine serotype, is the most frequent causative agent of invasive pneumococcal diseases All participants were provided a written consent form. For children consent was obtained from one of the parents or guardians. [29]. In our study, this serotype was also one of the most frequent carriage isolates (5.5%, n = 52) and one of the most resistant serotype to all antimicrobial agents tested. These results are in accordance with earlier reports [30].
Hackel et al., reported that serotype 15A was highly resistant to erythromycin and penicillin in clinical strains worldwide [31]. In our study, 15A representing 2.6% of all pneumococcal isolates (n = 24), was one of the most resistant serotypes to penicillin, ceftazidime, clarithromycin, clindamycin and tetracycline. Serotype 35B was, after 15A, the second most resistant non-vaccine serotype to penicillin and ceftazidime (38.2% of serotype 35B strains were resistant for both antibiotics). In the US, this serotype is becoming the dominating serotype in carriage and invasive pneumococcal disease, This is due to a clonal shift after the implementation of PCV7 and a spread of a β –lactam resistant clonal complex after the implementation of PCV13 [8, 32].
Conclusions
In conclusion, pneumococcal vaccination is associated with a higher risk of non PCV10 serotypes colonization and antimicrobial resistance independently of country and vaccine used. Serotypes 14 (PCV-7), 15A (non-vaccine serotype) and 19A (PCV-13) had the highest proportion of antimicrobial resistance and multidrug resistance. The emergence of new serotypes and related prevalence of antimicrobial resistance might justify at the short-term, a continuous evaluation and adjustment of available vaccines, in order to include newly emerged serotypes. At the long-term, the implementation of new vaccines that could cover all pneumococcal serotypes such as whole cell vaccines, might be helpful.
Abbreviations
- APRES:
-
“The Appropriateness of prescribing antimicrobial agents in primary health care in Europe with respect to antimicrobial resistance” study
- CDC:
-
Centers for Disease Control and Prevention
- CST:
-
Capsular Sequence Typing
- CT:
-
capsular sequence type
- EUCAST:
-
European Committee on Antimicrobial Susceptibility Testing
- GP:
-
general practitioners
- NIP:
-
National Immunization Programs
- NVT:
-
strains non-vaccine type
- PCR:
-
Polymerase Chain Reaction
- PCV:
-
pneumococcal conjugate vaccine
- PPV:
-
pneumococcal polysaccharide vaccine
- RIVM:
-
The National Institute for Public Health and the Environment
- VT:
-
vaccine serotype
References
Gray BM, Dillon HC Jr. Clinical and epidemiologic studies of pneumococcal infection in children. Pediatr Infect Dis. 1986;5(2):201–7.
Kadioglu A, Weiser JN, Paton JC, Andrew PW. The role of Streptococcus pneumoniae virulence factors in host respiratory colonization and disease. Nat Rev Microbiol. 2008;6(4):288–301.
Kay EJ, Yates LE, Terra VS, Cuccui J, Wren BW. Recombinant expression of Streptococcus pneumoniae capsular polysaccharides in Escherichia coli. Open Biol. 2016;6(4):150243.
Weinberger DM, Malley R, Lipsitch M. Serotype replacement in disease after pneumococcal vaccination. Lancet. 2011;378(9807):1962–73.
Whitney CG, Farley MM, Hadler J, Harrison LH, Bennett NM, Lynfield R, Reingold A, Cieslak PR, Pilishvili T, Jackson D, et al. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med. 2003;348(18):1737–46.
Grijalva CG, Nuorti JP, Arbogast PG, Martin SW, Edwards KM, Griffin MR. Decline in pneumonia admissions after routine childhood immunisation with pneumococcal conjugate vaccine in the USA: a time-series analysis. Lancet. 2007;369(9568):1179–86.
Kyaw MH, Lynfield R, Schaffner W, Craig AS, Hadler J, Reingold A, Thomas AR, Harrison LH, Bennett NM, Farley MM, et al. Effect of introduction of the pneumococcal conjugate vaccine on drug-resistant Streptococcus pneumoniae. N Engl J Med. 2006;354(14):1455–63.
Metcalf BJ, Gertz RE Jr, Gladstone RA, Walker H, Sherwood LK, Jackson D, Li Z, Law C, Hawkins PA, Chochua S, et al. Strain features and distributions in pneumococci from children with invasive disease before and after 13-valent conjugate vaccine implementation in the USA. Clin Microbiol Infect. 2016;22(1):60. e69–60 e29
Centers for Disease C, Prevention. Progress in introduction of pneumococcal conjugate vaccine - worldwide, 2000-2012. MMWR Morbidity and mortality weekly report. 2013;62(16):308–11.
van Bijnen EM, den Heijer CD, Paget WJ, Stobberingh EE, Verheij RA, Bruggeman CA, Pringle M, Goossens H, Schellevis FG. The appropriateness of prescribing antibiotics in the community in Europe: study design. BMC Infect Dis. 2011;11:293.
Elberse KE, van de Pol I, Witteveen S, van der Heide HG, Schot CS, van Dijk A, van der Ende A, Schouls LM. Population structure of invasive Streptococcus pneumoniae in the Netherlands in the pre-vaccination era assessed by MLVA and capsular sequence typing. PLoS One. 2011;6(5):e20390.
Mavroidi A, Godoy D, Aanensen DM, Robinson DA, Hollingshead SK, Spratt BG. Evolutionary genetics of the capsular locus of serogroup 6 pneumococci. J Bacteriol. 2004;186(24):8181–92.
EUCAST Definitive Document E.DEF 3.1, June 2000. Determination of minimum inhibitory concentrations (MICs) of antibacterial agents by agar dilution. Clin Microbiol Infect 2000. 6(9):509–15.
Wyllie AL, Rumke LW, Arp K, Bosch AA, Bruin JP, Rots NY, Wijmenga-Monsuur AJ, Sanders EA, Trzcinski K. Molecular surveillance on Streptococcus pneumoniae carriage in non-elderly adults; little evidence for pneumococcal circulation independent from the reservoir in children. Sci Rep. 2016;6:34888.
McElligott M, Vickers I, Cafferkey M, Cunney R, Humphreys H. Non-invasive pneumococcal serotypes and antimicrobial susceptibilities in a paediatric hospital in the era of conjugate vaccines. Vaccine. 2014;32(28):3495–500.
Steens A, Caugant DA, Aaberge IS, Vestrheim DF. Decreased carriage and genetic shifts in the Streptococcus pneumoniae population after changing the seven-valent to the thirteen-valent pneumococcal vaccine in Norway. Pediatr Infect Dis J. 2015;34(8):875–83.
Hammitt LL, Bruden DL, Butler JC, Baggett HC, Hurlburt DA, Reasonover A, Hennessy TW. Indirect effect of conjugate vaccine on adult carriage of Streptococcus pneumoniae: an explanation of trends in invasive pneumococcal disease. J Infect Dis. 2006;193(11):1487–94.
Galanis I, Lindstrand A, Darenberg J, Browall S, Nannapaneni P, Sjostrom K, Morfeldt E, Naucler P, Blennow M, Ortqvist A, et al. Effects of PCV7 and PCV13 on invasive pneumococcal disease and carriage in Stockholm, Sweden. Eur Respir J. 2016;47(4):1208–18.
Black S, Shinefield H, Fireman B, Lewis E, Ray P, Hansen JR, Elvin L, Ensor KM, Hackell J, Siber G, et al. Efficacy, safety and immunogenicity of heptavalent pneumococcal conjugate vaccine in children. Northern California Kaiser Permanente vaccine study center group. Pediatr Infect Dis J. 2000;19(3):187–95.
Impact of childhood pneumococcal vaccination programmes and activities for pneumococcal vaccines in the EU and EEA \EFTA countries. [http://venice.cineca.org/VENICE_Survey_PNC_1_2012-02-24.pdf]. Accessed 2011.
Grall N, Hurmic O, Al Nakib M, Longo M, Poyart C, Ploy MC, Varon E, Raymond J. Epidemiology of Streptococcus pneumoniae in France before introduction of the PCV-13 vaccine. Eur J Clin Microbiol Infect Dis. 2011;
Strutton DR, Farkouh RA, Earnshaw SR, Hwang S, Theidel U, Kontodimas S, Klok R, Papanicolaou S. Cost-effectiveness of 13-valent pneumococcal conjugate vaccine: Germany, Greece, and the Netherlands. J Inf Secur. 2012;64(1):54–67.
Thoon KC, Chong CY, Tee NW. Early impact of pneumococcal conjugate vaccine on invasive pneumococcal disease in Singapore children, 2005 through 2010. Int J Infect Dis. 2012;16(3):e209–15.
Weil-Olivier C, van der Linden M, de Schutter I, Dagan R, Mantovani L. Prevention of pneumococcal diseases in the post-seven valent vaccine era: a European perspective. BMC Infect Dis. 2012;12:207.
Principi N, Terranova L, Zampiero A, Montinaro V, Ierardi V, Peves Rios W, Pelucchi C, Esposito S. Pharyngeal colonization by Streptococcus pneumoniae in older children and adolescents in a geographical area characterized by relatively limited pneumococcal vaccination coverage. Pediatr Infect Dis J. 2015;34(4):426–32.
Farrell DJ, Klugman KP, Pichichero M. Increased antimicrobial resistance among nonvaccine serotypes of Streptococcus pneumoniae in the pediatric population after the introduction of 7-valent pneumococcal vaccine in the United States. Pediatr Infect Dis J. 2007;26(2):123–8.
Leibovitz E. The effect of vaccination on Streptococcus pneumoniae resistance. Curr Infect Dis Rep. 2008;10(3):182–91.
Goossens H, Ferech M, Vander Stichele R, Elseviers M. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005;365(9459):579–87.
Navarro Torne A, Dias JG, Quinten C, Hruba F, Busana MC, Lopalco PL, Gauci AJ, Pastore-Celentano L, disease Ecefp. European enhanced surveillance of invasive pneumococcal disease in 2010: data from 26 European countries in the post-heptavalent conjugate vaccine era. Vaccine. 2014;32(29):3644–50.
Song JH, Dagan R, Klugman KP, Fritzell B. The relationship between pneumococcal serotypes and antibiotic resistance. Vaccine. 2012;30(17):2728–37.
Hackel M, Lascols C, Bouchillon S, Hilton B, Morgenstern D, Purdy J. Serotype prevalence and antibiotic resistance in Streptococcus pneumoniae clinical isolates among global populations. Vaccine. 2013;31(42):4881–7.
Chochua S, Metcalf BJ, Li Z, Walker H, Tran T, McGee L, Beall B. Invasive serotype 35B pneumococci including an expanding serotype switch lineage, United States, 2015-2016. Emerg Infect Dis. 2017;23(6):922–30.
Acknowledgements
We thank all members of medical microbiology laboratory at Maastricht University Medical Centre (MUMC) and the National Institute for Public Health and the Environment (RIVM) for their support.
Funding
This study has been funded by the European Commission - DG Research within its 7th Framework Program (Grant Agreement 223083).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
CDJH, WJP and EES coordinated the strain collection as members of the APRES study. RYY performed the data analysis, the strains identification and the antimicrobial susceptibility. HJB and GNP performed the Capsular Sequence Typing (CST). WJP and PS performed the multilevel logistic regression. RYY, HJB, KT and EES interpreted the results. RYY, HJB K.T and EES drafted the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for this study has been obtained in all of the participating countries, from the following ethics committees:
-
Austria: Ethik-Kommission der Medizinischen Universität Wien und des Allgemeinen Krankenhauses der Stadt Wien Akh (number: 568/2010)
-
Belgium: Commissie Medische Ethiek van de Universitaire Ziekenhuizen K.U.Leuven (number: ML6355)
-
Croatia: Sveučilišta u Zagrebu Medicinski Fakultet Ethical Committee (number: 04–77/2010–246)
-
France: Comité de protection des personnes CPP “Ile-de-France III” (number: 2010-A01004–35 (2853))
-
Hungary: Egészségügyi Tudományos Tanács, Tudományos es Kutatásetikai Bizottság (ETT TUKEB) (number:5635–0/2010-1018EKU (401/PI/010)
-
The Netherlands: Medisch Ethische Commissie azM/UM (number: MEC 10–4-030.4/pl)
-
Spain: Clinical Ethics Committee of the IDIAP Jordi Gol and Gurina (number: P10/55)
-
Sweden: Regionala Etikprövningsnämnden i Linköping (number: 2010–326-31)
All participants provided written informed participatory consent and in the case of children aged less than 16, their parents or guardians provided written informed participatory consent on their behalf.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Table S1. a: Infants vaccination in National Immunization Program in the nine participating countries. b: Vaccination in elderly and risk patients in the nine participating countries. Table S2. Association between age and vaccination status in (non-) vaccinated participants in participants with known age range. Table S3. Serotypes distribution by country (%). Serotypes listed in order from highest to lowest in frequency among all S. pneumoniae strains cultured in the study as reported in the last column. Table S4. Serotypes distribution by age category (%). Serotypes listed in order from highest to lowest in frequency. Only serotypes represented by more than 10 strains among all S. pneumoniae strains cultured in the study are reported. Correlation between serotypes frequency in different age groups is shown in the last column. Table S5. Primers used in this study. (DOCX 67 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yahiaoui, R.Y., Bootsma, H.J., den Heijer, C.D.J. et al. Distribution of serotypes and patterns of antimicrobial resistance among commensal Streptococcus pneumoniae in nine European countries. BMC Infect Dis 18, 440 (2018). https://doi.org/10.1186/s12879-018-3341-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-018-3341-0