Abstract
Background
The Xpert® MTB/RIF (Xpert) assay is a rapid PCR-based assay for the detection of Mycobacterium tuberculosis complex DNA (MTBc) and mutations associated with rifampin resistance (RIF). An updated version introduced in 2011, the G4 Xpert, included modifications to probe B and updated analytic software.
Methods
An analytical study was performed to assess Xpert detection of mutations associated with rifampin resistance in rifampin-susceptible and -resistant isolates. A clinical study was performed in which specimens from US and non-US persons suspected of tuberculosis (TB) were tested to determine Xpert performance characteristics. All specimens underwent smear microscopy, mycobacterial culture, conventional drug-susceptibility testing and Xpert testing; DNA from isolates with discordant rifampin resistance results was sequenced.
Results
Among 191 laboratory-prepared isolates in the analytical study, Xpert sensitivity for detection of rifampin resistance associated mutations was 97.7% and specificity was 90.8%, which increased to 99.0% after DNA sequencing analysis of the discordant samples. Of the 1,096 subjects in the four clinical studies, 49% were from the US. Overall, Xpert detected MTBc in 439 of 468 culture-positive specimens for a sensitivity of 93.8% (95% confidence interval [CI]: 91.2%–95.7%) and did not detect MTBc in 620 of 628 culture-negative specimens for a specificity of 98.7% (95% CI: 97.5%–99.4%). Sensitivity was 99.7% among smear-positive cases, and 76.1% among smear-negative cases. Non-determinate MTBc detection and false-positive RIF resistance results were low (1.2 and 0.9%, respectively).
Conclusions
The updated Xpert assay retained the high sensitivity and specificity of the previous assay versions and demonstrated low rates of non-determinate and RIF resistance false positive results.
Similar content being viewed by others
Background
The Xpert® MTB/RIF (Xpert) assay [1, 2] detects the presence of Mycobacterium tuberculosis complex DNA (MTBc) and mutations associated with resistance to rifampin (RIF) in clinical samples in under two hours. Xpert was endorsed by the World Health Organization (WHO) in December 2010 [2, 3] and recent meta-analyses describe the assay’s excellent performance characteristics in the field [4, 5]. Since the release of Xpert for use, several modifications have been made to improve assay performance. The updated version, the G4 Xpert, includes modifications to one of the five rpoB-specific assay probes (probe B) and to the analytic software settings with the goal of decreasing both false positive RIF resistance results and the >5% non-determinate result rate reported in some settings [6].
Although the updated G4 Xpert assay was available for use in December 2011 [6], most published Xpert performance reports were conducted using previous versions of the assay [4]. In addition, few studies have reported the performance of the G4 Xpert on samples from both high- and low-tuberculosis (TB) prevalence populations. Here we present data on G4 Xpert assay performance from analytical testing and multi-site clinical studies in various settings, including settings with a low prevalence of TB.
Methods
Study design and specimen inclusion criteria
Analytical testing of rifampin resistance detection performance
Xpert performance of RIF resistance detection was evaluated using 200 unique clinical isolates spiked into pooled human sputum. The isolates were selected from the specimen bank at the Massachusetts Supranational Tuberculosis Reference Laboratory at the University of Massachusetts Medical School and had been obtained from standard of care (SOC) sputum specimens from individuals in Russia, Peru, Hong Kong, Haiti, and USA. Isolates were selected based on phenotypic drug susceptibility test results. One hundred RIF susceptible isolates, 100 RIF resistant isolates and an additional 50 aliquots of MTB culture-negative pooled human sputum were randomized and blinded for testing.
Clinical studies
Four clinical studies were conducted to assess Xpert detection of MTBc and RIF resistance in specimens from patients 18 years of age or older with suspected TB. Clinical study 1 (CS1) included four collections of archived MTB culture-positive and -negative specimens collected from non-US regions as part of research studies conducted by the Foundation for Innovative New Diagnostics [7]. Subject inclusion criteria were: 1) pulmonary TB symptoms (see Additional file 1); and 2) no anti-TB medication in the 60 days prior to sample collection. Xpert testing was performed at New Jersey Medical School (NJMS).
Clinical study 2 (CS2) specimens consisted of archived MTB culture-positive and culture-negative sputum specimens that were leftover from SOC evaluations of US patients with suspected TB illness. Xpert testing was done at the State of New York Department of Health in Albany, NY.
Clinical study 3 (CS3) and 4 (CS4) tested up to three prospectively collected leftover SOC specimens from US (CS3) and Mexican (CS4) patients suspected to have TB; the first specimen with sufficient volume was selected for Xpert testing. CS3 Xpert testing was done at the New York State Department of Health in Albany, NY, the Florida Department of Health, Bureau of Public Health Laboratories in Jacksonville, FL, and the Orange County Health Care Agency in Santa Ana, CA. CS4 Xpert testing was performed at the Orange County Health Care Agency in Santa Ana, CA.
See Additional file 1 for further details on study design and specimen inclusion criteria.
Laboratory testing
In the analytical study, culture-positive isolates were confirmed to be MTBc positive by AccuProbe MTBC Identification Test (Hologic Incorporated, Marlborough, MA). Rifampin susceptibility was determined via the Middlebrook agar proportion method [8] according to each laboratory’s standard operating procedure. Bi-directional sequencing of the rpoB core region was performed for all specimens with discordant RIF resistance results. The culture isolates were spiked at low, moderate, or high concentrations into sputa (see Additional file 1) and tested with the Xpert assay. Fifty aliquots of pooled MTB negative human sputum were interspersed randomly during testing as a negative control.
The methods used at each of the clinical study sites for AFB smear, MTB culture, and DST are summarized in Table 1. Samples in all studies were tested by Xpert according to the package insert instructions [9]. All frozen specimens were stored at -70 °C and all prospectively collected samples were stored per the sample storage constraints described in the package insert. If multiple samples from each patient were available, the first specimen with sufficient volume for testing was used. Duplicate specimen enrollment for the same patient for Xpert testing was not allowed. Bi-directional sequencing of the rpoB core region was performed on MTB culture-positive isolates with discordant Xpert MTB or RIF susceptibility results. No sequencing was performed for MTB culture-negative specimens with discordant Xpert results. Sequencing of concordant samples was omitted. Sequencing was performed in Borstel Germany for CS1, at the NY State Department of Health for CS2 and CS3, and at the University of Massachusetts Medical School for CS4.
Clinical study case definitions
AFB smear status was determined using the specimen with a corresponding Xpert result. An MTB positive case was defined as MTB growth on solid or liquid culture from any specimen. An MTB negative case was defined as no MTB growth from any baseline specimen; baseline was defined as collected within seven days of presentation. A case was defined as MTB indeterminate when all cultures were overgrown by non-MTB bacteria or fungi and an MTB positive or negative culture result could not be determined. Phenotypic resistance was determined to be present if 1% or more of the test population grew in the presence of the critical concentration of rifampicin, defined as 1.0 μg/mL.
The GeneXpert software (Version 4.3) reported MTB results as “MTB detected” or “MTB not detected” and RIF resistance results as “MTB detected; RIF resistance detected”, “MTB detected; RIF resistance not detected”, and “MTB detected; RIF resistance indeterminate”. Xpert results of “invalid”, “error” or “no result” were defined as “non-determinate”.
Statistical analysis
Xpert detection of MTBc DNA was assessed relative to culture; culture indeterminate and Xpert non-determinate specimens were excluded. Xpert detection of mutations associated with RIF resistance was assessed relative to DST; specimens where DST results were not available, MTBc was not detected by Xpert, or MTBc was detected but RIF resistance results were indeterminate were excluded. See Additional file 1 for further details including sample size calculations.
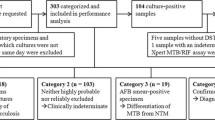
For the clinical studies, any specimens involved in protocol deviations were excluded from analysis (see Figs. 1, 2 and 3). Specimens in CS1 were collected from subjects participating in a research study and specimens tested in CS2-4 were SOC specimens. Data from the four clinical studies were tested for homogeneity across multiple parameters using the Fisher’s Exact Test. A critical p-value was set to 0.01 due to multiple testing in several categories (Bonferroni principle).
Results
Specimen inclusion and clinical demographics
Analytical study
Of the 200 culture-positive isolates from the specimen bank at the Massachusetts Supranational TB Reference Laboratory identified for inclusion in this study, nine were excluded due to: no culture growth (n = 4); specimen was not inoculated on LJ media (n = 4); specimen was lost (n = 1); and specimen was from a duplicate subject (n = 1). Of the remaining 191, 118 (62%) were from Peru, 64 (34%) were from the U.S., 8 (4%) were from Russia, and one was from an unknown WHO collection site. No other demographic information was collected for this study.
Clinical studies
A total of 1,026 specimens were obtained in the four collections of specimens included in CS1. After the 400 specimens in collection two were excluded due to insufficient volume, 626 total specimens remained; of these, 544 were eligible for Xpert testing (Fig. 1). Among these, 358 (66%) were from males and 183 (34%) were from females; the gender of the patient was unknown for three specimens. The average age of the patient at the time of specimen collection was 38 years (range 18-83 years). Two hundred and eighty-eight (53%) patients were from Vietnam, 174 (32%) were from Peru, 79 (15%) were from South Africa, and 3 (0.6%) were from Bangladesh. Thirteen specimens were excluded because Xpert results were non-determinate, resulting in 531 available for inclusion.
Of 100 specimens identified for CS2, 92 were eligible for inclusion in this analysis (Fig. 2). Of these, 51 (55%) were from males, 37 (40%) were from females and the gender of the patient was unknown for 4 (4%). The average age of the patient at the time of specimen collection was 52.6 years (range 18 to 91 years).
CS3 and CS4 were analyzed separately and subsequently combined because specimens in both studies were collected and tested prospectively. Of the 621 subjects initially enrolled (592 in CS3 and 29 in CS4), 473 specimens were eligible for inclusion in the analysis (Fig. 3). Of the enrolled subjects, 274 (60%) were male and 185 (40%) were female; gender was unknown for 14. The age of the subject was known for 118 (24.9%) of study participants; of these, the average age at specimen collection was 52.4 years (range 19 to 88 years). Forty-eight percent (n = 227) of the specimens were from California, 25% (n = 118) were from New York, 22% (n = 105) were from Florida, and 5% (n = 23) were from Mexico.
HIV status was either negative or not captured in the clinical studies.
Xpert performance
Analytical study
Of the 191 clinical isolates, 185 were from Xpert positive specimens, four were from MTB not detected specimens, and two were from specimens reported as non-determinate. Xpert reported RIF resistance in 85 of 87 isolates that were RIF resistant by DST for a sensitivity of 97.7% (95% CI: 92.0%-99.4%). The Xpert assay was negative for RIF resistance in 89 of 98 specimens that were RIF susceptible by DST for a specificity of 90.8% (95% CI: 83.5%-95.1%). There were no Xpert RIF indeterminate results. The rpoB core region was sequenced for all 15 isolates with discordant Xpert results (Table 2a); Xpert reported RIF resistance in all cases where there was a mutation in the rpoB core region associated with RIF resistance and in one case where there was not. Using resistance associated rpoB core region mutations to define RIF resistance, Xpert sensitivity for RIF resistance increased to 97.7% (95% CI: 92.0%-99.4%) and specificity to 99.0% (95% CI: 94.4%-99.8%).
Clinical studies
The results for all four clinical studies were analyzed together across multiple parameters (see Additional file 1 for results of CS1 alone and poolability analysis).
Subject demographics
Among 1,096 subjects for which MTB culture results were available, 679 (62%) were male and 396 (36%) were female; gender was unknown for 21 (2%). The subjects were from geographically diverse regions: 542 (49%) were from the US (California, New York and Florida) and 554 (51%) were from outside the US (Vietnam, Peru, South Africa, Mexico and Bangladesh). Of the 542 US specimens, 450 (83%) were collected prospectively and 92 (17%) were from an archived specimen bank; of the 554 non-US specimens, 23 (4%) were prospectively collected and 531 (96%) were from an archived specimen bank. One sputum specimen was collected from 34% of subjects, two from 44%, and 3 from 22%. An Xpert result was obtained with the first specimen collected for 86% of subjects, with the second for 11% of subjects, and with the third for 0.3% of subjects; for 3% of specimens it was unknown which sputum was used for Xpert testing.
Xpert assay performance for detection of MTB
Overall, Xpert detected MTBc in 439 of 468 total specimens that were culture positive for MTB for a sensitivity of 93.8% (95% CI: 91.2%-95.7%). Xpert did not detect MTBc in 620 of 628 culture-negative specimens for a specificity of 98.7% (95% CI: 97.5%-99.4%). Among smear-positive, culture-positive cases, Xpert detected MTBc in 350 of 351 cases for a sensitivity of 99.7% (95% CI: 98.4%-99.9%). Among smear-negative, culture-positive cases, Xpert detected MTBc in 89 of 117 cases for a sensitivity of 76.1% (95% CI: 67.6%-82.9%). Discordant results are presented in Table 2b.
Among US specimens (low prevalence settings), Xpert sensitivity for detection of MTBc was 91.0% (95% CI: 83.3%-95.4%; n = 89) and specificity was 99.3% (95% CI: 98.1%-99.9%; n = 453). Among non-US specimens (high prevalence settings), Xpert sensitivity for detection of MTBc was 94.5% (95% CI: 91.7%-96.3%; n = 379) and specificity was 97.1% (95% CI: 93.5%-98.8%; n = 175). Xpert performance characteristics for detection of MTBc are stratified by sample collection method (535 expectorated, 234 induced, 327 unknown) and type of specimen (606 specimens were raw and 490 were concentrated) in Table 3.
Xpert assay performance for detection of RIF resistance
MTB positive culture isolates were tested for susceptibility to rifampin using DST and results were compared with Xpert detection of mutations associated with RIF resistance. Of the 1,096 subjects tested by Xpert, 1,082 were included in the analysis. Eight subjects that did not have DST results were excluded. Six of 447 (1.3%, 95% CI: 0.6%-2.9%) specimens that were positive for MTBc and RIF resistance indeterminate by Xpert were also excluded; one of 351 (0.3%, 95% CI: 0.01%-1.6%) smear-positive specimens and five of 96 (5.2%, 95% CI: 2.2%-11.6%) smear-negative specimens.
Of the 1,082 included samples, 627 were culture negative and did not have DST. Of 455 remaining, 21 were RIF resistant and 434 were RIF susceptible by DST. Among the 21 samples with RIF resistance by DST, two were Xpert MTBc negative and one was MTBc detected, RIF resistance not detected. Excluding Xpert MTBc negative samples, Xpert detected mutations associated with RIF resistance in 18 of 19 samples for a sensitivity of 94.7% (95% CI: 75.4%-99.1%). Of 434 samples that were RIF susceptible by DST, 26 were Xpert MTBc negative. Excluding those, Xpert did not report RIF resistance in 404 of 408 samples for a specificity of 99.0% (95% CI: 97.5-99.6%). Four samples were determined to be RIF susceptible by DST and RIF resistant by Xpert. One was tested by Agar Proportions using LJ in Peru and three were tested using MGIT SIRE (BD BACTEC™ MGIT™ 960 SIRE Kits For the Antimycobacterial Susceptibility Testing of Mycobacterium tuberculosis): one in South Africa and two in Vietnam.
Bi-directional sequencing was performed on all isolates from culture-positive specimens with discrepant results (Table 2b). The one Xpert false RIF-susceptible sample was determined to contain a mixture of wild type and mutant rpoB core region DNA by sequencing. Three of the four apparent Xpert false RIF resistant samples had rpoB core mutations. One of these three was a silent mutation (514ttt) while the other two had rpoB core mutations associated with clinically relevant resistance not always identified by phenotypic RIF susceptibility testing [10–13]. Overall, four (0.9%) had false positive rifampin resistance test results; if using sequencing based mitigation, two (0.5%) had false positive rifampin resistance test results.
Of 1,126 tested specimens, 17 were excluded from the sensitivity and specificity analysis due to culture contamination. However, all 17 specimens had valid Xpert results on the first attempt and were included in the calculated non-determinate rate. Of the 1,126 specimens, 24 were non-determinate for the following reasons: 17 probe check failures, two temperature being out of range, two signal losses, one SPC failure, one syringe motion, and one cartridge integrity. Of the 24 non-determinate, 11 were successful on repeat test and 13 were not repeated due to low sample volume. Overall, 13 (1.2%, 95% CI: 0.7% to 2.0%) of 1,126 specimens had a non-determinate Xpert result.
Positive predictive value (PPV) and negative predictive value (NPV) for Xpert detection of MTB and RIF resistance
The likelihood that a positive test result is a true positive will vary based on the prevalence of TB in the population and whether the AFB smear is positive or negative. A prospective clinical evaluation of Xpert in patients suspected of active TB in the United States resulted in a prevalence of 11.8% and a percentage of AFB-positive smears among MTB culture positive subjects of 75.5%[14]. Hypothetical estimated PPV and NPV of MTB detection using Xpert for different prevalence rates of MTB are shown in Table 4. These calculations are based on the overall sensitivity and specificity observed in all four clinical studies (as above, sensitivity of 99.7% for smear positive specimens, 76.1% for smear-negative specimens and overall specificity of 98.7%).
Hypothetical estimated predictive values for the result “MTB Detected, RIF Resistance DETECTED” for different prevalence rates of MTB culture positive subjects and different prevalence rates of RIF resistance among MTB culture positive subjects are shown in Table 5. These calculations are based on hypothetical prevalences and the overall sensitivity and specificity of Xpert RIF resistance detection observed in all four clinical studies (sensitivity 94.7% and specificity of 99.0%). In the US population with TB the prevalence of rifampin resistance is approximately 1.8% [14].
Discussion
We found high G4 Xpert sensitivity and specificity for detection of MTBc and RIF resistance in both analytical and clinical specimens collected from TB culture positive and negative subjects from US and non-US settings. Sensitivity for detection of MTBc in clinical samples was 99.7% among smear-positive specimens, 76.1% among smear-negative specimens and specificity was 98.7%. These results are very similar to the 2013 Cochrane review which found sensitivity of 98% and 67% for smear positive and smear negative specimens respectively, and a pooled specificity of 98% among studies using prior versions of the assay [4]. Xpert sensitivity and specificity for RIF resistance detection was 94.7% and 99% respectively in our combined clinical studies. This also compared well to reports using prior Xpert versions (94% and 98%, respectively [4]). In our analytical study, sensitivity and specificity for RIF resistance detection was 97.7% and 90.8%, respectively. However, this changed to 97.7% and 99.0%, respectively, when DNA sequencing was used as the reference method. Several recent studies have shown that some rpoB mutations are associated with low-level RIF resistance that are not detected by phenotypic testing, yet have poor clinical outcomes equivalent to patients with high level RIF resistance [10–13].
A small study by Sohn et al. [15] evaluated the diagnostic accuracy of both G4 and the previous version of the Xpert assay using induced sputum samples from 502 subjects in Montreal, Canada. The overall sensitivity of Xpert was very low: 11/25 (46%) overall, 6/7 (86%) for smear-positive specimens, and 5/17 (29%) for smear-negative specimens. Sensitivity of the G4 (5/15, 33%) was observed to be lower than the previous version (6/10, 60%), but this difference was not significant and was not stratified by smear status. The authors hypothesized that the lower sensitivity may have been related to lower bacillary load at presentation. Another possibility is that target bacilli may have been diluted by the saline used for induction [16].
We observed a statistically significant decrease in sensitivity among induced sputum samples compared to expectorated sputum for AFB smear-negative subjects (4/10 vs. 77/97; p-value <0.01), but not in smear positive samples (15/15 induced, 285/286 expectorated). However, other studies have observed that induced sputum samples had a higher diagnostic yield by culture [17] and shorter times to positivity by MGIT [18].
Thirteen (1.2%) of 1,126 specimens had a non-determinate Xpert result, which was lower than previously reported rates of >5% using earlier Xpert versions. Four samples were determined to be RIF susceptible by DST and RIF resistant by Xpert and three were determined to have RIF resistance-associated mutations in the rpoB core region by bi-directional sequencing although one was a non-resistance associated silent mutation. This leads to a 0.94% (4/427) false positive rate, or 0.47% (2/427) if using sequencing based mitigation.
There are several limitations to this study. First, sample collection, processing, shipment, storage and testing were done across various settings, which may have introduced some variability to our data collection and sample processing methods. In particular, one of the clinical studies was conducted as part of a research study, while the others analyzed leftover SOC specimens. For this reason the research clinical study was analyzed separately (see Additional file 1) and a poolability analysis was conducted to demonstrate that the four clinical studies could be combined. In addition, some specimens had been frozen and stored prior to testing, which may have introduced variability in testing results.
Conclusions
We found that the G4 Xpert assay had low rates of non-determinate and false positive RIF resistance results that were not consistent with previously reported rates observed at some sites. In addition, we found high sensitivity and specificity for MTBc and RIF resistance detection that compared well to the previous versions of the assay [4]. Most published reports of Xpert assay performance were conducted using the previous versions of the assay; our findings represent one of the first large studies reporting G4 Xpert assay performance and add to the growing literature [19–22] in both high- and low-TB prevalence settings.
Abbreviations
- CS1:
-
Clinical study 1
- CS2:
-
Clinical study 2
- CS3:
-
Clinical study 3
- CS4:
-
Clinical study 4
- NJMS:
-
New Jersey Medical School
- NPV:
-
Negative predictive value
- PCR:
-
Polymerase chain reaction
- PPV:
-
Positive predictive value
- RIF:
-
Rifampin
- SOC:
-
Standard of care
- TB:
-
Tuberculosis
- WHO:
-
World Health Organization
- Xpert:
-
Xpert® MTB/RIF
References
Helb D, Jones M, Story E, Boehme C, Wallace E, Ho K, Kop J, Owens MR, Rodgers R, Banada P, et al. Rapid detection of Mycobacterium tuberculosis and rifampin resistance by use of on-demand, near-patient technology. J Clin Microbiol. 2010;48(1):229–37.
World Health Organization. Policy statement: automated real-time nucleic acid amplification technology for rapid and simultaneous detection of tuberculosis and rifampicin resistance: Xpert MTB/RIF system. Geneva, Switzerland: World Health Organization; 2011. [http://apps.who.int/iris/handle/10665/44586]. Accessed 22 Nov 2016.
World Health Organization. WHO monitoring of Xpert MTB/RIF roll-out [http://www.who.int/tb/areas-of-work/laboratory/mtb-rif-rollout/en/]. Accessed 22 Nov 2016.
Steingart KR, Sohn H, Schiller I, Kloda LA, Boehme CC, Pai M, Dendukuri N. Xpert(R) MTB/RIF assay for pulmonary tuberculosis and rifampicin resistance in adults. Cochrane database of Syst Rev. 2013;1:CD009593.
Steingart KR, Schiller I, Horne DJ, Pai M, Boehme CC, Dendukuri N. Xpert(R) MTB/RIF assay for pulmonary tuberculosis and rifampicin resistance in adults. Cochrane Database Syst Rev. 2014;1:CD009593.
Foundation for Innovative New Diagnostics. Performance of Xpert MTB/RIF version G4 assay. Geneva: Foundation for Innovative New Diagnostics; 2011. http://www.stoptb.org/wg/gli/assets/documents/map/findg4cartridge.pdf. Accessed 22 Nov 2016.
Foundation for Innovative New Diagnostics [http://www.finddx.org]. Accessed 22 Nov 2016.
Kent PT, Kubica GP. Public health mycobacteriology: a guide for the level III laboratory: Centers for Disease Control. GA: Atlanta; 1985.
Cepheid. Xpert MTB/RIF assay (package insert). Sunnyvale: Cepheid; 2013. http://www.cepheid.com/manageddownloads/xpert-mtb-rif-english-package-insert-301-1404-rev-c.pdf. Accessed 22 Nov 2016.
Boehme CC, Nabeta P, Hillemann D, Nicol MP, Shenai S, Krapp F, Allen J, Tahirli R, Blakemore R, Rustomjee R, et al. Rapid molecular detection of tuberculosis and rifampin resistance. N Engl J Med. 2010;363(11):1005–15.
Rigouts L, Gumusboga M, de Rijk WB, Nduwamahoro E, Uwizeye C, de Jong B, Van Deun A. Rifampin resistance missed in automated liquid culture system for Mycobacterium tuberculosis isolates with specific rpoB mutations. J Clin Microbiol. 2013;51(8):2641–5.
Williamson DA, Roberts SA, Bower JE, Vaughan R, Newton S, Lowe O, Lewis CA, Freeman JT. Clinical failures associated with rpoB mutations in phenotypically occult multidrug-resistant Mycobacterium tuberculosis. Int J Tuberc Lung Dis. 2012;16(2):216–20.
Van Deun A, Aung KJ, Bola V, Lebeke R, Hossain MA, de Rijk WB, Rigouts L, Gumusboga A, Torrea G, de Jong BC. Rifampin drug resistance tests for tuberculosis: challenging the gold standard. J Clin Microbiol. 2013;51(8):2633–40.
CDC. Reported Tuberculosis in the United States, 2011. Atlanta: Department of Health and Human Services, CDC; 2012.
Sohn H, Aero AD, Menzies D, Behr M, Schwartzman K, Alvarez GG, Dan A, McIntosh F, Pai M, Denkinger CM. Xpert MTB/RIF testing in a low tuberculosis incidence, high-resource setting: limitations in accuracy and clinical impact. Clin Infect Dis. 2014;58(7):970–6.
Theron G, Peter J, Calligaro G, Meldau R, Hanrahan C, Khalfey H, Matinyenya B, Muchinga T, Smith L, Pandie S, et al. Determinants of PCR performance (Xpert MTB/RIF), including bacterial load and inhibition, for TB diagnosis using specimens from different body compartments. Sci Rep. 2014;4:5658.
Peter JG, Theron G, Pooran A, Thomas J, Pascoe M, Dheda K. Comparison of two methods for acquisition of sputum samples for diagnosis of suspected tuberculosis in smear-negative or sputum-scarce people: a randomised controlled trial. Lancet Respir Med. 2013;1(6):471–8.
Geldenhuys HD, Whitelaw A, Tameris MD, Van As D, Luabeya KK, Mahomed H, Hussey G, Hanekom WA, Hatherill M. A controlled trial of sputum induction and routine collection methods for TB diagnosis in a South African community. Eur J Clin Microbiol Infect Dis. 2014;33(12):2259–66.
Ardizzoni E, Fajardo E, Saranchuk P, Casenghi M, Page A, Varaine F, Kosack C, Hepple P. Implementing the Xpert® MTB/RIF diagnostic test for tuberculosis and rifampicin resistance: outcomes and lessons learned in 18 countries. PLoS One. 2015;10(12):e0144656.
Reechaipichitkul W, Phetsuriyawong A, Chaimanee P, Ananta P. Diagnostic test of sputum GeneXpert MTB/RIF for smear negative pulmonary tuberculosis. Southeast Asian J Trop Med Public Health. 2016;47(3):457–66.
Agrawal M, Bajaj A, Bhatia V, Dutt S. Comparative study of GeneXpert with ZN stain and culture in samples of suspected pulmonary tuberculosis. J Clin Diagn Res. 2016;10(5):DC09–12.
Sing S, Singh A, Prajapati S, Kabra SK, Lodha R, Mukherjee A, Singh V, Hesseling AC, Grewal HM. Delhi Pediatric TB study group: Xpert MTB/RIF assay can be used on archived gastric aspirate and induced sputum samples for sensitive diagnosis of paediatric tuberculosis. BMC Microbiol. 2015;15:191.
Van Deun A, Barrera L, Bastian I, Fattorini L, Hoffmann H, Kam KM, Rigouts L, Rüsch-Gerdes S, Wright A. Mycobacterium tuberculosis strains with highly discordant rifampin susceptibility test results. J Clin Microbiol. 2009;47(11):3501–6.
Van Deun A, Aung KJ, Bola V, Lebeke R, Hossain MA, de Rijk WB, Rigouts L, Gumusboga A, Torrea G, de Jong BC. Rifampin drug resistance tests for tuberculosis: challenging the gold standard. Int J Tuber Lung disease. 2013;51(8):2633–40.
Scott LE, McCarthy K, Gous N, Nduna M, Van Rie A, Sanne I, Venter WF, Duse A, Stevens W. Comparison of Xpert MTB/RIF with other nucleic acid technologies for diagnosing pulmonary tuberculosis in a high HIV prevalence setting: a prospective study. PLoS Med. 2011;8(7):e1001061.
Acknowledgements
We would like to acknowledge Discovery Life Sciences, Los Osos, CA for facilitating access to the specimens from Mexico.
Funding
This work was supported by Cepheid, Inc, USA. The paper was prepared by the authors at the following investigational sites: New Jersey Medical School, Rutgers, the State University of New Jersey, Newark, New Jersey, USA; University of Massachusetts Medical School, Boston, Massachusetts, USA; Orange County Health Care Agency, Santa Ana, California, USA; Wadsworth Center, New York State Department of Health, Albany, New York, USA; Florida Department of Health, Jacksonville, Florida, USA; Clínica y Laboratorio de Tuberculosis, Hospital General Tijuana, Tijuana, Mexico; Foundation for Innovative New Diagnostics, Geneva, Switzerland. The data analysis was performed by Cepheid statisticians in collaboration with the authors.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publically available because they are part of a confidential submission to the FDA.
Authors’ contributions
NJD participated in the analysis and interpretation of data and drafting the manuscript. RB participated in the acquisition of data, the analysis and interpretation of data, and critically revising the manuscript. AS participated as PI and in the acquisition of data and critically revising the manuscript. DK participated in the acquisition of data and critically revising the manuscript. RCA participated as PI and in the acquisition of data and critically revising the manuscript. MG participated in the acquisition of data and critically revising the manuscript. KAM participated as PI and in the acquisition of data and critically revising the manuscript. VEE participated in the acquisition of data and critically revising the manuscript. MR participated in the acquisition of data and critically revising the manuscript. SC participated as PI and in the acquisition of data and critically revising the manuscript. RL participated as PI and in the acquisition of data and critically revising the manuscript. EV participated in the acquisition of data and critically revising the manuscript. PN participated as PI and in the acquisition of data and critically revising the manuscript. PJ participated in conception and design of the study, in the analysis and interpretation of the data, and in critically revising the manuscript. DA participated in conception and design of the study, in the analysis and interpretation of the data, and in critically revising the manuscript and as PI. All authors read and approved the final manuscript.
Competing interests
D.A. is one of a group of co-investigators who invented molecular beacon technology and who receive income from licensees, including a license to Cepheid for M. tuberculosis detection. However, the income attributable to the Xpert MTB/RIF assay which he may receive has been irrevocably capped at $5000 per year as a management of this conflict of interest. P.J. receives salary and benefits from Cepheid, and is a shareholder in Cepheid. None of the other authors have any conflicts to declare.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study protocol and procedures were reviewed and approved by the regulatory bodies at all involved local clinical and laboratory sites, including: New Jersey Medical School, Rutgers, the State University of New Jersey, Newark, New Jersey, USA; University of Massachusetts Medical School, Boston, Massachusetts, USA; Orange County Health Care Agency, Santa Ana, California, USA; Wadsworth Center, New York State Department of Health, Albany, New York, USA; Florida Department of Health, Jacksonville, Florida, USA; Clínica y Laboratorio de Tuberculosis, Hospital General Tijuana, Tijuana, Mexico; Foundation for Innovative New Diagnostics, Geneva, Switzerland; and Cepheid, Inc., Sunnyvale, California, USA. No investigational device test results were provided to the healthcare provider or study participants during the study. No informed consent was required as the samples were de-identified and the data were analyzed anonymously.
Author information
Authors and Affiliations
Corresponding authors
Additional file
Additional file 1:
Supplementary Materials. (PDF 239 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Dharan, N.J., Blakemore, R., Sloutsky, A. et al. Performance of the G4 Xpert® MTB/RIF assay for the detection of Mycobacterium tuberculosis and rifampin resistance: a retrospective case-control study of analytical and clinical samples from high- and low-tuberculosis prevalence settings. BMC Infect Dis 16, 764 (2016). https://doi.org/10.1186/s12879-016-2039-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-016-2039-4