Abstract
Background
The majority of persons with dementia (PWD) are mainly cared for by their family members in the home. Evidence is however scarce on family caregivers’ psychosocial burden and quality of life in Asian countries including Malaysia. This study describes the baseline data of a telephone-delivered psychoeducational intervention study and examines the determinants of outcome measures (caregiver burden, depressive and anxiety symptoms, quality of life and caregiving self-efficacy) among Malaysian family caregivers to PWD.
Methods
This was a cross-sectional study originated from the baseline survey of a randomized control trial of 121 family caregivers recruited from lists of PWD who were registered at memory and psychiatry clinics in three tertiary care hospitals in Malaysia. The participants were assessed for caregiver burden by the Zarit Burden Interview, depressive and anxiety symptoms by the Hospital Anxiety and Depression Scale, quality of life by the Control, Autonomy, Self-Realization, and Pleasure Scale, and caregiving self-efficacy by the Revised Scale for Caregiving Self-Efficacy.
Results
Prevalence of caregiver burden was 69.4%, depressive symptoms 32.2% and anxiety symptoms 32.2%. Family caregivers to PWD having perceived peer support e.g., social/family/friend/significant other supports were less likely to report caregiver burden, depressive and anxiety symptoms, and more likely to report higher levels of quality of life and caregiving self-efficacy. Being married and PWD’s ability to self-care were associated with lesser likelihood of experiencing caregiver burden, depressive and anxiety symptoms. The other determinants of greater probability of reporting better quality of life were caregivers’ employment and having Islamic faith. Marital status (married), PWD’s ability to self-care, spousal relationship with PWD and shared caregiving process were associated with higher likelihood of reporting caregiving self-efficacy.
Conclusion
Caregiver burden, depressive and anxiety symptoms are prevalent in family caregivers to PWD in Malaysia. Social support and caregiving related factors influence family caregivers’ quality of life and caregiving self-efficacy. Implementing psychoeducational intervention and support in the psychiatry and memory clinics may help improve the psychosocial burden, quality of life and caregiving self-efficacy in family caregivers of PWD.
Trial registration
ISRCTN14565552 (retrospectively registered).
Similar content being viewed by others
Background
Globally, variations exist in cultural norms and factors such as accessibility, affordability of health and social services which impact reliance of persons with dementia (PWD) on family members to take on a caregiver role [1]. Malaysia as an aging society with a rapid demographic change has, similar to other countries, a growing number of PWD, creating challenges for health and social care [2]. Due to the trajectory of the disease, providing care for a PWD can entail long care hours over a prolonged period impacting on the caregiver and family function and challenging stability of the family [3]. Caring for a family member with dementia can be demanding and stressful. Caregivers to PWD have shown to be at higher risk of developing depression and anxiety than persons caring for family members with other illnesses [4], experience significantly higher levels of caregiver burden [5], low level of quality of life [6] and low level of self-efficacy [7].
Self-reported symptoms of depression and anxiety are common in family caregivers impacting on health and quality of life while caring for a PWD [8]. Women and spousal caregivers are reported as more likely to develop anxiety and depression than their counterparts [4, 8]. Factors that may moderate the presence of anxiety disorder in caregivers to PWD include living with the care recipient, level of dependence of PWD, being a female caregiver, poor relationship with the care recipient and health of the caregiver [9]. According to Wulff et al. [8], the amount of time spent caring for the family member and the severity of person’s dementia impact on the levels of depression and anxiety experienced.
Caregiving responsibilities for a PWD include supporting the person with instrumental activities of daily living such as cooking, shopping, etc., and even basic activities of daily living such as bathing, dressing, mobility, etc. [10, 11]. For a PWD living at home, such support is often provided by family members, 70% of whom are female [12]. According to Tulek et al. [6] high level of caregiver burden is related to low quality of life. Family caregivers’ quality of life can directly impact on the care they provide for the PWD, and how they cope with their own life situation. As dementia is a progressive disease, the family caregiver’s quality of life changes over time in relation to the needs of the caregiver and ability to handle the care recipient’s deteriorating condition.
There are multiple benefits of caring for a PWD which include perception of caring as a meaningful task, a feeling of giving back to the loved one, sense of close family relationship and satisfaction of providing care [5, 13]. However, positive aspects of caregiving can be accompanied by the strains of caregiving leading to a sense of caregiver burden [5]. This in turn can negatively impact caregivers multi-dimensionally, i.e., physically, psychologically, emotionally, behaviourally and financially [14]. Evidence from around the world such as China [15], Indonesia [16], Turkey [6] indicate high levels of caregiver burden for family caregivers to PWD living at home. Several factors are identified as predictors of caregiver burden. These include neuropsychiatric symptoms of PWD [17], functional (cognitive and physical) decline of the PWD cared for which is related to increased number of hours spent in caregiving activities [18], and lack of perceived social support [15, 16]. Spouses to PWD identified that their partners had between five to eight co-existing neuropsychiatric symptoms causing varied levels of distress for the spouses concerned [19]. Family caregivers’ socio-demographic characteristics such as being a woman [16, 20], cohabitation and spousal relationship with the PWD [18] are also identified as significant predictors of caregiver burden.
Several studies suggest that self-efficacy can be a useful concept for explaining variations in caregiving abilities of family caregivers of PWD. Self-efficacy refers to the perception of a person´s capacity to manage responsibilities and tasks successfully and confidently [21]. In relation to family caregiving in dementia, self-efficacy has also been suggested to represent family caregiver’s knowledge and preparedness in managing the challenges of care [22]. Feeling prepared is reported to be associated with low levels of distress [7]. Improvements of caregiver self-efficacy may positively influence caregiver health and well-being [22] and reduce levels of caregiver burden [23]. Likewise, education and skills training, case management, and interventions that target caregiver’s negative emotions are associated with improvements in self-efficacy [24].
Various educational, psychosocial, and multicomponent interventions have demonstrated modest success in improving the quality of life and negative consequences associated with caregiving for persons with dementia [17, 25]. In-person interventions can be difficult for caregivers due to lack of transportation, being homebound, living in a rural setting, time pressures of caregiving, or stigma associated with seeking help [25]. In response to these issues, telephone-based interventions have been reported to improve functioning in caregivers, to persons with dementia, with a variety of clinical problems in USA [25], Australia [26], UK [27], Europe [28] and Hong Kong [29]. Due to its high accessibility and cost-effective implementation, the telephone-delivered support services for dementia caregivers have received global attention. Studies indicated that telephone-based interventions benefited caregivers by means of increasing use of appropriate community services, reducing caregiver burden, depression and distress related to care recipient behaviour, and improving caregiving self-efficacy and quality of life [26, 30].
According to the Alzheimer Disease International [31], the prevalence of dementia in Malaysia was 0.063% in 2005 with the annual incidence rate of 0.020%, and in 2015 was 0.401%. It is projected that this figure will increase to 0.852% and 1.924% in 2030 and 2050, respectively. Like in many Asian countries, family members in Malaysia provide most of the care and support to PWD living in the community [32, 33]. With a view to develop and evaluate a care and support intervention for family caregivers to PWD living in the community in Malaysia, it is imperative to understand their current situation. Hence, this paper describes the baseline data of a telephone-delivered psychoeducational intervention study and explores the associated factors of the outcome measures caregiver burden, depressive and anxiety symptoms, self-efficacy, and quality of life among family caregivers to PWD living at home in Malaysia.
Methods
Study design and setting
Data for this cross-sectional study originated from the baseline survey of a randomized control trial (RCT) aimed to assess the efficacy of a telephone-delivered psychoeducational intervention. The intervention was delivered by healthcare professionals (occupational therapists and nurses) to reduce caregiver burden, depressive and anxiety symptoms, and improve caregiving self-efficacy and quality of life among family caregivers to PWD. Participants were recruited from lists of PWD over eight months (August 2022 to March 2023) who were registered at memory and psychiatry clinics of Universiti Kebangsaan Malaysia Medical Centre (UKMMC), Sultan Ahmad Shah Medical Centre (SASMEC) of International Islamic University Malaysia (IIUM) and Hospital Tengku Ampuan Afzan (HTAA). UKMMC (a university tertiary hospital) located in Selangor state, and SASMEC (a university tertiary hospital) and HTAA (a state level tertiary hospital) located in Pahang state in west and east coasts of Malaysia, respectively (see Additional file 1).
Participants
Participants in this study were family caregivers of PWD who had received a clinical diagnosis of dementia. Participants were included if they were Malaysian citizens, aged 18 years or over, able to read and write Malay, primary caregivers (in case of more than one caregiver), in caregiving role for at least 6 months with at least 4 h caregiving activities per day, and had smartphones. Exclusion criteria included if family caregivers described themselves as having any major acute medical illnesses or if they could not participate throughout the entire study due to lack of time.
Assuming a current improvement rate of 30% in caregiver burden and depressive symptoms, expected net improvement of 25–30% with the intervention [34], a significance level of 5% and power of 80%, the estimated sample size for the RCT was 100 (50 in intervention group and 50 in control group). In case of the secondary outcome i.e., quality of life, considering the mean (SD) in treatment group of 55.58 (17.75) and control of 50.00 (18.37) as a result of intervention [35], a median effect size of 0.5 [36], and a significance level of 5% and power of 80%, resulted in a calculated sample size of 51 (rounded to 50) in each group. In both calculations, the one-sided test was considered. Taking into account a drop-out rate of 20%, the estimated sample size was 60 participants in each group. Initially, 380 family caregivers were screened for eligibility and 121 were assigned to either a psychoeducation group (intervention group) or a control group using a computerized 4-block randomization program (Fig. 1).
Data collection
Baseline data for the RCT were collected from August 2022 to March 2023. Training of the research assistants included information on the questionnaire and data collection procedures. The trained research assistants were blinded to group assignment, communicated with the family caregivers by telephone to provide detailed information about the purpose and type of study. Further information was given about the psychoeducation intervention including its procedures and protocols, and risks as well as benefits of participating in the study. Only those family caregivers who provided informed consent to participate were enrolled in this study. The research assistants then interviewed the participants at baseline over telephone using structured questionnaire to collect information on their socioeconomic condition (family caregiver’s age, sex, education [primary, secondary or tertiary], occupation [homemaker/unemployed, retired, employed incorporating government and non-government employee], monthly household income [≥RM 10,960 categorized as high-, RM 4,581–RM 10,959 middle- and ≤RM 4.580 low-income]); caregiving information (duration of care, hours of caregiving per day, if the caregiving was shared by other family members, number of family members involved in shared caregiving, caregiver’s relationship with PWD); perceived social support. Perceived social support was assessed by the validated Malay version of the Multidimensional Scale of Perceived Social Support (MSPSS) [37]. MSPSS included 12 items, scored on a 7-point scale from 1 (very strongly disagree) to 7 (very strongly agree). MSPSS comprised of three subscales, including family support (4 items), friends’ support (4 items) and significant others’ support (4 items), a higher score indicating more support [38]. Significant support from others indicated support from a special person who was available when needed, was a real source of comfort. The scale demonstrated good internal consistency in the present study with Cronbach’s alpha of 0.93 on the whole scale and between 0.91 and 0.92 on the three subscales.
Outcome measures
The outcome measures in the study included caregiver burden, depressive and anxiety symptoms, quality of life and caregiving self-efficacy.
Caregiver burden
Caregiver burden was measured by the Zarit Burden Interview (ZBI). ZBI is a 22-item inventory, where each item is rated on a 5-point scale (0–4) with the total score ranging from 0 to 88. A higher score indicates greater burden. ZBI assesses caregiver’s subjective feelings of the negative impact of caregiving on emotional and physical health functioning, social life and financial status [39]. The ZBI has been validated in Malaysia, with 70.8% sensitivity and 69.2% specificity using an optimum cut-off score of 22 [40]. This cut-off score was used in this study to categorize family caregivers as having burden. The scale had good internal consistency with Cronbach’s α of 0.92.
Depressive and anxiety symptoms
Depressive and anxiety symptoms was assessed by the Hospital Anxiety and Depression Scale (HADS) [41]. The HADS is a 14-item scale that requires respondents to endorse a verbal response which is scored as an index of the severity of anxiety or depression. The HADS questionnaire has seven items each for depression and anxiety subscales. Scoring of each item ranges from zero to three, with three denoting highest anxiety or depression level. The Malay version of HADS showed a good sensitivity (90.0% for anxiety and 93.2% for depression) and specificity (86.2% for anxiety and 90.8% for depression) at the cut-off score of 8/9 [41]. Thus, a total subscale score of > 8 points out of a possible 21 denote considerable symptoms of anxiety or depression. The scale presented good reliability in the study with Cronbach’s α of 0.84 for anxiety and 0.78 for depression.
Quality of life
Quality of life was measured by the validated Malay version of Control, Autonomy, Self-Realization, and Pleasure (CASP-19) scale [42]. The CASP-19 consists of four domains: four items focus on control domain, five items cover the autonomy domain, and five questions each on self-realization and pleasure domains. Each item is rated on a 4-point scale from never (0) to often (3), with a total score ranging from 0 to 57 where higher score indicates better quality of life. CASP-19 showed a good reliability in the study with Cronbach’s α of 0.88.
Caregiving self-efficacy
The Revised Scale for Caregiving Self-Efficacy (RSCSE) was used to measure caregiving self-efficacy [43]. The RSCSE is a 15-item scale which rates caregivers’ beliefs about their ability to perform caregiving activities according to their recent situation from 0 (cannot do it at all) to 100 (certain they can do it). The scale consists of 3 subscales (5 items per subscale): obtaining respite (item 1 to 5), responding to disruptive patient behaviours (item 6 to 10), and controlling upsetting thoughts (item 11 to 15). The item scores within each subscale are averaged to obtain subscale ratings ranging between 0 and 100. Higher score indicates higher confidence in self-efficacy. The RSCSE has potential uses for both research and clinical purposes. The RSCSE was translated from English to Bahasa Melayu and then back to English again by two bilingual public health researchers. The translated Malay version of the instrument was then pretested with the family caregivers of PWD (not included in the study) to check appropriateness of the terminology in Bahasa Melayu. RSCSE demonstrated good internal consistency in the present study with the Cronbach’s α for subscales ranged from 0.86 to 0.94.
Data analysis
Descriptive analyses were performed to report participants’ background characteristics, caregiving information and outcome measures. An independent t-test, \(\:\mathcal{X}\)2 test and Fisher’s exact two-sided p test were conducted to compare means and proportions between groups. As the ZBI, HADS-depression and HADS-anxiety subscales had definitive cut-off points, we used these outcomes as dichotomous and multiple logistic regression were performed to determine their associated factors. We used multiple linear regression (Backward Method) model to assess the determinants of quality of life and caregiving self-efficacy. As the perceived social support and its three subscales were highly multicollinear, separate models were run for each of them. A p value of < 0.05 was considered for statistical significance.
Results
Sample profile
Table 1 shows the mean age of the 121 family caregivers of PWD included in the study was 52 years, ranging from 23 years to 85 years. 69% of the family caregivers were women and three-quarters were married. Although the mean years of schooling was 13, nearly half of them received tertiary level of education and were employed in private or public sectors. Approximately 56% of the participants were from low-income level and 8% from high-income level with median monthly income of RM 4000 (USD 1 = RM 4.5). About three-fourths of the caregivers were in non-spousal relationship and the majority were PWD’s own children. The family caregivers had been providing care for almost 47.9 months (≅ 4 years) spending about 19 h per day. The majority of PWD (63%) were women with the mean age of 75 years and 56% were able to take care of themselves (self-care). 60% of the caregivers stated that they received support from other family members in providing care for PWDs. The average scores were 59.3 for perceived social support, 21.1 for family support, 16.1 for friend support and 21.7 for significant other support.
Descriptives of the outcome measures
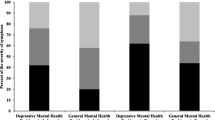
Of the 121 caregivers, 84 had ZBI score ≥22, indicating that the point prevalence of caregiver burden was 69.4% (CI95% 59.5 − 79.3%) with a mean score of 41.8 (SD 14.5). Similarly, the point prevalences of depressive and anxiety symptoms were 32.2% (CI95% 17.5 − 46.9%), mean score10.9 (SD 2.3) and 36.4% (CI95% 34.3 − 38.5%), mean score 11.3 (SD 3.3), respectively. The mean score was 40.3 (10.5) for quality of life and 71.8 (28.9), 71.1 (23.8) and 76.8 (19.3) on the three subscales of caregiving self-efficacy (Table 2).
Determinants of the outcome measures
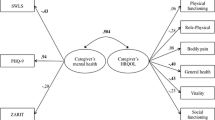
Table 3 reveals the adjusted odds ratio (OR) obtained in the multiple logistic regression models showed that family caregivers were less likely to report caregiver burden, depressive and anxiety symptoms if they were married and if the PWDs were able to self-care. Those with higher perceived social support, particularly family support were also less likely to report caregiver burden, depressive and anxiety symptoms. Support from a significant other was found to be significantly associated with caregiver burden and depressive symptoms but not with anxiety symptoms. Moreover, family caregivers in older age and with longer caregiving duration were less likely to report depressive symptoms. Hosmer and Lemeshow tests for caregiver burden (Chi-square = 4.386, p = 0.821), depressive symptoms (Chi-square = 4.885, p = 0.770) and anxiety symptoms (Chi-square = 4 = 10.157, p = 0.254) indicated that models fitted the data well.
Table 4 presents the adjusted linear regression models on the continuous outcome variables showed that the higher the perceived social support including family support, friend support and significant other support, the higher the quality of life and caregiving self-efficacy for obtaining respite among the family caregivers. However, friend support was not identified as a determinant for self-efficacy for responding to disruptive patient behaviors and self-efficacy for controlling upsetting thoughts about caregiving. In addition, family caregivers who were employed and identified themselves as Muslim were more likely to report better quality of life. Caregiving self-efficacy for responding to disruptive patient behavior was more likely to be reported if the family caregivers were married, and self-efficacy for controlling upsetting thoughts about caregiving if PWDs were able to care for themselves (self-care). Family caregivers who were spouses and shared caregiving were more likely to report caregiving self-efficacy for obtaining respite and controlling upsetting thoughts about caregiving. Moreover, duration of care was negatively associated with self-efficacy for obtaining respite.
Discussion
The current study examined baseline measures of a telephone-delivered psychoeducational intervention for family caregivers to PWD in Malaysia. The majority of the family caregivers in this study were married [20] and women, a similar pattern to that reported in Asia [44] and other parts of the world [45, 46]. Although spouses are often reported to take on the primary role as caregivers to PWD in countries, such as Shanghai, China [15] and Australia [20], most of the caregivers in this study were adult children. The majority of participants shared caregiving responsibilities with other family members over an average of four years. This timeframe concurs with similar studies from e.g. Argentina [45], United States of America [47], Canada [48], and Iran [5]. Where caregiving became a shared responsibility, women in mixed-gender sibling group, are shown to take the lead in caregiving [48].
In this study, the mean caregiving hours were on average 18 h per day. This figure exceeds data from European countries with a mean of 6 h/day [49], however, in line with a study from Malyasia 15 h caregiving was reported per day [50]. Family caregivers reported in the current study how their engagement in caregiving extended beyond caregiving activities. This perspective is potentially influenced by their cohabitation with the PWD and an ongoing sense of responsibility throughout the day. This aligns with findings from an Austrian study, showing that family caregivers feel the need to be constantly available and on guard due to the dependency of the PWD [51].
In the current study, the prevalence of caregiver burden was almost 70% compared to a meta-analysis where the prevalence ranged from 35.8 to 88.5% with a pooled prevalence of 62.5% [52]. The mean caregiver burden score of 32.9 in this study mirrors that of international studies using the ZBS, with scores of: 30.7 in Australia [20], 34.1–37.4 in Hong Kong, China [29] and lower scores in India of 47.9 [44]. In this study, family caregivers who were married were less likely to experience burden possibly due to support from their spouses in caregiving responsibilities. Family caregivers with higher perceived social support, particularly from family and significant others, were less likely to experience caregiver burden. A study from Nepal [53] suggested that the majority of family caregivers (88%) in their study who experienced little to no caregiver burden was attributed to cultural factors such as filial piety and responsibilities (Khanal & Chalise, 2020). The results of this study indicated the higher the level of self-care among PWD the less likely family caregivers reported burden of care. This has been attributed to how increasing function dependency due to severity of dementia entails longer caregiving hours, thereby contributing to greater caregiver burden [17].
In this study the prevalence of caregiver depressive and anxiety symptoms were 32% and 36%, respectively. Similar findings were reported by Collins and Kishita [52] with informal caregivers had a pooled prevalence of depression of 31% and a 32% pooled prevalence of anxiety [54]. Family caregivers were less likely to report depressive and anxiety symptoms if, they were married, if the PWD was able to care for self, and if social support was available, especially from family and significant others. Finally, older family caregivers who provided care over a long period of time reported less symptoms. An important determinant in protecting family caregivers from depression and anxiety, in an Asian population, is the caregiver´s perceived sense of control over the situation (also known as mastery) and level of competence. These factors were independently associated with negative outcomes associated with caregiver depression and anxiety [55].
The availability and accessibility of support in societies with mostly family caregivers are positively related to quality of life [1]. Consistent with other research [2, 56], the results indicate that family caregivers reporting a higher social support network from e.g. family, friends and significant others were more likely to report better quality of life. In addition, improved quality of life was more likely to be reported by family caregivers who were employed and identified themselves as Muslim. This can be explained by a perception of the importance of culture and belief as a family caregiver. As suggested in a review from China [57], family caregivers showed lower depressive symptoms most likely due to the perception of fulfilling society’s cultural requirements to take care of family members.
Similar to findings by Tan et al. [58], this study showed that older family caregivers were likely to report a high sense of self-efficacy in terms of controlling upsetting thoughts, partly due to their life experiences and age. This might partly explain why spouses of PWD were more likely to report high self-efficacy in terms of obtaining respite and controlling negative emotions, in comparison to their children, both in this study and Colloby et al. [59]. Familiarity of routines and aspects of relationship may act as a buffer for some initial challenges experienced by older family caregivers [59]. Both Tew et al. [60] and Tan et al. [58] mirror this study´s results, that caregivers living with the care recipient demonstrate lower levels of self-efficacy than others. This study shows that shared caregiving was positively associated with obtaining respite and controlling upsetting thoughts. According to Steffen et al. [43] increased social support, enhances the likelihood that the family caregiver will find someone to care for the PWD if respite is needed. Participants in this study scored notably higher mean scores (all above 71) of self-efficacy in all three domains of the Revised Scale For Caregiving Self-Efficacy; Obtaining Respite, Responding to Disruptive Patient Behaviors, and Controlling Upsetting Thoughts, compared to Steffen et al. [43]. Steffen, et al. [43] found that family caregivers with higher perceived social support reported greater care-giver efficacy. This aligns with the Social Cognitive Theory which suggests a bidirectional relationship between perceived coping efficacy and social support [21].
The current study has used locally validated instruments to measure caregiver burden, depressive and anxiety symptoms, and quality of life except for the caregiving self-efficacy. Translation and back translation were done on the RSCSE scale by two bi-lingual researchers, to help minimize error and inconsistencies. As the instrument has not been used in Malaysia before, the results should be interpreted with caution. The ZBI is known to have a high rate of false positive as the detection of levels of experienced burden can be impeded by respondent’s gender and culture. However, higher sensitivity of 70.8% with a lower but reasonable specificity of 69.2% at the recommended cut-off score in this study, indicated that a false negative rate is less desired than a false positive case [40]. Duration of caregiving per day were reported subjectively according to respondents’ perceptions may introduce bias through over-estimation. Although telephone interviews have been identified as cost-effective and time-efficient, the greatest challenge with this type of interview is the loss of several communication cues, distractions, and technical difficulties. However, by allowing flexibility and breaking the interview into multiple sessions can help overcome such challenges.
Conclusion
This study contributes to current research on protective factors that enhance sustainable support for family members caring for a PWD in Malaysia. This indicates a necessity of implementing a psychoeducational intervention for the family caregivers to a PWD in the memory, geriatric, and psychiatry clinics in Malaysia. Given the time and efforts associated with caring for PWDs, a telephone delivered intervention has the potential to be highly accessible for the family caregivers. Such an intervention needs to be culturally adopted and its efficacy examined in reducing psychosocial burden and improving quality of life and caregiving self-efficacy in family caregivers of PWDs in Malaysia. Further research is required in Asian countries to gain an understanding of cultural and economic factors and gender roles when designing support programmes for family caregivers in a community setting.
Data availability
The dataset generated and analysed during the current study are not publicly available due to confidentiality issues but are available from the corresponding author on reasonable request.
Abbreviations
- PWD:
-
Persons with dementia
- RCT:
-
Randomized control trial
- MSPSS:
-
Multidimensional Scale of Perceived Social Support
- ZBI:
-
Zarit Burden Interview
- HADS:
-
Hospital Anxiety and Depression Scale
- CASP:
-
Control Autonomy Self-Realization and Pleasure Scale
- RSCSE:
-
Revised Scale for Caregiving Self-Efficacy
- SD:
-
Standard deviation
References [Reference No. 12 should be changed to Reference No. 6. And, reference numbers 6 - 11 should be changed to 7 - 12]
Hazzan AA, Dauenhauer J, Follansbee P, Hazzan JO, Allen K, Omobepade I. Family caregiver quality of life and the care provided to older people living with dementia: qualitative analyses of caregiver interviews. BMC Geriatr. 2022;22(1):86. https://doi.org/10.1186/s12877-022-02787-0.
Ganapathy SS, Sooryanarayana R, Ahmad NA, Jamaluddin R, Abd Razak MA, Tan MP, Ibrahim N. Prevalence of dementia and quality of life of caregivers of people living with dementia in Malaysia. Geriatr Gerontol Int. 2020;20(Suppl 2):16–20. https://doi.org/10.1111/ggi.14031.
Hsin-Yi L, Lian-Hua H. The relationship between family functioning and caregiving appraisal of dementia family caregivers: caregiving self-efficacy as a mediator. Aging Ment Health. 2018;22(4):558–67. https://doi.org/10.1080/13607863.2016.1269148.
Bin SA, Sayampanathan AA, Cuttilan A, Chun-man Ho R. (2015). Prevalence of mental health disorders among caregivers of patients with Alzheimer disease. J Am Med Dir Assoc. 2015;16(12):1034–41.
Abdollahpour I, Nedjat S, Salimi Y. Positive aspects of Caregiving and Caregiver Burden: a study of caregivers of patients with dementia. J Geriatr Psychiatry Neurol. 2018;31(1):34–8. https://doi.org/10.1177/0891988717743590.
Tulek Z, Baykal D, Erturk S, Bilgic B, Hanagasi H, Gurvit IH, Caregiver, Burden. Quality of life and related factors in Family caregivers of Dementia patients in Turkey. Issues Ment Health Nurs. 2020;41(8):741–9. https://doi.org/10.1080/01612840.2019.1705945.
Wawrziczny E, Berna G, Ducharme F, Kergoat MJ, Pasquier F, Antoine P. Modeling the distress of spousal caregivers of people with dementia. J Alzheimers Dis. 2017;55(2):703–16.
Wulff J, Malmgren Fänge A, Lethin C, Chiatti C. Self-reported symptoms of depression and anxiety among informal caregivers of persons with dementia: a cross-sectional comparative study between Sweden and Italy. BMC Health Serv Res. 2020;20:1114. https://doi.org/10.1186/s12913-020-05964-2.
Mahoney R, Regan C, Katona C, Livingston G. Anxiety and depression in family caregivers of people with Alzheimer disease: the LASER-AD study. Am J Geriatr Psychiatry. 2005;13:795–801.
Tu JY, Jin G, Chen JH, Chen YC. Caregiver Burden and Dementia: a systematic review of Self-Report instruments. J Alzheimers Dis. 2022;86(4):1527–43. https://doi.org/10.3233/JAD-215082.
Del-Pino-Casado R, Priego-Cubero E, Lo´pez-Mart´ınez C, Orgeta V. (2021). Subjective caregiver burden and anxiety in informal caregivers: A systematic review and meta-analysis. PLoS ONE. 2021;16(3):e0247143. https://doi.org/10.1371/journal.pone.0247143.
WHO. Global status report on the public health response to dementia. Geneva: World Health Organization. 2021. Retrieved from https://iris.who.int/handle/10665/344701 License: CC BY-NC-SA 3.0 IGO.
Vikström S, Josephsson S, Stigsdotter-Neely A, Nygård L. Engagement in activities: experiences of persons with dementia and their caregiving spouses. Dementia. 2008;7(2):251–70.
Chiao CY, Wu HS, Hsiao CY. Caregiver burden for informal caregivers of patients with dementia: a systematic review. Int Nurs Rev. 2015;62(3):340–50.
Liu Z, Sun W, Chen H, et al. Caregiver burden and its associated factors among family caregivers of persons with dementia in Shanghai, China: a cross-sectional study. BMJ Open. 2022;12:e057817. https://doi.org/10.1136/bmjopen-2021-057817.
Putri YSE, Putra IGNE, Falahaini A, Wardani IY. Factors Associated with Caregiver Burden in caregivers of older patients with dementia in Indonesia. Int J Environ Res Public Health. 2022;19(19):12437. https://doi.org/10.3390/ijerph191912437.
Cheng ST. Dementia caregiver Burden: a Research Update and critical analysis. Curr Psychiatry Rep. 2017;19(9):64. https://doi.org/10.1007/s11920-017-0818-2.
Kim H, Chang M, Rose K, Kim S. Predictors of caregiver burden in caregivers of individuals with dementia. J Adv Nurs. 2012;68:846–55.
Tyrrell M, Hillerås P, Skovdahl K, Fossum B, Religa D. (2019). Voices of spouses living with partners with neuropsychiatric symptoms related to dementia. Dementia. 2019;18(3):903–19.
Connors MH, Seeher K, Teixeira-Pinto A, Woodward M, Ames D, Brodaty H. Dementia and caregiver burden: a three-year longitudinal study. Int J Geriatr Psychiatry. 2020;35(2):250–8. https://doi.org/10.1002/gps.5244.
Bandura A. Guide for constructing self-efficacy scales (Chap. 14). Self-efficacy beliefs of adolescents. Charlotte, North Carolina: Information Age Publishing; 2005. p. 307. Retrieved from https://www.uky.edu/eushe2/Bandura/BanduraGuide2006.pdf.
Merrilees JJ, Bernstein A, Dulaney S, Heunis J, Walker R, Rah E, Choi J, Gawlas K, Carroll S, Ong P, Feuer J, Braley T, Clark AM, Lee K, Chiong W, Bonasera SJ, Miller BL, Possin KL. The Care Ecosystem: promoting self-efficacy among dementia family caregivers. Dementia. 2018;19:6.
van der Lee J, Bakker TJ, Duivenvoorden HJ, Droes RM. Multivariate models of subjective caregiver burden in dementia: a systematic review. Ageing Res Rev. 2014;15:76–93. https://doi.org/10.1016/j.arr.2014.03.003.
Samia LW, O’Sullivan A, Fallon KC, Aboueissa A, Hepburn KW. Building on self-efficacy for experienced family caregivers: the Savvy Advanced Program. Gerontologist. 2018;00(00):1–11.
Tremont G, Davis JD, Papandonatos GD, Ott BR, Fortinsky RH, Gozalo P, Yue MS, et al. Psychosocial telephone intervention for dementia caregivers: a randomized, controlled trial. Alzheimer’s Dement. 2015;11:541–8.
Jackson D, Roberts G, Wu ML, Ford R, Doyle C. A systematic review of the effect of telephone, internet or combined support for car ers of people living with Alzheimer’s, vascular or mixed dementia in the community. Arch Gerontol Geriatr. 2016;66:218–36.
Alzheimer’s Society. Dementia 2014: Opportunity for change. UK: Alzheimer’s Society; 2014. Retrieved from https://www.alzheimers.org.uk/sites/default/files/migrate/downloads/dementia_2014_opportunity_for_change.
Hinton L, Tran D, Nguyen TN, Ho J, Gitlin L. Interventions to support family caregivers of people living with dementia in high, middle and low-income countries in Asia: a scoping review. BMJ Global Health. 2019;4:e001830.
Kwok T, Wong B, Ip I, Chui K, Young D, Ho F. Telephone-delivered psychoeducational intervention for Hong Kong Chinese dementia caregivers: a single-blinded randomized controlled trial. Clin Interv Aging. 2013;8:1191–97. https://doi.org/10.2147/cia.S48264.
Tremont G, Davis JD, Bishop DS, Fortinsky RH. Telephone-delivered psychosocial intervention reduces burden in dementia caregive rs. Dementia. 2008;7(4):503–20.
Alzheimer’s Disease International. World Alzheimer’s Report. 2015: The global impact of dementia, an analysis of prevalence, incidence cost and trend. London: Alzheimer’s Disease International; 2015. Retrieved from https://www.alzint.org/resource/world-alzheimer-report-2015/.
Mutalib ASA, Dahlan A, Danis A, Masuri MG. Independency and quality of life amongst malay older people in the community: an interpretative phenomenological analysis. Procedia Soc Behav Sci. 2016;234:90–7. https://doi.org/10.1016/j.sbspro.2016.10.223.
NurFatihah OA, Rahman MA, Rosnah S, Ismail D, Khadijah S, ShEzat SP. Quality of life among caregivers of elderly with dementia and its associated factors. IOSR J Nurs Health Sci. 2013;1:7–13.
Tremont G, Davis J, Papandonatos GD, Grover C, Ott BR, Fortinsky RH, Gozalo P, et al. A telephone intervention for dementia caregivers: background, design, and baseline characteristics. Contemp Clin Trials. 2013;36(2):338–47.
Meichsner F, Theurer C, Wilz G. (2019). Acceptance and treatment effects of an internet-delivered cognitive‐behavioral intervention for family caregivers of people with dementia: A randomized‐controlled trial. J Clin Psychol. 2019; 75(4):594–613.
Polit DF, Beck CT. Nursing research: Generating and assessing evidence for nursing practice. Wolters Kluwer Health: Lippincott Williams & Wilkins; 2017.
Ng CG, Nurasikin MS, Loh HS, Anne Yee HA, Zainal NZ. Factorial validation of the malay version of multidimensional scale of perceived social support among a group of psychiatric patients. Malaysian J Psychiatry 2012;21.
Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimesional scale of perceived social support. J Pers Assess. 1988;52:30–41. https://doi.org/10.1207/s15327752jpa5201_2.
Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20:649–55. https://doi.org/10.1093/geront/20.6.649.
Shim VK, Ng CG, Drahman I. Validation of malay version of Zarit Burden interview (MZBI). Malaysian J Psychiatry. 2018;26(2):3–18.
Yahya F, Othman Z. Validation of the malay version of hospital anxiety and Depression Scale (HADS) in hospital university sains Malaysia. Int Med J. 2015;22:80–2.
Nalathamby N, Morgan K, Mat S, Tan PJ, Kamaruzzaman SB, Tan MP. Validation of the CASP-19 quality of life measure in three languages in Malaysia. J Trop Psychol. 2017;7:1–8. https://doi.org/10.1017/jtp.2017.4.
Steffen AM, McKibbin C, Zeiss AM, Gallagher-Thompson D, Bandura A. The revised scale for caregiving self-efficacy: reliability and validity studies. J Gerontol B Psychol. 2002;57(1):P74–86. https://doi.org/10.1093/geronb/57.1.p74.
Sinha P, Desai NG, Prakash O, Kushwaha S, Tripathi CB. Caregiver burden in Alzheimer-type dementia and psychosis: a comparative study from India. Asian J Psychiatry. 2017;26:86–91. https://doi.org/10.1016/j.ajp.2017.01.002.
Panyavin I, Trujillo M, Peralta SV, Stolfi ME, Morelli E, Perrin PB, Peña J, Arango-Lasprilla JC. Examining the influence of family dynamics on quality of care by informal caregivers of patients with Alzheimer’s dementia in Argentina. Am J Alzheimers Disease Other Dement. 2015;30:613–21.
Pillemer S, Davis J, Tremont G. (2018). Gender effects on components of burden and depression among dementia caregivers. Aging Ment Health. 2018;22(9):1156–61. https://doi.org/10.1080/13607863.2017.1337718.
Jutkowitz E, Mitchell LL, Bardenheier BH, Gaugler JE. Profiles of caregiving arrangements of community-dwelling people living with probable dementia. J Aging Soc Policy. 2022;34(6):860–75. https://doi.org/10.1080/08959420.2021.1927613.
Kokorelias KM, Nguyen L, Elane G, Wasilewski MB, Rittenberg N, Cameron JI. Daughters’ experiences of shared caregiving to a parent with dementia. Scand J Caring Sci. 2021;35(3):853–59. https://doi.org/10.1111/scs.12901.
Haro JM, Kahle-Wrobleski K, Bruno G, Belger M, Dell’Agnello G, Dodel R, et al. Analysis of burden in caregivers of people with Alzheimer’s disease using self-report and supervision hours. J Nutr Health Aging. 2014;18(7):677–84. https://doi.org/10.1007/s12603-014-0500-x.
Tan KP, Ang JK, Koh EBY, Pang NTP, Mat Saher Z. Relationship of psychological flexibility and mindfulness to Caregiver Burden, and depressive and anxiety symptoms in caregivers of people with dementia. Int J Environ Res Public Health. 2023;20:5. https://doi.org/10.3390/ijerph20054232.
Krutter S, Schaffler-Schaden D, Essl-Maurer R, Wurm L, Seymer A, Kriechmayr C, et al. Comparing perspectives of family caregivers and healthcare professionals regarding caregiver burden in dementia care: results of a mixed methods study in a rural setting. Age Ageing. 2020;49(2):199–207. https://doi.org/10.1093/ageing/afz165.
Collins RN, Kishita N. Prevalence of depression and burden among informal care-givers of people with dementia: a meta-analysis. Ageing Soc. 2020;40(11):2355–92. https://doi.org/10.1017/S0144686X19000527.
Khanal B, Chalise H. Caregiver Burden among Informal caregivers of Rural Older persons in Nepal. J Health Care Res. 2020;1(3):149–56. https://doi.org/10.36502/2020/hcr.6173.
Kaddour L, Kishita N. Anxiety in Informal Dementia carers: a Meta-analysis of prevalence. J Geriatr Psychiatry Neurol. 2020;33(3):161–72. https://doi.org/10.1177/0891988719868313.
Chan EY, Glass G, Chua KC, Ali N, Lim WS. Relationship between mastery and caregiving competence in protecting against Burden, anxiety and depression among caregivers of Frail older adults. J Nutr Health Aging. 2018;22(10):1238–45. https://doi.org/10.1007/s12603-018-1098-1.
Nemcikova M, Katreniakova Z, Nagyova I. Social support, positive caregiving experience, and caregiver burden in informal caregivers of older adults with dementia. Front Public Health. 2023;11:1104250. https://doi.org/10.3389/fpubh.2023.1104250.
Wang Q, Xiao X, Zhang J, Jiang D, Wilson A, Qian B, et al. The experiences of east Asian dementia caregivers in filial culture: a systematic review and meta-analysis. Front Psychiatry. 2023;14:1173755. https://doi.org/10.3389/fpsyt.2023.1173755.
Tan GTH, Yuan Q, Devi F, Wang P, Ng LL, Goveas R, et al. Factors associated with caregiving self-efficacy among primary informal caregivers of persons with dementia in Singapore. BMC Geriatr. 2021;21:13. https://doi.org/10.1186/s12877-020-01951-8.
Colloby S, Whiting S, Warren A. Supporting the couple relationship following dementia diagnosis: a scoping review. Health Soc Care Community. 2022;30(6):e3643–55. https://doi.org/10.1111/hsc.14006.
Tew CW, Tan LF, Luo N, Ng WY, Yap P. Why family caregivers choose to institutionalize a loved one with dementia: a Singapore perspective. Dement Geriatr Cogn Disord. 2010;30(6):509–16.
Acknowledgements
The authors thank all clinic nurses and research assistants involved in helping the data collection. The authors also express gratitude to the family caregivers to PWD who participated in the study for generously giving their time and energy and providing personal details to the interviews.
Funding
The study was supported by grants from the Ministry of Higher Education, Malaysia under the Fundamental Research Grant Scheme (IIUM/504/RES/G/14/3/2/1/FRGS21-210-0819).
Author information
Authors and Affiliations
Contributions
H.E.N., Z.N.K., M.A.M.A., and K.H.A.A. participated in the planning and conception of the research questions and the study design. H.E.N. was the principal investigator of the study and primarily conceptualized the research. S.A.B.S.A., N.M.Z., and N.B.M.T. were responsible for retrieving the data. H.E.N. was responsible for analysing the data. H.E.N., Z.N.K., M.T., S.V., and A.C. participated in interpreting the data and drafted the article. H.E.N., Z.N.K., M.T., S.V., and A.C. critically revised the manuscript for important intellectual content. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study was approved by the Malaysia Medical Research and Ethics Committee [NMRR-22-00137-BUY(IRR)], the IIUM Research Ethics committee [IREC 2022-007] and the Research Ethics committee of Universiti Kebangsaan Malaysia [UKM PPI/111/8/JEP-2022-328]. Participants were informed in detail about the study and the interviews were conducted after obtaining their informed consent.
Consent for publication
Not applicable.
Competing interests
All authors declare that there are no personal, organizational, or financial conflicts of interest.
Authors’ information
Hashima E Nasreen, MBBS, MPH, PhD, Associate Professor of Epidemiology, Department of Community Medicine, Faculty of Medicine, International Islamic University Malaysia, Kuantan Campus, Pahang, Malaysia.
Marie Tyrrell, Associate Professor, Sophiahemmet Högskola, Valhallavägen, Stockholm, Sweden.
Sofia Vikström, PhD, Senior Lecturer, Department of Neurobiology, Care Sciences and Society, Division of Occupational Therapy, Karolinska Institutet, Stockholm, Sweden.
Åsa Craftman, PhD, Senior Lecturer, Department of Neurobiology, Care Sciences and Society, Division of Nursing, Karolinska Institutet, Stockholm, Sweden.
Syarifah Amirah Binti Syed Ahmad, Candidate for Masters in Medical Science, Department of Community Medicine, Faculty of Medicine, International Islamic University Malaysia, Kuantan Campus, Pahang, Malaysia.
Karimah Hanim Abd Aziz, MD, DrPH, Assistant Professor, Department of Community Medicine, Faculty of Medicine, International Islamic University Malaysia, Kuantan Campus, Pahang, Malaysia.
Noorlaili Binti Mohd Tohit, MD, MMeD, PhD, Associate Professor, Department of Family Medicine, Universiti Kebangsaan Malaysia, 56000 Bandar Tun Razak, Kuala Lumpur, Malaysia.
Nora Mat Zin, MD, MMeD, Associate Professor, Department of Psychoiatry, Faculty of Medicine, International Islamic University Malaysia, Kuantan Campus, Pahang, Malaysia.
Mohd Aznan Md Arid, MBBS, MMeD, Professor, Department of Family Medicine, Faculty of Medicine, International Islamic University Malaysia, Kuantan Campus, Pahang, Malaysia.
Zarina Nahar Kabir, PhD, Associate Professor of Public Health and Principal Researcher, Department of Neurobiology, Care Sciences and Society, Division of Nursing, Karolinska Institutet, Stockholm, Sweden.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nasreen, H.E., Tyrrell, M., Vikström, S. et al. Caregiver burden, mental health, quality of life and self-efficacy of family caregivers of persons with dementia in Malaysia: baseline results of a psychoeducational intervention study. BMC Geriatr 24, 656 (2024). https://doi.org/10.1186/s12877-024-05221-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05221-9