Abstract
Background
Falls are a common cause of fractures in older adults. This study aimed to investigate the factors associated with spontaneous falls among people aged ≥ 60 years in southern Iran.
Methods
The baseline data of 2,426 samples from the second stage of the first phase of a prospective cohort, the Bushehr Elderly Health (BEH) program, were included in the analysis. A history of spontaneous falls in the year before recruitment was measured by self-report using a standardized questionnaire. Demographic characteristics, as well as a history of osteoarthritis, rheumatoid arthritis, low back pain, Alzheimer’s disease, epilepsy, depression, and cancer, were measured using standardized questionnaires. A tandem gait (heel-to-toe) exam, as well as laboratory tests, were performed under standard conditions. A multiple logistic regression model was used in the analysis and fitted backwardly using the Hosmer and Lemeshow approach.
Results
The mean (standard deviation) age of the participants was 69.34 (6.4) years, and 51.9% of the participants were women. A total of 260 (10.7%, 95% CI (9.5–12.0)%) participants reported a spontaneous fall in the year before recruitment. Adjusted for potential confounders, epilepsy (OR = 4.31), cancer (OR = 2.73), depression (OR = 1.81), low back pain (OR = 1.79), and osteoarthritis (OR = 1.49) increased the risk of falls in older adults, while the ability to stand ≥ 10 s in the tandem gait exam (OR = 0.49), being male (OR = 0.60), engaging in physical activity (OR = 0.69), and having high serum triglyceride levels (OR = 0.72) reduced the risk of falls.
Conclusion
The presence of underlying diseases, combined with other risk factors, is significantly associated with an increased risk of falls among older adults. Given the relatively high prevalence of falls in this population, it is crucial to pay special attention to identifying and addressing these risk factors.
Similar content being viewed by others
Introduction
Falling is an unexpected event in which a person moves downward to make contact with the ground, floor, or a lower level [1]. According to the World Health Organization, falls cause 684,000 deaths yearly, making it the second leading cause of unintentional injury deaths [2]. Globally, 30–40% of people over the age of 65 fall at least once a year, with 15% of them falling twice or more [3]. For those over the age of 80, the rate is 50% [4]. A recent study showed that this number is higher in the Middle East region (Gulf Cooperation Council countries: 46.9%) [5]. About 15% of falls result in non-fatal injuries such as bruises, lacerations, and hip fractures, while 23–40% of injury-related deaths in older people are caused by falls [6, 7]. Additionally, 5–10% of falls lead to severe injuries like brain damage [8]. These non-fatal injuries can result in a loss of independence and psychological stress, increasing morbidity in older adults [9, 10]. Studies have shown that after experiencing a fall, the fear of falling again leads to decreased daily mobility, which in turn increases the risk of falling [11, 12]. Approximately 4.1% of falls result in fractures, with hip fractures being associated with the greatest decrease in mobility (a 76% decline) [13, 14]. Overall, falls account for 0.85–1.5% of all healthcare costs [15].
Falling risk factors vary worldwide. These risk factors depend on aging patterns (genetic factors that contribute to different aging conditions) as well as environmental factors such as elder safety programs. Previous studies have identified risk factors such as demographic variables, systemic conditions, cardiovascular disease, neurological and mental disorders, medication, and location [3, 16].
According to previous studies, population aging in Asia, especially in East Asia, is on the rise [17, 18]. Given the knowledge about injuries related to falls, it is crucial to determine their prevalence in different groups and the associated factors in all regions of the world. Few studies on falls among older adults have been conducted in our region, and these studies have shown relatively significant differences in results [5]. The importance of investigating these differences is to establish preventive measures. In this study, we aim to investigate falls and their associated factors in a southern province of Iran for the first time.
Methods
Study design
The present study is a cross-sectional analysis that utilizes the baseline data collected during the second stage of the initial phase of the ongoing Bushehr Elderly Health Program (BEHP) [19, 20]. BEHP is a multi-phasic, population-based prospective cohort study conducted in a southern city of Iran. Its focus is on studying non-communicable diseases and their associated risk factors. In the first stage of the first phase, 3000 participants over 60 years old were studied regarding cardiovascular risk factors and events [19]. The second stage of the first phase of BEHP focused on musculoskeletal and cognitive diseases and started in 2015 with 2426 participants from the previous stage [20]. Sampling for this study was done using a multistage cluster random method from the population living in 75 strata in Bushehr city. The detailed methodology of BEHP is mentioned in its protocol [19, 20]. The study was approved by the Research Ethics Committee of Bushehr University of Medical Sciences (Ethical Code: B-91-14-2) and the Ethical Board Committee of the Endocrinology & Metabolism Research Institute of Tehran University of Medical Sciences (Ethical Code: IR.TUMS.EMRI.REC.1394.0036). Enrolled patients signed a written consent form after the study’s objectives were explained by the interviewer.
Measurements
In the second stage of the first phase of the BEHP, the data were collected through standardized questionnaires, physical examination, dual x-ray absorptiometry, and laboratory tests [20].
A history of spontaneous falls in the year before recruitment was measured through self-report using a standardized questionnaire (see Additional file 1). Demographic characteristics, as well as the history of smoking alongside past medical history including osteoarthritis, rheumatoid arthritis, low back pain, Alzheimer’s disease, epilepsy, depression, and cancer, were measured using standardized questionnaires (see Additional file 1).
The physical activity level over a 24-hour period, including sports, work, and leisure time on an average weekday, was assessed using a validated self-report questionnaire that ranked activities based on nine metabolic equivalents (0.9 to > 6 METs) [21, 22]. The time spent on each activity was multiplied by the MET level to calculate a MET.time sum for the entire day [21, 23]. All data were collected by a trained nurse. Height and weight were measured with a fixed stadiometer and a digital scale following the standard protocol. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured using a standardized mercury sphygmomanometer on the right arm after 15 min of rest in a seated position. The first and fifth Korotkoff sounds were recorded as SBP and DBP, respectively. The average of the two readings was calculated as the participant’s blood pressure. During the full tandem balance test, the interviewer assists by supporting one arm while participants position their feet. The interviewer then asks if they are ready and subsequently releases the support, commencing the timing. The timer is stopped either after 10 s have passed or if participants move their feet. Body composition for each participant is measured using dual x-ray absorptiometry (DXA, Discovery WI, Hologic, Bedford, Virginia, USA). This measurement includes: (1) bone mineral density in the lumbar spine and hip, (2) appendicular skeletal muscle mass, and (3) the skeletal muscle mass index. Osteoporosis was defined as a T-score ≤ -2.5 (in any sex compared to the BMD of a young, healthy Caucasian person of the same sex) at any site of total hip, spine, or neck of femur.
An overnight fasting venous blood sample of 25 cc was obtained from each participant for all laboratory tests and bio-bank studies of the first phase of the study. Laboratory tests including lipid profiles, fasting blood sugar, and HbA1c were performed under standard conditions [20].
Statistical analysis
For describing continuous variables, we used the mean (standard deviation). For categorical variables, we presented the number (percent). The simple logistic regression model investigated the association between each risk factor and the history of spontaneous falls in the previous year. Following risk factors were assessed: age, gender, education, high levels of cholesterol, high levels of low-density lipoprotein (LDL), high levels of triglyceride, low levels of high-density lipoprotein (HDL), physical activity, osteoporosis, past medical history of disease (osteoarthritis, rheumatoid arthritis, back pain, Alzheimer, seizure, depression, and cancer), balance status, type 2 diabetes mellitus, hypertension, smoking status, and body mass index (BMI). To adjust for potential confounding effects, risk factors with a P-value of ≤ 0.25 in their association with the outcome in the previous analysis were entered into the multiple logistic model and were removed from the model based on the likelihood ratio test results. We used the strategy suggested by Hosmer and Lemeshow for model fitting [24, 25]. All analyses were carried out using STATA (Version 15.1), and a P-value of 0.05 was considered significant.
Results
A total of 2,426 older adults participated in this stage of the BEHP, and their data were used in the analysis. The mean age of the participants was 69.34 (± 6.4) years (range: 60 to 96). Of the overall 2,426 participants, 1,166 (48.06%) were men. Table 1 shows their socio-demographic characteristics.
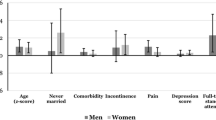
260 (10.73%) of the participants experienced falling in the last year of the study (95% CI: 9.55–12.02). Table 2 demonstrates the association between the risk factors and falling, utilizing simple logistic model analysis, alongside the number of falls in each group. The following variables were not presented in Table 2 since the P-value of the association between fall and these variables was > 0.25: type 2 diabetes mellitus, hypertension, low levels of HDL, smoking status, and BMI. In this analysis, age 65–69 (Crude OR = 0.69, 95% CI: 0.49–0.96, p = 0.03), male sex (0.44, 95% CI: 0.33–0.58, p < 0.001), having any levels of formal education above primary school (guidance school: 0.53, 95% CI: 0.30–0.93, p = 0.03; high school (trended towards significance): 0.66, 95% CI: 0.42–1.02, p = 0.06; academic degree: 0.53, 95% CI: 0.29–0.97, p = 0.04), higher degrees of physical activity (0.60, 95% CI: 0.42–0.85, p = 0.004), and the ability to stand ≥ 10 s in the tandem gait (0.37, 95% CI: 0.27–0.50, p < 0.001) were significantly associated with lower falls. Meanwhile, a diagnosis of epilepsy (3.91, 95% CI: 1.47–10.37, p = 0.006), cancer (3.12, 95% CI: 1.30–7.50, p = 0.01), rheumatoid arthritis (2.86, 95% CI: 1.47–5.56, p = 0.002), depression (2.20, 95% CI: 1.34–3.62, p = 0.002), low back pain (2.17, 95% CI: 1.65–2.86, p < 0.001), osteoarthritis (1.83, 95% CI: 1.31–2.55, p < 0.001), and osteoporosis (1.57, 95% CI: 1.21–2.03, p = 0.001) significantly correlated with higher fall rates.
After adjusting for potential confounders using multiple logistic regression analysis, the overall falling rates were significantly and independently lower in men (adjusted OR = 0.60, 95% CI: 0.44–0.81, p = 0.001), the participants aged 65 to 74 but not the patients older than 75 (65–69 y: 0.62, 95% CI: 0.44–0.88, p = 0.01; 70–74 y: 0.59, 95% CI: 0.38–0.93, p = 0.02), higher physical activity at the time of the study (0.69, 95% CI: 0.48–0.99, p = 0.046), and participants with higher triglyceride levels above 150 mg/dL (0.72, 95% CI: 0.53–0.97, p = 0.03) (Table 3). The ability to stand more than 10 s in the tandem gait examination was also significantly associated with lower falls (0.49, 95% CI: 0.35–0.69, p < 0.001). Fall rates increased in people with a history of epilepsy (4.31, 95% CI: 1.54–12.07, p = 0.005), cancer (2.73, 95% CI: 1.09–6.84, p = 0.005), depression (1.81, 95% CI: 1.08–3.06, p = 0.02), low back pain (1.79, 95% CI: 1.33–2.40, p < 0.001), and osteoarthritis (1.49, 95% CI: 1.05–2.11, p = 0.02). As shown above, a diagnosis of epilepsy posed the highest risk of falling among the aforementioned risk factors.
Discussion
This study found that, adjusted for potential confounders, having epilepsy, cancer, depression, low back pain, and osteoarthritis is associated with an increased risk of spontaneous falls in older adults. Moreover, the ability to maintain a tandem gait for ≥ 10 s, being male, engaging in physical activity during the study, and having high serum triglyceride levels are associated with a decreased risk of falls.
Our results show that epilepsy can be associated with an increased risk of falling. Epilepsy, with or without seizures, can cause different fall-related injuries, including fractures (two-fold increase), concussion, and cranial hemorrhage [26,27,28]. One reason is directly related to the seizure episodes and loss of consciousness, while another reason is complications such as reduced bone density, dizziness/sedation, ataxia/gait disturbance (caused by hyperammonemia), and cognitive impairment caused by antiepileptic drugs [29,30,31,32]. On the other hand, low compliance with antiepileptic drugs can also lead to injuries. Antiepileptic drugs in old age have other uses as well, such as for mood disturbance and neuropathic pain [33]. Management of epilepsy in the elderly has controversial details, such as the cost-benefits of prescribing antiepileptic drugs. It seems that the best solution to decrease the risk of falling is tight medical control and consultation on avoiding risky behaviors in elders with epilepsy [28].
Based on the results of this study, it appears that one of the events that occurs in individuals with cancer is falling. More than half of diagnosed cancers occur in people over 65 years old [34, 35]. The toxic effects of chemotherapeutic treatments on different body systems may be an important cause of falls. For example, chemotherapy can cause limb neuropathy, resulting in poor balance [36]. Additionally, other complications such as muscle weakness, frailty, brain and central nervous system metastases, cognitive impairment, depression, and polypharmacy are more common in older adults with cancer [35]. Furthermore, some patients with cancer may face an increased risk of injury and fractures after falls due to factors such as osteoporosis related to parathyroid-related peptides (PTHrp), bone invasion, and metastasis [35]. Because of the nature of cancers, fall-related hospitalization can increase the mortality rate in patients. Therefore, balancing the therapeutic and toxic effects of chemotherapy, especially in high-risk patients, is recommended. Recent studies show that performing a geriatric assessment before cancer treatment could decrease its negative impacts [37].
Neurological diseases (such as Alzheimer’s disease, Parkinson’s disease, and stroke) can increase the risk of falling, and as high as 60–80% of the elderly with dementia experience falling annually. For many years, gait and postural instability were considered the major risk factors for falling; however, some studies have shown that elders’ cognitive state also plays an important role [38,39,40]. The exact link between depression and falls is unclear, but a recent study showed that isolation and depressive symptoms could increase the risk of falls by 30% [41]. Maintaining balance requires a fast and accurate response to perturbation. This response includes physiological and cognitive factors that all come together as reaction time [42,43,44]. Due to the increasing prevalence of depression, cognitive assessment must be a part of any preventive program. However, the main challenge is whether to treat depression in fall-prone elders or not. Antidepressants often have side effects such as orthostatic hypotension, impaired attention, and movement disorders. Additionally, studies have suggested polypharmacy and withdrawal syndrome as risk factors for falling [45, 46]. In this regard, other approaches like Cognitive Behavioral Therapy could be helpful [46, 47].
Musculoskeletal pains increase with aging. Back pain is more common in developing countries [48, 49]. It causes limited physical activity, reduces muscle strength, and has psychological effects such as isolation [38, 50]. Recent studies have focused on low back pain as an independent risk factor for falling [51, 52]. In a recent study, Wong et al. found that chronic lower back pain is significantly associated with osteoarthritis [53]. Patients with low back pain or osteoarthritis have extended degrees of disability, increasing the risk of falling. It also has a synergetic negative effect on the quality of life and abilities of elders [54, 55]. These two factors can also cause higher morbidity after falls, such as fractures [56]. Some studies have shown that low back pain is associated with abdominotrunkal muscle weakness, and patients with pain are predisposed to falling due to its psycho-cognitive effects [57, 58].
We suggest physical activity as a protective factor against falls among the elderly. Exercise and physical activity reduce physical and mental risk factors for falling, prevent sarcopenia, and improve balance and Body Mass Index (BMI) among underweight subjects, as past studies have shown that lower BMI increases fall risk [4]. Additionally, the elderly who exercise more often have less fear of falling as a psychological factor [59]. However, while usual physical activity is beneficial, daily activities like walking need to be a part of a comprehensive strength and balance training program to be effective, as routine life activity cannot be considered an effective tool for preventing falls [60].
We suggest a tandem gait test for assessing the risk of falling in older adults. Our results show that older adults who are able to stand for at least 10 s in the tandem gait exam are less likely to fall. Some recent studies focus on gait features as an accurate classifier for the risk of falling in older adults [61].
Our findings show that high levels of serum triglycerides could be a preventive factor for falling in older adults. The adverse effects of metabolic syndrome in middle age are not applicable to everyone. However, some findings show that in elderly people, metabolic syndrome and its related components can have a positive impact on daily and cognitive function [62]. One possible explanation is that elderly individuals with higher levels of serum triglycerides may lack other more significant risk factors such as muscle mass loss, grip strength, poor nutritional state, etc., which play a greater role in the risk of falling. Another possible explanation at the molecular level involves peroxisome proliferator-activated receptor (PPAR-gamma). PPAR-gamma plays a role in fat tissue differentiation and fatty acid metabolism. More importantly, it has an anti-inflammatory and protective role against cell apoptosis in the central nervous system and skeletal muscles [63, 64]. Further studies are needed to determine the threshold for treating high levels of serum triglycerides in individuals at high risk of falling.
Our results show that older women are more prone to falling. Despite the lower mortality rate of falls in women, conditions such as hip fractures are more common in women. One possible explanation is that the aging process in women is associated with greater muscle mass loss.
Due to the multifactorial nature of falls, we need to approach them differently and design programs that take into account the unique characteristics of each population. Studies have shown that these interventions can reduce falls by 20-40% [65]. Programs such as Stopping Elderly Accidents, Deaths & Injuries (STEADI) (designed by the CDC), the Otago Exercise Program, or the Lifestyle-integrated Functional Exercise Program focus on modifiable risk factors and include screening conducted by physicians to implement preventive measures such as medication adjustment, balance improvement, and physical therapy [60, 66, 67]. Such programs are necessary due to the increasing population of individuals over 65 years old, and especially those over 85.
Since the BEH program did not include people living in nursing homes, our findings may underestimate the rate of falls [20, 68]. Additionally, when interpreting the results, attention should be given to the cross-sectional nature of the study design and the possibility of a reverse causation phenomenon, as well as the potential presence of unknown confounding factors. Furthermore, some studies suggest that low back pain is associated with osteoarthritis, which could lead to misinterpretation if each of these factors is considered an independent risk factor for falling [51].
Limitations and strength
This study was conducted using data from a large cohort study that focused on the health of the elderly. The aim of the study was to determine the factors contributing to spontaneous falls in this population. The large number of participants and the specific target population of this cohort made it appropriate for the purpose of this study.
However, this study does have some limitations. The scope of the study did not permit a comprehensive analysis of rare diseases or risk factors like alcohol abuse. Specific subtypes of the underlying conditions mentioned, such as various types of epilepsy or specific cancer subtypes, were not examined in detail. Moreover, the absence of data on potential risk factors for falls (e.g., number of medications) limited the ability to study the impact of these factors or address their potential confounding effects. Lastly, as the study was based on cross-sectional data from the baseline measurements of the BEHP, we can only report associations and not establish causal relationships. Further research utilizing follow-up data from cohort studies is necessary to establish causal relationships.
Conclusions
The elderly are at an increased risk of falls and subsequent complications. The presence of underlying diseases, combined with other risk factors such as older age, lower physical activity, and female sex, is associated with a significantly increased risk of falls among older adults. Therefore, this population requires preventive measures to identify and address their increased risk of falls, as well as specific attention and care to minimize the incidence of falls and their complications.
Data availability
Data supporting this study are available from the principal investigator (Dr. Iraj Nabipour, Email: inabipour@gmail.com) of Bushehr Elderly Health (BEH) program. However, the data were used under license for the current study and are not publicly available; so, restrictions apply to the availability of these data.
References
Duthie EH. Falls. Med Clin North Am. 1989;73:1321–36. https://doi.org/10.1016/S0025-7125(16)30601-0.
Falls. https://www.who.int/multi-media/details/falls. Accessed 27 May 2022.
Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75:51–61. https://doi.org/10.1016/J.MATURITAS.2013.02.009.
Phelan EA, Ritchey K. Fall Prevention in Community-Dwelling older adults. Ann Intern Med. 2018;169:ITC81–96. https://doi.org/10.7326/AITC201812040.
Alqahtani BA, Alshehri MM, Hoover JC, Alenazi AM. Prevalence of falls among older adults in the Gulf Cooperation Council countries: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2019;83:169–74. https://doi.org/10.1016/J.ARCHGER.2019.04.006.
Mager DR. Orthostatic hypotension: pathophysiology, problems, and prevention. Home Healthc Nurse. 2012;30:525–30. https://doi.org/10.1097/NHH.0B013E31826A6805.
Secretariat MA. Prevention of Falls and fall-related injuries in Community-Dwelling seniors: an evidence-based analysis. Ont Health Technol Assess Ser. 2008;8:1.
Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;18:141–58. https://doi.org/10.1016/S0749-0690(02)00002-2.
King MB, Tinetti ME. Falls in community-dwelling older persons. J Am Geriatr Soc. 1995;43:1146–54. https://doi.org/10.1111/J.1532-5415.1995.TB07017.X.
Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001;50:116–9. https://doi.org/10.1097/00005373-200101000-00021.
Denkinger MD, Lukas A, Nikolaus T, Hauer K. Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: a systematic review. Am J Geriatr Psychiatry. 2015;23:72–86. https://doi.org/10.1016/J.JAGP.2014.03.002.
Tinetti ME, Franklin Williams T, Mayewski R. Fall risk index for elderly patients based on number of chronic disabilities. Am J Med. 1986;80:429–34. https://doi.org/10.1016/0002-9343(86)90717-5.
Goldacre MJ, Roberts SE, Yeates D. Mortality after admission to hospital with fractured neck of femur: database study. BMJ. 2002;325:868–9. https://doi.org/10.1136/BMJ.325.7369.868.
How best to fix a broken hip | The Medical Journal of Australia. https://www.mja.com.au/journal/1999/170/10/how-best-fix-broken-hip. Accessed 27 May 2022.
Heinrich S, Rapp K, Rissmann U, et al. Cost of falls in old age: a systematic review. Osteoporos Int. 2010;21:891–902. https://doi.org/10.1007/S00198-009-1100-1.
Gazibara T, Kurtagic I, Kisic-Tepavcevic D, et al. Falls, risk factors and fear of falling among persons older than 65 years of age. Psychogeriatrics. 2017;17:215–23. https://doi.org/10.1111/PSYG.12217.
MENA Generation 2030 - UNICEF DATA. https://data.unicef.org/resources/middle-east-north-africa-generation-2030/. Accessed 3 Jun 2022.
Mate K, Bryan C, Deen N, McCall J. Review of Health systems of the Middle East and North Africa Region. Int Encyclopedia Public Health. 2017;347. https://doi.org/10.1016/B978-0-12-803678-5.00303-9.
Ostovar A, Nabipour I, Larijani B, et al. Bushehr elderly health (BEH) Programme, phase i (cardiovascular system). BMJ Open. 2015;5. https://doi.org/10.1136/BMJOPEN-2015-009597.
Shafiee G, Ostovar A, Heshmat R, et al. Bushehr Elderly Health (BEH) programme: study protocol and design of musculoskeletal system and cognitive function (stage II). BMJ open. 2017;7. https://doi.org/10.1136/BMJOPEN-2016-013606.
Aadahl M, Jørgensen T. Validation of a new self-report instrument for measuring physical activity. Med Sci Sports Exerc. 2003;35:1196–202. https://doi.org/10.1249/01.MSS.0000074446.02192.14.
Kelishadi R, Famuri F, Sadeghi M. Assessment of physical activity of adolescents in Isfahan. J Shahrekord Univ Med Sci. 2001;3:27–33.
Aadahl M, Andreasen AH, Hammer Helmich L, et al. Recent temporal trends in sleep duration, domain-specific sedentary behaviour and physical activity. A survey among 25-79-year-old Danish adults. Scand J Public Health. 2013;41:706–11. https://doi.org/10.1177/1403494813493151.
Jewell NP. Statistics for epidemiology. Chapman & Hall/CRC; 2004.
Vellas B, Guigoz Y, Garry PJ, et al. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition. 1999;15:116–22. https://doi.org/10.1016/S0899-9007(98)00171-3.
O’loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137:342–54. https://doi.org/10.1093/OXFORDJOURNALS.AJE.A116681.
Kannus P, Sievänen H, Palvanen M, et al. Prevention of falls and consequent injuries in elderly people. Lancet (London England). 2005;366:1885–93. https://doi.org/10.1016/S0140-6736(05)67604-0.
Saengsuwan J, Laohasiriwong W, Boonyaleepan S, et al. Seizure-related vehicular crashes and falls with injuries for people with epilepsy (PWE) in northeastern Thailand. Epilepsy Behavior: E&B. 2014;32:49–54. https://doi.org/10.1016/J.YEBEH.2013.12.021.
Wirrell EC. Epilepsy-related injuries. Epilepsia 47 Suppl. 2006;179–86. https://doi.org/10.1111/J.1528-1167.2006.00666.X.
Huang AR, Mallet L, Rochefort CM, et al. Medication-related falls in the elderly: causative factors and preventive strategies. Drugs Aging. 2012;29:359–76. https://doi.org/10.2165/11599460-000000000-00000.
Deandrea S, Lucenteforte E, Bravi F, et al. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiol (Cambridge Mass). 2010;21:658–68. https://doi.org/10.1097/EDE.0B013E3181E89905.
Souverein PC, Webb DJ, Weil JG, et al. Use of antiepileptic drugs and risk of fractures: case-control study among patients with epilepsy. Neurology. 2006;66:1318–24. https://doi.org/10.1212/01.WNL.0000210503.89488.88.
Johnell K, Fastbom J. Antiepileptic drug use in community-dwelling and institutionalized elderly: a nationwide study of over 1,300,000 older people. Eur J Clin Pharmacol. 2011;67:1069–75. https://doi.org/10.1007/S00228-011-1051-2.
Maddams J, Utley M, Møller H. Projections of cancer prevalence in the United Kingdom, 2010–2040. Br J Cancer. 2012;107:1195–202. https://doi.org/10.1038/BJC.2012.366.
Stone CA, Lawlor PG, Savva GM, et al. Prospective study of falls and risk factors for falls in adults with advanced cancer. J Clin Oncology: Official J Am Soc Clin Oncol. 2012;30:2128–33. https://doi.org/10.1200/JCO.2011.40.7791.
Bao T, Basal C, Seluzicki C, et al. Long-term chemotherapy-induced peripheral neuropathy among breast cancer survivors: prevalence, risk factors, and fall risk. Breast Cancer Res Treat. 2016;159:327–33. https://doi.org/10.1007/S10549-016-3939-0.
Mohile SG, Mohamed MR, Xu H, et al. Evaluation of geriatric assessment and management on the toxic effects of cancer treatment (GAP70+): a cluster-randomised study. Lancet (London England). 2021;398:1894–904. https://doi.org/10.1016/S0140-6736(21)01789-X.
Cuevas-Trisan R. Balance problems and fall risks in the Elderly. Phys Med Rehabil Clin North Am. 2017;28:727–37. https://doi.org/10.1016/J.PMR.2017.06.006.
Booth V, Harwood R, Hood V, et al. Understanding the theoretical underpinning of the exercise component in a fall prevention programme for older adults with mild dementia: a realist review protocol. Syst Reviews. 2016;5. https://doi.org/10.1186/S13643-016-0212-X.
Shaw FE, Bond J, Richardson DA, et al. Multifactorial intervention after a fall in older people with cognitive impairment and dementia presenting to the accident and emergency department: randomised controlled trial. BMJ (Clinical Res ed). 2003;326:73–5. https://doi.org/10.1136/BMJ.326.7380.73.
Quach LT, Burr JA. Perceived social isolation, social disconnectedness and falls: the mediating role of depression. Aging Ment Health. 2021;25:1029–34. https://doi.org/10.1080/13607863.2020.1732294.
Richardson JK. Imbalanced: the confusing circular nature of Falls Research… and a possible antidote. Am J Phys Med Rehabil. 2017;96:55–9. https://doi.org/10.1097/PHM.0000000000000591.
Lord SR, Menz HB, Sherrington C. Falls in older people. Osteoporos Clin Pract. 2004;93–99. https://doi.org/10.1007/978-0-85729-402-9_12.
Kearney FC, Harwood RH, Gladman JRF, et al. The relationship between executive function and falls and gait abnormalities in older adults: a systematic review. Dement Geriatr Cogn Disord. 2013;36:20–35. https://doi.org/10.1159/000350031.
van Poelgeest EP, Pronk AC, Rhebergen D, van der Velde N. Depression, antidepressants and fall risk: therapeutic dilemmas-a clinical review. Eur Geriatr Med. 2021;12:585–96. https://doi.org/10.1007/S41999-021-00475-7.
Iaboni A, Flint AJ. The complex interplay of depression and falls in older adults: a clinical review. Am J Geriatric Psychiatry: Official J Am Association Geriatric Psychiatry. 2013;21:484–92. https://doi.org/10.1016/J.JAGP.2013.01.008.
Parry SW, Bamford C, Deary V, et al. Cognitive-behavioural therapy-based intervention to reduce fear of falling in older people: therapy development and randomised controlled trial - the strategies for increasing independence, confidence and energy (STRIDE) study. Health technology assessment. (Winchester England). 2016;20:1–206. https://doi.org/10.3310/HTA20560.
Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet (London England). 2018;391:2356–67. https://doi.org/10.1016/S0140-6736(18)30480-X.
Buchbinder R, van Tulder M, Öberg B, et al. Low back pain: a call for action. Lancet (London England). 2018;391:2384–8. https://doi.org/10.1016/S0140-6736(18)30488-4.
Tsonga T, Michalopoulou M, Malliou P, et al. Analyzing the history of falls in patients with severe knee osteoarthritis. Clin Orthop Surg. 2015;7:449. https://doi.org/10.4055/CIOS.2015.7.4.449.
Iijima H, Shimoura K, Aoyama T, Takahashi M. Low back Pain as a risk factor for recurrent falls in people with knee osteoarthritis. Arthritis Care Res. 2021;73:328–35. https://doi.org/10.1002/ACR.24136.
Bell T, Pope C, Fazeli P, et al. The Association of Persistent Low Back Pain with older Adult Falls and collisions: a longitudinal analysis. J Appl Gerontology: Official J South Gerontological Soc. 2021;40:1455–64. https://doi.org/10.1177/0733464820966517.
Wong CK, Mak RY, Kwok TS, et al. Prevalence, incidence, and factors Associated with non-specific chronic low back Pain in Community-Dwelling older adults aged 60 years and older: a systematic review and Meta-analysis. J pain. 2022;23:509–34. https://doi.org/10.1016/J.JPAIN.2021.07.012.
Suri P, Morgenroth DC, Kwoh CK, et al. Low back pain and other musculoskeletal pain comorbidities in individuals with symptomatic osteoarthritis of the knee: data from the osteoarthritis initiative. Arthritis Care Res. 2010;62:1715–23. https://doi.org/10.1002/ACR.20324.
Iijima H, Suzuki Y, Aoyama T, Takahashi M. Interaction between low back pain and knee pain contributes to disability level in individuals with knee osteoarthritis: a cross-sectional study. Osteoarthr Cartil. 2018;26:1319–25. https://doi.org/10.1016/J.JOCA.2018.06.012.
Smith TO, Higson E, Pearson M, Mansfield M. Is there an increased risk of falls and fractures in people with early diagnosed hip and knee osteoarthritis? Data from the Osteoarthritis Initiative. Int J Rheum Dis. 2018;21:1193–201. https://doi.org/10.1111/1756-185X.12871.
Kato S, Murakami H, Demura S, et al. Abdominal trunk muscle weakness and its association with chronic low back pain and risk of falling in older women. BMC Musculoskelet Disord. 2019;20. https://doi.org/10.1186/S12891-019-2655-4.
Nakai Y, Takenaka T, Kubozono T, et al. Falls in Community-Dwelling older adults with Lower back or knee Pain are Associated with Cognitive and emotional factors. Int J Environ Res Public Health. 2020;17:1–8. https://doi.org/10.3390/IJERPH17144960.
Kendrick D, Kumar A, Carpenter H et al. (2014) Exercise for reducing fear of falling in older people living in the community. The Cochrane database of systematic reviews 2014:. https://doi.org/10.1002/14651858.CD009848.PUB2.
Gardner MM, Buchner DM, Robertson MC, Campbel AJ. Practical implementation of an exercise-based falls prevention programme. Age Ageing. 2001;30:77–83. https://doi.org/10.1093/AGEING/30.1.77.
Lockhart TE, Soangra R, Yoon H et al. (2021) Prediction of fall risk among community-dwelling older adults using a wearable system. Scientific reports 11:. https://doi.org/10.1038/S41598-021-00458-5.
Association of metabolic. syndrome with falls in patients with Parkinson’s disease - PubMed. https://pubmed.ncbi.nlm.nih.gov/26907583/. Accessed 14 Oct 2022.
Jay M, Ren J. Peroxisome proliferator-activated receptor (PPAR) in metabolic syndrome and type 2 diabetes Mellitus. Curr Diabetes Rev. 2007;3:33–9. https://doi.org/10.2174/157339907779802067.
Swanson C, Emborg M. (2014) Expression of peroxisome proliferator-activated receptor-gamma in the substantia nigra of hemiparkinsonian nonhuman primates. https://doi.org/101179/1743132813Y0000000305 36:634–646. https://doi.org/10.1179/1743132813Y.0000000305.
Gillespie LD, Robertson MC, Gillespie WJ et al. (2012) Interventions for preventing falls in older people living in the community. The Cochrane database of systematic reviews 2012:. https://doi.org/10.1002/14651858.CD007146.PUB3.
Moreland B, Kakara R, Henry A. Trends in Nonfatal Falls and fall-related injuries among adults aged ≥ 65 years — United States, 2012–2018. MMWR Morbidity Mortal Wkly Rep. 2020;69:875–81. https://doi.org/10.15585/MMWR.MM6927A5.
Clemson L, Fiatarone Singh MA, Bundy A, et al. Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): randomised parallel trial. BMJ (Clinical Res ed). 2012;345. https://doi.org/10.1136/BMJ.E4547.
Ostovar A, Nabipour I, Larijani B, et al. Bushehr Elderly Health (BEH) Programme, phase I (cardiovascular system). BMJ Open. 2015;5:9597. https://doi.org/10.1136/BMJOPEN-2015-009597.
Acknowledgements
We would like to thank all the personnel of the Bushehr Elderly Health program and all the people involved in this study.
Funding
No fundings were received for conducting this study.
Author information
Authors and Affiliations
Contributions
K.K: Study design, data collection and analysis, critical revision of the manuscript R.S, A.H.H, H.A, A.K: Study design, Drafting the original manuscript N.F, M.S, M.J.M, I.N, B.L, A.O: Study design, critical revision of the manuscript All the authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol of Bushehr Elderly Health (BEH) program was approved by both ethics committee of Endocrinology and Metabolism Research Institute, affiliated to Tehran University of Medical Sciences (code: IR.TUMS.EMRI.REC.1394.0036), and the Research Ethics Committee of Bushehr University of Medical Sciences (code of ethics: B-91-14-2). All the included patients gave written informed consent to enter the study. Whenever a patient could not read and write, they were asked to be accompanied by a literate person familiar with the local dialect to provide the patient with necessary explanations. Then, the patient and their companion both signed the informed consent after making sure that they both understood all aspects of the study. Ethics committees approved the aforementioned approach. Both ethics committees approved using the BEH program data for the current study.
Consent for publication
The obtained written informed consent included permissions to use the data for publications in domestic or international journals.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Khalagi, K., Hoveidaei, A.H., AziziKia, H. et al. Identifying determinants for falls among Iranian older adults: insights from the Bushehr Elderly Health Program. BMC Geriatr 24, 588 (2024). https://doi.org/10.1186/s12877-024-05180-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05180-1