Abstract
Background
The association between vitamin D supplementation and the risk of falls in older adults has been controversial. This systematic review and network meta-analysis aims to assess the efficacy of vitamin D, calcium, and combined supplementation in the prevention of falls.
Methods
Randomized controlled trials (RCTs) on the efficacy of vitamin D in fall prevention were systematically searched in PubMed, Embase, Cochrane Library, and Web of Science from inception to May 9, 2023. The network meta-analysis was performed using a random effects model in R4.1.3 and Stata15.0. Heterogeneity was evaluated by the I2 statistic, and publication bias was assessed using funnel plots, Begg’s test, and Egger’s tests. Data were pooled and expressed as relative risk (RR) and 95% confidence interval (CI).
Results
A total of 35 RCTs involving 58,937 participants were included in this study, among which 11 RCTs (31.4%) applied calcium combined with vitamin D. There was low heterogeneity (I2 = 11%) among the included studies. Vitamin D supplementation at 800–1000 International Unit (IU)/d resulted in a lower risk of falls than placebo or no treatment (RR = 0.85, 95%CI: 0.74–0.95). In addition, 800–1000 IU/d of vitamin D with or without calcium were more effective in preventing falls than calcium alone. High-dose vitamin D (> 1000 IU/day) increased the risk of falls compared with 800–1000 IU/d of vitamin D. According to the subgroup analysis, daily administration of 800–1000 IU/d vitamin D was associated with a 22% reduction in the risk of falls (RR = 0.78, 95%CI:0.64–0.92), whereas intermittent vitamin D administration had no preventive effect. Furthermore, 800–1000 IU/d of vitamin D also significantly decreased the risk of falls in old adults with ≤ 50 nmol/L 25-hydroxyvitamin D [25(OH)D] (RR = 0.69, 95%CI:0.52–0.86) but not in individuals with > 50 nmol/L 25(OH)D.
Conclusion
Vitamin D supplementation at 800–1000 IU/d is associated with a lower risk of falls among older adults. 800-1000IU/d of vitamin D has a benefit on prevention of falls in population received daily dose regimens and in population with vitamin D deficiency.
Similar content being viewed by others
Background
Falls and fall-related injuries are common and potentially preventable causes of functional disability, morbidity, and increased health-care utilization among older individuals [1]. It was reported that one of every three individuals over 65 years of age has experienced at least one fall, with 5–6% of falls resulting in a fracture [2, 3]. Therefore, fall prevention is paramount for preventing fractures and reducing morbidity and mortality. Fall prevention guidelines have recommended vitamin D as a component of multifactorial interventions along with other strategies such as gait and balance training, home assessment and modifications, reduction or withdrawal of psychotropic drugs, treatment of impaired vision, management of postural hypotension, treatment of heart rate and abnormal heart rhythm, suitable footwear, and education [4, 5].
Vitamin D supplements are commonly taken to maintain bone health. The Bone Health and Osteoporosis Foundation (BHOF) recommends a daily intake of 800 to 1000 units of vitamin D for adults aged 50 years and older [6]. According to the Institute of Medicine (IOM) [7], the recommended daily intake of vitamin D is 600 International Unit (IU) for adults < 70 years of age and 800 IU for those ≥ 70 years of age.
However, previous randomized controlled trials (RCTs) have shown inconsistent effectiveness of vitamin D, calcium, and combined supplementation in fall prevention, which may be attributed to differences in vitamin D doses, mode of administration, and other regimen design features [8]. Previous systematic review and meta-analyses also had different recommendations. A recent meta-analysis reported that vitamin D supplementation had no impact on the incidence of fractures or falls nor clinically meaningful effects on bone mineral density [9]. On the other hand, Wu et al. found that vitamin D combined with calcium, but not vitamin D2 or D3 alone, significant lowered the risk of falls [10]. Similarly, Thanapluetiwong et al. [11] showed that vitamin D3 decreased the incidence of falls only when supplemented with calcium, but neither of the two articles conducted subgroup analysis of different vitamin D doses. Kong et al. revealed that 800–1000 IU/d of vitamin D was associated with lower risks of falls [12]. Ling et al. reported that combined supplementation of vitamin D (daily doses of 700–1000 IU) and calcium resulted in 12% reduction in the risk of falls [13]. Furthermore, Wei et al. found that 700–2000 IU/d of vitamin D was correlated with a lower risk of falls among ambulatory and institutionalized older adults [14].
With regard to higher doses of vitamin D, > 1000 IU/d of vitamin D supplementation resulted in an increased risk of first-time falls with fractures among community-dwelling older adults [15]. A daily dose of 2000 IU vitamin D in the VITAL trial failed to decrease the risk of falls in generally healthy adults [16].
Differences in vitamin D dosage, frequency of administration, and patient populations in the literature made it challenging to identify the best dose of vitamin D supplementation. A network meta-analysis (NMA) can pool the evidence from multiple RCTs through direct and indirect comparisons and thus provide a more comprehensive insight [17]. In the present study, we stratified subjects into various vitamin D dose groups and compared the risk of falls across different doses of vitamin D, calcium, and combined supplementation using NMA. We assigned probability ranking to each dosing regimen in order to identify the best concentration of vitamin D intake for older individuals aged 50 years and older.
Methods
This study was performed in accordance with the Preferred Reporting Items for Systemic Reviews and Meta-Analyses (PRISMA) guidelines [18] (Table S1) and was registered on the international prospective system evaluation registration platform PROSPERO (CRD42023435299).
Search strategy
Relevant studies published in English were systematically searched in PubMed, Embase, Cochrane Library, and Web of Science from inception to May 9, 2023 using the MeSH and free terms “vitamin D”, “ergocalciferol”, “accidental fall”, “fall” and “randomized controlled trial”. The literature search strategy is summarized in Table S2. The references of published systematic reviews were also manually searched to identify potential eligible studies.
Eligibility criteria
Inclusion criteria: (1) RCTs published in English; (2) Vitamin D2 or D3 with or without calcium in the intervention groups (including daily, weekly, monthly or yearly intake); (3) Reported outcome data of falls; (4) Follow-up durations of at least three months. Exclusion criteria: (1) Animal or cell experiments, case reports, scientific experiment plans, reviews, letters, editorials, and conference abstracts; (2) Inaccessible full text; (3) Unextractable outcome data; (4) Combined with other therapies such as nutritional support, hormones, other medications, exercise training, or use of vitamin D analogues (e.g., calcitriol) or hydroxylated vitamin D; (5) If the same population was used in multiple studies, the studies with smaller dataset were excluded.
The abstract and full text of each study were independently screened by two reviewers (XXZ, LT) to determine eligibility, and any disagreements were resolved through discussion or by a third author (RQH).
Data extraction
Data were extracted independently by two reviewers (XXZ and LT), including first author, year of publication, country, intervention and control measures, follow-up period, baseline serum 25-hydroxyvitamin D [25(OH)D] concentration, dwelling and study outcomes.
Quality assessment
The quality of the included studies was independently evaluated by two researchers using the Cochrane risk of bias tool for randomized trials (RoB2) [19], and any disagreement was resolved by discussion with a third researcher. The RoB2 assessment has five domains (Table S3), namely bias arising from the randomization process, bias due to deviation from intended intervention, bias due to missing outcome data, bias in outcome measurement, and bias in selection of the reported result. Each domain is judged as “low risk of bias”, “high risk of bias”, and “some concerns”.
Statistical analysis
The included studies varied in vitamin D dosage, frequency of administration and administration of calcium. To improve the mergeability of results, intermittent vitamin D intake was converted into daily intake by calculating the average dose per day. Based on the converted dose, subjects were divided into the ≤ 500 IU/d, 600–700 IU/d, 800-1000IU/d, 1100-1900IU/day, and ≥ 2000 IU/d groups. In addition, for vitamin D with calcium supplementation, subjects were classified based on whether or not calcium was also administered.
Data were analyzed by GeMTC and JAGS in R4.1.3. A Bayesian NMA was performed using the Markov Chain Monte Carlo (MCMC) methods [20, 21]. NMA is an extension of the standard meta-analysis that compares multiple treatments. Treatment effect can be evaluated by NMA using both direct and indirect comparisons. Due to variations among regimens, such as different dosages and various frequencies of administration, a standard random effects model was applied to provide more conservative estimations of effect size. Model convergence was performed using four Markov chains for simulation analysis with an initial value of 2.5 and 15,000 pre-simulated iterations for annealing, followed by 20,000 iterations. Model fit and global consistency were evaluated by the Deviation Information Criterion (DIC). The overall consistency between direct evidence and indirect evidence was analyzed using the consistent and inconsistent DIC values, respectively [22]. A difference in DIC of < 5 indicates no inconsistency, and the consistency model is fitted; otherwise, the inconsistency model is fitted. If there is a closed-loop network, local consistency was analyzed using a node splitting method [23]. A P < 0.05 indicates local inconsistency. Heterogeneity among studies was evaluated by the I2 statistic, and a value of > 50% indicates significant heterogeneity. Publication bias was assessed by comparison-adjusted funnel plots, Begg’s rank correlation test, and Egger’s test. Sensitivity analyses were conducted on studies without high risk of bias. Post-hoc subgroup analyses were also performed by various factors including gender, dwelling, dosing frequency of vitamin D (daily and intermittent), and baseline 25(OH)D concentrations. Categorical variables are expressed as risk ratios (RR) and 95% confidence interval (CI). If the value of “1” is not included in the 95% CI, the difference is considered statistically significant.
The efficacy of all treatment regimens was simultaneously assessed using a Bayesian framework-based random effects model. Network relationship graphs for outcome indicators, cumulative probability ranking graphs, league tables, and “comparison-corrected” funnel plots were generated. The effects of each intervention were estimated, ranked, and clustered based on the surface under the cumulative ranking curve (SUCRA), and the quality of intervention measures was ranked according to the SUCRA value. The SUCRA represents the percent of efficacy or safety achieved by an agent compared to an imaginary agent that is always the best without uncertainty (e.g., SUCRA = 100%). The SUCRA score is a percentage that ranges from 0 to 100%, and a score closer to 100% indicates a more effective intervention [24]. The NMA was completed using R4.1.3 and Stata 15.0.
Results
Study search and characteristics
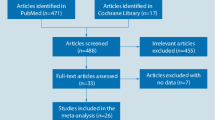
We initially identified 2790 studies, of which 1496 were removed due to duplication, 1424 were excluded after initial review of the title and abstract, and 72 studies were retrieved for full-text review. A final total of 35 eligible studies were included in this meta-analysis. The specific screening process is shown in Fig. 1.
The 35 studies [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59] involving 58,937 patients were conducted in Europe (n = 19), Australia (n = 7), North America (n = 6), Asia (n = 2) and South America (n = 1). The mean age of the patients varied from 59 to 89 years of age. Calcium and vitamin D combined supplementation was used in 11 studies(31.4%), 800–1000 IU/d of vitamin D in 19 studies, < 800 IU/d of vitamin D in 6 studies, and > 1000 IU of vitamin D in 18 studies. The characteristics of the included studies are summarized in Table 1.
Quality and risk of bias assessment
As shown in Fig. 2, the risk of bias arising from the randomization process was high in one studies, of some concerns in 11 studies due to the lack of random allocation sequence concealment, and low in the remaining studies. For biases due to deviations from intended interventions, 4 studies had high risk, 6 studies had some concerns, and the remaining studies had low risk. For biases due to missing outcome data, 2 studies had high risk and 10 studies had some concerns. For biases in measurement of the outcome, 14 studies had high risk and 3 studies had some concerns and the remaining had low risk. Lastly, for biases in selection of the reported results, 13 studies had some concerns and the remaining had low risk. Overall, twenty studies(57.1%) were rated as having low-to-moderate risk of bias.
Bayesian NMA
Network plot
The network plot for the effectiveness of vitamin D supplementation in fall prevention is shown in Fig. 3. Directly comparable treatments are connected by a line, and the thickness of the line is proportional to the number of studies compared in pairs. The diameter of the circle is proportional to the number of participants who received the intervention measures.
Outcomes
There was no significant heterogeneity (I2 = 11%) among the included studies. The pooled results of 35 RCTs showed that 800–1000 IU/d of vitamin D significantly lowered the risk of falls compared to the placebo or no treatment (RR = 0.85, 95%CI: 0.74–0.95) (Table 2; Fig. 4). In addition, 800–1000 IU/d of vitamin D with or without calcium also decreased the frequency of falls compared with calcium alone (RR = 0.74, 95%CI: 0.60–0.90; RR = 0.67, 95%CI: 0.50–0.86; respectively). However, vitamin D supplementation at doses of ≤ 500 IU/d (RR = 1.2, 95%CI: 1.02–1.45), 1100–1900 IU/d (RR = 1.22, 95%CI: 1.04–1.47), 1100–1900 IU/d + Ca (RR = 1.44, 95%CI: 1.06–2.1), and ≥ 2000 IU/d (RR = 1.23, 95%CI: 1.06–1.45) resulted in significantly increased frequency of falls compared with 800–1000 IU/d of vitamin D. Other vitamin D doses showed no significant impact on the risk of falls.
SUCRA ranking
Cumulative probability ranking revealed that 800–1000 IU/d of vitamin D (SUCRA: 91.1%), 600–700 IU/d vitamin D with calcium (SUCRA: 80.8%), and 800–1000 IU/d of vitamin D with calcium (SUCRA: 77.3%) may be the best three regimens for lowering the risk of falls (Fig. 5).
Comparison of the effectiveness of different interventions based on the surface under the cumulative ranking curves (SUCRA). Note In this graphical approach, rankings are made based on the area under the curve (AUC). The greater the AUC, the higher the likelihood that an intervention is in the top rank or one of the top ranks
Publication bias and local inconsistency
The comparison-corrected funnel plot was roughly symmetrical (Fig. 6). However, the Begg’s and Egger’s tests indicated some publication bias in the studies (P = 0.7 Begg’s test, P = 0.033 Egger’s test).
Comparison-corrected funnel plot. A, ≤ 500 IU/d vitamin D; B, 600–700 IU/d vitamin D; C, 600-700IU/d vitamin D + Ca; D, 800–1000 IU/d vitamin D; E, 800–1000 IU/d vitamin D + Ca; F, 1100–1900 IU/d vitamin D; G, 1100–1900 IU/d vitamin D + Ca; H, ≥ 2000 IU/d vitamin D; I, Calcium; J, Placebo or no treatment
We performed a node-splitting analysis to determine the consistency in any closed loops of two interventions. Inconsistency was present in comparisons of ≥ 2000 IU/d vitamin D with placebo or no treatment (P = 0.01). Compared with ≥ 2000 IU/d of vitamin D, the RR (95%CI) of the placebo or no treatment group was 1.02 (95%CI: 0.92–1.14) according to direct comparison, 0.73 (95%CI:0.59–0.91) according to indirect comparison, and 0.96 (95%CI:0.85–1.09) according to the overall result. Consistency in direct and indirect estimates was detected (P > 0.05) in all other closed loops.
Subgroup analysis
As shown in Fig. 7, we performed subgroup NMA by various factors including gender, dwelling, dosing frequency of vitamin D (daily and intermittent), and baseline 25(OH)D concentrations.
Network meta-analysis maps of subgroup analyses. (a) Daily dosing regimens; (b) Intermittent dosing regimens; (c) Ambulatory and community-dwelling elderly; (d) Institution-dwelling elderly; (e) Mean baseline 25(OH)D concentration ≤ 50 nmol/L; (f) Mean baseline 25(OH)D concentration > 50 nmol/L; (g) Female subjects only; (h) Both male and female subjects
Subgroup analysis of vitamin D dosing frequency
In 19 studies that applied daily dosing (Fig. 7a), 800–1000 IU/d of vitamin D significantly lowered the risk of falls (by 22%) compared with placebo or no treatment (RR = 0.78, 95%CI:0.64–0.92), calcium alone (RR = 0.63, 95%CI:0.45–0.83), ≤ 500 IU/d vitamin D (RR = 0.74, 95%CI:0.58–0.91), and ≥ 2000 IU/d vitamin D (RR = 0.63, 95%CI:0.48–0.83). In addition, 800–1000 IU/d vitamin D combined with calcium resulted in lower risk of falls compared with calcium alone (RR = 0.74, 95%CI:0.6–0.9)(Table S4, Fig. S1). Of the 18 studies that applied intermittent dosing (Fig. 7b), NMA was performed on 16 studies since the other two studies were unable to form a network structure with other studies. No significant differences in the risk of falls were detected among different supplementation regimens (Fig. S2).
Subgroup analysis of dwelling
In 24 studies involving ambulatory and community-dwelling elderly individuals (Fig. 7c), 800–1000 IU/d of vitamin D significantly lowered the risk of falls compared with placebo or no treatment (RR = 0.88, 95%CI:0.76–0.98), calcium alone (RR = 0.71, 95%CI:0.5–0.96), and ≥ 2000 IU/d of vitamin D (RR = 0.83, 95%CI:0.69–0.98). Furthermore, 800–1000 IU/d of vitamin D combined with calcium led to reduced risk of falls compared with calcium alone (RR = 0.74, 95%CI:0.58–0.91)(Table S5, Fig. S3). In studies with institution-dwelling elderly (Fig. 7d), the width of the CI was wide due to limited number of studies (Table S6, Fig. S4). Nonetheless, the risk of falls was significantly lower in the 800–1000 IU/d vitamin D group than in the placebo or no treatment (RR = 0.40, 95%CI:0.16–0.88) and ≤ 500 IU/d of vitamin D (RR = 0.37, 95%CI:0.12–0.99) groups. No significant differences in the risk of falls were detected among other regimens.
Subgroup analysis of baseline 25(OH)D concentration
In the 18 studies with a mean baseline 25(OH)D concentration of ≤ 50 nmol/L(Fig. 7e), 800–1000 IU/d of vitamin D significantly lowered the risk of falls compared with placebo or no treatment (RR = 0.69, 95%CI:0.52–0.86), calcium alone (RR = 0.57, 95%CI:0.34–0.85), ≤ 500 IU/d of vitamin D (RR = 0.67, 95%CI:0.49–0.88), 600–700 IU/d of vitamin D (RR = 0.57, 95%CI:0.34–0.98), 800–1000 IU/d of vitamin D plus calcium (RR = 0.72, 95%CI:0.5–0.98), 1100–1900 IU/d of vitamin D ( RR = 0.67, 95%CI:0.5–0.91), and ≥ 2000 IU/d of vitamin D (RR = 0.7, 95%CI:0.48–0.97)(Table S7, Fig. S5). Of the 11 studies with a mean baseline 25(OH)D concentration > 50 nmol/L(Fig. 7f), NMA was only performed on 9 studies since two studies were unable to form a network structure with other studies. The width of CIs was wide and no significant differences were detected among the different supplementation regimens (Fig. S6).
Subgroup analysis of gender
Among the 13 studies that only included females (Fig. 7g), 800–1000 IU/d of vitamin D decreased the risk of falls by 22% compared with placebo or no treatment (RR = 0.78, 95%CI:0.55–0.97). There were no significant differences in risk of falls between higher doses of vitamin D and 800–1000 IU/d of vitamin D (Table S8 and Fig. S7). Of the 21 studies that enrolled both male and female subjects (Fig. 7h), NMA was performed on 19 studies since two studies were unable to form a network structure with other studies. Our results showed that 800–1000 IU/d of vitamin D significantly lowered the risk of falls compared with placebo or no treatment (RR = 0.86, 95%CI:0.7–0.99) and ≥ 2000 IU/d of vitamin D ( RR = 0.8, 95%CI:0.64–0.95) (Table S9 and Fig. S8).
Collectively, our data demonstrated that 800–1000 IU/d of vitamin D was associated with a significantly lower risk of falls in all subgroups except in populations with serum 25(OH)D levels > 50 nmol/L and receiving intermittent doses of vitamin D (Fig. 8).
Sensitivity analysis
Fifteen studies with high risk of bias were removed from the sensitivity analysis. NMA was performed on 15 studies since five studies were unable to form a network structure with other studies. The results remained robust in the sensitivity analysis (Table S10 and Fig. S9).
Discussion
Our NMA of 35 RCTs involving 58,937 elderly individuals demonstrated that vitamin D supplementation at 800–1000 IU/d significantly lowered the incidence of falls by 15%, and the results were robust in the sensitivity analysis. In addition, 800-1000IU/d of vitamin D was associated with a significantly lower risk of falls regardless of gender composition and dwelling. This reduction remained significant in population with vitamin deficiency, while any dose of vitamin D had no effect in older adults with baseline 25(OH)D levels > 50 nmol/L. In terms of dosing frequency, daily administration of 800–1000 IU/d vitamin D reduced the risk of falls by 22%, whereas intermittent administration of vitamin D had no preventive effect on falls (Fig. 8).
Our results are consistent with a previous meta-analysis by Kong et al. [12], in which 800–1000 IU/d of vitamin D was found to be associated with lower risks of falls. Our results are also in line with other meta-analyses indicating that vitamin D can lower the risk of falls despite differences in the recommended doses. The doses that were proposed for fall prevention in these meta-analyses were 700–1000 IU/d of vitamin D by Bischoff-Ferrari et al. [2], 700–2000 IU/d of vitamin D by Wei et al. [14], and 700-1000IU/d vitamin D by Ling et al. [13] According to Thanapluetiwong et al. [11], vitamin D3 decreased the incidence of falls only when supplemented with calcium (RR = 0.881, 95% CI 0.821–0.945), but subgroup analyses were not performed on the different vitamin D doses. Due to differences in the preferred doses of vitamin D in the included studies, we divided vitamin D use into different dose groups and conducted a NMA to test the effectiveness of different dose ranges. We found that only 800–1000 IU/d of vitamin D reduced the risk of falls. Our cumulative probability results based on SUCRA showed that the top three regimens with decreasing effectiveness were 800–1000 IU/d vitamin D alone, 600–700 IU/d vitamin D combined with calcium, and 800–1000 IU/d vitamin D combined with calcium. Our data indicated that 800-1000IU/d of vitamin D was the best dosage for reducing falls. Of note, several meta-analyses indicated that vitamin D decreased the incidence of falls only when supplemented with calcium [10, 11, 13, 14]. In contrast, we found that 800–1000 IU/d vitamin D combined with calcium was only beneficial when compared with calcium alone but not with placebo or no treatment. This discrepancy may be attributed to different control groups. Most of previous meta-analyses used both placebo and calcium alone as the control group, while we assigned placebo and calcium as separate groups. Nevertheless, our results were in agreement with some published recommendations. The BHOF and International Osteoporosis Foundation (IOF) both recommend a daily intake of 800–1000 IU vitamin D for seniors to improve bone health and reduce the risk of falls [6, 60, 61] However, the meta-analysis by Bolland et al. revealed no effect of vitamin D on falls [9], which could be related to the exclusion of studies that compared vitamin D and calcium combined supplementation with placebo. Additionally, the authors did not compare specific dose subgroups with the controls.
High-dose vitamin D application has been shown to be non-beneficial or even harmful. Higher monthly doses of vitamin D (60,000 IU/m) were found to be effective for achieving a serum level of at least 30 ng/mL of 25-hydroxyvitamin D and were associated with an increased risk of falls [52]. Wanigatunga et al. [15] reported that > 1000 IU/d of vitamin D increased the risk of first-time falls with fractures but lowered the risk of outdoor falls in community-dwelling older adults with 25-72.5 nmol/L baseline 25(OH)D level. In our NMA, the incidence of falls did not differ significantly between > 1000 IU/d vitamin D and placebo or no treatment. However, the frequency of falls was significantly higher in the > 1000 IU/d vitamin D groups than in the 800–1000 IU/d group.
Another important finding is that the efficacy of vitamin D in fall prevention depends on the baseline serum level of 25(OH)D in the elderly population and the dosing frequency of vitamin D (daily or intermittent). We found that vitamin D was only beneficial for fall prevention in population with vitamin D deficiency. The US Preventive Services Task Force reported a lack of association between vitamin D supplementation and falls [62] based on only 7 trials, wherein the mean baseline serum 25(OH)D levels ranged from 65.9 to 79.4 nmol/L. Vitamin D supplementation in population without vitamin D deficiency did not have meaningful effects on falls. Moreover, intermittent vitamin D supplementation also showed no protective effect on falls, which was consistent with some previous studies [14, 63]. A meta-analysis published in 2023 showed that intermittent or single high-dose vitamin D3 supplementation increased the risk of falls, and the association was close to statistically significant [63]. Therefore, vitamin D supplementation may be helpful for fall prevention in population with vitamin D deficiency, and is more effective when administered daily rather than intermittently.
Previous studies have suggested that low baseline 25(OH)D may contribute to muscle strength decline in the elderly [64] and is associated with lower 6-minute walking test score and weaker strength [65]. The mechanisms by which vitamin D decreases the occurrence of falls can be partially explained by the findings that vitamin D can regulate calcium homeostasis and improve muscle strength and balance, ultimately leading to a reduced risk of falling [26, 66]. Daily vitamin D supplementation at 800 to 1,000 IU consistently demonstrated beneficial effects on strength and balance [67]. Though, a negative effect of 70 µg (2800 IU)/d of vitamin D on muscle strength and physical performance was reported by Bislev et al. [68]. However, the effect of vitamin D remains controversial. Aschauer et al. [69] revealed that neither muscle strength endurance, nor functional mobility were modulated by vitamin D supplementation (800 IU/d vitamin D3, 50,000 IU/month vitamin D3 or nothing). Therefore, even though our data are consistent with some prior studies, the physiology of vitamin D in falls remains unclear and needs further investigation.
Surprisingly, calcium alone without vitamin D resulted in increased frequency of falls compared with placebo or no treatment, and the association was close to statistically significant (RR = 1.26, 95%CI: 0.997–1.62). Calcium supplementation has been considered to be beneficial for the prevention of osteoporosis and fractures [70, 71]. Though, the usefulness of calcium supplementation in prevention of fractures has been questioned [72]. Warensjö et al. [73] found that dietary calcium intake of > 1,137 mg/d could increase the risk of hip fractures in women. Likewise, a meta-analysis reported that calcium supplementation (480–1000 mg/d elemental calcium) may increase the risk of hip fractures [74]. Reid et al. [75] also found that 5,500 women involved in three trials of calcium monotherapy (480–1000 mg/d elemental calcium) exhibited consistent adverse trends in the number of hip fractures (RR = 1.50, 95%CI: 1.06–2.12). However, there was no direct comparison between calcium alone (without vitamin D) and placebo in our meta-analysis, and indirect comparison was performed through the intermediate node of vitamin D plus calcium. Therefore, further RCTs are warranted to elucidate the impact of calcium supplementation without vitamin D on falls.
There are several limitations in our study. First, the small sample size and use of primary outcomes other than fall in some studies may confound the results. Second, the dosage and frequency of vitamin D administration varied greatly among studies. Although we pooled intermittent doses by calculating the average dose per day, this may lead to bias in the findings considering that various dosing regimens may result in different vitamin D status in the body. Also, we divided vitamin D usage into different dose groups based on previous studies and meta-analyses, which might introduce some bias as a result of the method of grouping. Third, studies performed in different dwellings were included in the NMA and hence our results should be interpreted with caution. Fourth, we excluded non-English articles from our literature search, which may cause selection bias. Indeed, our Egger’s test result indicated the presence of publication bias in our study. Last, there are other confounding factors present in this study, such as potential missing data, meta-biases, and heterogeneity of NMA.
Conclusion
This is the first systematic review and NMA comparing the efficacy of different concentrations of vitamin D, calcium, and combined supplementation in fall prevention. Based on our NMA, 800–1000 IU/d of vitamin D supplement is associated with a lower risk of falling among older adults. Vitamin D is effective for preventing falls in populations on a daily dosing schedule and deficient in vitamin D, but not in populations receiving intermittent dosing schedule or without vitamin D deficiency. Nevertheless, further well-designed RCTs are warranted to confirm these findings.
Data availability
All data generated or analyzed during this study are included in this published article and supplementary materials.
Abbreviations
- BHOF:
-
Bone Health and Osteoporosis Foundation
- CI:
-
Confidence interval
- DIC:
-
Deviation Information Criterion
- ESCEO:
-
European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases
- IOM:
-
Institute of Medicine
- IOF:
-
International Osteoporosis Foundation
- IU:
-
International Unit
- MCMC:
-
Markov Chain Monte Carlo
- NMA:
-
Network meta-analysis
- RCT:
-
Randomized controlled trial
- RR:
-
Relative risk
- PRISMA:
-
Preferred Reporting Items for Systemic Reviews and Meta-Analyses
- SUCRA:
-
Surface under the cumulative ranking curve
References
Tinetti ME. Prevention of falls and fall injuries in elderly persons: a research agenda. Prev Med. 1994;23(5):756–62.
Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, Orav JE, Stuck AE, Theiler R, Wong JB, Egli A, Kiel DP, Henschkowski J. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339:b3692.
Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–7.
Chevalley T, Brandi ML, Cashman KD, Cavalier E, Harvey NC, Maggi S, Cooper C, Al-Daghri N, Bock O, Bruyere O, et al. Role of vitamin D supplementation in the management of musculoskeletal diseases: update from an European society of clinical and economical aspects of osteoporosis, Osteoarthritis and Musculoskeletal diseases (ESCEO) working group. Aging Clin Exp Res. 2022;34(11):2603–23.
WHO. Step safely: strategies for preventing and managing falls across the life-course. Licence: CC BY-NC-SA 30 IGO. 2021.
Bone Health & Osteoporosis Foundation. Calcium and Vitamin D. https://www.bonehealthandosteoporosis.org/patients/treatment/calciumvitamin-d/.
Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and calcium. In: Ross AC, Taylor CL, Yaktine AL, and Del Valle HB, editors. Dietary reference intakes for calcium and Vitamin D, 2011.
Tang O, Juraschek SP, Appel LJ. Design features of Randomized clinical trials of vitamin D and falls: a systematic review. Nutrients. 2018;10(8):964.
Bolland MJ, Grey A, Avenell A. Effects of vitamin D supplementation on musculoskeletal health: a systematic review, meta-analysis, and trial sequential analysis. Lancet Diabetes Endocrinol. 2018;6(11):847–58.
Wu H, Pang Q. The effect of vitamin D and calcium supplementation on falls in older adults: a systematic review and meta-analysis. Orthopade. 2017;46(9):729–36.
Thanapluetiwong S, Chewcharat A, Takkavatakarn K, Praditpornsilpa K, Eiam-Ong S, Susantitaphong P. Vitamin D supplement on prevention of fall and fracture: a Meta-analysis of Randomized controlled trials. Med (Baltim). 2020;99(34):e21506.
Kong SH, Jang HN, Kim JH, Kim SW, Shin CS. Effect of vitamin D supplementation on risk of fractures and falls according to dosage and interval: a Meta-analysis. Endocrinol Metab (Seoul). 2022;37(2):344–58.
Ling Y, Xu F, Xia X, Dai D, Xiong A, Sun R, Qiu L, Xie Z. Vitamin D supplementation reduces the risk of fall in the vitamin D deficient elderly: an updated meta-analysis. Clin Nutr. 2021;40(11):5531–7.
Wei FL, Li T, Gao QY, Huang Y, Zhou CP, Wang W, Qian JX. Association between Vitamin D Supplementation and fall Prevention. Front Endocrinol (Lausanne). 2022;13:919839.
Wanigatunga AA, Sternberg AL, Blackford AL, Cai Y, Mitchell CM, Roth DL, Miller ER 3rd, Szanton SL, Juraschek SP, Michos ED, et al. The effects of vitamin D supplementation on types of falls. J Am Geriatr Soc. 2021;69(10):2851–64.
LeBoff MS, Murata EM, Cook NR, Cawthon P, Chou SH, Kotler G, Bubes V, Buring JE, Manson JE. VITamin D and OmegA-3 TriaL (VITAL): effects of vitamin D supplements on risk of Falls in the US Population. J Clin Endocrinol Metab. 2020;105(9):2929–38.
Catala-Lopez F, Tobias A, Roque M. Basic concepts for network meta-analysis. Aten Primaria. 2014;46(10):573–81.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Neupane B, Richer D, Bonner AJ, Kibret T, Beyene J. Network meta-analysis using R: a review of currently available automated packages. PLoS ONE. 2014;9(12):e115065.
Gelman A, Rubin DB. Markov chain Monte Carlo methods in biostatistics. Stat Methods Med Res. 1996;5(4):339–55.
Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29(7–8):932–44.
Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades AE. Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Med Decis Mak. 2013;33(5):641–56.
Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–71.
Graafmans WC, Ooms ME, Hofstee HM, Bezemer PD, Bouter LM, Lips P. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol. 1996;143(11):1129–36.
Pfeifer M, Begerow B, Minne HW, Abrams C, Nachtigall D, Hansen C. Effects of a short-term vitamin D and calcium supplementation on body sway and secondary hyperparathyroidism in elderly women. J Bone Min Res. 2000;15(6):1113–8.
Chapuy MC, Pamphile R, Paris E, Kempf C, Schlichting M, Arnaud S, Garnero P, Meunier PJ. Combined calcium and vitamin D3 supplementation in elderly women: confirmation of reversal of secondary hyperparathyroidism and hip fracture risk: the Decalyos II study. Osteoporos Int. 2002;13(3):257–64.
Bischoff HA, Stahelin HB, Dick W, Akos R, Knecht M, Salis C, Nebiker M, Theiler R, Pfeifer M, Begerow B, et al. Effects of vitamin D and calcium supplementation on falls: a randomized controlled trial. J Bone Min Res. 2003;18(2):343–51.
Trivedi DP, Doll R, Khaw KT. Effect of four monthly oral vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community: randomised double blind controlled trial. BMJ. 2003;326(7387):469.
Dhesi JK, Jackson SH, Bearne LM, Moniz C, Hurley MV, Swift CG, Allain TJ. Vitamin D supplementation improves neuromuscular function in older people who fall. Age Ageing. 2004;33(6):589–95.
Harwood RH, Sahota O, Gaynor K, Masud T, Hosking DJ. Nottingham Neck of Femur S: a randomised, controlled comparison of different calcium and vitamin D supplementation regimens in elderly women after hip fracture: the Nottingham Neck of Femur (NONOF) Study. Age Ageing. 2004;33(1):45–51.
Flicker L, MacInnis RJ, Stein MS, Scherer SC, Mead KE, Nowson CA, Thomas J, Lowndes C, Hopper JL, Wark JD. Should older people in residential care receive vitamin D to prevent falls? Results of a randomized trial. J Am Geriatr Soc. 2005;53(11):1881–8.
Porthouse J, Cockayne S, King C, Saxon L, Steele E, Aspray T, Baverstock M, Birks Y, Dumville J, Francis R, et al. Randomised controlled trial of calcium and supplementation with cholecalciferol (vitamin D3) for prevention of fractures in primary care. BMJ. 2005;330(7498):1003.
Bischoff-Ferrari HA, Orav EJ, Dawson-Hughes B. Effect of cholecalciferol plus calcium on falling in ambulatory older men and women: a 3-year randomized controlled trial. Arch Intern Med. 2006;166(4):424–30.
Law M, Withers H, Morris J, Anderson F. Vitamin D supplementation and the prevention of fractures and falls: results of a randomised trial in elderly people in residential accommodation. Age Ageing. 2006;35(5):482–6.
Smith H, Anderson F, Raphael H, Maslin P, Crozier S, Cooper C. Effect of annual intramuscular vitamin D on fracture risk in elderly men and women–a population-based, randomized, double-blind, placebo-controlled trial. Rheumatology (Oxford). 2007;46(12):1852–7.
Broe KE, Chen TC, Weinberg J, Bischoff-Ferrari HA, Holick MF, Kiel DP. A higher dose of vitamin d reduces the risk of falls in nursing home residents: a randomized, multiple-dose study. J Am Geriatr Soc. 2007;55(2):234–9.
Prince RL, Austin N, Devine A, Dick IM, Bruce D, Zhu K. Effects of Ergocalciferol added to calcium on the risk of falls in elderly high-risk women. Arch Intern Med. 2008;168(1):103–8.
Pfeifer M, Begerow B, Minne HW, Suppan K, Fahrleitner-Pammer A, Dobnig H. Effects of a long-term vitamin D and calcium supplementation on falls and parameters of muscle function in community-dwelling older individuals. Osteoporos Int. 2009;20(2):315–22.
Karkkainen MK, Tuppurainen M, Salovaara K, Sandini L, Rikkonen T, Sirola J, Honkanen R, Arokoski J, Alhava E, Kroger H. Does daily vitamin D 800 IU and calcium 1000 mg supplementation decrease the risk of falling in ambulatory women aged 65–71 years? A 3-year randomized population-based trial (OSTPRE-FPS). Maturitas. 2010;65(4):359–65.
Sanders KM, Stuart AL, Williamson EJ, Simpson JA, Kotowicz MA, Young D, Nicholson GC. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA. 2010;303(18):1815–22.
Witham MD, Crighton LJ, Gillespie ND, Struthers AD, McMurdo ME. The effects of vitamin D supplementation on physical function and quality of life in older patients with heart failure: a randomized controlled trial. Circ Heart Fail. 2010;3(2):195–201.
Glendenning P, Zhu K, Inderjeeth C, Howat P, Lewis JR, Prince RL. Effects of three-monthly oral 150,000 IU cholecalciferol supplementation on falls, mobility, and muscle strength in older postmenopausal women: a randomized controlled trial. J Bone Min Res. 2012;27(1):170–6.
Witham MD, Price RJ, Struthers AD, Donnan PT, Messow CM, Ford I, McMurdo ME. Cholecalciferol treatment to reduce blood pressure in older patients with isolated systolic hypertension: the VitDISH randomized controlled trial. JAMA Intern Med. 2013;173(18):1672–9.
Wood AD, Secombes KR, Thies F, Aucott LS, Black AJ, Reid DM, Mavroeidi A, Simpson WG, Fraser WD, Macdonald HM. A parallel group double-blind RCT of vitamin D3 assessing physical function: is the biochemical response to treatment affected by overweight and obesity? Osteoporos Int. 2014;25(1):305–15.
Houston DK, Tooze JA, Demons JL, Davis BL, Shertzer-Skinner R, Kearsley LB, Kritchevsky SB, Williamson JD. Delivery of a Vitamin D Intervention in homebound older adults using a meals-on-Wheels Program: a pilot study. J Am Geriatr Soc. 2015;63(9):1861–7.
Hansen KE, Johnson RE, Chambers KR, Johnson MG, Lemon CC, Vo TN, Marvdashti S. Treatment of Vitamin D Insufficiency in Postmenopausal women: a Randomized Clinical Trial. JAMA Intern Med. 2015;175(10):1612–21.
Uusi-Rasi K, Patil R, Karinkanta S, Kannus P, Tokola K, Lamberg-Allardt C, Sievanen H. Exercise and vitamin D in fall prevention among older women: a randomized clinical trial. JAMA Intern Med. 2015;175(5):703–11.
Cangussu LM, Nahas-Neto J, Orsatti CL, Poloni PF, Schmitt EB, Almeida-Filho B, Nahas EA. Effect of isolated vitamin D supplementation on the rate of falls and postural balance in postmenopausal women fallers: a randomized, double-blind, placebo-controlled trial. Menopause. 2016;23(3):267–74.
Imaoka M, Higuchi Y, Todo E, Kitagwa T, Ueda T. Low-frequency Exercise and vitamin D supplementation reduce Falls among Institutionalized Frail Elderly. Int J Gerontol. 2016;10(4):202–6.
Jin X, Jones G, Cicuttini F, Wluka A, Zhu Z, Han W, Antony B, Wang X, Winzenberg T, Blizzard L, et al. Effect of vitamin D supplementation on tibial cartilage volume and knee Pain among patients with symptomatic knee osteoarthritis: a Randomized Clinical Trial. JAMA. 2016;315(10):1005–13.
Bischoff-Ferrari HA, Dawson-Hughes B, Orav EJ, Staehelin HB, Meyer OW, Theiler R, Dick W, Willett WC, Egli A. Monthly high-dose vitamin D treatment for the Prevention of Functional decline: a Randomized Clinical Trial. JAMA Intern Med. 2016;176(2):175–83.
Levis S, Gomez-Marin O. Vitamin D and physical function in sedentary older men. J Am Geriatr Soc. 2017;65(2):323–31.
Hin H, Tomson J, Newman C, Kurien R, Lay M, Cox J, Sayer J, Hill M, Emberson J, Armitage J, et al. Optimum dose of vitamin D for disease prevention in older people: BEST-D trial of vitamin D in primary care. Osteoporos Int. 2017;28(3):841–51.
Khaw KT, Stewart AW, Waayer D, Lawes CMM, Toop L, Camargo CA Jr., Scragg R. Effect of monthly high-dose vitamin D supplementation on falls and non-vertebral fractures: secondary and post-hoc outcomes from the randomised, double-blind, placebo-controlled ViDA trial. Lancet Diabetes Endocrinol. 2017;5(6):438–47.
Aspray TJ, Chadwick T, Francis RM, McColl E, Stamp E, Prentice A, von Wilamowitz-Moellendorff A, Schoenmakers I. Randomized controlled trial of vitamin D supplementation in older people to optimize bone health. Am J Clin Nutr. 2019;109(1):207–17.
Prithiani SL, Kumar R, Mirani SH, Ibrahim S, Ansari TA, Kumar B, Arshad T, Hassan SM. Effect of monthly 100,000 IU vitamin D supplementation on falls and non-vertebral fractures. Cureus. 2021;13(1):e12445.
Waterhouse M, Sanguineti E, Baxter C, Duarte Romero B, McLeod DSA, English DR, Armstrong BK, Ebeling PR, Hartel G, Kimlin MG, et al. Vitamin D supplementation and risk of falling: outcomes from the randomized, placebo-controlled D-Health trial. J Cachexia Sarcopenia Muscle. 2021;12(6):1428–39.
Appel LJ, Michos ED, Mitchell CM, Blackford AL, Sternberg AL, Miller ER 3rd, Juraschek SP, Schrack JA, Szanton SL, Charleston J, et al. The effects of four doses of vitamin D supplements on falls in older adults: a Response-Adaptive, randomized clinical trial. Ann Intern Med. 2021;174(2):145–56.
LeBoff MS, Greenspan SL, Insogna KL, Lewiecki EM, Saag KG, Singer AJ, Siris ES. The clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022;33(10):2049–102.
International Osteoporosis Foundation. Vitamin D. https://www.osteoporosis.foundation/patients/prevention/vitamin-d.
Force USPST, Grossman DC, Curry SJ, Owens DK, Barry MJ, Caughey AB, Davidson KW, Doubeni CA, Epling JW Jr., Kemper AR, et al. Interventions to Prevent Falls in Community-Dwelling older adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319(16):1696–704.
Myung SK, Cho H. Effects of intermittent or single high-dose vitamin D supplementation on risk of falls and fractures: a systematic review and meta-analysis. Osteoporos Int. 2023;34(8):1355–67.
Granic A, Hill TR, Davies K, Jagger C, Adamson A, Siervo M, et al. Vitamin D status, muscle strength and physical performance decline in very old adults: a prospective study. Nutrients. 2017;9(4):379.
Toffanello ED, Perissinotto E, Sergi G, Zambon S, Musacchio E, Maggi S, Coin A, Sartori L, Corti MC, Baggio G, et al. Vitamin D and physical performance in elderly subjects: the Pro.V.A study. PLoS ONE. 2012;7(4):e34950.
Lagari V, Gomez-Marin O, Levis S. The role of vitamin D in improving physical performance in the elderly. J Bone Min Res. 2013;28(10):2194–201.
Muir SW, Montero-Odasso M. Effect of vitamin D supplementation on muscle strength, gait and balance in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2011;59(12):2291–300.
Bislev LS, Langagergaard Rodbro L, Rolighed L, Sikjaer T, Rejnmark L. Effects of vitamin D3 supplementation on muscle strength, Mass, and physical performance in women with vitamin D insufficiency: a randomized placebo-controlled trial. Calcif Tissue Int. 2018;103(5):483–93.
Aschauer R, Unterberger S, Zohrer PA, Draxler A, Franzke B, Strasser EM, et al. Effects of vitamin D3 supplementation and resistance training on 25-Hydroxyvitamin D status and functional performance of older adults: a randomized placebo-controlled trial. Nutrients. 2022;14(1):86.
Dawson-Hughes B, Dallal GE, Krall EA, Sadowski L, Sahyoun N, Tannenbaum S. A controlled trial of the effect of calcium supplementation on bone density in postmenopausal women. N Engl J Med. 1990;323(13):878–83.
Tang BM, Eslick GD, Nowson C, Smith C, Bensoussan A. Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis. Lancet. 2007;370(9588):657–66.
Chiodini I, Bolland MJ. Calcium supplementation in osteoporosis: useful or harmful? Eur J Endocrinol. 2018;178(4):D13–25.
Warensjo E, Byberg L, Melhus H, Gedeborg R, Mallmin H, Wolk A, Michaelsson K. Dietary calcium intake and risk of fracture and osteoporosis: prospective longitudinal cohort study. BMJ. 2011;342:d1473.
Bischoff-Ferrari HA, Dawson-Hughes B, Baron JA, Burckhardt P, Li R, Spiegelman D, Specker B, Orav JE, Wong JB, Staehelin HB, et al. Calcium intake and hip fracture risk in men and women: a meta-analysis of prospective cohort studies and randomized controlled trials. Am J Clin Nutr. 2007;86(6):1780–90.
Reid IR, Bolland MJ, Grey A. Effect of calcium supplementation on hip fractures. Osteoporos Int. 2008;19(8):1119–23.
Acknowledgements
Not applicable.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: Long Tan, Xiaoxue Zheng; Methodology: Long Tan, Ruiqian He, Xiaoxue Zheng; Formal analysis and investigation: Long Tan, Ruiqian He, Xiaoxue Zheng; Manuscript drafting: Long Tan; Manuscript drafting, review and editing: Xiaoxue Zheng; Resources: Long Tan, Ruiqian He, Xiaoxue Zheng; Supervision: Xiaoxue Zheng. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tan, L., He, R. & Zheng, X. Effect of vitamin D, calcium, or combined supplementation on fall prevention: a systematic review and updated network meta-analysis. BMC Geriatr 24, 390 (2024). https://doi.org/10.1186/s12877-024-05009-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05009-x