Abstract
Background
Evidence indicates frailty before intensive care unit (ICU) admission leads to poor outcomes. However, it is unclear whether quality of life (QOL) and activities of daily living (ADL) for survivors of critical illness admitted to the ICU via the emergency department remain consistent or deteriorate in the long-term compared to baseline. This study aimed to evaluate long-term QOL/ADL outcomes in these patients, categorized by the presence or absence of frailty according to Clinical Frailty Scale (CFS) score, as well as explore factors that influence these outcomes.
Methods
This was a post-hoc analysis of a prospective, multicenter, observational study conducted across Japan. It included survivors aged 65 years or older who were admitted to the ICU through the emergency department. Based on CFS scores, participants were categorized into either the not frail group or the frail group, using a threshold CFS score of < 4. Our primary outcome was patient-centered outcomes (QOL/ADL) measured by the five-level EuroQol five-dimensional questionnaire (EQ-5D-5L) and the Barthel Index six months post-ICU admission, comparing results from baseline. Secondary outcomes included exploration of factors associated with QOL/ADL six months post-ICU admission using multiple linear regression analyses.
Results
Of 514 candidates, 390 participants responded to the EQ-5D-5L questionnaire, while 237 responded to the Barthel Index. At six months post-admission, mean EQ-5D-5L values declined in both the not frail and frail groups (0.80 to 0.73, p = 0.003 and 0.58 to 0.50, p = 0.002, respectively); Barthel Index scores also declined in both groups (98 to 83, p < 0.001 and 79 to 61, p < 0.001, respectively). Multiple linear regression analysis revealed that baseline frailty (β coefficient, -0.15; 95% CI, − 0.23 to − 0.07; p < 0.001) and pre-admission EQ-5D-5L scores (β coefficient, 0.14; 95% CI, 0.02 to 0.26; p = 0.016) affected EQ-5D-5L scores at six months. Similarly, baseline frailty (β coefficient, -12.3; 95% CI, − 23.9 to − 0.80; p = 0.036) and Barthel Index scores (β coefficient, 0.54; 95% CI, 0.30 to 0.79; p < 0.001) influenced the Barthel Index score at six months.
Conclusions
Regardless of frailty, older ICU survivors from the emergency department were more likely to experience reduced QOL and ADL six months after ICU admission compared to baseline.
Similar content being viewed by others
Background
The number of older patients visiting the emergency department is rising, with a subset of these individuals requiring critical care in the intensive care unit (ICU). This trend mirrors the dramatic increase in the older population [1,2,3]. Frailty in older individuals is characterized by weakness, reduced muscle mass, decreased mobility, diminished cognitive function, and poor nutritional status. The Clinical Frailty Scale (CFS) offers a flexible approach to evaluating frailty, considering a wide array of health deficits to assess frailty as a spectrum [4]. Elevated CFS scores have been linked with increased mortality and adverse outcomes, suggesting it as a suitable tool for ICU triage [5]. The LIFE Study further highlighted that CFS score is an independent predictor of long-term mortality among critically ill older patients admitted to the ICU through the emergency department in Japan [6]. The implications of this study are beneficial to clinicians, offering patients and their surrogates vital prognostic information about survival. Yet, long-term patient-centered outcomes such as quality of life (QOL), activities of daily living (ADL), return to home, and mental health outcomes are also significant concerns despite limited evidence [7, 8]. Tools such as the five-level EuroQol five-dimensional questionnaire (EQ-5D-5L) [9] and the Barthel Index [10], which measure QOL and ADL, respectively, should be considered in healthcare resource allocation decisions. While clinicians often predict future QOL/ADL based on their clinical experience without objective indicators, a poor CFS score before ICU admission might predict unfavorable outcomes [11, 12]. It remains unclear whether QOL/ADL in critical illness survivors remains unchanged or deteriorates in the long-term compared to baseline, as well as which factors are associated with long-term, patient-centered outcomes.
Therefore, this study aimed to investigate the long-term, patient-centered outcomes of ICU survivors expressed as a composite EQ-5D-5L/Barthel Index score grouped by frailty based on CFS score compared to baseline. Additionally, we evaluated the impact of this composite score on the QOL/ADL of these patients in the long term and explored the factors associated with QOL/ADL.
Methods
Study protocol
We conducted a post hoc analysis of the LIFE Study, which was registered in the University Hospital Medical Information Network Clinical Trials Registry (ID: UMIN000037430, date of registration: July 20, 2019), focusing on the QOL/ADL of LIFE Study survivors at six months post-ICU admission. The detailed study design and methods have been previously reported [6]. In brief, the LIFE Study was a prospective, multicenter, observational study conducted in 17 Japanese ICUs. Its primary objective was to determine whether baseline frailty impacted six-month mortality following ICU admission. All participants aged 65 years or older who were admitted to the ICU through the emergency department, including those requiring emergency surgery, between November 2019 and April 2020 were eligible for the LIFE Study analysis. The exclusion criteria included patients who did not provide consent, those without CFS data before ICU admission, and those lost to follow-up. In this post hoc analysis, we further excluded patients who died within six months and those lacking patient-centered data such as EQ-5D-5L and Barthel Index scores at both ICU admission and at the six-month follow-up.
The original study protocol was approved by the ethics committees of all participating institutions. Additionally, our post hoc analysis received approval from the Okayama University Hospital Ethics Committee (approval number: K-2308-008). Clinical investigations were conducted in accordance with the provisions of the Declaration of Helsinki. Patient consent was waived for all participants enrolled in this study by the Okayama University Hospital Ethics Committee, as the consent had already been obtained, and the data were analyzed anonymously.
Assessment of frailty, QOL and ADL
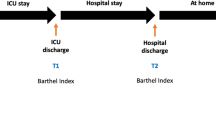
On ICU admission, CFS scores were used to assess the frailty of all participating patients as they presented prior to the onset of the acute illness/injury (approximately two weeks earlier). The CFS is a pictographic scale that ranges from 1 (very fit) to 9 (terminally ill) [4]. Patients with scores of 1 to 3 are considered “not frail,” those with a score of 4 are termed “pre-frail” or “vulnerable,” and those with scores of 5 to 9 are considered “frail” [13]. Additionally, eligible participants completed questionnaires prior to ICU admission to assess baseline QOL and ADL. QOL was measured using the EQ-5D-5L, a general instrument that measures five dimensions: self-care, mobility, activities, anxiety/depression, and pain/discomfort. Each dimension is measured with scores ranging from 1 (no problems) to 5 (extreme problems) [9]. Specific EQ-5D-5L scores calculated using country-specific scores, with 1 indicating the best possible QOL and 0 indicating death [9]. The Barthel Index was utilized to evaluate the level of dependency in ADL. The Barthel Index encompasses ten domains: feeding, movement, adjustment, bathing, toilet use, mobility, dressing, stairs, bladder control, and bowel control, with possible scores of 0, 5, 10, or 15 points for each domain [10]. A higher Barthel Index score, ranging from 0 to 100 points, indicates a lower level of dependency. In a similar manner, a follow-up survey was conducted six months post-ICU admission to evaluate these patient-centered outcomes, again assessed using the EQ-5D-5L and Barthel Index. Upon ICU admission, trained study investigators obtained CFS and Barthel Index scores from either the patient or their surrogate. In addition, a survey to gather EQ-5D-5L score was administered to the patient or surrogate. Six months post-admission, a second questionnaire was mailed to patients and/or their surrogates to collect data on both the EQ-5D-5L and Barthel Index. Of note, Barthel Index data was collected from patients who were included since January 2020.
Data collection
We collected the following data: patient characteristics (gender, age, body mass index, Charlson Comorbidity Index score, and ICU admission category such as cardiology, pulmonary, gastrointestinal, neurology, trauma, endocrine, skin/tissue, urology, or other); ICU admission type (medical or surgical); and illness severity (based on Acute Physiology and Chronic Health Evaluation (APACHE) 2 score on the first day after ICU admission), laboratory findings (specifically, maximum lactate concentrations during ICU admission); procedures during ICU admission (including mechanical ventilation, tracheostomy, renal replacement therapy, vasopressor support, and extracorporeal membrane oxygenation); presence of conditions such as sepsis or acute kidney injury during ICU admission; and outcome measures (such as discharge destination and length of ICU and hospital stay).
Outcomes
Participants were categorized into two groups for analysis. The “not frail” and “frail” groups were defined based on the presence or absence of frailty, determined by a CFS score of 4 or greater before ICU admission [14]. Our primary outcome was patient-centered outcomes (specifically QOL/ADL assessed by EQ-5D-5L and Barthel Index) six months after ICU admission, comparing results from baseline, assigned by the not frail and frail groups.
Secondary outcomes included distinct functional capacities in QOL/ADL for both the not frail group and the frail group. Furthermore, we evaluated the impact of frailty on QOL/ADL six months after ICU admission and identified the factors associated with these changes.
Statistical analyses
Categorical variables are presented as counts and percentages, while continuous variables are summarized using medians and interquartile ranges (IQRs) or means and standard deviations (SD). Changes in QOL/ADL scores from baseline to six months post-ICU admission are presented as mean differences and were analyzed using the paired-sample Student’s t-test. To compare between groups, the Mann-Whitney U test was used for continuous variables and Fisher’s exact test for categorical variables. A negative mean difference in EQ-5D-5L values and Barthel Index scores indicates worsening of QOL/ADL.
To assess the impact of CFS score on patient outcomes, multiple linear regression analyses were employed to estimate adjusted effects on QOL/ADL. These models controlled for variables such as gender, age, Charlson Comorbidity Index, body mass index, ICU admission category, ICU admission type, APACHE2 score, maximum lactate levels, presence of acute kidney injury, sepsis, length of ICU stay, and whether the patient was in the not frail or the frail group, as well as their EQ-5D-5L or Barthel Index scores prior to admission. In the model, variables with missing data, including APACHE2 score and lactate levels, were treated as missing. Results were presented as β coefficients with 95% confidence intervals (CIs).
We also conducted two sensitivity analyses. Firstly, we used an alternative definition for “frailty” based on a previous study [7], defining it as a CFS score of 5 or greater [14]. Secondly, we analyzed CFS as a continuous variable.
In addition, we compared the characteristics of patients who had complete EQ-5D-5L or Barthel Index data at both admission and 6 months with those who did not, to examine potential differences between them. For the Barthel Index analysis, we included patients admitted on or after January 1, 2020, which is when we began collecting this data.
A p-value of < 0.05 was considered statistically significant. All statistical analysis was performed using Stata version 17 (StataCorp LP, College Station, TX).
Results
During the six-month period, 955 older participants admitted to ICUs via an emergency department visit were identified. After excluding specific cases (n = 305) and those who died within six months (n = 136), 514 participants (68.5%) had survived the six-month period. Of these, 390 participants provided complete responses to the EQ-5D-5L. Meanwhile, during a four-month time period, 237 participants provided Barthel Index responses (Fig. 1).
Ultimately, of the EQ-5D-5L responders, 242 participants were assigned to the not frail group and 148 to the frail group. For the Barthel Index responders, 132 were categorized into the not frail group and 105 into the frail group. The demographics and clinical characteristics of the participants are presented in Table 1. No patients with CFS scores of 8 or 9 were categorized.
The mean (SD) EQ-5D-5L scores decreased over six months for both not frail (0.80 [0.26] to 0.73 [0.27], p = 0.003) and frail groups (0.58 [0.26] to 0.50 [0.31], p = 0.002) (Fig. 2A). Similarly, Barthel Index scores dropped for not frail (98 [10] to 83 [31], p < 0.001) and frail (79 [27] to 61 [40], p < 0.001) (Fig. 2B). After stratification by each CFS score, both the EQ-5D-5L scores and Barthel Index scores showed a decreasing trend at six months compared to baseline (Additional file 1).
Differences in EQ-5D-5L scores between the not frail and frail groups are illustrated in a spider graph, capturing all five domains (Additional file 2). Regardless of the presence of frailty, the scores for mobility, self-care, and activities worsened significantly. However, unexpectedly, the scores for pain/discomfort in the frail group showed significant improvement. The differences in ADL between the not frail and the frail groups are summarized in a spider graph, depicting all 10 domains (Additional file 3). The mean scores for all domains, including feeding, movement, adjustment, bathing, toilet use, stairs, mobility, dressing, bladder control, and bowel control decreased from baseline to six months after admission for both the not frail and the frail groups.
Multiple linear regression analysis was conducted to determine the factors associated with the EQ-5D-5L and Barthel Index scores, respectively, at six months post-admission. The analysis demonstrated that frailty, based on CFS scores (1 to 3) at baseline before ICU admission (β coefficient, -0.15; 95% CI, − 0.23 to − 0.07; p < 0.001), APACHE2 score (β coefficient, -0.005; 95% CI, − 0.01 to − 0.002; p = 0.039), EQ-5D-5L score before ICU admission (β coefficient, 0.14; 95% CI, 0.02 to 0.26; p = 0.016), and length of ICU stay (β coefficient, -0.004; 95% CI, − 0.009 to − 0.0001; p < 0.001) were significantly associated with EQ-5D-5L scores at six months post-admission. Similarly, frailty (β coefficient, -12.3; 95% CI, − 23.9 to − 0.08; p = 0.036) and Barthel Index score before ICU admission (β coefficient, 0.54; 95% CI, 0.30 to 0.79; p < 0.001) were significantly associated with Barthel Index score at six months post-admission (Table 2).
In sensitivity analysis, frailty was associated with EQ-5D-5L and Barthel Index scores at six months post-ICU admission, even when using an alternative definition of frailty or treating it as a continuous variable (Additional files 4 and 5).
In additional analysis, the majority of patients with missing EQ-5D-5L or Barthel Index data were found to be missing this information at the 6-month follow-up, rather than at admission. Although the characteristics of patients with complete Barthel Index data and those with missing data were similar, patients with missing EQ-5D-5L data had higher CFS scores at admission (Additional file 6).
Discussion
In this post hoc analysis of the LIFE Study, a prospective, multicenter cohort study conducted in Japan, we found that older patients admitted to the ICU via the emergency department typically experienced a decline in QOL/ADL at six months post-ICU admission, irrespective of their frailty status. The APACHE2 score, initial EQ-5D-5L score, and Barthel Index score before ICU admission were significant predictors of long term health related QOL and ADL. Moreover, longer ICU stays negatively correlated with QOL. This study provides pivotal insights that could influence decisions regarding ICU admissions for older patients, given the limited available evidence.
Frailty, as gauged by CFS, plays an instrumental role in predicting unfavorable outcomes post-ICU admission. Our results reinforce frailty’s robust link to diminished QOL (EQ-5D-5L scores) and ADL (Barthel Index scores) over a six-month post-ICU period [15,16,17,18]. A recent study assessed the risk of in-hospital death among critically ill patients with pneumonia using CFS scores upon admission [19]. The findings suggest that frailty alone might not be an effective criterion for predicting short-term mortality. Nonetheless, recognizing the significant differences between frail and non-frail individuals is essential, not just for immediate survival but also for enhancing longer-term, patient-centered outcomes [20]. Our study uniquely focused on older patients in emergency intensive care in Japan, a country with a notably high proportion of older individuals, emphasizing the importance of long-term care and QOL post-emergency. Both the not frail and frail groups demonstrated a marked decline in QOL and ADL scores six months after ICU admission. This suggests that while frailty exacerbates the decline, ICU admission due to acute illness or injury poses a substantial burden to older patients, even if they were not frail at onset.
In examining the distinct functional capacities in QOL/ADL for both the not frail and the frail groups, we observed a deterioration in physical function post-ICU admission. However, the anxiety/depression composite remained stable. These findings are consistent with those from previous studies indicating that these psychological symptoms can remain stable over time in ICU survivors [21, 22]. Unexpectedly, there was a noticeable improvement in pain/discomfort scores in the frail group. This improvement might be partly attributed to the possibility that scores on ICU admission were inflated by the surrogate, given the patient’s ICU admission due to an acute illness or injury. Additionally, it is proposed that frail individuals might have an increased pain tolerance or could be underreporting their pain [23].
Our study aligns with previous research, which found that factors such as the APACHE2 score and initial EQ-5D-5L and Barthel Index scores prior to ICU admission were significant predictors for declines in QOL and ADL, respectively [18, 24, 25]. This emphasizes the criticality of initial assessments in anticipating long-term outcomes. Furthermore, in line with prior studies [24, 25], a longer ICU stay was significantly negatively correlated with QOL scores, suggesting it can predict a decline in long-term QOL.
The strength of this study lies in its examination of the associations between frailty and long-term patient-centered outcomes originating from the emergency department. This provides invaluable data for making decisions about ICU admission and predicting long-term outcomes after discharge. However, several limitations should be acknowledged. First, the measurement of CFS and QOL/ADL in this study was based on self-reporting. Patients or their surrogates might not accurately estimate CFS, QOL, and ADL prior to critical illness due to recall bias. Second, while the response rate for EQ-5D-5L was 76%, the Barthel Index had a lower response rate of only 46%. This discrepancy was because we did not collect Barthel Index data during the first two months of the entire six-month study period. Nonetheless, the fact that patients with missing EQ-5D-5L data had higher CFS scores at admission suggests the possibility of potential selection bias, warranting consideration in the interpretation of our findings. Third, we did not record the details of clinical course between ICU discharge and six months after ICU admission. Additional unmeasured or potential confounders such as physical rehabilitation and the other further complications may exist. Indeed, post-hospitalization interventions could lead to a subjective improvement in QOL for patients at risk of post-intensive care syndrome [26]. Fourth, assessing outcomes at a single time point (i.e., six months) may overlook important trends. Fifth, source of infection, which would impact long-term outcomes, was not available. Finally, the study is specific to the Japanese demographic and might need validation in other cultural and ethnic settings.
Despite these limitations, our study offers invaluable insights into the impact of ICU admissions on the QOL and ADL of older patients. It underscores the critical role frailty plays in the deterioration of patient outcomes, regardless of whether patients were frail at the onset of their ICU stay. Moreover, our findings have potential implications for healthcare providers in patient or family counseling and tailoring post-ICU care for the older patients. Future research should also prioritize the prevention of long-term QOL/ADL deterioration.
Conclusions
Our findings stress the importance of comprehensive assessments and shed light on the profound impacts on the long-term well-being of older patients, regardless of their baseline frailty. While ICU admissions undoubtedly save lives, post-ICU QOL/ADL for older patients, both frail and non-frail, should be a primary concern. Future research should prioritize the development of strategies that can mitigate the negative impacts of ICU admissions on the older patients, aiming for not just survival but also enhanced QOL/ADL post-ICU.
Availability of data and materials
The datasets from this study are available from the corresponding author upon request.
Abbreviations
- ADL:
-
Activities of daily living
- APACHE:
-
Acute Physiologic and Chronic Health Evaluation
- CFS:
-
Clinical Frailty Scale
- CI:
-
Confidence interval
- EQ-5D-5L:
-
Five-level EuroQol five-dimensional questionnaire
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- QOL:
-
Quality of life
- SD:
-
Standard deviations
References
Vincent JL, Creteur J. Appropriate care for the elderly in the ICU. J Intern Med. 2022;291:458–69.
Guidet B, de Lange DW, Flaatten H. Should this elderly patient be admitted to the ICU? Intensive Care Med. 2018;44:1926–8.
Groenland CNL, Termorshuizen F, Rietdijk WJR, van den Brule J, Dongelmans DA, de Jonge E, et al. Emergency department to ICU time is associated with hospital mortality: a registry analysis of 14,788 patients from Six University hospitals in the Netherlands. Crit Care Med. 2019;47:1564–71.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–95.
Muscedere J, Waters B, Varambally A, Bagshaw SM, Boyd JG, Maslove D, et al. The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med. 2017;43:1105–22.
Inaba M, Naito H, Yorifuji T, Nakamichi C, Maeyama H, Ishikawa H, et al. Impact of frailty on long-term mortality in older patients receiving intensive care via the emergency department. Sci Rep. 2023;13:5433.
Guidet B, de Lange DW, Boumendil A, Leaver S, Watson X, Boulanger C, et al. The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med. 2020;46:57–69.
Vest MT, Murphy TE, Araujo KL, Pisani MA. Disability in activities of daily living, depression, and quality of life among older medical ICU survivors: a prospective cohort study. Heal Qual Life Outcomes. 2011;5:9.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20:1727–36.
Mahoney FI, Barthel DW. Functional evaluation: the barthel index. Md State Med J. 1965;14:61–5.
Wubben N, Zegers M, Bisschops LLA, Frenzel T, van der Hoeven JG, van den Boogaard M. Using long-term predicted quality of life in ICU clinical practice to prepare patients for life post-ICU: a feasibility study. J Crit Care. 2022;68:121–8.
Ehooman F, Biard L, Lemiale V, Contou D, de Prost N, Mokart D, et al. Long-term health-related quality of life of critically ill patients with haematological malignancies: a prospective observational multicenter study. Ann Intensive Care. 2019;9:2.
Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14:392–7.
Rottler M, Ocskay K, Sipos Z, Görbe A, Virág M, Hegyi P, et al. Clinical Frailty Scale (CFS) indicated frailty is associated with increased in-hospital and 30-day mortality in COVID-19 patients: a systematic review and meta-analysis. Ann Intensive Care. 2022;12:17.
Villa P, Pintado MC, Luján J, González-García N, Trascasa M, Molina R, et al. Functional status and quality of life in elderly intensive care unit survivors. J Am Geriatr Soc. 2016;64:536–42.
Brummel NE, Bell SP, Girard TD, Pandharipande PP, Jackson JC, Morandi A, et al. Frailty and subsequent disability and mortality among patients with critical illness. Am J Respir Crit Care Med. 2017;196:64–72.
Bagshaw SM, Stelfox HT, Johnson JA, McDermid RC, Rolfson DB, Tsuyuki RT, et al. Long-term association between frailty and health-related quality of life among survivors of critical illness: a prospective multicenter cohort study. Crit Care Med. 2015;43:973–82.
Heyland DK, Garland A, Bagshaw SM, Cook D, Rockwood K, Stelfox HT, et al. Recovery after critical illness in patients aged 80 years or older: a multi-center prospective observational cohort study. Intensive Care Med. 2015;41:1911–20.
Darvall JN, Bellomo R, Bailey M, Paul E, Young PJ, Rockwood K, et al. Frailty and outcomes from pneumonia in critical illness: a population-based cohort study. Br J Anaesth. 2020;125:730–8.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–62.
Jackson JC, Hart RP, Gordon SM, Shintani A, Truman B, May L, et al. Six-month neuropsychological outcome of medical intensive care unit patients. Crit Care Med. 2003;31:1226–34.
Hatch R, Young D, Barber V, Griffiths J, Harrison DA, Watkinson P. Anxiety, depression and post traumatic stress disorder after critical illness: a UK-wide prospective cohort study. Crit Care. 2018;22:310.
Herr KAGL. Assessment and measurement of pain in older adults. Clin Geriatr Med. 2001;17:457–78.
Herridge MS, Chu LM, Matte A, Tomlinson G, Chan L, Thomas C, et al. The RECOVER Program: disability risk groups and 1-Year outcome after 7 or more days of mechanical ventilation. Am J Respir Crit Care Med. 2016;194:831–44.
Cuthbertson BH, Roughton S, Jenkinson D, Maclennan G, Vale L. Quality of life in the five years after intensive care: a cohort study. Crit Care. 2010;10:R6.
Daniels LM, Johnson AB, Cornelius PJ, Bowron C, Lehnertz A, Moore M, et al. Improving quality of life in patients at risk for post-intensive care syndrome. Mayo Clin Proc Innov Qual Outcomes. 2018;2:359–69.
Acknowledgements
We thank the members of the LIFE study group for suggesting the study concept and design. The authors thank Christine Burr for editing the manuscript.
We thank Kaoru Masuda (Department of Emergency, Critical Care, and Disaster Medicine, Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences) for her assistance with data management.
LIFE Study Investigators
Mototaka Inaba - Department of Emergency, Critical Care, and Disaster Medicine, Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences, Okayama, Japan, Hiromichi Naito - Department of Emergency, Critical Care, and Disaster Medicine, Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences, Okayama, Japan, Takashi Yorifuji - Department of Epidemiology, Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences, Okayama, Japan, Chikaaki Nakamichi - Advanced Emergency and Critical Care Center, National Hospital Organization, Nagasaki Medical Center, Omura, Japan, Hiroki Maeyama - Emergency and Critical Care Center, Tsuyama Chuo Hospital, Tsuyama, Japan, Hideki Ishikawa - Trauma and Resuscitation Center, Teikyo University Hospital, Tokyo, Japan, Nobuaki Shime - Department of Emergency and Critical Care Medicine, Graduate School of Biomedical & Health Sciences, Hiroshima University, Hiroshima, Japan, Sadayori Uemori - Department of Emergency, Yodogawa Christian Hospital, Osaka, Japan, Satoshi Ishihara - Department of Emergency and Critical Care, Hyogo Emergency Medical Center, Kobe, Japan, Makoto Takaoka - Acute care division, Harima-himeji General Medical Center, Himeji, Japan, Tsuyoshi Ohtsuka - Emergency Department, National Hospital Organization Yokohama Medical Center, Yokohama, Japan, Masahiro Harada - Department of Emergency and Critical Care, National Hospital Organization Kumamoto Medical Center, Kumamoto, Japan, Satoshi Nozaki - Emergency Department, Okayama Saiseikai General Hospital, Okayama, Japan, Keisuke Kohama - Department of Emergency, Disaster, and Critical Care Medicine, Hyogo College of Medicine, Nishinomiya, Japan, Ryota Sakurai - Department of Emergency and Critical Care Medicine, Faculty of Medicine, Saga University, Saga, Japan, Shuho Sato - Emergency Medical Center, Saiseikai Senri Hospital, Suita, Japan, Shun Muramatsu - Emergency Department, Japanese Red Cross Medical Center, Tokyo, Japan, Kazunori Yamashita - Acute & Critical Care Center, Nagasaki University Hospital, Nagasaki, Japan, Toshihiko Mayumi - Department of Emergency Medicine, University of Occupational and Environmental Health Hospital, Kitakyushu, Japan, Kaoruko Aita - Uehiro Division, Center for Death and Life Studies and Practical Ethics, Graduate School of Humanities and Sociology, University of Tokyo, Tokyo, Japan, Atsunori Nakao - Department of Emergency, Critical Care, and Disaster Medicine, Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences, Okayama, Japan, Satoshi Mochizuki - National Hospital Organization Yokohama Medical center, Yokohama, Japan, Hirofumi Itoh - National Hospital Organization Yokohama Medical center, Yokohama, Japan, Asase Senda - Saiseikai Senri Hospital, Suita, Japan, Kana Otani - Yodogawa Christian Hospital, Osaka, Japan, Chison Gon - National Hospital Organization Nagasaki Medical Center, Omura, Japan, Shunsuke Taito - Hiroshima University Hospital, Hiroshima, Japan, Takeshi Ohnishi - Hyogo Emergency Medical Center, Kobe, Japan, Yuji Taguchi - Steel Memorial Hirohata Hospital, Himeji, Japan, Toru Miike - Saga University Hospital, Saga, Japan, Koki Umeda - University of Occupational and Environmental Health Hospital, Kitakyushu, Japan, Yuji Kondo - Japanese Red Cross Medical Center, Tokyo, Japan, Takao Arai - Tokyo Medical University Hachioji Medical Center, Hachioji, Japan, Junya Tsurukiri - Tokyo Medical University Hachioji Medical Center, Hachioji, Japan.
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Consortia
Contributions
TH, TYu, MI, ST, and HN designed the concept of the study. TH, TYu, MI, ST, and HN conducted the study and performed the data acquisition. TH, TYu, TYo, HN, and AN assessed the quality of the study and performed the data analysis and interpretation. TH, TYu, HN, and AN wrote the manuscript, and the other authors made substantial revisions and edits. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study conforms to the principles outlined in the Declaration of Helsinki and was approved from the Okayama University Hospital Ethics Committee, ID: K-2308-008. Patient consent was waived for all participants enrolled in this study from the Okayama University Hospital Ethics Committee, because of the retrospective study design.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hongo, T., Yumoto, T., Inaba, M. et al. Long-term, patient-centered, frailty-based outcomes of older critical illness survivors from the emergency department: a post hoc analysis of the LIFE Study. BMC Geriatr 24, 257 (2024). https://doi.org/10.1186/s12877-024-04881-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-04881-x