Abstract
Background
Frailty is a common geriatric syndrome related to multiple adverse outcomes. Sex differences in its prevalence and impact on mortality remain incompletely understood.
Methods
This study was conducted with data from the I-Lan Longitudinal Aging Study, in which community-dwelling subjects aged > 50 years without coronary artery disease or diabetes were enrolled. Sex disparities in phenotypically defined frailty and sex–morality predictor interactions were evaluated. Sex- and frailty-stratified analyses of mortality were performed.
Results
The sample comprised 1371 subjects (51.4% women, median age 61 years). The median follow-up period was 6.3 (interquartile range, 5.8–7.0) years. The frailty prevalence did not differ between men (5.3%) and women (5.8%). Frail individuals were older and less educated and had poorer renal function than did non-frail individuals. Body composition trends differed between sexes, regardless of frailty. Relative to non-frail men, frail men had significantly lower body mass indices (BMIs; 24.5 vs. 23.4 kg/m2, p = 0.04) and relative appendicular skeletal muscle masses (7.87 vs. 7.05 kg/m2, p < 0.001). Frail women had significantly higher BMIs (25.2 vs. 23.9 kg/m2, p = 0.02) and waist circumferences (88 vs. 80 cm, p < 0.001) than did non-frail women. Frailty was an independent mortality predictor for men only [hazard ratio (95% confidence interval) = 3.395 (1.809–6.371), psex–frailty interaction = 0.03].
Conclusion
Frailty reflected poorer health in men than in women in the present cohort. This study revealed sex disparities in the impact of frailty on mortality among relatively healthy community-dwelling older adults.
Similar content being viewed by others
Introduction
Frailty is a complex geriatric syndrome representing cumulative physiological decline, increased vulnerability, and the depletion of health reserves [1,2,3]. The commonly used phenotypic Fried frailty index (FFI) consists of five criteria: unintentional weight loss, exhaustion, low energy expenditure, slow gait speed, and weak grip strength [4]. Frailty affects older adults and those in the middle years by FFI or deficits accumulation approach [5,6,7]. Physical frailty is related to unfavorable health-related outcomes in nearly 500,000 participants with a mean age of 56 and is probably associated with altering brain structure [8]. Epidemiological studies have demonstrated that frailty, although inconclusively defined, frailty is significantly associated with mortality, including middle-aged individuals with or without comorbidities [1, 9, 10].
Reported effects of sex on the prevalence of frailty and its association with mortality are inconsistent and highly variable due to the use of different frailty assessments and the diversity of study populations [1, 10]. In community-dwelling and institutionalized populations, frailty has been reported to be more prevalent among women than among men of the same age [11, 12]. In contrast, no sex difference in the prevalence of frailty was observed in the Korean population without diabetes [13]. Few studies have directly compared the frailty–mortality relationship according to sex [14,15,16]. A meta-analysis revealed that females live longer than males in the general population despite comorbidities or frailty. Still, the authors noted that the included studies exhibited high heterogeneity [11]. In contrast, another study showed no significant sex difference in all-cause mortality for frail older men and women relative to robust individuals [17]. The impact of frailty–sex interaction on mortality remains uncertain [18, 19].
Although the FFI criteria are used most in clinical practice and could identify the shirking syndrome [4], body weight and body composition in frail populations were contradictory, and few studies examined only in elderly populations [20,21,22]. Higher body fat and body mass index (BMI) are positively correlated with frailty in a total of 29,937 participants aged ≥50 years from 2 large cohorts [23]; however, there were potential sex differences in the defining of frailty and body composition characteristics. We performed this study to 1) differentiate biological factors of frailty between sexes and 2) directly compare the relationship between phenotypic frailty and all-cause mortality between relatively healthy middle-aged to older men and women in Taiwan.
Methods
Study population
The present retrospective cohort study was performed with data from the I-Lan Longitudinal Aging Study (ILAS), conducted with a cohort of community-dwelling adults aged > 50 years who were recruited randomly via household registration records in I-Lan County, Taiwan. The exclusion criteria were: (i) inability to cooperate or communicate with the investigators; (ii) refusal of consent; (iii) current institutionalisation; (iv) known active disease, such as cancer, sepsis, heart failure or chronic obstructive pulmonary disease, or functional dependence; (v) life expectancy < 6 months; and (vi) plan to leave I-Lan County in the near future. The participants were randomly sampled through the county’s household registrations in Youanshan Township of I-lan County. The selected residents were invited to participate by mail or telephone invitations extended by the research team. From August 2011 to August 2013, well-trained research nurses interviewed all potential participants in person to assess their eligibility before they provided written informed consent. The ILAS design, participant recruitment and data collection have been reported elsewhere [24]. The study was conducted according to the Declaration of Helsinki and was approved by the institutional review board of National Yang-Ming Chiao Tung University (no. YM103008).
Collection of anthropometric, demographic and laboratory data
A research nurse collected demographic and medical data (e.g. educational level, smoking habit, medical history) on the participants via personal interviews and medical records review. Participants’ brachial blood pressure was measured with a mercury sphygmomanometer after they had rested for at least 15 min. Peripheral blood samples were collected between 7 and 9 am after a ≥ 10-h fast for determination of the of haemoglobin A1c (HbA1c), fasting blood glucose (FBG), total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein, triglyceride (TG) and uric acid (UA) concentrations using an automatic analyser (ADVIA 1800; Siemens, Malvern, PA, USA).
Metabolic syndrome (MS) was defined according to the criteria proposed by Taiwan’s Ministry of Health and Welfare as the presence of more than three of the following risk determinants: (i) waist circumference (WC) > 90 cm for men or > 80 cm for women; (ii) systolic blood pressure ≥ 130 mmHg, diastolic blood pressure ≥ 85 mmHg or antihypertensive agent use; (iii) HDL concentration < 40 mg/dL for men or < 50 mg/dL for women; (iv) TG concentration ≥ 150 mg/dL; and (v) FBG level ≥ 100 mg/dL or antihyperglycemic agent use. Central obesity was evaluated with the WC and waist-to-height ratio (WHtR) [25]. Chronic kidney disease was defined as estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73 m2, calculated using the Chronic Kidney Disease Epidemiology Collaboration equation [26]. Hypertension was defined as self-reported current antihypertensive medication prescription, systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg. Multimorbidity was identified using the Charlson comorbidity index (CCI) [27].
Assessment of body composition, muscle strength and physical performance
Participants’ total fat mass and fat-free lean body mass were measured by whole-body dual-energy X-ray absorptiometry using a Lunar Prodigy device (GE Healthcare, Madison, WI, USA). The total body fat percentage was calculated as the total fat mass divided by the total body mass multiplied by 100 [28]. Handgrip strength was measured with a digital dynamometer (Smedlay’s Dynamo Meter; TTM, Tokyo, Japan), with the best performance among three trials recorded [29]. The appendicular skeletal muscle mass (ASM) was calculated as the sum of the four limbs’ lean soft-tissue mass, determined by dual-energy X-ray absorptiometry. The height-adjusted muscle index, or relative appendicular skeletal muscle mass (RASM), was calculated by dividing the ASM by the height squared [28]. Low muscle mass was defined according to the recommendation of the Asian Working Group for Sarcopenia [30] as RASM < 7.0 kg/m2 for men and < 5.4 kg/m2 for women.
Physical frailty assessment
Physical frailty was identified using the FFI criteria [4], and participants’ physical activity was assessed using the Taiwanese version of the short-form Instrumental Physical Activity Questionnaire (IPAQ) [31]. The interviewer measured participants’ gait speed using the 6-m straight-line walking test and a stopwatch (HS-70 W; Casio Computer Co., Ltd., Tokyo, Japan) [32]. The low activity level, weakness and slowness parameters were defined by the lowest quintiles of the IPAQ score, sex-specific handgrip strength and sex-specific gait speed, respectively. Unintentional weight loss was ascertained using the threshold of ≥4.5 kg in the past year. Exhaustion was defined by self-reported ease of becoming weary or tired or inability to carry out ordinary daily tasks within the past week. Participants who fulfilled at least three FFI criteria were classified as frail, those who fulfilled one or two criteria were classified as prefrail and those who fulfilled no criterion were classified as robust. Non-frailty was defined as robustness and prefrailty.
Determination of mortality
Follow-up were conducted between January 2018 and December 2019 according to telephone calls, and participants’ vital status was determined by telephone interviews. As follow-up medical records were not available, the causes of mortality were unknown.
Statistical analysis
Categorical variables are expressed as frequencies and percentages, non-normally distributed continuous variables are expressed as medians with interquartile ranges and normally distributed continuous variables are expressed as means ± standard deviations. The Mann–Whitney U test and Fisher’s exact test were used to compare continuous and categorical variables, respectively, between groups. Stepwise backward logistic regression was used to identify significant predictors of physical frailty. Cox proportional-hazard regression analysis was used to examine the effect of frailty status on mortality separately among men and women. Factors that were significant in univariate regression analyses (p < 0.2) were entered into a multivariable regression analysis. Hazard ratios (HRs) with 95% confidence intervals (CIs) for mortality risk were calculated. Sex- and frailty-stratified mortality comparisons were performed using the log-rank test and Kaplan–Meier method. We performed the interaction testing to quantify the influence of sex on the relationship between characteristics and physical frailty and mortality. We were missing lean body mass and total body fat percentage data on 3 participants in frail men and women, repspectively and 9 in nonfrail women, 26 in nonfrail men. There were no significant differences in sex, age, or physical frailty status between those with and without the DXA scan data. The statistical analyses were performed using the SPSS software (version 23.0; IBM Corporation, Armonk, NY, USA). Two-tailed p values < 0.05 were regarded as significant.
Results
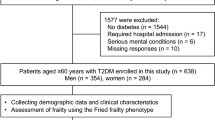
Of 1798 community-dwelling older adults attending initial interviews, 427 subjects were excluded from the ILAS because they had coronary artery disease (n = 90), diabetes (n = 320) or incomplete data (n = 10; Fig. 1). The study sample thus comprised 1371 participants (51.4% women) with a median age of 61.0 years. The median follow-up period was 6.3 (interquartile range, 5.8–7.0) years and 147 (10.7%) participants died. The subjects’ frailty prevalence was 5.5%, and pre-fail was 38.7%. Women were significantly younger and had fewer years of education, a lesser smoking prevalence, a lesser RASM, and lower blood TG and UA levels than men. Women had significantly higher total body fat percentage, HDL and HbA1c concentrations and eGFRs than men. The prevalence of frailty, mortality rate, hypertension and MS and the CCI value did not differ between the sexes (Table 1).
Sex disparities stratified by frailty status are shown in Table 2. Frail subjects of both sexes were significantly older and had less education, poorer renal function, higher CCI values and higher mortality than did their non-frail counterparts. Among women, frail subjects had significantly lower total cholesterol and HDL levels and higher TG levels than did non-frail subjects. Frail men had lower HDL levels than did non-frail men, with no difference in any other lipid parameter or the FBG, HbA1c or UA level. Different trends in body composition were observed in men and women. Compared with non-frail women, frail women had significantly higher body mass indices (frail vs non-frail, 25.2 vs. 23.9 kg/m2, p = 0.02), WCs (frail vs non-frail, 88 vs. 80 cm, p < 0.001), and WHtRs (frail vs non-frail, 0.58 vs. 0.52, p < 0.001). In contrast, frail males had significantly lower BMIs (frail vs non-frail, 23.4 vs. 24.5 kg/m2, p = 0.04) and RASMs (frail vs non-frail, 7.05 vs. 7.99 kg/m2, p < 0.001) than did non-frail males, with no difference in the WHtR (0.54 and 0.51, respectively) or WC (87 and 85 cm, respectively). Significant BMI, WC, and WHtR interaction between sexes was detected. No sex disparity in low muscle mass was observed. The impact of frailness on mortality in men is more dominant than in women (women frail vs. non-frail 22.0 vs 9.2; men frail vs non-frail 48.6 vs 9.5).
In examining the individual physical frailty criteria, self-reported exhaustion was significantly more prevalent among women than men in frail participants (Supplement Fig. 1a). Different from the characteristics of frail, pre-frail women were more likely than men to meet the criteria for low activity; otherwise, prefrail men were greater of slowness (Supplement Fig. 1b.).
In the adjusted multivariate analyses, mortality was associated independently with age [HR (95% CI) = 1.038 (1.005–1.073)] and low muscle mass [HR (95% CI) = 2.243 (1.275–3.946)] among women, and with age [HR (95% CI) = 1.060 (1.028–1.092)], smoking [HR (95% CI) = 1.926 (1.190–3.119)] and frailty [HR (95% CI) = 3.395 (1.809–6.371)] among men (Table 3). The survival rate was lowest for frail men (Log ranp < 0.001; Fig. 2).
Discussion
In this study, the prevalence of frailty did not differ between men and women aged > 50 years. The mortality rate was higher for frail than for non-frail subjects. Frail men had significantly less muscle mass and central obesity and were thinner than non-frail men, whereas frail women had a higher BMI, WC and WHtR, but not reduced muscle mass compared with non-frail women. Frailty was an independent risk factor for all-cause mortality for men, but not women. Thus, the main study finding is that the frailty phenotype is a more pronounced indicator of poor health among men than among women.
Our results differ from previous findings in that women was not more prevalent than men, possibly because healthier subjects were enrolled in our study. Although frailty increases the risk of mortality under various assessing approaches, the prevalence of frailty was heterogeneous. The results include that females were more prevalent of frailty by Fried frailty criteria [10], and frailty index [33, 34] and the contrary result even using the same evaluation methods of frailty [15, 35, 36]. Sex may have a different impact on the association of frailty using physical frailty or accumulation deficit model [15, 36]. In this study, we used physical criteria to analyze the relationship between frailty and mortality between sexes; we also incorporated body composition in the analysis of frailty, which was a lack of investigation in the previous studies.
Frailty in relation to sex differences in body composition and cultural factors
Frailty involves complex interplay among biological, behavioural and social factors, which may underpin the sex difference therein. Our study revealed opposing trends in body composition among frail men and women. Lower muscle mass was more prevalent among frail men than among frail women but was an independent mortality risk factor only for women in analyses adjusted for multiple variables. Our findings demonstrate that frail men reflect more cachexia condition and adequately capture the health deficits than do women.
Consistent with our results, women have been found to be more likely to self-report exhaustion than other clinical frailty components [35]. However, women appear to be more likely to demonstrate difficulty with instrumental activities of daily living, non-lethal functional problems and depressive symptoms [37]. Both men and women report fatigue, but women exhibit more related psychosocial problems, whereas men more often report disability [38]. From a pathophysiological perspective, the chronic disease hypothesis may explain these patterns. Sex differences in multimorbidity have been reported and women presented functional impairment but the non-fatal spectrum of diagnoses [39]. Central obesity, which may have non-fatal sequelae such as osteoarthritis, has more significant impacts and leads to lengthier disability in females than in males [37, 40].
Limitations
This study has several limitations. First, as it was observational, the adjustment of the analyses may not have covered all potential confounding factors. Second, frail status was not reassessed again in this study; therefore, we could not know the dynamic change of frailty during follow-up duration, like non-frail (including prefrail and robust) became frailty. Third, there are numerous differences between sex and probably related to frailty, including biological factors, nutrition, frequency of exercise and the social aspects are the possible confounders which could not be wholly excluded. Fourth, as disabled subjects and those unable to complete the physical function evaluation were not enrolled in the ILAS, the prevalence of frailty may have been underestimated. Fifth, confined by the cohort longitudinal observational study, the possible underlying pathophysiology could not be elucidated. The intervention to reverse frailty and the generalisability of our findings must be investigated in further research.
Conclusion
Although the prevalence of frailty did not differ between sexes in this study, the impact of frailty on all-cause mortality was more pronounced for men than for women. The observed sex disparities in the effects of frailty on health outcomes warrant further exploration.
Availability of data and materials
The datasets analysed during the current study available from the corresponding author on reasonable request. Please contact the corresponding author, Po-Hsun, Huang (huangbsvgh@gmail.com ), for data access.
References
Shamliyan T, Talley KMC, Ramakrishnan R, Kane RL. Association of frailty with survival: a systematic literature review. Ageing Res Rev. 2013;12(2):719–36.
Eeles EM, White SV, O'Mahony SM, Bayer AJ, Hubbard RE. The impact of frailty and delirium on mortality in older inpatients. Age Ageing. 2012;41(3):412–6.
Walston J, Hadley EC, Ferrucci L, Guralnik JM, Newman AB, Studenski SA, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging research conference on frailty in older adults. J Am Geriatr Soc. 2006;54(6):991–1001.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56.
Ghosh A, Kundu M, Devasenapathy N, Woodward M, Jha V. Frailty among middle-aged and older women and men in India: findings from wave 1 of the longitudinal ageing study in India. BMJ Open. 2023;13(7):e071842.
Jang AR, Sagong H, Yoon JY. Frailty trajectory among community-dwelling middle-aged and older adults in Korea: evidence from the Korean longitudinal study of aging. BMC Geriatr. 2022;22(1):524.
Segaux L, Broussier A, Oubaya N, Leissing-Desprez C, Laurent M, Naga H, et al. Several frailty parameters highly prevalent in middle age (50-65) are independent predictors of adverse events. Sci Rep. 2021;11(1):8774.
Jiang R, Noble S, Sui J, Yoo K, Rosenblatt M, Horien C, et al. Associations of physical frailty with health outcomes and brain structure in 483 033 middle-aged and older adults: a population-based study from the UK biobank. Lancet Digit Health. 2023;5(6):e350–9.
Pritchard JM, Kennedy CC, Karampatos S, Ioannidis G, Misiaszek B, Marr S, et al. Measuring frailty in clinical practice: a comparison of physical frailty assessment methods in a geriatric out-patient clinic. BMC Geriatr. 2017;17(1):264.
Hanlon P, Nicholl BI, Jani BD, Lee D, McQueenie R, Mair FS. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493 737 UK biobank participants. Lancet Public Health. 2018;3(7):e323–32.
Gordon EH, Peel NM, Samanta M, Theou O, Howlett SE, Hubbard RE. Sex differences in frailty: a systematic review and meta-analysis. Exp Gerontol. 2017;89:30–40.
Chen C-Y, Wu S-C, Chen L-J, Lue B-H. The prevalence of subjective frailty and factors associated with frailty in Taiwan. Arch Gerontol Geriatr. 2010;50:S43–7.
Kang S, Oh TJ, Cho BL, Park YS, Roh E, Kim HJ, et al. Sex differences in sarcopenia and frailty among community-dwelling Korean older adults with diabetes: the Korean frailty and aging cohort study. J Diabetes Investig. 2021;12(2):155–64.
Srinonprasert V, Chalermsri C, Aekplakorn W. Frailty index to predict all-cause mortality in Thai community-dwelling older population: a result from a National Health Examination Survey cohort. Arch Gerontol Geriatr. 2018;77:124–8.
Berges I-M, Graham JE, Ostir GV, Markides KS, Ottenbacher KJ. Sex differences in mortality among older frail Mexican Americans. J Women’s Health. 2009;18(10):1647–51.
Kulmala J, Nykänen I, Hartikainen S. Frailty as a predictor of all-cause mortality in older men and women. Geriatr Gerontol Int. 2014;14(4):899–905.
Fan Y, Huang J, Zhou Y, Gu X, Gong D. Does the impact of frailty on all-cause mortality in older persons differ between women and men? A Meta-analysis. J Am Med Dir Assoc. 2021;22(3):606.e601–6.
Maeda D, Matsue Y, Kagiyama N, Jujo K, Saito K, Kamiya K, et al. Sex differences in the prevalence and prognostic impact of physical frailty and sarcopenia among older patients with heart failure. Nutr Metab Cardiovasc Dis. 2022;32(2):365–72.
Sun LY, Tu JV, Coutinho T, Turek M, Rubens FD, McDonnell L, et al. Sex differences in outcomes of heart failure in an ambulatory, population-based cohort from 2009 to 2013. CMAJ : Canad Med Assoc. 2018;190(28):E848–e854.
Blaum CS, Xue QL, Michelon E, Semba RD, Fried LP. The association between obesity and the frailty syndrome in older women: the Women's health and aging studies. J Am Geriatr Soc. 2005;53(6):927–34.
Boutin E, Natella P-A, Schott A-M, Bastuji-Garin S, David J-P, Paillaud E, et al. Interrelations between body mass index, frailty, and clinical adverse events in older community-dwelling women: the EPIDOS cohort study. Clin Nutr. 2018;37(5):1638–44.
Sheehan KJ, O’Connell MDL, Cunningham C, Crosby L, Kenny RA. The relationship between increased body mass index and frailty on falls in community dwelling older adults. BMC Geriatr. 2013;13(1):132.
Jayanama K, Theou O, Godin J, Mayo A, Cahill L, Rockwood K. Relationship of body mass index with frailty and all-cause mortality among middle-aged and older adults. BMC Med. 2022;20(1):404.
Liu LK, Lee WJ, Chen LY, Hwang AC, Lin MH, Peng LN, et al. Sarcopenia, and its association with cardiometabolic and functional characteristics in Taiwan: results from I-Lan longitudinal aging study. Geriatr Gerontol Int. 2014;14(Suppl 1):36–45.
Ashwell M, Hsieh SD. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int J Food Sci Nutr. 2005;56(5):303–7.
Liu X, Gan X, Chen J, Lv L, Li M, Lou T. A new modified CKD-EPI equation for Chinese patients with type 2 diabetes. PLoS One. 2014;9(10):e109743.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Peng LN, Lee WJ, Liu LK, Lin MH, Chen LK. Healthy community-living older men differ from women in associations between myostatin levels and skeletal muscle mass. J Cachexia Sarcopenia Muscle. 2018;9(4):635–42.
Xue QL, Bandeen-Roche K, Varadhan R, Zhou J, Fried LP. Initial manifestations of frailty criteria and the development of frailty phenotype in the Women's health and aging study II. J Gerontol A Biol Sci Med Sci. 2008;63(9):984–90.
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15(2):95–101.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95.
Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K. Validity and reliability of the Edmonton frail scale. Age Ageing. 2006;35(5):526–9.
García-González JJ, García-Peña C, Franco-Marina F, Gutiérrez-Robledo LM. A frailty index to predict the mortality risk in a population of senior mexican adults. BMC Geriatr. 2009;9(1):47.
Dallmeier D, Braisch U, Rapp K, Klenk J, Rothenbacher D, Denkinger M, et al. Frailty index and sex-specific 6-year mortality in community-dwelling older people: the ActiFE study. J Gerontol: Series A. 2020;75(2):366–73.
Theou O. O‘Connell MDL, king-Kallimanis BL, O'Halloran AM, Rockwood K, Kenny RA: measuring frailty using self-report and test-based health measures. Age Ageing. 2015;44(3):471–7.
Bartley MM, Geda YE, Christianson TJ, Pankratz VS, Roberts RO, Petersen RC. Frailty and mortality outcomes in cognitively Normal older people: sex differences in a population-based study. J Am Geriatr Soc. 2016;64(1):132–7.
Crimmins EM, Kim JK, Solé-Auró A. Gender differences in health: results from SHARE, ELSA and HRS. Eur J Pub Health. 2011;21(1):81–91.
Bensing JM, Hulsman RL, Schreurs KM. Gender differences in fatigue: biopsychosocial factors relating to fatigue in men and women. Med Care. 1999;37(10):1078–83.
Abad-Díez JM, Calderón-Larrañaga A, Poncel-Falcó A, Poblador-Plou B, Calderón-Meza JM, Sicras-Mainar A, et al. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr. 2014;14:75.
Ferrucci L, Turchi A, Fumagalli S, Di Bari M, Silvestrini G, Zacchei S, et al. Sex-related differences in the length of disability prior to death in older persons. Aging Clin Exp Res. 2003;15(4):310–4.
Acknowledgements
We are grateful to all participants for their involvement.
Funding
This study was supported in part by research grants from the Novel Bioengineering and Technological Approaches to Solve Two Major Health Problems in Taiwan program, sponsored by the Taiwan Ministry of Science and Technology Academic Excellence Program (MOST 108–2633-B-009-001); Taipei Veterans General Hospital (VGH-V100E2–002 and VGHUST103-G7–2-1); the National Taiwan University Hospital, Hsinchu Branch (107-HCH002 and 108-HCH004); and the Ministry of Science and Technology (MOST-105-2314-B-002–119, 106–2314-B-002–173-MY3, MOHW 106-TDU-B-211-113001). The funding institutions took no part in the study design, data collection or analysis, publication intent, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
Data were interpreted and analyzed by YWL and CCC with assistance from RHC. YWL drafted the manuscript. CCC and PHH revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional review board of National Yang-Ming Chiao Tung University (no. YM103008). All participants provided written informed consent before enrolment. All methods were performed in accordance with the relevant guidelines and regulations (Declaration of Helsinki).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lu, YW., Chang, CC., Chou, RH. et al. Sex differences in the frailty phenotype and mortality in the I-Lan longitudinal aging study cohort. BMC Geriatr 24, 182 (2024). https://doi.org/10.1186/s12877-024-04785-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-04785-w