Abstract
Background
Good oral health is an important part of healthy ageing, yet there is limited understanding regarding the status of oral health care for older people globally. This study reviewed evidence (policies, programs, and interventions) regarding oral health care for older people.
Methods
A systematic search of six databases for published and grey literature in the English language by the end of April 2022 was undertaken utilising Arksey and O’Malley’s scoping review framework.
Results
The findings from oral health policy documents (n = 17) indicated a lack of priorities in national health policies regarding oral health care for older people. The most common oral health interventions reported in the published studies (n = 62) included educational sessions and practical demonstrations on oral care for older adults, nurses, and care providers. Other interventions included exercises of facial muscles and the tongue, massage of salivary glands, and application of chemical agents, such as topical fluoride.
Conclusion
There is currently a gap in information and research around effective oral health care treatments and programs in geriatric dental care. Efforts must be invested in developing guidelines to assist both dental and medical healthcare professionals in integrating good oral health as part of healthy ageing. Further research is warranted in assessing the effectiveness of interventions in improving the oral health status of the elderly and informing approaches to assist the integration of oral health into geriatric care.
Similar content being viewed by others

Background
The ageing population worldwide is increasing rapidly. Worldwide, there were over 703 million (9%) people aged 60 years or older in 2020, and expected to increase to 1.5 billion (16.0%) by 2050 [1]. The population is ageing in low-and middle-income countries (LMICs) as well as in high-income countries (HICs) [1, 2], however, the majority (> 80%) will be living in LMICs by 2050 [2]. Ageing is often associated with physiological changes, low appetite, and nutritional problems. Chronic diseases and any medications taken for them may result in a decrease in salivary flow (hyposalivation), leading to chewing (mastication) and swallowing difficulties (dysphagia), which may prevent adequate nutritional intake [3,4,5]. People with dysphagia are also reported to have a lower quality of life. Further, hyposalivation can lead to a greater incidence of coronal and root caries and periodontitis, which ultimately may lead to tooth loss [6, 7] that in turn negatively impacts chewing function, aesthetics, self-perception, and quality of life. Periodontitis, the prevalence of which also increases with age, affects the majority of seniors [8, 9], is causally linked with aspiration pneumonia, resulting in morbidity, hospitalization, and mortality [8]. Further, poor oral health is linked to, and compounded by, the development of several systemic health conditions, such as cardiovascular disease [3, 10] and diabetes mellitus [11,12,13], and all which compromise the health of older people.
Globally, the share of chronic and non-communicable diseases (NCDs), such as cardiovascular diseases, cancer, diabetes, and chronic obstructive pulmonary diseases (COPD), is substantially greater among older populations than in younger age groups [14, 15]. Oral diseases share the common risk factors such as unhealthy diet high in sugar, use of tobacco, and harmful use of alcohol with these other major NCDs [3, 10]. Older populations with NCDs are also more likely to develop oral health problems and those with poor oral health conditions are likely to manage their NCDs poorly. Ageing population are likely to develop NCDs which have a negative impact on oral health [16], that is associated with overall health, comfort, dignity, and well-being [17].
Poor oral health, including dental caries, periodontal diseases and the resulting tooth loss, induce a change in food selection and dietary patterns, potentially resulting in frailty and dependency [18,19,20], subsequently affecting general well-being and quality of life [21]. There are several factors causing poor oral health outcomes among the older population. A recently conducted systematic review identified some key determinants to oral health frailty among older populations, including oral health status deterioration, few remaining teeth, reduced oral motor skills, oral diadochokinetic and chewing, swallowing, and saliva disorders [22].
Improving oral health outcomes of the older population requires adequate oral health interventions tailored to the specific needs of this age group that will influence their quality of life [23, 24]. Improvement in oral health status can have a significant positive impact. For example, older people with more natural, intact teeth have reported a perceived greater quality of life, positive body image, increased self-worth, maintenance of oral function, and sense of achievement [25, 26]. However, there are currently several barriers to receiving oral healthcare for the older population, such as limited access to professional oral health care providers. Furthermore, geriatric dentistry is not a recognized specialty in most countries [27]. Within this context, innovative oral health promotion programs that co-manage oral health problems with other healthcare providers may be important to address the unmet needs of older populations. Oral health promotion programs at a primary care level can play a significant role in maintaining better overall health and quality of life outcomes for the aging population. However, there is limited understanding in these areas. Moreover, there is also a paucity of information on programs that have involved non-dental professionals to address the oral health problems of older populations [28].
Some programs do exist, for instance one in Australia, where Registered Nurses (RNs) and General Practitioners (GPs) involved in aged care settings across the country were trained to promote oral health, with this program successfully being rolled out to more than 80% of residential aged care homes nationally. However, a thorough synthesis of evidence available regarding oral health care for older people has yet to be undertaken. Furthermore, it appears that there is limited among older populations knowledge and understanding of oral health care for older people residing in LMICs [29].
Objectives
This scoping review was undertaken to identify and synthesise the existing evidence on the following aspects:
-
oral health policies, strategies and guidelines discussing about promoting oral health in older people, and
-
interventions/programs that have been implemented to improve oral health of older people.
Methods
This review was conducted using a scoping review framework first outlined by Arksey and O’Malley [30] and later revised [31, 32]; and findings are reported in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) checklist [33]. The application of a scoping review format aids in identifying available peer-reviewed and grey literature in this area and to identify gaps in the pertinent evidence base [30]. The scoping design further allows for an iterative process that will facilitate a more comprehensive review of the literature compared to applying a priori fixed criteria [30]. As scoping reviews aim to map existing evidence on the topic and not produce critically appraised and synthesised results, it is not essential to undertake quality assessment of included studies [30]. Finally, a scoping review provides a basis for assessment of the relevance and feasibility of subsequently conducting a systematic review, in this case regarding assessment and synthesis of the best evidence to promote oral health of older people in primary health care settings.
Eligibility criteria
Published or unpublished/grey literature available as full text in the English language by the end of April 2022 that addressed at least one of the oral health areas: policies, guidelines, or programs, and interventions for improving oral health of the older people, were eligible for inclusion, with no restrictions regarding study design, settings, or quality.
Information sources
Individually adapted systematic search strategies were designed and conducted among records of published literature in the following six databases: PubMed, CINAHL, EMBASE, Cochrane Database of Systematic Reviews, Scopus, and ProQuest. Individual search strategies were developed for each database in consultation with an experienced information specialist (a. k. a. librarian). Grey literature was searched using Google Scholar and ProQuest Dissertation and Thesis and also through webpages of relevant organisations and agencies, such as the WHO NCD Documents Repository (https://extranet.who.int/ncdccs/documents/Db) and International Association of Gerontology & Geriatrics (IAGG) (https://www.iagg.net/). In addition, the reference lists in relevant papers were reviewed manually to identify additional publications on the topic.
Search strategy
The search strategies included use of combination of keywords/free text terms and Medical Subject Headings (MeSH) using Boolean operators. Use of diverse terminology and the spelling of keywords were considered to aid in the identification of relevant literature using truncations and wildcards. As per the focus of the scoping questions, the following keywords were used in the search under the following PICO (population, intervention, context/comparison/control, and outcomes) terms [34].
Population
Aging, OR aging population OR aged OR elder OR older OR geriatric OR aged care OR residential care OR nursing home OR care home.
Intervention
Policies OR strategies OR guidelines OR practice guidelines OR intervention OR trial OR health promotion OR health program OR preventive services OR management services OR recommendation OR consensus OR resolution.
Context/comparison/control
N/A.
Outcomes
Oral hygiene OR oral health OR tooth brushing OR interdental cleaning OR flossing OR dental visit OR dental check-up OR nutritional intake OR nutritional status OR malnutrition OR nutritional assessment OR quality of life OR QoL OR oral health related quality of life OR OHRQL OR mastication OR chewing ability OR oral function OR swallowing ability OR diadochokinesis OR oral frailty OR cognitive status OR frailty.
Selection process
After removal of duplicates, the titles and abstracts were screened for fulfillment of the inclusion/exclusion criteria. The full texts of potentially eligible scientific reports were retrieved and independently reviewed by two authors (GP, RA) for inclusion. Further, national policies, guidelines, and strategies from any country or geographic region focusing on oral health aspects of older persons were reviewed for their relevance to the aim of the study. Any discrepancies between reviewers during the screening process was resolved through discussion and consensus with other authors (PP, LBR). Similarly, the full texts of the articles were reviewed (GP, RA), and were discussed with the other authors (PP, LBR).
All literature and policy documents relating to at least one of the focus areas were included in the review.
Data collection process
Data on key information relating to the stated aims were extracted, including author name, publication year, country, study focus/aim, study design, intervention, study setting, sample characteristics and size, key findings, conclusions, and recommendations. Data were collated, summarised, and narratively reported, using synthesizing text and presented in table form by two authors (RA & GP) under the guidance of (PP and LBR). The methodologic quality of the studies were not assessed, as the focus of this scoping review was to synthesise and present the current evidence on this emerging topic, regardless of study design and quality, which would be assessed in a future systematic review, if warranted.
Data items (outcomes)
The data items/outcomes relating to policy included: access to oral health care services and education (training) in oral health care of older population. In the published studies, the outcomes included interventions implemented in improving oral health problems or oral health status at a) nursing homes/RACFs/long-term care settings b) hospitals/clinics/other health facilities, and c) community-based settings.
Results
The results of this scoping review are presented in the following two focus areas: (A) Evidence from policy documents and guidelines/strategies regarding oral health for the older population; and (B) Evidence from the scientific literature concerning preventive and therapeutic interventions relevant to the oral health of the older population.
A) Selection of policy documents and guidelines/strategies regarding oral health for the older population
A total of 104 records of policy documents from 71 countries were retrieved through the WHO data repository [35]. Of these, 66 were excluded due to publication language other than English (n = 60) or unavailability of the full text (n = 6). Of the remaining 38 documents, 17 specified oral health aspects of the older population [36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52]. The majority (n = 9) of the policies were from HICs, including Canada (n = 2), Ireland (n = 1), Australia (n = 1), Japan (n = 1), Barbados (n = 1), Cook Islands (n = 1), New Zealand (n = 1), and Trinidad and Tobago (n = 1) [36, 37, 40, 41, 43, 46, 47, 50, 52].
The findings from the review of the 17 included policy documents are presented under the following two broad topics, namely access to oral health care services and provision of oral health training (Table 1).
Access to oral health care services
Irelands’ National Oral Health Policy discusses the need to ensure access to appropriate health care professionals to supplement primary oral health care services for more vulnerable populations, including older people [37]. The policy specifically depicts the development of models of care specific to the older populations ages 65–69 and > 70 years [37]. Australia’s National Oral Health Plan 2015–2024 [2015] emphasized that all older adults should be able to receive an oral health check-up and preventative oral health care at least every 2 years [47]. The plan also stipulates that the oral health risk assessment should be included as a component of the general health assessment. Furthermore, it highlights that an oral health care plan must be developed and implemented in conjunction with a dental practitioner for those entering aged care facilities [47].
New Zealand’s Strategic Vision for Oral Health [2006] aims to develop oral health policy for older adults [41]. This initiative is intended to aid in providing oral health services for older adults by focusing on building the oral health workforce, such as community based general dentists. Furthermore, it highlights a need to develop group specific strategies to promote the oral health of older adults, such as, to independent older adults, moderately dependent older adults, and highly dependent older adults [41]. Japan’s Oral Health Act [2011] emphasized ensuring preventive as well as t oral health services for the older population [52]. Jamaica’s Oral Health Policies & Business Plan for the Repositioning of Oral Health Services [2017] highlighted that older people should have access to high quality oral health care at an affordable cost [49]. It also highlighted the importance of maintaining good oral health, which correlates with general health, for improved quality of life. Furthermore, the policy emphasizes the importance of oral disease prevention programs, such as dental prophylaxis (cleaning) to prevent gum disease, as well as application of fluoride varnish and dental sealants to prevent caries. The Cook Island’s National Oral Health Strategy (2014–2018) focused on providing rehabilitative oral care services to older people, restoring their oral functions and improving the oral health as well as overall health [36].
Similarly, this review identified policies from different countries, namely, Canada [46], Trinidad and Tobago [43], Nigeria [45], Vanuatu [38], Malaysia [44], Timor-Leste [39], and Rwanda [48] that shared a common goal of improving access to quality, affordable, timely, preventative, and effective oral health services. The Uganda’s National Oral Health Policy (2007) lacked in providing information regarding the definitive aspects of older population’s oral health care [42].
Provision of oral health training
Oral health policy documents from some countries, namely Jamaica [49], Barbados [50], Grenada [51] and Canada [46] stated the need to foster public and/or health care professionals’ awareness regarding the importance of oral health care. These policies also highlighted the relationship of oral health with overall well-being among the older population [40, 49,50,51]. The Canadian Oral Health Strategy (2005) stated the needs for educating oral health practitioners regarding oral health care as well as focusing on follow-up of the cases of dental neglect and studying the barriers to oral health care of older populations can improve the target population’s accessibility to oral health services [40]. Furthermore, the policy mentioned that this can in turn facilitate the aim of this initiative to improve the overall oral health of Canadians by identifying inequalities in the system, disparities in health, and barriers to achieving optimal oral health [40]. Barbados’ Oral health policy (2009) stated the needs for improving the oral health of Barbadians by minimising the rate of oral health problems and unmet oral health needs through public education for all age groups, including the older population, and early detection and treatment/prevention of oral health diseases, such as oral cancer [50]. Likewise, Grenada’s Oral Health Policy (2014) described the promotion for older age groups [51]. It also mentioned that launching special oral health care education for older people and their caregiver/family is essential to preventing adverse effects of aging on oral health of older population. Similarly, Jamaica’s oral health policies mentioned that oral health education programmes need to be launched to promote older population’s oral health [49].
B) Selection of scientific published literature relating to preventive and therapeutic interventions to ensure good oral health in the older population
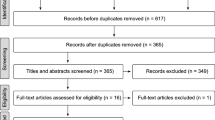
The systematic bibliographic database searches retrieved a total of 2776 records. After excluding 752 duplicates and another 1912 records due to ineligibility upon screening of the title and abstract, 112 records remained for full-text review. Thirteen citations were further excluded because the full text versions could not be readily accessed. Of the 99 full-texts, 62 met the inclusion criteria and were included in this scoping review (Fig. 1).
Study selection process (PRISMA-ScR) [33]
Study characteristics
Study design
The characteristics of the 62 studies included in this review are presented in Table 1. The most common study design was interventional study (n = 57) followed by observational study (n = 4) and a comparative/review study (n = 1).
Geographical location
The majority of the included studies were conducted in HICs (n = 56), namely, the United States of America (n = 8), Australia (n = 7), Japan (n = 7), South Korea (n = 6), United Kingdom (n = 4), Canada (n = 3), Germany (n = 3), Netherlands (n = 2), Hong Kong (n = 2), Taiwan (n = 2), and others. Only six studies were from LMICs, namely India, Indonesia, Colombia, Iran, Brazil, and Thailand.
Study settings and number of participants
The majority of the studies were conducted in aged care facilities/ nursing homes/ long-term care institutions (n = 33/62), followed by community settings (n = 19/62) and hospitals/ clinics/ health care facilities (n = 6). In addition, two studies included nationwide samples, one aimed to assess change in dental service use after implementing the national health insurance covering dental services to older population whereas the other study assessed the usefulness of practical oral care video among the video purchasers. Moreover, a study was conducted among the service providers from long-term and community-licensed healthcare professionals. Furthermore, a qualitative study was conducted among the state level dental professionals or representatives. The sample size in the included studies varied widely, ranging between 12 and 17,264 (Table 2).
Types of intervention/program
The majority of studies included interventions for prevention and management of oral health conditions among older populations. A wide range of oral care interventions/programs were adopted and the target groups included both the older people (and family members) and care providers. The most common intervention (n = 24) was to raise awareness on oral health through courses, trainings or educational sessions and distribution of Information Education and Communication (IEC). The educational intervention was provided using a wide range of methods, such as, face to face interview, group sessions, practical oral care videos and text messages via phone, and smartphone applications. Similarly, some studies (n = 6) also involved practical sessions and demonstrations, along with the educational session. Two studies (n = 2) applied motivational interviewing techniques to educate on oral health and assess the treatment fidelity of motivational interviewing. Furthermore, three studies (n = 3) adopted mobile phone-based text messages and two studies (n = 2) involved web-based online oral health education and promotion programs to improve knowledge, attitudes, and self-care practices aimed at attaining and maintaining oral hygiene and health.
Several studies also involved interventions to improve oral health status, such as improving salivary flow and oral wetness. The interventions used in these studies included application of silver diamine fluoride (n = 2), toothbrushing with fluoride toothpaste (n = 6), fluoride varnish (n = 2), chlorhexidine rinsing(n = 6), ultrasonic devices for denture cleaning (n = 1), and lip muscles trainer device and sonic toothbrush (n = 1).
In addition, a qualitative study among dental professionals explored understanding of the ongoing oral health programs for older adults. Similarly, one retrospective study assessed the effectiveness of 5-year clinical and radiologic performance of fixed implant-supported prostheses placed in edentulous older people.
Involvement of dental professionals
The most common dental professionals providing intervention were dental/oral hygienists (n = 17), followed by dentists (n = 8), both hygienists and dentists (n = 4), oral health therapists (n = 2), dental nurse (n = 1), and dental students (n = 1). Five studies used a combination of dental and non-dental professionals, namely nurses, physicians, dieticians, pathologists, and pharmacists, whereas one study involved community health workers providing the oral health intervention. Information regarding who provided the interventions was not clearly reported in 24 studies.
Results from published literature
The results of the studies (Table 3) are reported as per the study settings.
Nursing homes/RACFs/long-term care settings
The major interventions conducted in the nursing home, RACFs, or long-term care setting were oral health education and promotion programs for the older residents that included hands-on guidance and support in oral care [87], toothbrushing [64, 85], oral hygiene and denture care [72, 77, 82], and oral functional exercises [75]. Such interventions reported significant reduction in plaque and gingival index and improved oral health related quality of life of these older residents.
Two studies focused on interventions for the caretakers of older residents that included educational sessions and demonstrations on oral hygiene and denture care [92, 98]. Such intervention reduced the plaque and gingival indexes in the older residents and improved knowledge and attitudes on oral health among their caretakers.
Four studies enrolled both the older residents and staff consisting of care givers and nurses [63, 78, 79, 87]. Interventions included instruction on oral health care and daily oral hygiene routines [87], training on oral assessments and saliva testing [78], installation of an oral hygiene trolley, protocol for oral hygiene, and provision of education [63] and educational sessions and training on oral care [79]. The results were improved oral health status of the older residents and enhanced oral health competencies of the nurses and caregivers [82].
Seven studies involved clinical interventions among older adults through mobilizing their care givers and nursing staff. The interventions included tongue cleaning and wiping the oral mucosa with a sponge soaked in chlorhexidine [64]; professional oral health care programs involving dentists and dental hygienists regularly monitoring and managing the oral health of older residents [70, 115]; application of chlorhexidine varnish [58, 61, 62], and fluoride [106]. The results of such interventions were significant declines in plaque and gingival indexes, reduced opportunistic infections, and prevention of incident root caries in these older residents.
Hospitals/clinics/other health facilities
Of six studies, four studies included only older people attending for care, with the remaining two studies also included other age groups. A wide range of oral health interventions were used in these studies, including face-to-face motivational interview sessions on oral health [94, 95], application of a lip muscle trainer device and sonic toothbrush [93], electric toothbrush and interdental brushes [59], and text messages on tooth brushing, flossing, fluoride use, and denture cleaning [109]. These interventions resulted in improved oral health outcomes, such as improvement in the salivary flow rate, oral wetness, and denture and oral hygiene.
A retrospective review of fixed implant-supported prostheses comparing the clinical performances among edentulous older patients and younger patients reported the clinical performances were similar between the groups [56]. However, cleaning problems; mucositis; and tongue, lip, and cheek biting were more common among the older compared to younger patients. A qualitative study was conducted with state level dental professionals, managers, or representatives [110] The study reported that the majority of oral health programs were focused on institutionalized patients and their caregivers; and that oral healthcare needs of older adults have been realized and can be best addressed by coordinating or lobbying with local advocacy groups.
Community-based settings
The interventions in community-based settings were mostly directed to independent older adults without physical limitations. The interventions on this setting were largely focused on organizing seminars, education, and demonstration sessions on oral health and hygiene [53, 57, 68, 76, 80, 89]; instruction in interdental flossing, and tooth brushing [65, 81, 90, 104]; denture and oral mucosa cleaning [80]; application of fluoride [73], silver diamine fluoride [68], and fluoride dentifrice [91]; and videos on tooth brushing and denture care methods [102]. In addition, oral function promotion programmes, including knowledge on oral health and encouragement of facial muscle and tongue exercises and salivary gland massage, were conducted [60, 74, 96]. Such interventions improved swallowing; reduced plaque index scores, gingival inflammation, oral malodour and oral dryness; and prevented root caries. Moreover, knowledge level and attitude and self-care behaviours regarding oral health also improved among these older adults.
A study from The Netherlands evaluated the public project “Don’t forget the mouth!” (DFTM project) involving healthcare providers from general medical practices, general dental practices, and home care organizations [101]. The health care providers participating in the DFTM project were provided with theoretical and practical sessions on oral health being associated with general health; oral health status of frail older adults; familiarization with oral health screening and referral tools. This study found that the DFTM project was effective in increasing the oral health awareness among the health care providers and hence in improving the oral health of the frail older adults. Nonetheless, several barriers exist with large-scale implementation, such as poor physical access to and lack of sufficient numbers of oral care providers and financial considerations [101].
Discussion
The health burden and disease conditions in the older populations are likely to increase significantly with poor oral health status, if no appropriate actions are taken [1, 2, 11]. Efforts to save teeth and maintain good oral health, therefore, are crucial in geriatric populations. In this context, this scoping review explored (“scoped”) the existing evidence regarding oral health care for older population, namely policies/guidelines and interventions.
Polices and strategies to promote oral health
This study identified only 17 policies specifically mentioned about oral health needs of the elderly. These polices primarily focused on access to oral health care services for older populations, as well as educating health professionals on the importance of oral health care and the relationship of oral health with overall health among the older population. Oral health policies that mentioned and prioritised oral health care for older people were from mainly from high income countries (HICs). Few policies, namely from Ireland [37], New Zealand [41] and Australia [47] and recognised the older population as a “vulnerable” group and highlighted their need for specific care models that could assist in accessing and navigating oral health care services. Furthermore, a need to include oral health risk assessment for all older people and development of an oral health care plan for those entering care facilities were also emphasized in these polices [47] [41]. It was emphasised that developing similar plans can potentially result in positive outcomes in relation to oral health status of older people [41]. The policies also emphasised the need for regular dental visits, oral prophylaxis (dental cleaning), and fluoride application in improving and maintaining good oral health of older populations [49]. These are considered important preventive measures to decrease the incidence of dental decay and periodontitis to prevent loss of teeth among older people [116].
Since access to dental care is often challenging for geriatric populations, particularly the institutionalised, there is an urgent need to develop policies and strategies that include measures to facilitate regular dental check-ups for this vulnerable group. In the absence of policies, it is challenging to address social determinants of oral health inequalities [117]. As such, clinicians may face difficulties in making decisions in the absence of clear guidelines [118], and prioritise integration of oral health care as a needed part of healthy ageing. This is reflected in the findings of the WHO survey (2017–2018) which showed that only 20% of the 101 countries surveyed, reported having programmes for oral health of older people, and this was even found less in low-income countries (4.8%) [119]. Overall, it is evident that there is currently limited focus and support for oral health of older people at the government level [119], which highlights the responsibility of the countries to formulate geriatric oral health polices and guidelines for prevention and management of oral diseases in older people.
In 2021, the 74th World Health Assembly (WHA74) approved the WHO resolution on oral health [120], recognising the global burden of oral diseases and their associations with systemic conditions, and urged all countries to address shared risk factors, enhance the professional capacity of oral health professionals, and include oral health in universal health coverage (UHC) benefit packages. The Global Strategy on Oral Health pointed out that the negative impact of oral health problems accumulate over time and have complex consequences in later life, particularly in relation to other NCDs [121] and the need of locally tailored and age-appropriate oral health strategies integrated within relevant health programmes across the life course [121]. This is even more important in the context of low income countries, since oral health may not be a priority for people in these regions due to other health priorities, so dental problems are often left untreated [119]. Furthermore, it is also reported that there is less emphasis on primary prevention of oral diseases and limited access to oral health care in developing countries [119]. Thus, these aspects need to be taken into consideration while developing geriatric-specific oral health care policies and strategies.
Preventive measures to improve oral health
The studies included in this review used a range of interventions in promoting oral health among geriatric populations. They included educational sessions and demonstrations to older adults and their caregivers on oral hygiene and denture care [72, 77, 82] and tooth brushing [64]. Some studies also used one-to-one and face-to-face motivational interview sessions on oral health [94, 95]. Such programs were reported to improve awareness about the importance of oral health and oral/denture hygiene of older populations, resulting in a decrease in plaque and gingival index scores [80], and ultimately improving oral health related quality of life [75, 81, 94, 95]. Since the compliance with the recommended annual dental check-ups and good home oral hygiene behaviours (brushing twice and floss/clean dentures daily) is reported to be lower among older residents [122], increasing awareness about the importance of oral health and oral health problems and their association with systemic diseases could be an effective strategy to improve compliance with the recommended preventive behaviours. Studies report that people who are better informed about the risks and consequences of poor oral health are more likely to engage in positive health behaviours [123]. Therefore, health care providers should be motivated to play a proactive role to provide oral health education and motivation to the older patients to perform self-care oral hygiene, as these are effective to reduce the risks of oral diseases [124, 125].
The studies included in this review also reported a range of preventative and therapeutic measures that oral health care professionals employed to improve oral health outcomes of older population. These included tongue cleaning with a sponge [64], wiping oral mucous with a sponge brush soaked in chlorohexidine [64], application of chlorhexidine varnish [58, 61, 62], fluoride (toothpaste and or varnish) [73, 106], fluoride varnish [62], fluoride dentifrice (5000 ppm) [91], silver diamine fluoride [68], and xylitol or chlorhexidine [73], facial muscle and tongue exercise and salivary gland massages [60] including use of lip trainer device to perform facial mimetic muscle training [74, 93, 96], and scaling and cleaning the teeth’s crown and root surfaces [73].
It is widely known that decreased salivary flow (hyposalivation) is commonly found in older persons due to general pathologies and especially to the medications taken, which leads to difficulties in swallowing (dysphagia) and chewing (mastication) [3,4,5]. Furthermore, hyposalivation can lead to greater incidence of coronal and root caries and periodontitis [6, 7], dental diseases that are very prevalent in older populations [8, 9]. The studies included in this review reported interventions, such as exercise of facial muscle and tongue to be effective in improving salivary flow rate [60, 74, 93, 96]. A recent meta-analysis (n = 18 studies) explored the effectiveness of oral exercise in improving the masticatory function among people ages 18 years and older and reported that resistance exercises, such as chewing or clenching, were the most beneficial exercises to improve the bite force, while simple oral exercises was not found to have any significant effect [126]. The Japanese study included in this review used a lip trainer device for muscle training and found this to be effective in improving salivary flow and dry mouth [93]. However, it is also important to consider that mastication is a complicated process involving the movements of lips, jaw, tongue, cheek, soft palate and masticatory muscles, therefore, it may require more efforts than just the oral exercise for improvement [126].
The studies included in this review reported the benefits of application of antimicrobial agents or varnishes, such as fluoride, sliver diamine fluoride, chlorhexidine varnish, or fluoride and chlorhexidine combined, in the prevention of root caries. However, results regarding effectiveness of application of different antimicrobial agents reported in various RCTs/systematic reviews are inconsistent. A systematic review (n = 6 studies) looking at the effect of chlorhexidine varnish found little or no additional effect to professional cleaning and good home oral hygiene. Nonetheless, the meta-analysis of only three studies showed benefit for high-risk patients, such as the elderly with dry mouth [127]. Similarly, results from a systematic review of RCTs (n = 3) supports the effectiveness of sliver diamine fluoride in prevention of root caries in older population [128].
The studies also included interventions involving non-dental care professionals, mostly nurses and public health professionals, and included education, training or meetings [63, 82, 97, 101], daily use of checklist for oral care [92], observation delivery of integrated oral health program [114], and development of an oral health protocol [63] to facilitate integration of oral health, such as education, oral assessments and referrals. These interventions were found to improve oral health care related knowledge and attitudes, and competencies [63, 82, 97, 101, 114], as nurses were positive about accepting oral hygiene into their daily routine care [63], This is consistent with the results reported in systematic reviews [129, 130]. Such practices, as reported in the Australian study, also resulted in improving oral health outcomes among older people, including reductions in plaque scores, gingivitis, and pocket depths [63].
Our study did not find any studies involving only dental care professionals. It is commonly reported that there is a gap in the knowledge and confidence among oral health care professionals (OHCP) regarding provision of oral care for old people [131], as older people are often vulnerable due to the weakening physical ability and cognition, and comorbidities. Furthermore, a systematic review reported lack of adequate equipment and space for oral treatment in care homes, as well as education and guidelines to manage oral health problems as commonly reported barriers among OHCPs [132]. These are perceived barriers for non-dental care professionals as well [133]. This warrants a need for education, training, and hands-on sessions for OHCPs as dental care needs and problems in geriatric population are often complex [134]. Providing this education and practice in undergraduate courses across disciplines is desirable to improve the oral health knowledge and competency of new graduates. Furthermore, providing dental treatment for people with impaired cognitive function make geriatric dental care even more challenging [134]. All these complexities together demand a shift in the oral health care model, as there is a need for multidisciplinary approach of oral health promotion in older people that involves nurses and other health professionals, such as GPs and dietitians, and the integration of oral health into overall health management of older people. As evidenced in several studies, nurses can provide support to dentists and can also independently play a proactive role in promoting goof oral health among older people in RACF, provided that they are supported with education and resources [28].
Overall, the findings of this review suggest that there is lack of policies and guidelines regarding oral health care for older people. A wide range of interventions are used to promote oral health care of older populations, however, there is a lack of information and research regarding the most effective treatments and evidenced-based guidelines for providing oral health care to older people.
Implication of the findings
The results of this review have several implications for policy makers, geriatric care providers and oral health care professionals. The national oral health policies should focus and priorities to address oral health needs and care of geriatric population and prioritise to develop guidelines relating to oral health care of older people. Geriatric care providers could play a more active role in promoting oral health among their patients, such as in educating patients about their increased risk for oral health complications and advise them for regular dental visits. Oral health care professionals also should look for opportunities to train them to address oral health concerns of older people. Specific guidelines need to be developed to assist both, oral health care professionals and geriatric care providers in promoting oral health care in older people.
Limitation
The scoping review undertaken has few limitations. The review did not look for policies published in other than English languages and as well as for unpublished articles in the interventions/programs and hence there is a possibility that this review may not have retrieved all policies/studies in this area. Similarly, there is a possibility that the search may have missed to capture articles due to the search in particular databases (six) and the search strategies. Lastly, although quality assessments of the studies were not undertaken, this additional information may have useful for synthesising the evidence.
Conclusion
The findings of this review suggest that educating patients about oral health problems and the importance of oral health can significantly improve oral hygiene behaviours of older patients. Similarly, the common preventive measure such as application of fluoride may decrease the incidence of caries also among older people. However, there is currently a gap in information and research around effective oral health care treatments and programs in geriatric dental care and how this can be integrated into overall health management. Due to the lack of policies and guidelines, there is uncertainty regarding how oral health care can be integrated into geriatric medical care. Therefore, further research is warranted to assess the effectiveness of interventions in improving the oral health status in the elderly, and based on such evidence, efforts must be invested in developing guidelines to assist both dental and medical health care professionals in integrating good oral health as part of healthy ageing. There is no overall health without oral health.
Availability of data and materials
The data supporting the conclusion of this article is included within the article.
References
United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2019 (ST/ESA/SER.A/444). 2020. Available from https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Report.pdf. [cited: 25 October 2021]
World Health Organization. Ageing and Health: Key facts: WHO; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. [Cited: 25 October 2021].
Joshy G, Arora M, Korda RJ, Chalmers J, Banks E. Is poor oral health a risk marker for incident cardiovascular disease hospitalisation and all-cause mortality? Findings from 172 630 participants from the prospective 45 and up study. BMJ Open. 2016;6(8):e012386.
Tonetti MS, Bottenberg P, Conrads G, Eickholz P, Heasman P, Huysmans M-C, et al. Dental caries and periodontal diseases in the ageing population: call to action to protect and enhance oral health and well-being as an essential component of healthy ageing – consensus report of group 4 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol. 2017;44(S18):S135–44.
Beard JR, Officer A, de Carvalho IA, Sadana R, Pot AM, Michel J-P, et al. The world report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145–54.
Lu T-Y, Chen J-H, Du J-K, Lin Y-C, Ho P-S, Lee C-H, et al. Dysphagia and masticatory performance as a mediator of the xerostomia to quality of life relation in the older population. BMC Geriatr. 2020;20(1):1–11.
Hung M, Moffat R, Gill G, Lauren E, Ruiz-Negrón B, Rosales MN, et al. Oral health as a gateway to overall health and well-being: surveillance of the geriatric population in the United States. Special Care Dentist. 2019;39(4):354–61.
Scannapieco FA, Cantos A. Oral inflammation and infection, and chronic medical diseases: implications for the elderly. Periodontol. 2000;72(1):153–75.
Van Lancker A, Verhaeghe S, Van Hecke A, Vanderwee K, Goossens J, Beeckman D. The association between malnutrition and oral health status in elderly in long-term care facilities: a systematic review. Int J Nurs Stud. 2012;49(12):1568–81.
Cheng F, Zhang M, Wang Q, Xu H, Dong X, Gao Z, et al. Tooth loss and risk of cardiovascular disease and stroke: a dose-response meta analysis of prospective cohort studies. PLoS One. 2018;13(3):e0194563.
Gil-Montoya JA, de Mello ALF, Barrios R, Gonzalez-Moles MA, Bravo M. Oral health in the elderly patient and its impact on general well-being: a nonsystematic review. Clin Interv Aging. 2015;10:461–7.
Simpson TC, Weldon JC, Worthington HV, Needleman I, Wild SH, Moles DR, et al. Iheozor-Ejiofor Z: treatment of periodontal disease for glycaemic control in people with diabetes mellitus. Cochrane Database Syst Rev. 2015;2015(11)):Cd004714.
Borgnakke WS, Poudel P. Diabetes and Oral health: summary of current scientific evidence for why transdisciplinary collaboration is needed. Front Dental Med. 2021;2(50).
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990;#x2013;2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
World Health Organization. Non-communicable Diseases (NCDs) Key Facts 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases. [Cited: 25 October 2021]
Griffin SO, Jones JA, Brunson D, Griffin PM, Bailey WD. Burden of oral disease among older adults and implications for public health priorities. Am J Public Health. 2012;102(3):411–8.
Gibney JM, Naganathan V, Lim M. Oral health is essential to the well-being of older people. Am J Geriatr Psychiatry. 2021;29(10):1053–7.
Tanaka T, Takahashi K, Hirano H, Kikutani T, Watanabe Y, Ohara Y, et al. Oral frailty as a risk factor for physical frailty and mortality in community-dwelling elderly. J Gerontol A Biol Sci Med Sci. 2018;73(12):1661–7.
Razak PA, Richard KMJ, Thankachan RP, Hafiz KAA, Kumar KN, Sameer KM. Geriatric oral health: a review article. J Int Oral Health. 2014;6(6):110–6.
Azzolino D, Passarelli PC, De Angelis P, Piccirillo GB, D’Addona A, Cesari M. Poor Oral health as a determinant of malnutrition and Sarcopenia. Nutrients. 2019;11(12).
Huang DL, Chan KC. Young BA: poor oral health and quality of life in older U.S. adults with diabetes mellitus. J Am Geriatr Soc. 2013;61(10):1782–8.
Dibello V, Zupo R, Sardone R, Lozupone M, Castellana F, Dibello A, et al. Oral frailty and its determinants in older age: a systematic review. Lancet Healthy Longevity. 2021;2(8):e507–20.
Gamage MWK, Hewage C, Pathirana KD. Effect of cognitive and executive functions on perception of quality of life of cognitively normal elderly people dwelling in residential aged care facilities in Sri Lanka. BMC Geriatr. 2018;18(1):256.
Ćwirlej-Sozańska AB, Sozański B, Wiśniowska-Szurlej A, Wilmowska-Pietruszyńska A. Quality of life and related factors among older people living in rural areas in South-Eastern Poland. Ann Agric Environ Med. 2018;25(3):539–45.
Niesten D, van Mourik K, van der Sanden W. The impact of having natural teeth on the QoL of frail dentulous older people A qualitative study. BMC Pub Health. 2012;12:839.
Starr JM, Hall R. Predictors and correlates of edentulism in healthy older people. Curr Opin Clin Nutr Metab Care. 2010;13(1):19–23.
Brondani M, Ardenghi D, Mariño RJ. Dental specialties: how to choose yours. Career Paths in Oral Health. Cham: Springer International Publishing; 2018. p. 79–92.
Poudel P, Griffiths R, Wong VW, Arora A, George A. Knowledge and practices of diabetes care providers in oral health care and their potential role in oral health promotion: a scoping review. Diabetes Res Clin Pract. 2017;130:266–77.
León S, De Marchi RJ, Tôrres LH, Hugo FN, Espinoza I, Giacaman RA. Oral health of the Latin American elders: what we know and what we should do-position paper of the Latin American Oral geriatric Group of the International Association for dental research. Gerodontol. 2018;35(2):71–7.
Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371–85.
Daudt HM, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13(1):1–9.
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Richardson WS, Wilson MC, Nishikawa J, Hayward RS. The well-built clinical question: a key to evidence-based decisions. ACP J Club. 1995;123(3):A12–3.
World Health Organisation. Noncommunicable Disease Document Repository 2022. Available from: https://extranet.who.int/ncdccs/documents/Db. [Cited: 28 July 2022].
Ministry of Health Dental Services. The Cook Islands National Oral Health Strategy 2014–2018 The Cook Islands2019. Available from: https://extranet.who.int/ncdccs/Data/cok_B8_Cook-Islands-National-Oral-Health-Strategy-2014-2018.pdf. [Cited: 29 June 2022].
Department of Health. National Oral Health Policy Ireland2019. Available from: https://extranet.who.int/ncdccs/Data/IRL_B8_20190425%20National-Oral_Health_Policy_SmileAgusSlainte.pdf. [Cited: 29 June 2022].
Ministry of Health. National Oral Health Policy 2019–2023: Government of Vanuatu 2019. Available from: https://extranet.who.int/ncdccs/Data/VUT_B8_Document%20VNOHP2.pdf. [Cited: 29 June 2022].
Ministry of Health. National Strategy for Oral Health And National Oral Health Action Plan 2015–2020: Timor-Leste Available from: https://extranet.who.int/ncdccs/Data/TLS_B8_Timor-Leste%20Strategic%20Plan%20for%20Oral%20Health%202015-2020%20final%20draft.pdf. [Cited: 29 June 2022].
Canadian Association of Public Health Dentistry. Federal, Provincial and Territorial Dental directors. A Canadian Oral Health Strategy 2005. Available from: https://www.caphd.ca/sites/default/files/Canadian%20Oral%20Health%20Strategy%20-%20Final.pdf. [Cited: 29 June 2022].
Ministry of Health. Good Oral Health for All, for Life: The Strategic Vision for Oral Health in New Zealand Wellington: Ministry of Health2006. Available from: https://extranet.who.int/ncdccs/Data/NZL_B8_good-oral-health-strategic-vision-2006.pdf. [Cited: 29 June 2022].
Ministry of Health. National Oral Health Policy: The Republic of Uganda; 2007. Available from: https://extranet.who.int/ncdccs/Data/UGA_B8_National%20Oral%20Health%20Policy.pdf. [Cited: 29 June 2022].
Ministry of Health. The Oral Health Policy: Trinidad and Tobago; 2010. Available from: https://extranet.who.int/ncdccs/Data/TTO_B8_Oral%20Health%20Policy%20TTO%20-%20Final%20%20(1).pdf. [Cited: 29 June 2022].
Ministry of Health. National Oral Health Plan for Malaysia 2011–2020: ; 2011. Available from: https://extranet.who.int/ncdccs/Data/MYS_B8_nohp20112020.pdf. [Cited: 29 June 2022].
Federal Ministry of Health. National Oral Health Policy Nigeria2012. Available from: https://extranet.who.int/ncdccs/Data/NGA_B8_ORALHEALTHPOLICY.pdf. [Cited: 29 June 2022].
The Government of Quebec. A Canadian Oral Health Framework: 2013–2018 2013. Available from: https://extranet.who.int/ncdccs/Data/CAN_B8_Canadian%20Oral%20Health%20Framework.pdf. [Cited: 29 June 2022].
Government of Australia. Healthy Mouths, Healthy Lives. Australia's National Oral Health Plan 2015–2024 2015. Available from: https://extranet.who.int/ncdccs/Data/AUS_B8_Australia's%20National%20Oral%20Health%20Plan%202015-2024_uploaded%20170216%20(1).pdf. [Cited: 29 June 2022].
Ministry of Health. National Oral Health Strategic Plan 2019–2024: Republic of Rwanda 2019. Available from: https://extranet.who.int/ncdccs/Data/RWA_B8_s21_National_Oral_Health_Strategic_Plan_2019-2024.pdf. [Cited: 29 June 2022].
McKenzie IF. Oral Health Policies & Business Plan for the Repositioning of Oral Health Services 2017. Available from: https://extranet.who.int/ncdccs/documents/db. [Cited: 29 June 2022].
Thompson FV. Oral Health Policy for Barbados Barbados: Ministry of Health & Pan American Health Organization/World Health Organization (PAHO/WHO). 2009. Available from: https://extranet.who.int/ncdccs/Data/BRB_B8_Oral%20Health%20Policy%20for%20Barbados%202009.pdf. [Cited: 29 June 2022]
Vincent H. Oral Health Policy for Grenada Grenada: Ministry of Health & Pan American Health Organization/World Health Organization (PAHO/WHO). 2014. Available from: https://extranet.who.int/ncdccs/Data/GRD_B8_2014%20ORAL%20HEALTH%20POLICY%20FOR%20GRENADA%20-%20APPROVED-%20HVINCENT.pdf. [Cited: 29 June 2022]
Government of Japan. Act on the Promotion of Oral Health 2011. Available from: https://extranet.who.int/ncdccs/documents/Db. [Cited: 29 June 2022].
Little SJ, Hollis JF, Stevens VJ, Mount K, Mullooly JP, Johnson BD. Effective group behavioral intervention for older periodontal patients. J Periodontal Res. 1997;32(3):315–25.
Mojon P, Rentsch A, Budtz-Jørgensen E, Baehni PC. Effects of an oral health program on selected clinical parameters and salivary bacteria in a long-term care facility. Eur J Oral Sci. 1998;106(4):827–34.
Simons D, Brailsford S, Kidd EA, Beighton D. The effect of chlorhexidine acetate/xylitol chewing gum on the plaque and gingival indices of elderly occupants in residential homes. J Clin Periodontol. 2001;28(11):1010–5.
Engfors I, Örtorp A, Jemt T. Fixed implant-supported prostheses in elderly patients: a 5-year retrospective study of 133 edentulous patients older than 79 years. Clin Implant Dent Relat Res. 2004;6(4):190–8.
Mariño R, Calache H, Wright C, Schofield M, Minichiello V. Oral health promotion programme for older migrant adults. Gerodontol. 2004;21(4):216–25.
Wyatt CC, MacEntee MI. Caries management for institutionalized elders using fluoride and chlorhexidine mouthrinses. Commun Dent Oral Epidemiol. 2004;32(5):322–8.
Peltola P, Vehkalahti MM, Simoila R. Effects of 11-month interventions on oral cleanliness among the long-term hospitalised elderly. Gerodontol. 2007;24(1):14–21.
Hakuta C, Mori C, Ueno M, Shinada K, Kawaguchi Y. Evaluation of an oral function promotion programme for the independent elderly in Japan. Gerodontol. 2009;26(4):250–8.
Baca P, Clavero J, Baca AP, González-Rodríguez MP, Bravo M, Valderrama MJ. Effect of chlorhexidine-thymol varnish on root caries in a geriatric population: a randomized double-blind clinical trial. J Dent. 2009;37(9):679–85.
Tan HP, Lo EC, Dyson JE, Luo Y, Corbet EF. A randomized trial on root caries prevention in elders. J Dent Res. 2010;89(10):1086–90.
Blinkhorn F, Weingarten L, Boivin L, Plain J, Kay M. An intervention to improve the oral health of residents in an aged care facility led by nurses. Health Educ J. 2012;71(4):527–35.
Tashiro K, Katoh T, Yoshinari N, Hirai K, Andoh N, Makii K, et al. The short-term effects of various oral care methods in dependent elderly: comparison between toothbrushing, tongue cleaning with sponge brush and wiping on oral mucous membrane by chlorhexidine. Gerodontol. 2012;29(2):e870–82.
Mariño R, Calache H, Morgan M. A community-based culturally competent oral health promotion for migrant older adults living in Melbourne. Austral J Am Geriatr Soc. 2013;61(2):270–5.
van der Putten G-J, Mulder J, de Baat C, De Visschere LM, Vanobbergen JN. Schols JM: effectiveness of supervised implementation of an oral health care guideline in care homes; a single-blinded cluster randomized controlled trial. Clin Oral Investig. 2013;17(4):1143–53.
Zenthöfer A, Dieke R, Dieke A, Wege KC, Rammelsberg P, Hassel AJ. Improving oral hygiene in the long-term care of the elderly--a RCT. Commun Dent Oral Epidemiol. 2013;41(3):261–8.
Zhang W, McGrath C, Lo EC, Li JY. Silver diamine fluoride and education to prevent and arrest root caries among community-dwelling elders. Caries Res. 2013;47(4):284–90.
Bonwell PB, Parsons PL, Best AM, Hise S. An interprofessional educational approach to oral health care in the geriatric population. Gerontol geriat educ. 2014;35(2):182–99.
Morino T, Ookawa K, Haruta N, Hagiwara Y, Seki M. Effects of professional oral health care on elderly: randomized trial. Int J Dent Hyg. 2014;12(4):291–7.
Kammers AC, Zanetti AL, Lacerda TE, Aroca JP, Camilotti V, Mendonça MJ. Toothbrush handles individually adapted for use by elderly patients to reduce biofilm on complete dentures: a pilot study. J Clin Diagn Res. 2015;9(5):Zc94–7.
Khanagar S, Naganandini S, Tuteja JS, Naik S, Satish G, Divya KT. Improving oral hygiene in institutionalised elderly by educating their caretakers in Bangalore city, India: a randomised control trial. Canadian Geriatrics J. 2015;18(3):136–43.
Komulainen K, Ylostalo P, Syrjala AM, Ruoppi P, Knuuttila M, Sulkava R, et al. Oral health intervention among community-dwelling older people: a randomised 2-year intervention study. Gerodontol. 2015;32(1):62–72.
Ohara Y, Yoshida N, Kono Y, Hirano H, Yoshida H, Mataki S, et al. Effectiveness of an oral health educational program on community-dwelling older people with xerostomia. Geriatr Gerontol Int. 2015;15(4):481–9.
Kim YS, Choi HS, Kim YS, Kim GY. Effects on quality of life and oral health of the elderly in an oral health promotion program. Indian. J Sci Technol. 2016;9(20).
Mariño RJ, Marwaha P, Barrow SY. Web-based oral health promotion program for older adults: development and preliminary evaluation. Int J Med Inform. 2016;91:e9–e15.
Avellaneda CPR, Angarita Díaz MDP, Ramírez LFN, Castro LAP, Herrera YTR, Baquero ILR, et al. Oral health strategy for the older people in social protection centers in Villavicencio. Colombia Work Older People. 2017;21(3):167–77.
Deutsch A, Siegel E, Cations M, Wright C, Naganathan V, Brodaty H. A pilot study on the feasibility of training nurses to formulate multicomponent oral health interventions in a residential aged care facility. Gerodontol. 2017;34(4):469–78.
Ildarabadi EH, Armat MR, Motamedosanaye V, Ghanei F. Effect of Oral health care program on Oral health status of elderly people living in nursing homes: a quasi-experimental study. Mater Sociomed. 2017;29(4):263–7.
Nihtilä A, Tuuliainen E, Komulainen K, Autonen-Honkonen K, Nykänen I, Hartikainen S, et al. Preventive oral health intervention among old home care clients. Age Ageing. 2017;46(5):846–51.
Sakashita R, Hamada M, Sato T, Abiko Y, Takami M. Oral health promotion program for fostering self-management of the elderly living in communities. Intell Autom Soft Comp. 2017;23(3):535–41.
Schwindling FS, Krisam J, Hassel AJ, Rammelsberg P, Zenthöfer A. Long-term success of oral health intervention among care-dependent institutionalized seniors: findings from a controlled clinical trial. Commun Dent Oral Epidemiol. 2018;46(2):109–17.
Fjeld KG, Eide H, Mowe M, Sandvik L, Willumsen T. A 1-year follow-up of a randomized clinical trial with focus on manual and electric toothbrushes' effect on dental hygiene in nursing homes. Acta Odontol Scand. 2018;76(4):257–61.
Janssens B, Vanobbergen J, Petrovic M, Jacquet W, Schols JM, De Visschere L. The impact of a preventive and curative oral healthcare program on the prevalence and incidence of oral health problems in nursing home residents. PLoS One. 2018;13(6):e0198910.
Lavigne SE, Doupe MB, Iacopino AM, Mahmud S, Elliott L. The effects of power toothbrushing on periodontal inflammation in a Canadian nursing home population: a randomized controlled trial. Int J Dent Hyg. 2017;15(4):328–34.
Marchini L, Recker E, Hartshorn J, Cowen H, Lynch D, Drake D, et al. Iowa nursing facility oral hygiene (INFOH) intervention: a clinical and microbiological pilot randomized trial. Spec Care Dentist. 2018;38(6):345–55.
Seleskog B, Lindqvist L, Wårdh I, Engström A, von Bültzingslöwen I. Theoretical and hands-on guidance from dental hygienists promotes good oral health in elderly people living in nursing homes, a pilot study. Int J Dent Hyg. 2018;16(4):476–83.
Berniyanti T, Kusumo A, Bramantoro T, Wening G, Palupi R. Dental and oral health education for elderly age group: full and partial edentulous teeth brushing method. J Int Oral Health. 2019;11(2):104–6.
Iwao Y, Shigeishi H, Takahashi S, Uchida S, Kawano S, Sugiyama M. Improvement of physical and oral function in community-dwelling older people after a 3-month long-term care prevention program including physical exercise, oral health instruction, and nutritional guidance. Clin experiment dental res. 2019;5(6):611–9.
Keyong E, Thitasomakul S, Tianviwat S. Effectiveness of an oral health promotion program for the elderly in Khiri mat district, Sukhothai province: a randomized control trial. J Intl Soc Prev Community Dent. 2019;9(3):225–31.
León S, González K, Hugo FN, Gambetta-Tessini K, Giacaman RA. High fluoride dentifrice for preventing and arresting root caries in community-dwelling older adults: a randomized controlled clinical trial. J Dent. 2019;86:110–7.
Laurence B, Rogers I, Grant-Mills D, Smith D, Tefera E, Barbarinde A, et al. Reducing dental plaque scores in long-term care facilities using a checklist and random inspections: a pilot study. Bull Tokyo Dent Coll. 2019;60(3):177–84.
Saleem M, Yoshinari N, Nakamura S, Sumi Y, Iwai Y, Ozaki Y, et al. Improvement of salivary flow and oral wetness by a lip trainer device and sonic toothbrush in older Japanese men and women with dry mouth. J Oral Sci. 2019;61(2):221–8.
Tellez M, Myers Virtue S, Neckritz S, Bhoopathi V, Hernández M, Shearer B. Motivational interviewing and oral health education: experiences from a sample of elderly individuals in north and Northeast Philadelphia. Special Care Dentist. 2019;39(2):201–7.
Tellez M, Myers Virtue S, Neckritz S, Lim S, Bhoopathi V, Hernandez M, et al. Randomised clinical trial of a motivational interviewing intervention to improve oral health education amongst older adults in Philadelphia: 12-month evaluation of non-clinical outcomes. Gerodontol. 2020;37(3):279–87.
Ting CC, Ko EC, Chen CC, Chang WY, Tu HP, Chang CS. Effectiveness of an oral function intervention for older Taiwanese people. Gerodontol. 2019;36(4):374–81.
Johansson I, Torgé CJ, Lindmark U. Is an oral health coaching programme a way to sustain oral health for elderly people in nursing homes? A feasibility study. Int J Dent Hyg. 2020;18(1):107–15.
Konstantopoulou K, Kossioni A, Karkazis H, Polyzois G. Implementation and evaluation of an oral health education programme for caregivers in nursing homes. Spec Care Dentist. 2021;41(2):154–63.
Lee KH, Lee KY, Choi YY, Jung ES. Effects of professional Oral health care programs for elderly residents of nursing facilities. J Dent Hyg. 2020;94(6):33–9.
Lee KH, Choi YY, Jung ES. Effectiveness of an oral health education programme for older adults using a workbook. Gerodontol. 2020;37(4):374–82.
Ho BV, van der Maarel-Wierink CD, Rollman A, Weijenberg RAF, Lobbezoo F. Don't forget the mouth!': a process evaluation of a public oral health project in community-dwelling frail older people. BMC Oral Health. 2021;21(1):536.
Ki JY, Jo SR, Cho KS, Park JE, Cho JW, Jang JH. Effect of Oral health education using a Mobile app (OHEMA) on the Oral health and swallowing-related quality of life in community-based integrated Care of the Elderly: a randomized clinical trial. Int J Environ Res Public Health. 2021;18(21).
Lee KH, Choi YY, Jung ES. Effectiveness of an oral health education programme for older adults using a workbook. Gerodontology. 2020;37(4):374–82.
Northridge ME, Wu Y, Troxel AB, Min D, Liu R, Liang LJ, et al. Acceptability of a community health worker intervention to improve the oral health of older Chinese Americans: a pilot study. Gerodontol. 2021;38(1):117–22.
Peroz I, Klein C. Influence of professional dental hygiene on oral and general health of retirement home residents: a comparative study. Clin Experiment Dental Res. 2022;8(1):45–53.
Patel R, Fitzgerald R, Warburton F, Robertson C, Pitts NB, Gallagher JE. Refocusing dental care: a risk-based preventative oral health programme for dentate older people in UK care homes. Gerodontol. 2021.
Pawluk DL, Dale C, Lai JY, Villacorta-Siegal N, Smith J, Joseph K, et al. The impact of oral health education taken by personal support workers caring for a geriatric population in a long-term care facility: a mixed-methods study. Gerodontol. 2021;38(4):373–86.
Sun KT, Shieh TM, Hsia SM, Ningrum V, Lin XY, Shih YH. Easy to read health education material improves oral health literacy of older adults in rural community-based care centers: a quasi-experimental study. Healthcare (Basel). 2021;9(11).
Wanyonyi K, Couch C, John J, Louca C. E-Oral health interventions for older patients in an outreach primary dental care Centre: a pilot trial nested acceptability study. Gerodontol. 2021.
Strayer MS. Oral public health programs for the elderly: 1989. Am J Public Health. 1991;81(3):382–4.
Chalmers JM, Robinson J, Nankivell N. The practical oral care video - evaluation of a dental awareness month initiative. Aust Dent J. 2005;50(2):75–80.
McAnulla A, Reid B, Zieba M. Developing an integrated resource to promote oral health in nursing homes. Nurs Older People. 2018;30(2):25–8.
Lee YS, Kim J, Choy YS, Kim E, Yoo J. Change in denture procedures after implementation of National Health Insurance Coverage for the elderly in Korea: a Nationwide database. Int J Environ Res Pub Health. 2021;18(5).
Tynan A, Deeth L, McKenzie D. An integrated oral health program for rural residential aged care facilities: a mixed methods comparative study. BMC Health Serv Res. 2018;18(1):1–12.
Kyeong Hee L, Keun Yoo L, Yoon Young C, Eun Seo J. Effects of professional Oral health care programs for elderly residents of nursing facilities. J Dent Hyg. 2020;94(6):33–9.
Schwendicke F, Dörfer C, Schlattmann P, Page LF, Thomson W, Paris S. Socioeconomic inequality and caries: a systematic review and meta-analysis. J Dent Res. 2015;94(1):10–8.
Watt RG, Daly B, Allison P, Macpherson LM, Venturelli R, Listl S, et al. Ending the neglect of global oral health: time for radical action. Lancet. 2019;394(10194):261–72.
Natsch S, Van Der Meer J. The role of clinical guidelines, policies and stewardship. J Hosp Infect. 2003;53(3):172–6.
Petersen PE, Baez RJ, Ogawa H. Global application of oral disease prevention and health promotion as measured 10 years after the 2007 world health assembly statement on oral health. Commun Dent Oral Epidemiol. 2020;48(4):338–48.
World Health Organisation. WHO resolution on Oral health Geneva. Switzerland: WHO; 2021.
World Health Organization. WHO Discussion paper on Draft Global Strategy on Oral Health, Draft Version 9, August 2021. WHO; 2021. Available from: https://www.who.int/publications/m/item/who-discussion-paper-draft-globalstrategy-on-oral-health. [Cited: 28 October 2022]
Wong FM, Ng YT, Leung WK. Oral health and its associated factors among older institutionalized residents—a systematic review. Int J Environ Res Public Health. 2019;16(21):4132.
Poudel P, Griffiths R, Wong VW, Arora A, Flack JR, Khoo CL, et al. Oral health knowledge, attitudes and care practices of people with diabetes: a systematic review. BMC Pub Health. 2018;18(1):1–12.
Huang J, Yao Y, Jiang J, Li C. Effects of motivational methods on oral hygiene of orthodontic patients: a systematic review and meta-analysis. Med. 2018;97(47):e13182.
Garcia-Pola M-J, Rodriguez-Lopez S, Fernanz-Vigil A, Bagan L, Garcia-Martin J-M. Oral hygiene instructions and professional control as part of the treatment of desquamative gingivitis. Systematic review. Med oral, patol oral y cirugia bucal. 2019;24(2):e136–44.
Shu X, He S, Lo E, Leung K. A systematic review and Meta-analysis of the effect of Oral exercises on masticatory function. J Dent Res. 2022;101(5):515–25.
Slot D, Vaandrager N, Van Loveren C, Helderman WVP, Van der Weijden G. The effect of chlorhexidine varnish on root caries: a systematic review. Caries Res. 2011;45(2):162–73.
Hendre AD, Taylor GW, Chávez EM, Hyde S. A systematic review of silver diamine fluoride: effectiveness and application in older adults. Gerodontol. 2017;34(4):411–9.
de Lugt-Lustig KH, Vanobbergen JN, van der Putten GJ, De Visschere LM, Schols JM, de Baat C. Effect of oral healthcare education on knowledge, attitude and skills of care home nurses: a systematic literature review. Commun Dent Oral Epidemiol. 2014;42(1):88–96.
Brady MC, Furlanetto D, Hunter R, Lewis SC, Milne V. Staff-led interventions for improving oral hygiene in patients following stroke. Cochrane Database Syst Rev. 2006;4.
Bots-VantSpijker PC, Bruers JJ, Bots CP, Vanobbergen JN, De Visschere LM, de Baat C, et al. Opinions of dentists on the barriers in providing oral health care to community-dwelling frail older people: a questionnaire survey. Gerodontol. 2016;33(2):268–74.
Bots-VantSpijker PC, Vanobbergen JN, Schols JM, Schaub RM, Bots CP, de Baat C. Barriers of delivering oral health care to older people experienced by dentists: a systematic literature review. Commun Dent Oral Epidemiol. 2014;42(2):113–21.
Patterson Norrie T, Villarosa AR, Kong AC, Clark S, Macdonald S, Srinivas R, et al. Oral health in residential aged care: perceptions of nurses and management staff. Nursing open. 2020;7(2):536–46.
Ástvaldsdóttir Á, Boström AM, Davidson T, Gabre P, Gahnberg L, Sandborgh Englund G, et al. Oral health and dental care of older persons—a systematic map of systematic reviews. Gerodontol. 2018;35(4):290–304.
Acknowledgements
The authors of the paper appreciate technical and financial supports from the Healthy Ageing Unit, World Health Organization in the completion of the project upon which the paper was developed. The funders had no role in the design or conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, and approval of the manuscript.
Funding
The authors of the paper acknowledge the technical and financial support received from the Healthy Ageing Unit, WHO for the completion of the project.
Author information
Authors and Affiliations
Contributions
PP, AG and LBR conceived the idea and study design of this review. RA and GP conducted a search, screening, and analysis of data under the supervision of PP, LBR, AG, and WSB. PP, LBR, AG, WSB, RA, and GP prepared the first draft. All authors provided input into versions of the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Poudel, P., Paudel, G., Acharya, R. et al. Oral health and healthy ageing: a scoping review. BMC Geriatr 24, 33 (2024). https://doi.org/10.1186/s12877-023-04613-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04613-7