Abstract
Background
This cross-sectional study evaluated the impacts of functional tooth loss on oral health-related quality of life (OHRQoL) among elderly people compared with the impacts of several common indicators of oral health. Additionally, the cut-off of functional tooth loss needed for a better OHRQoL was investigated to establish a new measure for successful oral ageing.
Methods
Data from people aged 65–74 were extracted from the Fourth National Oral Health Survey in Sichuan, China. Functional tooth loss was defined as both natural tooth loss and nonfunctional teeth, such as third molars, residual roots, and removable dentures. The cut-offs of tooth loss were first identified as 12, based on the previous definition of functional dentition (≥20 natural teeth except the third molars), and 14, 16, or 18 for further investigation. OHRQoL was evaluated by the standardized Geriatric Oral Health Assessment Index (sGOHAI) score. Logistic regression was performed to estimate the impacts on OHRQoL. Additionally, subgroup analyses were conducted using the stratified chi-square test to explore the effect of functional tooth loss at each position.
Results
The mean GOHAI score of the 744 participants was 48.25 ± 7.62. Elderly people who had lost ≤12 functional teeth had greater odds of reporting a higher sGOHAI score than those who had lost more functional teeth (odds ratio (OR) 1.49, 95% confidence interval (CI) 1.05–2.11). No significant difference in the sGOHAI score was detected between people who had lost 13–16 functional teeth and those who had lost ≤12 functional teeth (0.61, 0.35–1.07). The loss of second premolars and first and second molars had great impacts on the sGOHAI score when ≤12 or ≤ 16 functional teeth had been lost.
Conclusions
Compared with natural tooth loss, functional dentition and occluding pairs, functional tooth loss can be a better indicator of OHRQoL in the elderly population. Sixteen remaining functional teeth seem to be sufficient to maintain good OHRQoL and successful oral ageing despite that number being previously acknowledged as ≥20 teeth.
Similar content being viewed by others
Background
With the global demographic transition, including an increase in life expectancy and a growth in the proportion of older people, there is an urgent need for geriatric oral health care [1,2,3]. The World Health Organization (WHO) states that population ageing can result in difficulties in the management and maintenance of acceptable oral health and necessary oral functions [1]. Consequences of poor oral health among older adults can include pain and suffering, aesthetic concerns, psychosocial distress, and adverse impacts on the quality of life in this specific vulnerable population [4,5,6,7], which can hardly achieve successful oral ageing, the process of developing and maintaining oral function that enables well-being in old age [8]. Therefore, oral health-related quality of life (OHRQoL), which indicates the self-perceived impacts of oral health on physical and psychosocial well-being [9], has generally been considered an important patient-centred parameter to comprehensively evaluate an individual’s oral health status, particularly among older persons [10,11,12].
Tooth loss reflects the complex outcome of oral diseases and the individual’s history of dental treatment over the life course [4, 13] and is considered a common indicator of OHRQoL [14,15,16]. However, the results of the literature are still inconsistent regarding the relationship between tooth loss/retention and OHRQoL [1, 17]. Some research has shown that the number of natural teeth might have a positive association with OHRQoL [18], and the cut-off of the number of teeth indicating successful oral ageing (which is also called functional dentition by the WHO) associated with a higher OHRQoL varied between 20 and 21 [13, 19]. However, some studies reported that there was no significant association between the number of natural teeth and OHRQoL [1, 18]. Instead, some researchers have suggested that the number of occluding pairs might have more potential to identify OHRQoL [20, 21], but notably, it might take more time and effort to determine and record the occlusal relationship than to simply count the number of teeth.
Teeth that function well in mastication, including sound natural teeth, teeth with early-stage caries, teeth with enamel, teeth with dentin decay, and filled teeth, are defined as functional teeth, while teeth with severe or pulpal decay and stump teeth, third molars and residual roots are considered nonfunctional teeth [22, 23]. Removable dentures are regarded as nonfunctional due to their controversial effect on oral function [24]. Therefore, we further defined “functional tooth loss” as follows: natural and nonfunctional tooth loss, such as the third molars, residual roots, and the use of removable dentures. To our knowledge, no studies have confirmed the association between functional tooth loss and OHRQoL.
Thus, this study aimed to determine the relationship between functional tooth loss and OHRQoL in older people compared with the relationships between OHRQoL and several common indicators (i.e., natural tooth retention, functional dentition, and occluding pairs) of oral health. A significant association was assumed to be found between functional tooth loss and OHRQoL in the older population (hypothesis). Additionally, the cut-off of the number of missing functional teeth (functional tooth loss) associated with a high OHRQoL was investigated to establish a new measure for successful oral ageing, providing clinicians and clinical researchers with a new approach for clinical decision-making and support for the formulation of relevant oral health care policies.
Methods
The present observational study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement, and all relevant information was reported according to the STROBE checklist for cross-sectional studies.
Study design
As a part of the Fourth National Oral Health Survey of China, this cross-sectional study was completed in Sichuan in 2016, after the validation of the pretest finished in the same target population in August 2015 [17, 25, 26]. Ethical approval was granted by a local stomatological ethics committee. Data from participants aged 65–74 years were used in this study.
Survey sampling
A four-stage stratified random cluster sampling was conducted using the probability proportional to size (PPS) method [25]. Six areas, including three districts and three counties, were randomly selected in the first two stages. Three communities were then selected in each respective area, and participants were randomly selected by a quota sampling method in the fourth stage [25]. Individuals with serious physical or psychological illness or disadvantages and those who were unable or unwilling to complete the survey were excluded [25, 27].
Subjects
The target population was residents aged 65–74 years, and the minimum required sample size of 696 was calculated based on the following formula [25]:
where deff as the design efficiency was 2.5; p as the prevalence of caries in this population of older people in the Third National Oral Health Survey was 86.0%; the nonresponse rate was 15%; μ as the level of confidence was 1.96; and ε as the margin of error was 10%.
Clinical examination
According to the fifth version of the World Health Organization Oral Health Survey-Basic Methods [28], participants received an oral clinical examination executed by three licenced dentists (LC, JL, LL) and recorded by three trained individuals (HC, FZ, SD). All examiners were trained by the standard examiner and passed the consistency check before this study. Interobserver variability was analysed, and the mean kappa values were both > 0.85.
The standardized oral examination focused on dentition status, including tooth loss, coronal and root caries, and denture conditions. Teeth missing for any reason were classified as natural tooth loss. A number of remaining natural teeth (except the third molars, which are usually nonfunctional) ≥20 was considered functional dentition [22, 23, 29]. Tooth pairs with occlusal contact, according to the normal tooth position in centric occlusion, were regarded as occluding pairs [30]. Functional tooth loss was defined to include both natural tooth loss and nonfunctional teeth (those remaining but not achieving oral function, i.e., residual roots, third molars, etc.) (Fig. 1). Removable dentures were also included as functional tooth loss, as their effects on oral function are controversial [31, 32]. Fixed prostheses and dental implants were considered remaining functional teeth because recent studies have proven their positive effects on OHRQoL [33, 34]. The number 12 was identified as the cut-off of natural tooth loss, which equalled 20 remaining natural teeth [13, 18, 19]. Similarly, the cut-off of functional tooth loss was also identified to be 12, which equalled 20 functional remaining teeth. To explore the minimum number of functional teeth needed for better OHRQoL, 14 was also taken as the cut-off value, which divided the number of functional tooth losses into three groups: > 14, 13–14, and ≤ 12, as well as 16 and 18. Additionally, participants were identified into six classes (complete dentition, type I, type II, type III, type IV, edentulous) by two independent, experienced dentists (LC, HC) according to the Kennedy classification, and any disagreements were resolved through discussion with a third assessor (TH).
Questionnaire
Participants’ basic information, including demographic variables (age, sex, educational status, and household annual income), health behaviours including smoking and drinking habits, medical history, and self-rated oral health status, was extracted from a self-report questionnaire, and all records were verified before entry. The participants’ educational status was classified into two levels: “low” (“junior high school” or below) and “high” (“high school” or above). Household annual income per capita was categorized into three categories (<10, 10–20, > 20 thousand) [35]. Smoking and drinking habits were dichotomized as “yes” (“past or current smoking/drinking”) or “no” (“never smoking/drinking”). Medical history was evaluated as “yes” or “no” according to the presence of any systemic diseases. Self-rated oral health status was evaluated by a 1–5 Likert scale: “very poor”, “poor”, “fair”, “good”, and “very good”. The variables above and tooth loss were considered explanatory variables for the analyses with OHRQoL.
OHRQoL was measured in the questionnaire using the Chinese version of the 12-item Geriatric Oral Health Assessment Index (GOHAI), which evaluated the impacts of oral conditions on daily activities, such as physical function, pain and discomfort, and psychosocial function [36]. Responses were made on a 5-point Likert scale (1 = “always”, 2 = “often”, 3 = “sometimes”, 4 = “seldom”, and 5 = “never”). The total scores for the GOHAI were summed by the ordinal value of each question, ranging from 12 to 60, where a higher GOHAI score indicated a better OHRQoL. To obtain a clearer distribution of GOHAI scores, we applied the following formulas to convert a raw score into a standardized score [37]:
The transformed GOHAI scores in all categories ranged from 0 to 10, and the mean standardized GOHAI (sGOHAI) score was 50, which was then divided into two categories: “low” (sGOHAI score ≤ 50) or “high” (sGOHAI score > 50).
Statistical analysis
All questionnaires and examination reports were double-entered by two trained dentists (YC, YX). Categorical and continuous variables are presented as prevalences and proportions or means±standard deviations (SDs). The frequency of functional tooth loss at each tooth position is shown in heatmaps, demonstrated by a commonly used thermogram and heatmaps shown in dentitions. The frequency of the Kennedy classifications is shown in a circular graph. Binary logistic regression was performed to calculate unadjusted and adjusted (sex, age, educational status, household annual income level, smoking and drinking habits, medical history, and self-rated oral health) odds ratios (ORs) and 95% confidence intervals (95% CIs), analysing the relationships of functional tooth loss, natural tooth loss, functional dentition, and occluding pairs with the total sGOHAI score and 12 sGOHAI item scores. Binary logistic regression was also used to evaluate the relationships among three groups of functional tooth loss with different cut-offs (12, 14, 16, and 18) and sGOHAI scores. Further analyses were conducted to explore the associations between the positions of the lost teeth and the sGOHAI score in different subgroups of people with ≤12, > 12, ≤16 or > 16 missing functional teeth using a stratified chi-square test. SPSS Statistics V.26.0 (IBM Corp., Armonk, NY) was used for data analysis and statistics.
Results
A total of 744 participants (48.7% males) were included in this study. All participants completed the clinical examination and the questionnaire. The mean age of the study population was 68.48 ± 2.76 years, and 86.2% of them had an educational level of no higher than junior high school. More than half of the subjects (61.8%) had been previously diagnosed with at least one systemic ailment. The demographic characteristics of the participants are reported in Table 1.
The mean GOHAI score was 48.25 ± 7.62, with a median score of 49, which was converted to 57.26 ± 4.34 after standardization. A total of 54.8% of the elderly participants had a better OHRQoL (sGOHAI score > 50) than the others. For responses to each item, almost half of the subjects reported problems with food selection and biting/chewing, while nearly one in every three older people indicated sensitive gums or showed worry or concern about their oral health problems (Table 2).
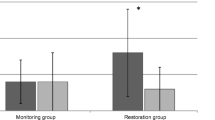
Regarding oral health status, 7.9% of the participants were edentulous, 71.9% had ≥20 natural teeth, and 20.2% had lost > 12 teeth (<20 teeth remained). The mean numbers of functional tooth loss, natural tooth loss and occluding pairs were 10.24 ± 9.18, 8.12 ± 8.35 and 9.18 ± 4.75, respectively. The frequency of molars lost was much higher than that of premolars, followed by incisors and canines. Maxillary teeth were more likely to be lost than mandibular teeth, but there was no significant difference between the left and right sides (Fig. 2).
The frequency of functional tooth loss for each tooth position. The dentitions show the frequency of functional tooth loss in each tooth position among elderly people with functional tooth loss ≤12, 13–16, and > 16, from 0% in blue to 100% in red. a The heatmap summarizing the frequency of functional tooth loss in each position in three groups; and b-d the frequency of functional tooth loss in each position among people who lost ≤12, 13–16, and > 16 functional teeth, where the upper and lower panel shows the frequency of functional tooth loss in maxillary and mandibular jaws, and the middle panel shows the bar chart for the frequency of functional tooth loss in each tooth position
Regarding restorations, 188 (183 of whom had lost ≤12 functional teeth) and 256 (253 of whom had lost ≤12 functional teeth) participants had no need for maxillary or mandibular restorations, respectively. Compared to those who had lost > 12 functional teeth, fewer participants were identified as Kennedy Class I (7.9% maxillary and 4.8% mandible) and Kennedy Class II (19.8 and 16.9%), but more were identified as Kennedy Class III (34.7 and 25.8%) in the group of older people who had lost fewer teeth. Sixty-six participants had a maxillary edentulous jaw, and 67 had a mandibular edentulous jaw (Fig. 3).
The Kennedy classification of participants (n = 744). Different colours indicate different classes of the Kennedy classification. The size of the rings represents the proportions of each type. The inner ring shows the classes of maxillary teeth, and the outer ring shows that of mandibular teeth. a the Kennedy classification of people with ≤12 functional tooth loss; b the Kennedy classification of people with > 12 functional tooth loss
After adjusting for confounders, such as sex, age, educational status, level of household per capita annual income, smoking habits, drinking habits, medical history, and self-rated oral health, the number of missing functional teeth was significantly associated with the OHRQoL among older adults (OR = 1.49, 95% CI 1.05 to 2.11, P = .026; Table 3). However, no significant association was found between the sGOHAI score and the number of missing natural teeth (1.39, 0.93 to 2.08, P = .114), the number of occluding pairs (1.03, 0.99 to 1.06, P = .154) or functional dentition (1.43, 0.96 to 2.13, P = .076) after adjustment.
Moreover, in further analysis, functional tooth loss was shown to be related to a greater number of GOHAI items than natural tooth loss, with a greater impact on oral physical and psychosocial function and the least impact on subjective feelings such as pain and discomfort. Functional tooth loss had the most profound impact on speech ability, as people who had lost ≤12 functional teeth had greater odds of speaking clearly (4.82, 3.17 to 7.33, P<.001) and had fewer limitations in having contact with others (2.52, 1.65 to 3.83; P<.001) than those who had lost > 12 functional teeth. Compared with natural tooth loss, the number of missing functional teeth was significantly associated with food selection (1.52, 1.05 to 2.19, P = .025), biting/chewing ability (1.58, 1.09 to 2.28, P = .015), and worry or concern (0.71, 0.51 to 0.98, P = .040). However, the effect of natural tooth loss (1.72, 1.15 to 2.59, P = .009) and functional dentition (1.58, 1.06 to 2.36, P = .025) on swallowing ability remained significant after adjustment, while the numbers of missing functional teeth and occluding pairs did not (Table 3).
Further analysis showed that no significant difference was found in sGOHAI scores between people who lost 13–14 (1.19, 0.60 to 2.33, P = .621) or 13–16 (0.90, 0.52 to 1.54, P = .694) functional teeth and those with ≤12 missing functional teeth. However, a significant difference was found between people who had lost > 16 functional teeth and those who had lost ≤12 (0.59, 0.40 to 0.88, P = .009). No significant difference was found between people with ≤12 and 13–14 missing functional teeth in terms of sGOHAI scores in all items. For the cut-off of 16, no significant association was found with most items. However, people with 13–16 missing functional teeth had greater odds of speaking clearly (0.41, 0.22 to 0.77, P = .006) and having worry or concern about their oral health problems (1.72, 1.02 to 2.89, P = .041) compared with those with ≤12 missing functional teeth. Although no significant difference was found in the total sGOHAI score between the elderly individuals who had lost 13–18 functional teeth and those who had lost ≤12 missing functional teeth (0.77, 0.49 to 1.24; P = .280), significant differences in more items were found between those groups than between the other groups (Table 4).
Further subgroup analyses showed significant associations between losing the second premolars (0.60, 95% CI 0.41 to 0.87, P = .012), first molars (0.65, 0.45 to 0.93, P = .018), or second molars (0.58, 0.40 to 0.83, P = .003) and the sGOHAI score when people had lost ≤12 functional teeth. For those who had lost ≤16 functional teeth, similar associations with the sGOHAI score were also found for the second molars (0.60, 0.42 to 0.84, P = .003), first molars (0.64, 0.46 to 0.90, P = .009) and second premolars (0.62, 0.44 to 0.87, P = .006). Moreover, among people who had lost > 16 functional teeth, a significant association was observed between the loss of central incisors and the sGOHAI score (8.78, 1.11 to 69.60, P = .015), while no such relationship was detected in other groups (Table 5).
Discussion
The present cross-sectional analysis of 744 older individuals aged 65–74 years comprehensively explored the relationship between tooth loss and OHRQoL. Compared with natural tooth loss, functional dentition, or occluding pairs, a more positive relationship was found between losing ≤12 (even ≤14 or ≤ 16) functional teeth and a better OHRQoL, especially in the physical and psychosocial function domains; the hypothesis of our study was confirmed. These findings highlight the importance of maintaining both tooth number and tooth function in the older population and establishing a new measure for good OHRQoL and successful oral ageing. The results were relatively reliable and showed good extrapolation and generalizability, with representative samples and effective control of the relevant bias.
Unlike the previous controversial results reported for common indicators [13, 32, 38, 39], the current study proposed the concept of functional tooth loss and explored its significant association with the OHRQoL of older persons, which mostly manifested in oral physiological and psychosocial functions. It was shown that functional tooth loss had greater effects on the OHRQoL of older adults than other common indicators, such as natural tooth loss, functional dentition, and occluding pairs. With increasing functional tooth loss, difficulties with food limitation, chewing difficulty, and speaking trouble were aggravated, which was consistent with previous studies [18, 20, 31]. Difficulties with smiling, speaking, aesthetics, and the social aspects of food brought by functional tooth loss might result in impaired self-esteem and social status as well as reduced emotional stability, thereby frustrating interpersonal relationships and leading to social fears and disorders [7, 38,39,40]. However, the effect of functional tooth loss on oral pain and discomfort was not detected in our study. The theory of response shift could be used to explain the irrelevance between tooth loss and oral pain. As a result of timing and the experience of poor health, older people might change their internal standards, values, or conceptualization of OHRQoL, which makes oral discomfort and pain unimportant at this point in their lives [1, 41].
However, compared with functional tooth loss, natural tooth loss and functional dentition were found to be significantly associated with swallowing function. We supposed that as a result of nonfunctional roots and third molars without chewing force, soft and chewable food was more likely to be subjectively chosen by the older population [20, 39, 42], which also contributed to the decrease in swallowing problems of older people [21, 42] and the increase in psychological stress [31]. When compared with occluding pairs, the relationship between functional tooth loss and physical or psychosocial function was not inferior, and it even had a more significant effect on the overall OHRQoL of older people. Moreover, without the need to record the occlusal relationship in detail, functional tooth loss might be more suitable for large-scale epidemiological investigation, which could be more convenient for quick inspection or recording.
Interestingly, we found that a smaller number of functional teeth was sufficient to maintain oral function in older participants. The older adults with 18–19 functional teeth (equal to the loss of 13–14 functional teeth) had a similar OHRQoL compared with those with ≥20 functional teeth remaining (i.e., the minimum number of teeth needed to maintain OHRQoL, according to the previous consensus). Moreover, compared with those who had lost ≤12 functional teeth, people with 13–16 missing functional teeth showed more difficulty speaking clearly and were more likely to be worried and concerned about their oral health problems. The results might be related to the significant association between central incisors and OHRQoL in the subgroup analysis, as anterior teeth, especially central incisors, generally have an important role in aesthetics and speech. However, more research with a larger sample size is needed to confirm this finding due to the limited sample size and skewed data distribution in the subgroup analysis. Even so, considering that these differences seemed to be acceptable while evaluating the OHRQoL of older people, we proposed that 16 functional teeth seemed to be the minimal requirement for maintaining good OHRQoL and successful oral ageing, which emphasized the importance of maintaining the function of remaining teeth rather than preserving or increasing the number of teeth in oral medicine.
Therefore, considering the importance of maintaining oral function via health promotion and disease prevention, several public health implications should be highlighted. On the one hand, a prevention-oriented oral medical system should be established to reduce the impact of functional tooth loss on OHRQoL and the economic burden of the older population, as tooth loss and the consequent oral diseases are preventable by promoting regular oral health care [11, 16, 43]. On the other hand, the goal of maintaining oral function should be prioritized in each clinical decision to ensure the acceptable OHRQoL of patients [13, 31]. Clinicians should make a comprehensive assessment of the impacts of any treatment modality on patients’ quality of life to provide patient-centred oral health care [13].
However, there were several limitations in this study. First, relevant data on functional tooth loss, natural tooth loss, functional dentition, and occluding pairs were obtained from the original records, which might introduce some bias to the study. Prospective studies evaluating occlusal functional or psychosocial function are needed to explore the differences in these indicators in clinical applications and to validate the results in the future. Second, the contribution of removable dentures to OHRQoL, of which the impact on oral function was reported to be controversial [31], was not involved in this study. The contribution of removable dentures to OHRQoL is reported to be difficult to evaluate in the short term due to the adaptation curve [24] and is inconclusive in the long term because of biological complications, including but not limited to caries and periodontal diseases [44]. Studies have shown that the function of removable dentures differs based on the position of replacement, denture self-satisfaction, patient outcome expectations and so on [33, 34]. Relevant research is needed to determine the effects of removable dentures on OHRQoL. Moreover, more experiments should be conducted to explore the mechanism of the impact of functional tooth loss on OHRQoL; for example, objective indicators are needed to evaluate changes in chewing function, swallowing function and other oral functions.
Conclusion
Functional tooth loss can be a better indicator of OHRQoL in the older population than some common indicators, such as natural tooth loss, functional dentition and occluding pairs. As the number of missing functional teeth increases, the OHRQoL of older people significantly decreases, particularly in the domains of physical and psychosocial functions. Moreover, at least 16 functional teeth seem to be the new measure of good OHRQoL and successful oral ageing. Global strategies aimed at preventing tooth loss and maintaining oral functions are needed to maintain acceptable OHRQoL in the ageing population.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- OHRQoL:
-
Oral health-related quality of life
- GOHAI:
-
The 12-item Geriatric Oral Health Assessment Index
- sGOHAI:
-
Standardized Geriatric Oral Health Assessment Index
- WHO:
-
World Health Organization
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- PPS:
-
Probability proportional to size
- SD:
-
Standard deviation
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Masood M, Newton T, Bakri NN, Khalid T, Masood Y. The relationship between oral health and oral health related quality of life among elderly people in United Kingdom. J Dent. 2017;56:78–83.
Kassebaum NJ, Smith AGC, Bernabé E, Fleming TD, Reynolds AE, Vos T, et al. Global, regional, and National Prevalence, incidence, and disability-adjusted life years for Oral conditions for 195 countries, 1990-2015: a systematic analysis for the global burden of diseases, injuries, and risk factors. J Dent Res. 2017;96(4):380–7.
Collaborators GDaIIaP. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–858.
Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, et al. Oral diseases: a global public health challenge. Lancet. 2019;394(10194):249–60.
Fang EF, Xie C, Schenkel JA, Wu C, Long Q, Cui H, et al. A research agenda for ageing in China in the 21st century (2nd edition): focusing on basic and translational research, long-term care, policy and social networks. Ageing Res Rev. 2020;64:101174.
Wong FMF, Ng YTY, Leung WK. Oral Health and Its Associated Factors Among Older Institutionalized Residents-A Systematic Review. Int J Environ Res Public Health. 2019;16(21):4132. https://doi.org/10.3390/ijerph16214132.
Rouxel P, Tsakos G, Chandola T, Watt RG. Oral Health-A Neglected Aspect of Subjective Well-Being in Later Life. J Gerontol B Psychol Sci Soc Sci. 2018;73(3):382–6. https://doi.org/10.1093/geronb/gbw024.
Sáenz-Ravello G, Contreras J, Baeza M, Silva AB, Danke K, Gonzalez S, et al. Functional dentition and well-being among Chilean 80-year-olds. Gerodontology. 2023. https://doi.org/10.1111/ger.12699.
Locker D. Measuring oral health: a conceptual framework. Community Dent Health. 1988;5(1):3–18.
Baniasadi K, Armoon B, Higgs P, Bayat AH, Mohammadi Gharehghani MA, Hemmat M, et al. The Association of Oral Health Status and socio-economic determinants with Oral health-related quality of life among the elderly: a systematic review and meta-analysis. Int J Dent Hyg. 2021;19(2):153–65.
Range H, Perier MC, Boillot A, Offredo L, Lisan Q, Guibout C, et al. Chewing capacity and ideal cardiovascular health in adulthood: a cross-sectional analysis of a population-based cohort study. Clin Nutr. 2020;39(5):1440–6.
Broadbent JM, Zeng J, Foster Page LA, Baker SR, Ramrakha S, Thomson WM. Oral health-related beliefs, behaviors, and outcomes through the life course. J Dent Res. 2016;95(7):808–13.
Tan H, Peres KG, Peres MA. Retention of teeth and Oral health-related quality of life. J Dent Res. 2016;95(12):1350–7.
Saito M, Shimazaki Y, Nonoyama T, Tadokoro Y. Association of oral health factors related to oral function with mortality in older Japanese. Gerodontology. 2021;38(2):166–73.
Watanabe Y, Okada K, Kondo M, Matsushita T, Nakazawa S, Yamazaki Y. Oral health for achieving longevity. Geriatr Gerontol Int. 2020;20(6):526–38.
Kassebaum NJ, Bernabe E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. Global burden of severe tooth loss: a systematic review and Meta-analysis. J Dent Res. 2014;93(7 Suppl):20S–8S.
Shao R, Hu T, Zhong YS, Li X, Gao YB, Wang YF, et al. Socio-demographic factors, dental status and health-related behaviors associated with geriatric oral health-related quality of life in southwestern China. Health Qual Life Outcomes. 2018;16(1):98.
van de Rijt LJM, Stoop CC, Weijenberg RAF, de Vries R, Feast AR, Sampson EL, et al. The influence of Oral health factors on the quality of life in older people: a systematic review. Gerontologist. 2020;60(5):e378–94.
WHO Expert Committee on Recent Advances in Oral Health & World Health Organization. Recent advances in oral health : report of a WHO expert committee [meeting held in Geneva from 3 to 9 December 1991] . World Health Organization. 1992. https://iris.who.int/handle/10665/39644.
Huang YF, Liu SP, Muo CH, Chang CT. The impact of occluding pairs on the chewing patterns among the elderly. J Dent. 2021;104:103511.
Lin YS, Wang Q, Shen ZK, Sun HX, Wu C, He H, et al. Association of Loss of occlusal pairs of teeth with sarcopenia in a Chinese population of community-dwelling elderly. J Nutr Health Aging. 2022;26(5):439–44.
Fukai K, Takiguchi T, Ando Y, Aoyama H, Miyakawa Y, Ito G, et al. Functional tooth number and 15-year mortality in a cohort of community-residing older people. Geriatr Gerontol Int. 2007;7(4):341–7.
Loureiro RM, Sumi DV, Tames H, Ribeiro SPP, Soares CR, Gomes RLE, et al. Cross-sectional imaging of third molar-related abnormalities. AJNR Am J Neuroradiol. 2020;41(11):1966–74.
Choong EKM, Shu X, Leung KCM, Lo ECM. Oral health-related quality of life (OHRQoL) after rehabilitation with removable partial dentures (RPDs): A systematic review and meta-analysis. J Dent. 2022;127:104351. https://doi.org/10.1016/j.jdent.2022.104351.
Yin W, Yang YM, Chen H, Li X, Wang Z, Cheng L, et al. Oral health status in Sichuan Province: findings from the oral health survey of Sichuan, 2015-2016. Int J Oral Sci. 2017;9(1):10–5.
The fourth national oral health epidemiology survey technology group, C.s.a.: Workbook of the fourth national oral health epidemiology survey (2015–2018). 2015.
Wang L, Cheng L, Yuan B, Hong X, Hu T. Association between socio-economic status and dental caries in elderly people in Sichuan Province, China: a cross-sectional study. BMJ Open. 2017;7(9):e016557.
Dioguardi M, Gioia GD, Illuzzi G, Laneve E, Cocco A, Troiano G. Endodontic irrigants: different methods to improve efficacy and related problems. Eur J Dentistry. 2018;12(3):459–66.
World Health Organization. Oral health surveys: basic methods. Geneva: World Health Organization; 2013.
Lin HC, Corbet EF, Lo EC, Zhang HG. Tooth loss, occluding pairs, and prosthetic status of Chinese adults. J Dent Res. 2001;80(5):1491–5.
Naka O, Anastassiadou V, Pissiotis A. Association between functional tooth units and chewing ability in older adults: a systematic review. Gerodontology. 2014;31(3):166–77.
Han JH, Lee HJ, Han JW, Suh SW, Lee JR, Byun S, et al. Loss of functional dentition is associated with cognitive impairment. J Alzheimers Dis. 2020;73(4):1313–20.
Garcia-Minguillan G, Preciado A, Romeo M, Rio JD, Lynch CD, Castillo-Oyague R. Differences in self-perceived OHRQoL between fully dentate subjects and edentulous patients depending on their prosthesis type, socio-demographic profile, and clinical features. J Dent. 2021;114:103756.
Ali Z, Baker SR, Shahrbaf S, Martin N, Vettore MV. Oral health-related quality of life after prosthodontic treatment for patients with partial edentulism: a systematic review and meta-analysis. J Prosthet Dent. 2019;121(1):59–68 e53.
Zhi QH, Si Y, Wang X, et al. Determining the factors associated with oral health-related quality of life in Chinese elders: Findings from the fourth national survey. Community Dent Oral Epidemiol. 2022;50(4):311–20. https://doi.org/10.1111/cdoe.12674.
Wong MCM, Liu JKS, Lo ECM. Translation and validation of the Chinese version of GOHAI. J Public Health Dent. 2002;42(2):78–83.
Ware JE: SF-36 health survey: Manual and interpretation guide. In: 2003.
Fukushima-Nakayama Y, Ono T, Hayashi M, Inoue M, Wake H, Ono T, et al. Reduced mastication impairs memory function. J Dent Res. 2017;96(9):1058–66.
Yin Z, Yang J, Huang C, Sun H, Wu Y. Eating and communication difficulties as mediators of the relationship between tooth loss and functional disability in middle-aged and older adults. J Dent. 2020;96:103331.
Verlaan S, Ligthart-Melis GC, Wijers SLJ, Cederholm T, Maier AB, de van der Schueren MAE. High prevalence of physical frailty among community-dwelling malnourished older adults-a systematic review and Meta-analysis. J Am Med Dir Assoc. 2017;18(5):374–82.
Feng Z, Glinskaya E, Chen H, Gong S, Qiu Y, Xu J, et al. Long-term care system for older adults in China: policy landscape, challenges, and future prospects. Lancet. 2020;396(10259):1362–72.
Maitre I, Lourtioux F, Picouet P, Braud A. Oral health-related food selectivity among French independently living elders. J Oral Rehabil. 2020;47(4):511–22.
Celeste RK, Eyjolfsdottir HS, Lennartsson C, Fritzell J. Socioeconomic life course models and Oral health: a longitudinal analysis. J Dent Res. 2020;99(3):257–63.
Moldovan O, Rudolph H, Luthardt RG. Biological complications of removable dental prostheses in the moderately reduced dentition: a systematic literature review. Clin Oral Investig. 2018;22(7):2439–61.
Acknowledgements
The authors would like to thank the Department of Preventive Dentistry, West China Hospital of Stomatology, Sichuan University, for conducting the survey and the Sichuan Centre for Disease Control and Prevention and oral institutions in Sichuan Province for their assistance, as well as all individuals who participated in this study.
Funding
This work was supported by the National Natural Science Foundation of China [grant numbers 72104162 and 82170948], Natural Science Foundation of Sichuan Province [grant number 2022NSFSC1377] and Research and Develop Program, West China Hospital of Stomatology Sichuan University [grant number LCYJ2020-DL-4].
Author information
Authors and Affiliations
Contributions
Y. Cheng and L. Cheng contributed to the study design, data acquisition, analysis, and interpretation and drafted and critically revised the manuscript. F. Zhu contributed to the study design, data acquisition and analysis and drafted and critically revised the manuscript. Y. Xiang and S. Duan contributed to data acquisition, analysis and interpretation and critically revised the manuscript. J. Luo and L. Lei contributed to the study design, data acquisition and interpretation and critically revised the manuscript. H. Cai contributed to the study design, data acquisition, analysis, and interpretation and drafted and critically revised the manuscript. T. Hu contributed to the study conception and design, data acquisition, analysis, and interpretation and critically revised the manuscript. All authors gave final approval and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present observational study was performed in accordance with the Declaration of Helsinki and followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cross-sectional studies. This study was approved by the Stomatological Ethics Committee of the Chinese Stomatological Association and the Ethics Committee of West China Hospital of Stomatology, Sichuan University (Approval No. 2014–003). Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cheng, Y., Cheng, L., Zhu, F. et al. New measure of functional tooth loss for successful Oral ageing: a cross-sectional study. BMC Geriatr 23, 859 (2023). https://doi.org/10.1186/s12877-023-04570-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04570-1