Abstract
Background
As the ageing population continues to grow in many countries, the prevalence of geriatric diseases is on the rise. In response, healthcare providers are exploring novel methods to enhance the quality of life for the elderly. Over the last decade, there has been a remarkable surge in the use of machine learning in geriatric diseases and care. Machine learning has emerged as a promising tool for the diagnosis, treatment, and management of these conditions. Hence, our study aims to find out the present state of research in geriatrics and the application of machine learning methods in this area.
Methods
This systematic review followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and focused on healthy ageing in individuals aged 45 and above, with a specific emphasis on the diseases that commonly occur during this process. The study mainly focused on three areas, that are machine learning, the geriatric population, and diseases. Peer-reviewed articles were searched in the PubMed and Scopus databases with inclusion criteria of population above 45 years, must have used machine learning methods, and availability of full text. To assess the quality of the studies, Joanna Briggs Institute's (JBI) critical appraisal tool was used.
Results
A total of 70 papers were selected from the 120 identified papers after going through title screening, abstract screening, and reference search. Limited research is available on predicting biological or brain age using deep learning and different supervised machine learning methods. Neurodegenerative disorders were found to be the most researched disease, in which Alzheimer’s disease was focused the most. Among non-communicable diseases, diabetes mellitus, hypertension, cancer, kidney diseases, and cardiovascular diseases were included, and other rare diseases like oral health-related diseases and bone diseases were also explored in some papers. In terms of the application of machine learning, risk prediction was the most common approach. Half of the studies have used supervised machine learning algorithms, among which logistic regression, random forest, XG Boost were frequently used methods. These machine learning methods were applied to a variety of datasets including population-based surveys, hospital records, and digitally traced data.
Conclusion
The review identified a wide range of studies that employed machine learning algorithms to analyse various diseases and datasets. While the application of machine learning in geriatrics and care has been well-explored, there is still room for future development, particularly in validating models across diverse populations and utilizing personalized digital datasets for customized patient-centric care in older populations. Further, we suggest a scope of Machine Learning in generating comparable ageing indices such as successful ageing index.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
The continuous progress in medical technology and advancements in living standards have enabled an increasing number of people to live to an advanced age. However, with old age comes a multitude of health issues, and simply living longer does not guarantee a state of good health. According to the World Health Organization (WHO) report, the share of the older population that is above 60 years of age is expected to double between 2015 and 2050, among which nearly 80 percent are from low and middle-income countries [1]. The persistence of communicable diseases, along with an increase in the prevalence of non-communicable diseases, has led to a reduction in the health and well-being of older people. To benefit from the changes in demographics, every nation faces significant challenges in ensuring that its healthcare and social systems are well prepared.
Health and well-being of the elderly
The absence of sickness is not the only indicator of good health. Health encompasses the aspects of physical, psychological, and social well-being [2]. The researchers given evidence that many older persons categorized as healthy based on the medical tests had vulnerabilities exposed to lifestyle-related or psychological problems, which affected their risks of dying or being handicapped within five years [3]. On the other side, some persons with chronic conditions possessed several qualities that kept them healthy. Overweight older persons with otherwise good physical and mental health, for example, had the lowest chance of dying or becoming handicapped. So, there are different kinds of illnesses faced by older adults. Physical vulnerabilities such as vision problems, loss of hearing, functional disability, chronic obstructive pulmonary diseases, cerebrovascular, cardiovascular diseases, and cancer are common illnesses experienced by old age people all over the world. Apart from these, obesity is another health concern that is affecting an increasing number of seniors around the country. Age-related increases in obesity peak in the 60 s and 70 s increasing the risk of diabetes, arthritis, cardiovascular disease, and several cancer types. According to the Longitudinal Ageing Study of India (LASI), 75% of the elderly suffer from chronic diseases and 40% have a disability due to various factors [4].
The mental health of older is equally significant as their physical health. With the increase in life expectancy, mental illness has significantly influenced the older person’s quality of life. Cognitive deficits, dementia, depression, and anxiety disorders are some of them. It has been pointed out by many researchers that middle- and low-income countries invest a very lesser amount for mental illness and most of it is neglected. At the same time, mental health disease awareness is minimal. Many individuals assume that memory issues and emotions of depression or pessimism are inevitable as they become older, so they delay or avoid getting help. As reported in the World Alzheimer Report 2021, 75% of people with dementia globally are undiagnosed [5]. Many elderly people, particularly those residing in long-term care institutions, are affected by depressive disorders and symptoms. As a result, the demand for mental health treatment in old age is becoming more widespread and urgent.
Machine learning in geriatric research
Machine Learning (ML) has revolutionized the technology sector with its day-to-day applications. Many developed countries are now adopting this technology to enhance their healthcare service [6]. This raises the question of whether ML will be a powerful tool for enhancing gerontological research. Developing an accurate and quick diagnosis is one of the most difficult aspects of care for geriatric patients. Such individuals bring complicated medical histories and clinical circumstances to healthcare settings, necessitating a focus on how to enhance patient care outcomes for this group. A statistical foundation underpins ML. This should be self-evident, given that ML requires data, which must be characterized using a statistical framework. It allows the user to submit an enormous quantity of data to a computer algorithm, which the computer may then evaluate and make data-driven suggestions and judgments based only on the supplied data [7]. This approach is promising since it readily discovers trends and patterns in a large dataset, is easy to handle multi-dimensional and multi-variety data, has wide applicability in practically every discipline, and is constantly improved.
Need of the study
Numerous systematic literature reviews have delved into the utilization of machine learning within the realm of geriatric research. Choudhury and colleagues conducted a comprehensive examination of the application of machine learning in geriatric clinical care, and they observed the absence of standardized metrics for evaluating machine learning models, as well as the pressing need for tailored data governance in the healthcare domain [8]. Another literature review explored the integration of machine learning and artificial intelligence in the context of geriatric mental health [9]. This review revealed that dementia stands as the most extensively researched mental health concern within this field, with inconsistent information availability for other mental health issues. Olender et al. undertook a systematic review of studies that used machine learning techniques to predict clinical outcomes in older populations [10], while Leghissa et al. scrutinized research papers focused on the detection, classification, and prediction of frailty in older adults using machine learning methods [11]. The summary of the objective and outcome of these studies have been described in Table 1. In the latter two decades of life, geriatric patients suffer from a variety of ailments, including chronic illnesses, frailty, cognitive decline, and functional dependency. These individuals require high-quality clinical treatment since their issues may lead to hospitalization. As a result, effective solutions for enhancing geriatric clinical care are required. Numerous studies from all over the world have used ML to identify older people at high risk for dementia, predict weakness, risk of falls, pneumonia, delirium, and acute kidney disease, and provide them care. The scope of this study encompasses a comprehensive examination of aging-related concerns, encompassing various facets such as brain age prediction, biological age prediction, chronic diseases, mental health issues, and cognitive disorders. Unlike previous literature, which often concentrated on singular aspects of aging, our research presents a holistic overview, shedding light on the multifaceted aspects of the aging process from creating successful ageing index to using genome data to understand biological ageing, from risk prediction, classification of around all geriatric diseases to multimorbidity, the current study has a broader coverage of literatures in ageing field. The present review mainly focuses on studies that have applied different ML algorithms for accessing the health and well-being and diseases in the elderly population.
In the present study, we sought to explore two research questions:
-
1.
What is the current state of research on the application of machine learning in addressing aging-related issues?
-
2.
How has machine learning been applied to study geriatric diseases, the type of population, methods, and datasets used?
So, the objective of the study is to understand the application of ML in solving ageing-related issues by studying the available literature and looking into the more refined measures and methodologies that will show a much better picture of the issue.
Methods
Literature search strategy
The systematic review followed the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [14]. In the current study, older adults are defined as individuals aged 45 and above. The study focuses on the healthy and successful attainment of ageing, with the illness older adults face during this process. PubMed and Scopus databases were used to search original articles, as the authors have access to these databases. The search was conducted focusing on the following three major domains:
-
Machine learning
-
Geriatric population
-
Diseases that occur in old age
For machine learning, we used the keywords Machine Learning, Unsupervised Machine Learning, Supervised Machine Learning. The second set of keywords is Geriatrics, Aged, Older Population for older adults. For the diseases, Diabetes Mellitus, Hypertension, Cancer, Cardiovascular Diseases, Heart Diseases, Lung Diseases, Chronic Obstructive Pulmonary Disease, Alzheimer’s Disease, Parkinson's Disease, Dementia, Mental Health Disorders were used as keywords with OR operator in both PubMed and Scopus for searching papers. Then we combined these three sets of keywords with AND operator to get results for all three domains at once. In the PubMed database, we used the available MeSH (Medical Subject Headings) terms related to our search. Only title, abstract, and keyword sections were selected for the search to get comprehensive and only important literature in the field. The literature search was done on 7th April 2023 and 10th October 2023. The search strategy is clearly explained in the Table 2.
The inclusion criteria of the study were:
-
Peer-reviewed papers with available full-text
-
Study includes older population and must have focused on any geriatric disease
-
Implementation of machine learning algorithm
Primarily, the research articles were excluded using the filter option of the database, based on the language (only English language articles were selected). We excluded papers focused on only the younger population, or have applied different methodology other than machine learning, and the papers whose full-text version is not available on the web are also excluded from our study. However, we included the studies covering both younger and older populations; and some studies have used deep learning methods, as this method is the advanced application of machine learning methods and is often considered as a subfield of it [15], the studies using only deep learning methods were decided to be included. Both the reviewers (A.D. & P.D.) carefully screened the titles and then abstracts of all the papers and discarded the papers that did not come under the scope of our research and violated our inclusion criteria. The selection of articles was initially done by one reviewer (A.D.) and then checked by another reviewer (P.D.). Figure 1 illustrates the PRISMA flowchart showing the number of articles screened, included, and excluded in each step.
Data collection process and critical analysis:
Both the reviewers (A.D. & P.D.) studied all the selected articles to collect useful information. The research articles were thoroughly read by one author (A.D.) and the objectives, type of data used and the machine learning methods used were summarised in an Excel sheet, which was further examined by another author (P.D.) to check the correctness.
Quality assessments of studies
The 70 studies were reviewed for quality by two authors, AD and PD, independently, and arrived at one score with mutual agreement using the Joanna Briggs Institute's (JBI) critical appraisal tool [16]. This tool is commonly employed for evaluating the methodological quality of studies, specifically analytical cross-sectional studies. It comprises eight questions that address issues related to internal validity and the risk of bias, including aspects such as confounding, selection, and the clarity of study sample reporting. A high risk of bias was determined if positive responses were 49% or lower, a moderate risk of bias if the measure fell between 50 and 69%, and a low risk of bias if positive responses exceeded 70%.
Results
The use of machine learning in geriatrics and ageing research has been on a significant rise since 2019, which is shown in Fig. 2. In 2021, the number of published papers was the highest compared to any other year.
Initially, we found 249 research articles from the PubMed database and 1415 research articles from the Scopus database, after using the filters according to our inclusion criteria, the number was cut down to 120 peer-reviewed research articles. However, out of these, only 100 papers had free access. After screening the titles of the articles, and screening the abstracts, a total of 70 articles were selected for the critical analysis. The score of the quality assessment of the studies conducted using the Joanna Briggs Institute's (JBI) critical appraisal tool which is available in Table- S2 of the supplementary file. Among the 70 studies, a specific number, only 3 studies showed a moderate risk of bias, while the remaining 67 studies demonstrated a low risk of bias. Importantly, none of the studies included in our review were identified as having a high risk of bias. A summary of the machine learning applications in different geriatric diseases and their objective, datasets, and findings are included in Table 3. Following are the findings from the table, grouped by disease type.
Biological and brain age prediction
Biological age refers to an individual's age as determined by their physical and physiological health, as opposed to their chronological age brain age on the other hand, is a measurement of the age of an individual's brain based on its physical condition and function. The concept of biological age and brain age is useful in understanding an individual's overall health and risk of age-related diseases. By using neural networks and supervised ML algorithms on clinical datasets, biological age prediction [15] and brain age prediction [12] were conducted by two different studies. Ageing-related problems [13], measurement of healthy ageing [17], and the association between the health status of older adults and environmental and social factors [18,19,20] were studied extensively.
Neurodegenerative disorders
There are many studies focused on neurodegenerative disorder, which includes Alzheimer’s disease, Parkinson’s disease, Dementia, and any type of cognitive disorders. Different types of deep neural networks were applied and compared with Cox proportional hazard models to predict the neurodegenerative disorders using population-based datasets [66], and another comparative analysis was done to understand the association between ageing process and these diseases [58]. Among all kinds of neurodegenerative diseases, Alzheimer’s disease was focused a lot. Some studies used biomarker data for example white matter hyperintensities [62], and particulate matter [70] to explore their role in causing Alzheimer’s disease. On the other hand, interestingly many studies have used social media (Twitter) data, to capture the sentiment of a large number of populations regarding the stigma of the disease [67]. Insurance claim data [57] is also used for the study. Most of the studies used regularised regression models, logistic regression, and deep learning models for capturing the risk. Among neurodegenerative disorders, another part of the disease is dementia [54, 61] and cognitive dysfunctions. Machine learning was used to diagnose and predict cognitive dysfunction mostly using population-based data [55, 56, 60, 72, 75], mostly using regression models from supervised ML, another type of studies have used biomarker variables [65], digital device features [59, 69], and hospital records [68] to analyse the risk factors of cognitive dysfunction. Similarly, for dementia, most of the studies used population-based surveys [63, 71, 73, 74] and clinical datasets [64] using classification and deep learning methods of ML. Mostly, logistic regression and random forest regression performed better than the other models applied.
Non-communicable diseases
Among NCDs, diabetes, hypertension, chronic kidney diseases, cancer, and cardiovascular diseases were explored. Diabetes mellitus is very common among the older population and machine learning has been extensively applied for the detection, prediction, and identification of risk factors of the disease. Studies have developed predictive models [34, 35] based on supervised ML (logistic regression, XG Boost, decision tree, etc.) and some studies identified associated risk factors [32, 33] using clustering algorithms (like principal component analysis), logistic regression classifiers, and other supervised ML algorithms. Predicative models for hypertension were developed by using population-based datasets [39], with the association of risk factors like high waist circumference [38], cognitive impairment [37], and sleep & pulmonary measures [36] discussed. LASSO (Least Absolute Shrinkage and Selection Operator) and Ridge regression were popularly used for finding the association of the risk factors and feature section for model building. Chronic kidney disease detection [42], predicting stone-free status [40], and identifying distinct types of kidney transplants [41] were the focus areas. Patient records from the hospital were the only source for this kind of study. To detect chronic kidney disease, image processing, and deep learning algorithms were used, for predicting stone-free status, supervised ML algorithms (like logistic regression, random forest, and XG Boost regressor) were used, and lastly for identifying the kidney transplants clustering approach was used on the organ sharing data of patients. We found two studies based on colorectal cancer [22] which evaluated its risk using a random forest model on primary care health records. Another study predicted the quality of colorectal cancer surgery [24] with the 30-day mortality data from a hospital record and applied supervised ML algorithms. Many studies applied cross-sectional health survey data [25, 26, 28] and administrative databases [27, 29, 31] for predicting the risk of cardiovascular diseases. These studies used deep learning algorithms, cluster analysis, and ensemble ML to identify risk factors.
Mental health conditions
Except physical health, mental health has equal importance for the overall body condition of older adults. Many types of mental health-related issues among the older population, for example, predicting depression from smartphone data using supervised ML models [46], identifying patients with depressive symptoms using random forest decision models on primary care visits [44], suicide prediction model [43], analysing the effect of environmental factors on mental health [45, 49], quantifying the psychotherapy content and its effect [47], and studying loneliness using social media data Twitter [48] and sentiment analysis were addressed by different studies. Most of the studies applied logistic regression, random forest, and deep learning models. The studies identifying environmental factors have used image data of surroundings along with neural networks and deep learning algorithms.
Furthermore, other diseases like oral health-related diseases, bone diseases, and multimorbidity were also covered. From our advanced search, we only found one study in the field of oral health, which predicted tooth loss among older adults using a population-based dataset and supervised ML classification algorithms [84]. One study on osteoporosis [21], which used CT (Computed Tomography) scan image data to develop various supervised ML models to develop prediction models was also found. Classification and prediction models for multimorbidity were developed using deep learning models, by comparing them with other ML algorithms [50]. For developing a score for an overall health condition, a set of multimorbidity was taken into account and analyzed with the help of logistic regression, and a gradient-boosted tree classifier [53].
Type of methods and datasets used in the included studies
We've provided an overview of model performance metrics in the final column of Table 3. These metrics include the Area Under the Curve—Receiver Operating Characteristic (AUC-ROC), accuracy, specificity, sensitivity, precision, and the F1 score. Based on these performance scores, the Random Forest algorithm demonstrated the highest performance, with Extreme Gradient Boosting and Neural Networks following as the second and third-best performers, respectively. To clarify, the AUC-ROC measures the ability of a model to distinguish between different classes, accuracy represents the proportion of correctly classified instances, specificity measures the ability to correctly identify negative cases, sensitivity assesses the ability to correctly identify positive cases, precision quantifies the accuracy of positive predictions, and the F1 score combines precision and sensitivity to provide a balanced evaluation of the model's performance.
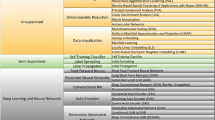
Figure 3 (a) & (b) shows the application of different types of ML methods and types of datasets used respectively. 67% of the papers included in our study have used supervised ML models, in which Random Forest, Logistic Regression, and the Decision Tree were the top three mostly used algorithms. After supervised ML, deep learning was the second most used algorithm, and lastly unsupervised ML. In unsupervised ML, the clustering technique was used often. Fig. 3 (b) shows the different types of datasets used. Nearly half of the studies (45%) used population-based surveys, while electronic health records and hospital-based data were the second highest used dataset. In the population-based datasets, two data sources English Longitudinal Study of Ageing (ELSA) and China Health and Retirement Longitudinal Study (CHARLS) were used more often. Then MRI/ CT images were the second highest used dataset. Many kinds of digitally traced data were also used, which includes internet databases like Kaggle, mobile application-based datasets, and data retrieved from social media APIs (Application Programming Interface) like Twitter.
The application of ML methods can be explained in three parts that is classification, risk prediction, and disease detection & diagnosis. The highest number of studies have predicted the risk factors or have built risk prediction models for different diseases. Under risk prediction, health survey datasets from population-based cross-sectional studies or biobank studies have been used to build the models. For the same, survival models like the Cox proportional hazard ratio model penalized regressions and supervised ML (decision tree, random forest, support vector machine, and logistic regression) were mostly used. Another type of data is nationally represented administrative population-based datasets, which have mostly focused on the sociodemographic and behavioral risk factors of the diseases. These studies have used supervised ML and deep learning methods to get the desired result. Except for these, some studies used hospital records, primary care visit records, and insurance data. The second category is disease detection and classification. Disease detection refers to the identification of the presence of a disease or condition usually through screening and testing. While, on the other hand, disease diagnosis is the process of identifying the specific disease or condition that is causing a person’s symptoms [85]. Generally, population-based datasets, biomarker data, and image-based data such as MRI, and retinal image data were used to detect or diagnose the disease in the studies. For image-based data, hierarchical clustering is used to detect the disease. In the case of other datasets, a mix of deep learning and supervised machine learning was used. The third category is disease classification. In the context of machine learning, disease classification refers to the process of developing algorithms or models that can automatically classify or categorize diseases based on labeled data separating diseases and not diseases or the severity of the illness. Ensemble ML algorithms, deep neural networks, random forests, and decision trees were the methods used for the classification of diseases using the health survey datasets containing phenotype data and national health survey datasets [86].
Discussion
The ML methods have been largely used to study different types of illness and in different kinds of datasets. The use of machine learning in the development of new treatments and interventions leads to the development of new drugs that can slow down the disease progression process [87]. The exponential increase in the use of machine learning in geriatric care is evidenced by the growing number of research studies in this field. There has been a significant number of published studies identified in the last decade and it’s growing day by day.
Machine learning is a relatively new technology in the field of geriatrics, and it has the potential to revolutionize the way we diagnose, treat, and manage geriatric diseases. In comparison to traditional methods, machine learning has several advantages that make it a promising tool for geriatric care. One of the most important advantages of ML is its ability to analyse a large amount of unstructured data like image data CT scans, MRI, tumor images, etc. It can find patterns and detect those morbidities quickly and more accurately [88,89,90]. While traditional methods rely on manual data analysis which is time-consuming and prone to human error, ML algorithms with their ability to learn and adapt, can be trained on large datasets and improve their accuracy over time [91]. In contrast, traditional methods rely on fixed rules and protocols that may not be able to adapt to the changing needs of geriatric patients. Machine learning algorithms can analyse patient data to identify those at high risk of developing a disease. This early identification can enable clinicians to intervene early and provide appropriate treatment to prevent or slow down the progression of the disease [92]. A paper by Ali et al. systematically reviewed 180 research articles according to the application of artificial intelligence in healthcare benefits, challenges, methodologies, and functionalities, which concluded that this novel method continues to outperform humans in terms of accuracy, efficiency, and fast execution of clinical processes [93]. Another systematic literature review by Battineni et al. suggested that in real-time clinical practice, there is no universally accepted approach for determining the optimal method, as each machine learning technique comes with its own set of strengths and limitations, however, Support Vector Machines (SVM) and Logistic Regression (LR) are two common machine learning methods that are used in most of the studies [94]. In another review article, the majority of the examined studies emphasized that the use of only machine learning methods or combining it with other intelligent techniques is popularly used to prevent emergencies [95]. This approach holds a significant promise for uncovering substantial patterns in both structured and unstructured datasets. The widespread adoption of these techniques generates curiosity about their global evolution and which countries utilize them most extensively. According to Tran et al., the trend of usage of machine learning and artificial intelligence in research is highest in the United States, followed by China and Italy [96]. Previous systematic literature studies have highlighted mostly clinical aspects of geriatrics and have only focused on chronic diseases [8, 10] and some have focused only on mental health disorders [9] or frailty [11]. The current study covers the total breadth of ageing from diseases to mental health problems and also the successful ageing, brain age, and biological age prediction. The study has also included literature which have used population-based surveys to build a successful ageing index by exploring new methods and datasets. Many kinds of digitally traced data [30, 46,47,48, 67, 69] are used in studies that have a future scope of application for improving geriatric research.
However, it is important to note that machine learning is not without its limitations. ML algorithms require large amounts of high-quality data to be effective, and there may be issues with data quality or bias that can impact the accuracy of the algorithms. Additionally, machine learning algorithms are not always transparent in their decision-making [97], which can make it difficult for clinicians to understand how the algorithms arrived at a particular diagnosis or treatment recommendation. So, in most cases, it may be suitable to use both the conventional methods and the ML methods side by side to get better results [98]. To summarize, machine learning offers several benefits in geriatric care such as its ability to rapidly and accurately analyse large amounts of data, learn and improve over time, and enhance the precision of diagnoses and treatment recommendations. However, it is crucial to acknowledge the potential limitations of machine learning and take necessary measures to ensure that the algorithms are fair, transparent, and validated before their implementation in clinical settings. The future scope of ML in geriatrics is vast and promising. With the aging population on the rise globally, there is a growing need for innovative technologies that can enhance the quality of care for the elderly. However, it is crucial to continue research and development to ensure that the algorithms are fair, transparent, and validated before their widespread implementation in clinical practice.
Conclusion
The current review found a wide variety of research papers analyzing different diseases using various machine learning algorithms in different kinds of datasets. Disease diagnostic criteria, risk prediction models, and factors were also highlighted and the application of machine learning in the field of geriatrics and care is well explored, but still, there is scope for future development. There is a need to validate that constructed machine learning models in large-scale datasets generalize the results across all age groups, gender, ethnicity, and other crucial factors. Also, there is a huge scope in using internet-based data and digital datasets from personalized applications in digital devices like smartphones and wearable technologies to provide customized patient-centric care for older populations.
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and Table- S1 of the supplementary information files].
References
Ageing and health. Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Cited 2023 Apr 28.
Constitution of the World Health Organization. Available from: https://www.who.int/about/governance/constitution. Cited 2023 Apr 28.
Nunes BP, Flores TR, Mielke GI, Thumé E, Facchini LA. Multimorbidity and mortality in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2016;67:130–8.
Longitudinal Ageing Study in India (LASI) | International Institute for Population Sciences (IIPS). Available from: https://www.iipsindia.ac.in/lasi. Cited 2023 Apr 28.
International AD, University M. World Alzheimer Report 2021: Journey through the diagnosis of dementia. 2021 Sep 21; Available from: https://www.alzint.org/resource/world-alzheimer-report-2021/. Cited 2023 Apr 28.
Pattnayak P, Panda AR. Innovation on Machine Learning in Healthcare Services—An Introduction. In: Tripathy HK, Mishra S, Mallick PK, Panda AR, editors. Technical Advancements of Machine Learning in Healthcare. Singapore: Springer; 2021. p. 1–30. (Studies in Computational Intelligence). Available from: https://doi.org/10.1007/978-981-33-4698-7_1. Cited 2023 Apr 28.
Machine learning, explained | MIT Sloan. Available from: https://mitsloan.mit.edu/ideas-made-to-matter/machine-learning-explained. Cited 2023 Apr 28.
Choudhury A, Renjilian E, Asan O. Use of machine learning in geriatric clinical care for chronic diseases: a systematic literature review. JAMIA Open. 2020;3(3):459–71. https://doi.org/10.1093/jamiaopen/ooaa034. Cited 2023 Oct 11.
Chowdhury M, Cervantes EG, Chan WY, Seitz DP. Use of Machine Learning and Artificial Intelligence Methods in Geriatric Mental Health Research Involving Electronic Health Record or Administrative Claims Data: A Systematic Review. Front Psychiatry. 2021;12. Available from: https://www.frontiersin.org/articles/https://doi.org/10.3389/fpsyt.2021.738466. Cited 2023 Oct 11.
Olender RT, Roy S, Nishtala PS. Application of machine learning approaches in predicting clinical outcomes in older adults – a systematic review and meta-analysis. BMC Geriatr. 2023;23(1):561. https://doi.org/10.1186/s12877-023-04246-w. (Cited 2023 Oct 11).
Leghissa M, Carrera Á, Iglesias CA. Machine learning approaches for frailty detection, prediction and classification in elderly people: A systematic review. Int J Med Inf. 2023;178:105172. Available from: https://www.sciencedirect.com/science/article/pii/S1386505623001909. Cited 2023 Oct 11.
Baecker L, Garcia-Dias R, Vieira S, Scarpazza C, Mechelli A. Machine learning for brain age prediction: Introduction to methods and clinical applications. eBioMedicine. 2021;72:103600. Available from: https://www.sciencedirect.com/science/article/pii/S2352396421003935. Cited 2023 Apr 8.
Fabris F, de Magalhães JP, Freitas AA. A review of supervised machine learning applied to ageing research. Biogerontology. 2017;18(2):171–88. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5350215/. Cited 2023 Apr 8.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;29:n160. Available from: https://www.bmj.com/lookup/doi/10.1136/bmj.n160. Cited 2023 Apr 21.
Kim I, Kim J. Comparison of biological age prediction models using clinical biomarkers commonly measured in clinical practice settings: ai techniques vs traditional statistical methods. Front Anal Sci. 2021;1:709589. Available from: https://www.frontiersin.org/articles/10.3389/frans.2021.709589. Cited 2023 Apr 8.
Joanna Briggs Institute. Joanna Briggs Institute Checklists. Available online: https://jbi.global/critical-appraisal-tools Accessed 24 Oct 2022.
Félix Caballero F, Soulis G, Engchuan W, Sánchez-Niubó A, Arndt H, Ayuso-Mateos JL, et al. Advanced analytical methodologies for measuring healthy ageing and its determinants, using factor analysis and machine learning techniques: the ATHLOS project. Sci Rep. 2017;10(7):43955. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5345043/. Cited 2023 Apr 8.
Qin FY, Lv Z, Wang DN, Hu B, Wu C. Health status prediction for the elderly based on machine learning. Arch Gerontol Geriatr. 2020;1(90):104121.
Engchuan W, Dimopoulos AC, Tyrovolas S, Caballero FF, Sanchez-Niubo A, Arndt H, et al. Sociodemographic indicators of health status using a machine learning approach and data from the english longitudinal study of aging (ELSA). Med Sci Monit Int Med J Exp Clin Res. 2019;25:1994–2001. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6436225/. Cited 2023 Apr 8.
Wong PH, Kourtit K, Nijkamp P. The ideal neighbourhoods of successful ageing: A machine learning approach. Health Place. 2021;72:102704. Available from: https://www.sciencedirect.com/science/article/pii/S1353829221002008. Cited 2023 Apr 8.
Huang CB, Hu JS, Tan K, Zhang W, Xu TH, Yang L. Application of machine learning model to predict osteoporosis based on abdominal computed tomography images of the psoas muscle: a retrospective study. BMC Geriatr. 2022;22(1):796.
Birks J, Bankhead C, Holt TA, Fuller A, Patnick J. Evaluation of a prediction model for colorectal cancer: retrospective analysis of 2.5 million patient records. Cancer Med. 2017;6(10):2453–60.
Sasani K, Catanese HN, Ghods A, Rokni SA, Ghasemzadeh H, Downey RJ, et al. Gait speed and survival of older surgical patient with cancer: prediction after machine learning. J Geriatr Oncol. 2019;10(1):120–5. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85049723929&doi=10.1016%2fj.jgo.2018.06.012&partnerID=40&md5=41cbcadb8cd6d3791b217c7c3c9a6d0f.
van den Bosch T, Warps ALK, de Nerée Tot Babberich MPM, Stamm C, Geerts BF, Vermeulen L, et al. Predictors of mortality among dutch patients undergoing colorectal cancer surgery. JAMA Netw Open. 2021;4(4):e217737.
Tseng RMWW, Rim TH, Shantsila E, Yi JK, Park S, Kim SS, et al. Validation of a deep-learning-based retinal biomarker (Reti-CVD) in the prediction of cardiovascular disease: data from UK Biobank. BMC Med. 2023;21(1):28.
Huang W, Ying TW, Chin WLC, Baskaran L, Marcus OEH, Yeo KK, et al. Application of ensemble machine learning algorithms on lifestyle factors and wearables for cardiovascular risk prediction. Sci Rep. 2022;12(1):1033.
Sajid MR, Almehmadi BA, Sami W, Alzahrani MK, Muhammad N, Chesneau C, et al. Development of nonlaboratory-based risk prediction models for cardiovascular diseases using conventional and machine learning approaches. Int J Environ Res Public Health. 2021;18(23):12586.
Kobayashi M, Huttin O, Magnusson M, Ferreira JP, Bozec E, Huby AC, et al. Machine learning-derived echocardiographic phenotypes predict heart failure incidence in asymptomatic individuals. JACC Cardiovasc Imaging. 2022;15(2):193–208.
Barbieri S, Mehta S, Wu B, Bharat C, Poppe K, Jorm L, et al. Predicting cardiovascular risk from national administrative databases using a combined survival analysis and deep learning approach. Int J Epidemiol. 2022;51(3):931–44.
Ghazal TM, Abbas S, Munir S, Khan MA, Ahmad M, Issa GF, et al. Alzheimer disease detection empowered with transfer learning. Comput Mater Contin. 2022;70(3):5005–19. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85117032728&doi=10.32604%2fcmc.2022.020866&partnerID=40&md5=d55bd08f1a9409d2027fe76173e9c0d4.
Li X, Bian D, Yu J, Li M, Zhao D. Using machine learning models to improve stroke risk level classification methods of China national stroke screening. BMC Med Inform Decis Mak. 2019;19(1):261.
Moradifar P, Amini H, Amiri MM. Hyperglycemia screening based on survey data: an international instrument based on WHO STEPs dataset. BMC Endocr Disord. 2022;22(1):316.
Chen Y, Duan W, Sehrawat P, Chauhan V, Alfaro FJ, Gavrieli A, et al. Improved perfusion pattern score association with type 2 diabetes severity using machine learning pipeline: pilot study. J Magn Reson Imaging JMRI. 2019;49(3):834–44.
Mansoori A, Sahranavard T, Hosseini ZS, Soflaei SS, Emrani N, Nazar E, et al. Prediction of type 2 diabetes mellitus using hematological factors based on machine learning approaches: a cohort study analysis. Sci Rep. 2023;13(1):663.
Lai H, Huang H, Keshavjee K, Guergachi A, Gao X. Predictive models for diabetes mellitus using machine learning techniques. BMC Endocr Disord. 2019;19(1):101.
Li R, Rueschman M, Gottlieb DJ, Redline S, Sofer T. A composite sleep and pulmonary phenotype predicting hypertension. EBioMedicine. 2021;68:103433.
Zhong X, Yu J, Jiang F, Chen H, Wang Z, Teng J, et al. A risk prediction model based on machine learning for early cognitive impairment in hypertension: Development and validation study. Front Public Health. 2023;11:1143019.
Sun JY, Ma YX, Liu HL, Qu Q, Cheng C, Kong XQ, et al. High waist circumference is a risk factor of new-onset hypertension: evidence from the China health and retirement longitudinal study. J Clin Hypertens Greenwich Conn. 2022;24(3):320–8.
AlKaabi LA, Ahmed LS, Al Attiyah MF, Abdel-Rahman ME. Predicting hypertension using machine learning: findings from Qatar biobank study. PLoS ONE. 2020;15(10):e0240370.
Alghafees MA, Abdul Rab S, Aljurayyad AS, Alotaibi TS, Sabbah BN, Seyam RM, et al. A retrospective cohort study on the use of machine learning to predict stone-free status following percutaneous nephrolithotomy: an experience from Saudi Arabia. Ann Med Surg. 2012;2022(84):104957.
Jadlowiec CC, Thongprayoon C, Leeaphorn N, Kaewput W, Pattharanitima P, Cooper M, et al. Use of machine learning consensus clustering to identify distinct subtypes of kidney transplant recipients with DGF and associated outcomes. Transpl Int Off J Eur Soc Organ Transplant. 2022;35:10810.
Sabanayagam C, Xu D, Ting DSW, Nusinovici S, Banu R, Hamzah H, et al. A deep learning algorithm to detect chronic kidney disease from retinal photographs in community-based populations. Lancet Digit Health. 2020;2(6):e295-302.
Cho SE, Geem ZW, Na KS. Development of a suicide prediction model for the elderly using health screening data. Int J Environ Res Public Health. 2021;18(19):10150.
Kasthurirathne SN, Biondich PG, Grannis SJ, Purkayastha S, Vest JR, Jones JF. Identification of patients in need of advanced care for depression using data extracted from a statewide health information exchange: a machine learning approach. J Med Internet Res. 2019;21(7):e13809.
Zhang A, Zhai S, Liu X, Song G, Feng Y. Investigating the association between streetscapes and mental health in Zhanjiang, China: Using Baidu street view images and deep learning. Int J Environ Res Public Health. 2022;19(24):16634.
Opoku Asare K, Terhorst Y, Vega J, Peltonen E, Lagerspetz E, Ferreira D. Predicting depression from smartphone behavioral markers using machine learning methods, hyperparameter optimization, and feature importance analysis: exploratory study. JMIR MHealth UHealth. 2021;9(7):e26540.
Ewbank MP, Cummins R, Tablan V, Bateup S, Catarino A, Martin AJ, et al. Quantifying the association between psychotherapy content and clinical outcomes using deep learning. JAMA Psychiat. 2020;77(1):35–43.
Guntuku SC, Schneider R, Pelullo A, Young J, Wong V, Ungar L, et al. Studying expressions of loneliness in individuals using twitter: an observational study. BMJ Open. 2019;9(11):e030355.
Helbich M, Yao Y, Liu Y, Zhang J, Liu P, Wang R. Using deep learning to examine street view green and blue spaces and their associations with geriatric depression in Beijing. China Environ Int. 2019;126:107–17.
Kim H, Lim DH, Kim Y. Classification and prediction on the effects of nutritional intake on overweight/obesity, dyslipidemia, hypertension and type 2 diabetes mellitus using deep learning model: 4–7th Korea national health and nutrition examination survey. Int J Environ Res Public Health. 2021;18(11):5597.
Sone D, Beheshti I, Shinagawa S, Niimura H, Kobayashi N, Kida H, et al. Neuroimaging-derived brain age is associated with life satisfaction in cognitively unimpaired elderly: a community-based study. Transl Psychiatry. 2022;12(1):25. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85123182065&doi=10.1038%2fs41398-022-01793-5&partnerID=40&md5=f58a8e67c66cb372909ffc9fdf060e4f.
Byeon H. Predicting the anxiety of patients with alzheimer’s dementia using boosting algorithm and data-level approach. Int J Adv Comput Sci Appl. 2021;12(3):107–13. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85104023644&doi=10.14569%2fIJACSA.2021.0120313&partnerID=40&md5=3e8889c1fbf90dda850c3e79afdbe32d.
Mahajan A, Deonarine A, Bernal A, Lyons G, Norgeot B. Developing the total health profile, a generalizable unified set of multimorbidity risk scores derived from machine learning for broad patient populations: retrospective cohort study. J Med Internet Res. 2021;23(11):e32900.
Spooner A, Chen E, Sowmya A, Sachdev P, Kochan NA, Trollor J, et al. A comparison of machine learning methods for survival analysis of high-dimensional clinical data for dementia prediction. Sci Rep. 2020;10(1):20410.
Tan WY, Hargreaves C, Chen C, Hilal S. A Machine learning approach for early diagnosis of cognitive impairment using population-based data. J Alzheimers Dis JAD. 2023;91(1):449–61.
Hu M, Shu X, Yu G, Wu X, Välimäki M, Feng H. A risk prediction model based on machine learning for cognitive impairment among chinese community-dwelling elderly people with normal cognition: development and validation study. J Med Internet Res. 2021;23(2):e20298.
Fukunishi H, Nishiyama M, Luo Y, Kubo M, Kobayashi Y. Alzheimer-type dementia prediction by sparse logistic regression using claim data. Comput Methods Programs Biomed. 2020;196:105582.
Shi F, He Y, Chen Y, Yin X, Sha X, Wang Y. Comparative analysis of multiple neurodegenerative diseases based on advanced epigenetic aging brain. Front Genet. 2021;12:657636.
Liang S, Gu Y. Computer-aided diagnosis of alzheimer’s disease through weak supervision deep learning framework with attention mechanism. Sensors. 2020;21(1):220.
Szlejf C, Batista AFM, Bertola L, Lotufo PA, Benseãor IM, Chiavegatto Filho ADP, et al. Data-driven decision making for the screening of cognitive impairment in primary care: a machine learning approach using data from the ELSA-Brasil study. Braz J Med Biol Res Rev Bras Pesqui Medicas E Biol. 2023;56:e12475.
Benhamou E, Zhao S, Sivasathiaseelan H, Johnson JCS, Requena-Komuro MC, Bond RL, et al. Decoding expectation and surprise in dementia: the paradigm of music. Brain Commun. 2021;3(3):fcab173.
Ithapu V, Singh V, Lindner C, Austin BP, Hinrichs C, Carlsson CM, et al. Extracting and summarizing white matter hyperintensities using supervised segmentation methods in Alzheimer’s disease risk and aging studies. Hum Brain Mapp. 2014;35(8):4219–35.
Gharbi-Meliani A, Husson F, Vandendriessche H, Bayen E, Yaffe K, Bachoud-Lévi AC, et al. Identification of high likelihood of dementia in population-based surveys using unsupervised clustering: a longitudinal analysis. MedRxiv Prepr Serv Health Sci. 2023;17:23286078.
Ford E, Rooney P, Oliver S, Hoile R, Hurley P, Banerjee S, et al. Identifying undetected dementia in UK primary care patients: a retrospective case-control study comparing machine-learning and standard epidemiological approaches. BMC Med Inform Decis Mak. 2019;19(1):248.
Casanova R, Saldana S, Lutz MW, Plassman BL, Kuchibhatla M, Hayden KM. Investigating predictors of cognitive decline using machine learning. J Gerontol B Psychol Sci Soc Sci. 2020;75(4):733–42.
Aguayo GA, Zhang L, Vaillant M, Ngari M, Perquin M, Moran V, et al. Machine learning for predicting neurodegenerative diseases in the general older population: a cohort study. BMC Med Res Methodol. 2023;23(1):8.
Oscar N, Fox PA, Croucher R, Wernick R, Keune J, Hooker K. Machine learning, sentiment analysis, and tweets: an examination of alzheimer’s disease stigma on twitter. J Gerontol Ser B. 2017;72(5):742–51. https://doi.org/10.1093/geronb/gbx014. (Cited 2023 Apr 8).
König A, Mallick E, Tröger J, Linz N, Zeghari R, Manera V, et al. Measuring neuropsychiatric symptoms in patients with early cognitive decline using speech analysis. Eur Psychiatry J Assoc Eur Psychiatr. 2021;64(1):e64.
Prange A, Sonntag D. Modeling users’ cognitive performance using digital pen features. Front Artif Intell. 2022;5:787179.
Younan D, Petkus AJ, Widaman KF, Wang X, Casanova R, Espeland MA, et al. Particulate matter and episodic memory decline mediated by early neuroanatomic biomarkers of Alzheimer’s disease. Brain J Neurol. 2020;143(1):289–302.
Aschwanden D, Aichele S, Ghisletta P, Terracciano A, Kliegel M, Sutin AR, et al. Predicting cognitive impairment and dementia: a machine learning approach. J Alzheimers Dis JAD. 2020;75(3):717–28.
Noh B, Yoon H, Youm C, Kim S, Lee M, Park H, et al. Prediction of decline in global cognitive function using machine learning with feature ranking of gait and physical fitness outcomes in older adults. Int J Environ Res Public Health. 2021;18(21):11347.
Jia Y, Chang CCH, Hughes TF, Jacobsen E, Wang S, Berman SB, et al. Predictors of dementia in the oldest old: a novel machine learning approach. Alzheimer Dis Assoc Disord. 2020;34(4):325–32.
de la Fuente GS, Ritchie CW, Luz S. Protocol for a conversation-based analysis study: PREVENT-ED investigates dialogue features that may help predict dementia onset in later life. BMJ Open. 2019;9(3):e026254.
Liu H, Zhang X, Liu H, Chong ST. Using machine learning to predict cognitive impairment among middle-aged and older Chinese: a longitudinal study. Int J Public Health. 2023;68:1605322.
Elgammal YM, Zahran MA, Abdelsalam MM. A new strategy for the early detection of alzheimer disease stages using multifractal geometry analysis based on K-Nearest Neighbor algorithm. Sci Rep. 2022;12(1):22381. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85144637119&doi=10.1038%2fs41598-022-26958-6&partnerID=40&md5=b9e22d812594decad3547073288678f7.
Sountharrajan S, Karthiga M, Suganya E. Alzheimer’s dementia: diagnosis and prognosis using neuro-imaging analysis. J Pharm Negat Results. 2022;13(4):46–63. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85143265988&doi=10.47750%2fpnr.2022.13.04.006&partnerID=40&md5=03ddefd038a81740e1c4cd05e1d075ef.
Toshkhujaev S, Lee KH, Choi KY, Lee JJ, Kwon GR, Gupta Y, et al. Classification of alzheimer’s disease and mild cognitive impairment based on cortical and subcortical features from MRI T1 brain images utilizing four different types of datasets. J Healthc Eng. 2020;2020:3743171. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85091264573&doi=10.1155%2f2020%2f3743171&partnerID=40&md5=eefc1596720714035adaddaf6f3e5f11.
Li Q, Yang MQ. Comparison of machine learning approaches for enhancing Alzheimer’s disease classification. PeerJ. 2021;9:e10549. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85101945960&doi=10.7717%2fpeerj.10549&partnerID=40&md5=655c6627de8dfc28dfc5bab48146c967.
Romero-Rosales BL, Tamez-Pena JG, Nicolini H, Moreno-Treviño MG, Trevino V. Improving predictive models for Alzheimer’s disease using GWAS data by incorporating misclassified samples modeling. PLoS ONE. 2020;15(4):e0232103. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85083712621&doi=10.1371%2fjournal.pone.0232103&partnerID=40&md5=74d4d214f0a872c3d98fb4e7b6db5d87.
Wang X, Ezeana CF, Wang L, Puppala M, Huang YS, He Y, et al. Risk factors and machine learning model for predicting hospitalization outcomes in geriatric patients with dementia. Alzheimers Dement Transl Res Clin Interv. 2022;8(1):e12351. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85145068383&doi=10.1002%2ftrc2.12351&partnerID=40&md5=c4d89d07520a4e000e7190c4bb84f560.
Tsang G, Zhou SM, Xie X. Modeling large sparse data for feature selection: hospital admission predictions of the dementia patients using primary care electronic health records. IEEE J Transl Eng Health Med. 2021;9:3000113. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85097206582&doi=10.1109%2fJTEHM.2020.3040236&partnerID=40&md5=048f1f807e0e682b4b6ea0164ba480b5.
Revathi A, Kaladevi R, Ramana K, Jhaveri RH, Rudra Kumar M, Sankara Prasanna kumar M. Early detection of cognitive decline using machine learning algorithm and cognitive ability test. Secur Commun Netw. 2022;2022:1–3. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85124127210&doi=10.1155%2f2022%2f4190023&partnerID=40&md5=9c474cc977ca4c53dad2cd79c9f2eb9b.
Cooray U, Watt RG, Tsakos G, Heilmann A, Hariyama M, Yamamoto T, et al. Importance of socioeconomic factors in predicting tooth loss among older adults in Japan: evidence from a machine learning analysis. Soc Sci Med. 2021;291:114486. Available from: https://www.sciencedirect.com/science/article/pii/S0277953621008182. Cited 2023 Apr 8.
Threats I of M (US) F on M. Detection and Diagnostics. In: Global Infectious Disease Surveillance and Detection: Assessing the Challenges—Finding Solutions, Workshop Summary. National Academies Press (US); 2007. Available from: https://www.ncbi.nlm.nih.gov/books/NBK52875/. Cited 2023 Apr 30.
Moreno-Ibarra MA, Villuendas-Rey Y, Lytras MD, Yáñez-Márquez C, Salgado-Ramírez JC. Classification of diseases using machine learning algorithms: a comparative study. Mathematics. 2021;9(15):1817. Available from: https://www.mdpi.com/2227-7390/9/15/1817. Cited 2023 Apr 30.
Dara S, Dhamercherla S, Jadav SS, Babu CM, Ahsan MJ. Machine learning in drug discovery: a review. Artif Intell Rev. 2022;55(3):1947–99. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8356896/. Cited 2023 Apr 30.
Rana M, Bhushan M. Machine learning and deep learning approach for medical image analysis: diagnosis to detection. Multimed Tools Appl. 2022 Dec 24; https://doi.org/10.1007/s11042-022-14305-w. Cited 2023 Apr 30.
Willemink MJ, Koszek WA, Hardell C, Wu J, Fleischmann D, Harvey H, et al. Preparing medical imaging data for machine learning. Radiology. 2020;295(1):4–15. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7104701/. Cited 2023 Apr 30.
Tchito Tchapga C, Mih TA, Tchagna Kouanou A, Fozin Fonzin T, Kuetche Fogang P, Mezatio BA, et al. Biomedical Image classification in a big data architecture using machine learning algorithms. J Healthc Eng. 2021;2021:e9998819. Available from: https://www.hindawi.com/journals/jhe/2021/9998819/. Cited 2023 Apr 30.
Evaluating Similarities and Differences between Machine Learning and Traditional Statistical Modeling in Healthcare Analytics | IntechOpen. Available from: https://www.intechopen.com/chapters/82063. Cited 2023 Apr 30.
Schaefer J, Lehne M, Schepers J, Prasser F, Thun S. The use of machine learning in rare diseases: a scoping review. Orphanet J Rare Dis. 2020;15(1):145. https://doi.org/10.1186/s13023-020-01424-6. (Cited 2023 Apr 30).
Ali O, Abdelbaki W, Shrestha A, Elbasi E, Alryalat MAA, Dwivedi YK. A systematic literature review of artificial intelligence in the healthcare sector: benefits, challenges, methodologies, and functionalities. J Innov Knowl. 2023;8(1):100333. Available from: https://www.sciencedirect.com/science/article/pii/S2444569X2300029X. Cited 2023 Oct 19.
Battineni G, Sagaro GG, Chinatalapudi N, Amenta F. Applications of machine learning predictive models in the chronic disease diagnosis. J Pers Med. 2020;10(2):21. Available from: https://www.mdpi.com/2075-4426/10/2/21. Cited 2023 Oct 19.
Priya RL, Jinny SV. Elderly healthcare system for chronic ailments using machine learning techniques – a review. Iraqi J Sci. 2021;31:38–51. Available from: https://ijs.uobaghdad.edu.iq/index.php/eijs/article/view/3135. Cited 2023 Oct 19.
Tran BX, Vu GT, Ha GH, Vuong QH, Ho MT, Vuong TT, et al. Global evolution of research in artificial intelligence in health and medicine: a bibliometric study. J Clin Med. 2019;8(3):360. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6463262/. Cited 2023 Oct 19.
Sanchez-Martinez S, Camara O, Piella G, Cikes M, González-Ballester MÁ, Miron M, et al. Machine learning for clinical decision-making: challenges and opportunities in cardiovascular imaging. Front Cardiovasc Med. 2022;8:765693. Available from: https://www.frontiersin.org/articles/10.3389/fcvm.2021.765693. Cited 2023 Apr 30.
Ahmad GN, Fatima H, Abbas M, Rahman O, Imdadullah MS, et al. Mixed machine learning approach for efficient prediction of human heart disease by identifying the numerical and categorical features. Appl Sci. 2022;12(15):7449. Available from: https://www.mdpi.com/2076-3417/12/15/7449. Cited 2023 Apr 30.
Acknowledgements
The authors are grateful to the researchers who have produced such informative articles (used in this review) and made those available on the internet.
Funding
We did not receive any grants from any funding agency in public, commercial, or non-profit sectors for conducting this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the manuscript. AD and PD have contributed to the conception, design and interpretation of the results. They drafted and critically revised the manuscript. All have contributed toward analysis of the papers and reviewing the manuscript. Moreover, all authors read, revised and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Since we have not used any dataset, there is no need for ethical clearance. The manuscripts didn’t need any report experiments involving the use of human embryos and gametes, human embryonic stem cells, and related materials. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1
. Research papers included in the review. Table S2. Risk of bias assessed by Joanna Briggs Institute (JBI) Critical Appraisal Tools.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Das, A., Dhillon, P. Application of machine learning in measurement of ageing and geriatric diseases: a systematic review. BMC Geriatr 23, 841 (2023). https://doi.org/10.1186/s12877-023-04477-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04477-x