Abstract
Background
Grassroots medical institutions are the primary “battlefield” of hypertension management based on hierarchical diagnosis and treatment policies in China. There is a considerable difference in the insured population and reimbursement ratio between different medical insurance programs. The management of hypertension directly affects the development trend of cardiovascular and cerebrovascular diseases.
Methods
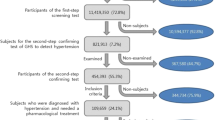
To understand the difference between different medical insurance programs regarding the management of older hypertensive patients, all outpatients aged 60 and above with hypertension in the basic medical insurance database of Beijing, China, from April 1, 2019, to January 31, 2020, were included. Medical behaviours included patients’ choice of hospital level, type of hospital, number of hospitals visited, grassroots medical institutions and cross-district visits. Medication adherence was evaluated by calculating the medication possession ratio of antihypertensive medications. First, we adopted a statistical description for medical behaviours and medication adherence. Then, multivariate logistic regression was used to analyse the influencing factors of medication adherence.
Results
This study included 1.29 million patients with Urban Employee Basic Medical Insurance (UEBMI) and 0.31 million patients with Urban‒Rural Resident Basic Medical Insurance (URRBMI). The proportions of patients with UEBMI who chose tertiary hospitals, comprehensive hospitals, grassroots medical institutions and cross-district visits were 25.84%, 56.09%, 57.34% and 39.32%, respectively, while those of patients with URRBMI were 11.14%, 60.59%, 81.28% and 6.07%, respectively. The medication adherence rates of men and women taking one medication were 61.04% and 55.86%, respectively. UEBMI patients who took their medication accounted for 62.36%, while only 40.27% of URRBMI patients adhered to their medication. The percentages of young-old, old-old and oldest-old patients who took their antihypertensive medications were 58.05%, 59.09% and 56.78%, respectively. The adherence to taking ≥ 2 medications (35.47%) was lower than that to taking one medication (58.33%). The medication adherence rates of patients with UEBMI and URRBMI for taking ≥ 2 medications were 37.21% and 27.45%, respectively.
Conclusions
Patients with UEBMI were more inclined to choose tertiary hospitals and cross-district visits than patients with URRBMI. The adherence of patients with UEBMI was better than that of patients with URRBMI in China.
Similar content being viewed by others
Introduction
The pace of population ageing is much faster than in the past, and the challenge of ensuring the health and social systems of older individuals during this demographic transition is experienced worldwide, as reported by the World Health Organization (WHO) [1]. Due to the absolute size of China’s older population (by 2020, the number of people aged 65 and above reached 190 million, accounting for 13.5% [2]), rapid development, lower life expectancy per capita than that of developed countries, an enormous gap between the supply and demand of older care, and unbalanced urban‒rural and regional development, China’s population ageing status is severe and faces more complex problems.
Hypertension in older people is a major factor that endangers survival and quality of life. Active treatment can substantially reduce the risk of moderate and major cardiovascular stroke events. In 2019, more than 1 billion people suffered from hypertension (82% of all hypertensive patients worldwide) in low-income and middle-income areas [3]. According to the Chinese Cardiovascular Health and Disease Report 2019 released by the Chinese Cardiovascular Center, the number of Chinese adult hypertensive patients reached 245 million. Among them, the prevalence of hypertension in Beijing was 35.9%, ranking first in the country [4]. Hypertension is relatively common in China, and its prevalence is increasing yearly, but it has not been fully controlled [5].
In 2015, China issued the Guiding Opinions of the General Office of the State Council on Promoting the Construction of a Hierarchical Diagnosis and Treatment System [6], which required that the pilot work of hierarchical diagnosis and treatment of chronic diseases such as hypertension be performed well. Hierarchical diagnosis and treatment refers to grading according to the priority of the disease and the difficulty of treatment. The framework of the hierarchical diagnosis and treatment system includes a community first diagnosis model, two-way referrals, urgent and timely treatment, and linkage between upper and lower levels. The first consultation at the grassroots level is to adhere to the principle of voluntary participation by the masses and encourage patients with common and frequently occurring diseases to seek medical treatment at grassroots medical institutions through policy guidance. Grassroots medical institutions are the primary “ battlefield” of hypertension management, and the management of hypertension directly affects the development trend of cardiovascular and cerebrovascular diseases in China. Compared with other cities in China, Beijing is a large city with high-quality medical resources, and the behaviours of older hypertensive patients in Beijing are worth studying.
It has been estimated that 33 ~ 69% of medication-related hospitalizations in the United States are due to poor medication adherence, with an annual cost of $100 billion [7]. For hypertension, the higher the adherence to treatment is, the lower the risk of hospitalization [8]. Treatment adherence is currently recognized as the key to effective antihypertensive treatment. However, adherence is often ignored in the management of hypertension. The reason is that there is no uniform standard and extremely complex methods of adherence assessment in clinical practice, as well as limitations in clinical practice [9]. Poor medication adherence undermines the expectation of medication treatment and increases the risk of occurrence and development of cardiovascular and cerebrovascular diseases and kidney diseases. Existing evidence shows that up to 90% of hypertensive patients may not insist on treatment, and approximately 50% may stop treatment within one year after diagnosis [10].
There are few studies on the medical behaviours of middle-aged and older hypertensive patients in China. Their data are from sample surveys, which do not reflect the overall situation of a city or region, and the sample size is within 5000 cases [11,12,13]. There are studies on medication adherence among hypertensive patients from Beijing [14], Shanghai [15], Shanxi [16], Hunan [17], Shaanxi [18] and Hong Kong [19] in China in which patients self-reported their adherence based on a scale. However, there is little research on the results of medication adherence among older hypertensive patients in China. Only the China Health and Retirement Longitudinal Study (CHARLS) in 2015 [20] evaluated the adherence of middle-aged and older hypertensive patients, and a survey based on a scale from Jiangsu [21] evaluated the adherence of older patients to antihypertensive medications in China.
There is a considerable difference in the insured population and reimbursement ratio between different medical insurance programs. Therefore, to understand the difference between different medical insurance programs for the management of older hypertensive patients in China, this study used a large number of claims data to study the medical behaviours and medication adherence of hypertensive patients aged 60 and above to improve the survival and quality of life of older hypertensive patients.
Methods
Data and subjects
This study was based on the “Study on the technical standard of capitation for chronic diseases” of the Beijing Medical Insurance Bureau. All outpatients aged 60 and above with hypertension in the basic medical insurance database of Beijing from April 1, 2019, to January 31, 2020, were included. The data were deidentified before analysis.
Definition
Patient characteristics. According to the WHO age classification standard for older people [22, 23], young-old people are 60 ~ 74 years old, old-old people are 75 ~ 89 years old, and oldest-old people are 90 years old and above. Sex was a binary variable. Medical insurance included 2 major health insurance schemes in China: Urban Employee Basic Medical Insurance (UEBMI) and Urban‒Rural Resident Basic Medical Insurance (URRBMI). The people who participate in UEBMI are mainly employees, including employees of companies, government agencies, public institutions, social organizations, and private noncompany workplaces. The reimbursement ratio for outpatient (emergency) consultations of in-service employees in Beijing has reached 70%, and that for retirees has reached 85%. The reimbursement ratio of community hospitals is 90%. Regarding outpatient reimbursements of over 20,000 Chinese yuan, if medical expenses are incurred again, 60% is reimbursed for in-service employees and 80% for retirees, with no upper limit. The people who participate in URRBMI are mainly urban and rural residents without workplaces. During a medical insurance year, 55% of outpatient (emergency) consultations for urban and rural residents covered by URRBMI are reimbursed at level 1 or below hospitals, and 50% are reimbursed at level 2 and level 3 hospitals; the upper limit is 4500 Chinese yuan.
Medical behaviours. Grassroots medical institutions in China include community health service centres (stations), outpatient departments, clinics, health centres (rooms), infirmaries, nursing stations, student health care centres, and village health rooms. In this study, we set grassroots medical institutions as a binary variable (whether a doctor was seen in a grassroots medical institution). Hospital levels included level 3, level 2, level 1 and no level, whereby the higher the level was, the larger the scale of the hospital. Type of hospital was divided into comprehensive hospitals, traditional Chinese medicine hospitals, specialized hospitals and community hospitals. There are 16 districts in Beijing. If the patient did not visit the hospital in their residential district, it was defined as a cross-district visit (binary: yes or no). The number of hospitals visited during the observation period was set as a categorical variable: 1, 2 and ≥ 3. Multiple visits from the same hospital counted as one.
Medication adherence. Since there are no gold standard methods for adherence evaluation, this study used claims data with low measurement costs to calculate adherence to antihypertensive medications. We used the medication possession ratio (MPR) to analyse adherence to antihypertensive medications, which was defined as the sum of all supply days of antihypertensive medications divided by the days during the observation period (from the first prescription to the last prescription) [24]. The patient had at least 3 outpatient visits and antihypertensive medication prescription records. When we calculated the total supply days of medications, the last outpatient visit was excluded. Antihypertensive medications were divided into five categories: thiazide diuretics, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs) and beta blockers. We estimated the medication adherence of each type of antihypertensive medication. When calculating the MPR of patients taking ≥ 2 medications, the numerator was the cumulative maximum supply days of medications per visit excluding the last visit, and the denominator remained unchanged. If the MPR was greater than or equal to 0.8, the patient was considered adherent; otherwise, the patient was considered nonadherent [25, 26].
Statistical analysis
Since it is easy to obtain significant differences using a large sample, we applied a statistical description to show the difference. Multivariate logistic regression was used to analyse the influencing factors, including sex, age, medical insurance program and medical behaviours, for adherence (binary: adherent and nonadherent), where the first visit in our observation time was selected for medical behaviours except for the number of hospitals visited. Odds ratios (ORs) and their 95% confidence intervals (CIs) were obtained from logistic regression. A 95% CI that did not cross 1 indicated statistical significance (P < 0.05). Our methods were carried out in accordance with SAMPL guidelines. All analyses were performed with R (Version 4.2.1).
Results
Basic characteristics
This study included 1.6 million older hypertensive outpatients in Beijing, China, comprising 1.29 million patients with UEBMI and 0.31 million patients with URRBMI. Less than 50% of the hypertensive patients were older males. Most patients were young-old, while oldest-old patients accounted for 1.89%. Each patient had an average of 13.55 outpatient visits and 288.39 days of observation time in this study. The average medical expense of each outpatient visit was 511.05 Chinese yuan. The visits with antihypertensive medications accounted for 63.89% of outpatient visits, in which the number of medication prescriptions from highest to lowest was calcium channel blockers, ARBs, beta blockers, thiazide diuretics and ACE inhibitors. Table 1 shows information on patients with UEBMI and URRBMI.
Medical behaviours
Compared with URRBMI patients, UEBMI patients tended to choose tertiary hospitals. Regarding the type of hospital, URRBMI patients were slightly more likely to choose a comprehensive hospital. URRBMI patients were more likely to choose grassroots medical institutions, while UEBMI patients were more likely to choose cross-district visits (Table 2). See Table S1, Table S2 and Table S3 for medical behaviours of young-old, old-old, and oldest-old patients.
Medication adherence
Regarding adherence to antihypertensive medications, more than half of the older hypertensive patients took their medications. The proportion of UEBMI patients with medication adherence was far higher than that of URRBMI patients, the proportion of males was higher than that of females, and the proportion of oldest-old patients was slightly lower than that of the other two age groups (Table 3). For those taking ≥ 2 antihypertensive medications, their medication adherence was much lower than that of those taking one medication, while differences in medication adherence between different groups were similar to those of the patients taking one medication (Table 4).
The MPRs of the five types of antihypertensive medications were different, whereby calcium channel blockers were the most common and beta blockers were the least common. Men generally had a higher MPR than women, UEBMI patients had a higher MPR than URRBMI patients, and oldest-old patients had a lower MPR than the other two age groups (Table 5).
Table 6 shows that there were differences in medication adherence to the five types of antihypertensive medications. Calcium channel blockers had the best adherence, which was 8.87% higher than the lowest adherence of beta blockers. The proportion of men with medication adherence was 3.29% higher than that of women on average. The proportion of UEBMI patients who were adherent to their antihypertensive medications was 15.46% higher than the proportion of URRBMI patients. There was no significant difference in the proportion of medication adherence among different age groups. In general, the proportion of patients aged 90 and above who adhered to their medication was smaller than that of the other two age groups.
For the five antihypertensive medications, the adherence of the old-old group was better or worse than that of the young-old group, but the adherence of the oldest-old group was worse than that of the young-old group. The type of medical insurance had the greatest impact on adherence. Patients who chose a tertiary hospital had higher adherence than those who did not. Patients who chose specialized hospitals and comprehensive hospitals had higher adherence than those who chose community hospitals, while patients who chose traditional Chinese medicine hospitals had lower adherence than those who chose community hospitals. Patients who chose grassroots medical institutions had higher adherence. The level of adherence of patients who chose a hospital outside of their district was inconsistent among the five types of antihypertensive medications (Table 7).
In general, sex, age, medical insurance program, and medical behaviours affected adherence. The more hospitals visited, the better the patients’ adherence. Regarding taking ≥ 2 antihypertensive medications, all factors except for age had statistical significance. The relationship between the number of hospitals visited and adherence was different among people taking one medication. In other words, these factors had different effects on people who took one medication and those who took ≥ 2 medications (Table 8).
Discussion
Based on claims data, this study analysed the medical behaviours and medication adherence of older hypertensive patients in Beijing, China, and revealed the current state of older hypertensive patients with different basic medical insurance schemes, providing a scientific basis for better management of hypertensive patients.
According to the Guiding Opinions of the General Office of the State Council on Promoting the Construction of a Hierarchical Diagnosis and Treatment System [6], grassroots medical institutions should provide medical services for patients with chronic diseases with a clear diagnosis and stable condition. The relevant national departments have successively issued preferential policies for the first diagnosis and reimbursement of chronic diseases at the grassroots level, aiming to further guide patients with chronic diseases to see doctors at the grassroots level. CHARLS showed that 57.63% of older people choose grassroots medical institutions when they visit a doctor in China [27]. In this study, 60.63% of older people with hypertension chose grassroots medical institutions for outpatient treatment. More than half of the older patients with hypertension chose comprehensive hospitals, and the proportion that chose tertiary hospitals was not low, which undoubtedly increases the burden on large hospitals crowded with visitors. It is necessary to further guide patients with chronic diseases such as hypertension to seek treatment in grassroots medical institutions. The proportion of UEBMI patients who chose tertiary hospitals and cross-district visits was higher than that of URRBMI patients, which may be related to the higher proportion of UEBMI reimbursement than that of URRBMI, indicating that the medical insurance policy has a great impact on patients’ medical behaviours. The difference between UEBMI and URRBMI patients aged 90 and above in choosing tertiary hospitals, grassroots medical institutions and cross-district visits was smaller than that of the other two age groups.
The medication adherence rates of hypertensive patients in China differ greatly. A survey from Beijing showed that 61.3% of 318 rural hypertensive patients had medication adherence, and 38.7% had no medication adherence [14]. A survey of outpatients in a hospital in Shanghai showed that 51.7% of the patients had high adherence to antihypertensive medications, 22.0% had moderate adherence, and 26.3% had low adherence [15]. A Hong Kong survey showed that 65.1% of patients had good adherence to antihypertensive medications, while 32.6% had poor adherence [19]. However, a survey in Jinzhong, Shanxi, showed that 21.3% of rural hypertensive patients insisted on taking medications, while 78.7% did not [16]. A survey in Changsha, Hunan, showed that 63.6% of hypertensive patients had low adherence, 29.5% had moderate adherence and 7.6% had high adherence [17]. According to a survey conducted at a hospital in Xi’an, Shaanxi, 27.46% of the patients complied with antihypertensive treatment [18]. The above medication adherence results were lower than the antihypertensive medication adherence results (75%) of Chinese immigrants to the United States [28].
With respect to the medication adherence of older patients with hypertension, a survey in Suzhou, Jiangsu, showed that 34.2% of older patients had good adherence to antihypertensive medications, while 65.8% had poor adherence [21]. The CHARLS showed that 77.2% of middle-aged and older hypertensive patients reported adherence to medication [20]. A systematic review showed that the self-reported medication adherence rate of hypertension patients over 60 years of age was 68.86%, and the adherence rate of patients in Western countries (e.g., Europe and the United States) was substantially higher than that of other patients [29]. Li et al. reported that the medication adherence of male and female older hypertensive patients who immigrated from China to the United States was 69% and 75%, respectively [30]. According to a survey by Hsu et al., 52% of older Chinese Americans insisted on taking antihypertensive medications [31]. These results on medication adherence vary greatly because of different measurement methods and samples. Their medication adherence results were based on self-reports, which is quite different from the calculation methods of this study. It is difficult to directly compare our rate of 58.33% among older hypertensive patients in Beijing with rates in other studies. Based on medical claims data, the results of sampling calculations from Manitoba, Canada, showed that 76.7% of hypertensive patients aged 65 or older were considered adherent when using the prescription-based MPR [32], which was higher than the adherence rate in this study. Our results showed that adherence to multiple medications was worse than adherence to only one medication. The reason may be that when the patient’s condition is severe, multiple antihypertensive medications are needed to control their blood pressure. Once their blood pressure is controlled, the patient may not want to take many medications, leading to poor adherence. This reveals that there is still much room for improvement in medication adherence in China. However, this study is the first to report the results of medication adherence among older patients with hypertension in a whole population of a city based on claims data in China, rather than a sampling survey. Our results are important for better management of older patients with hypertension.
Moreover, there were differences in medication adherence to different antihypertensive medications in this study. Calcium channel blockers have strong antihypertensive effects, good tolerance, no absolute contraindications, and a relatively wide range of applications. Calcium channel blockers are more suitable for simple systolic hypertension, which made adherence to them relatively high. The adherence to beta blockers was relatively low, which may be because the medication is mainly used in patients with a faster heart rate to lower it. The aggregated MPR and adherence rate were lower for multiple medications than for a single medication.
The difference between the two types of medical insurance populations led to differences in medication adherence. There are differences between men and women in the prevalence of hypertension, the effect of antihypertensive medications and the risk of side effects of antihypertensive medications [33], which may lead to differences in medication adherence between the sexes. The adherence of hypertension patients aged 90 and above is worse, which may be due to their own physical limitations. If there is someone to take care of these older patients, their medication adherence may improve.
Tertiary hospitals provide high-level specialized medical and health services in the region. Hospitals without a level have not been evaluated and graded, which can be a complex process, and these hospitals include both large and small hospitals. Compared with level 1 hospitals, patients may trust level 2 hospitals and no-level hospitals more, so their adherence was higher. Compared with community hospitals, patients in comprehensive hospitals and specialized hospitals may have higher adherence because they trust comprehensive hospitals and specialized hospitals more. The reason why the adherence of patients in traditional Chinese medicine hospitals was lower than that in community hospitals may be related to the nature of traditional Chinese medicine hospitals, as they can also prescribe these five antihypertensive medications. The reason for the higher adherence of patients who chose grassroots medical institutions may be that the patients’ condition was relatively stable, and the patients were clear about their needs, so they went directly to a grassroots medical institution that had few people and found it convenient to have medicine prescribed. The factors that affected the adherence of patients taking ≥ 2 medications were more complex. Compared to taking one medication, the factors that influenced the adherence of patients taking ≥ 2 medications had inconsistent effects. For example, the impact of age and medical insurance is decreasing. The role of number of hospitals visited is trending in the opposite direction. The reasons behind this are worth further investigation and research in the future.
Because we did not know the actual days or doses of patients taking medications, this study used the MPR to estimate medication adherence to antihypertensive medications, which may have overestimated the adherence of patients compared with the self-reported medication adherence evaluated by instruments such as the Morisky Medication Adherence Scale (MMAS). Some variables were not included in the establishment of the medical insurance database, such as income, which is an important factor that can affect patient medical behaviours and medication adherence, which is a limitation of this study. This was also a cross-sectional study that did not consider the patient’s first diagnosis of hypertension or subsequent disease development, thus ignoring the impact of the development of hypertension on medical adherence.
In summary, based on claims data, this study investigated the medical behaviours and medication adherence of older hypertensive patients in Beijing, China. Patients with UEBMI had a higher frequency of visits and higher average medical expenses per visit and were more inclined to choose tertiary hospitals and hospitals outside their district than patients with URRBMI. The adherence of patients with UEBMI was better than that of patients with URRBMI.
Data availability
The data used in the study is not publicly available, but the data used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
World Health Organization. Ageing and health. 2022.
National Bureau Of Statistics of China. China Statistical Yearbook 2021. Beijing: China Statistics Press; 2021.
Zhou B, Carrillo R, Danaei G, Riley L, Paciorek C, Stevens G, et al. Worldwide trends in Hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of Hypertension in China. Circulation. 2018;137:2344–56.
Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of Hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE million persons project). The Lancet. 2017;390:2549–58.
The State Council of the People’s Republic of China. Guiding Opinions of the General Office of the State Council on Promoting the Construction of a Hierarchical Diagnosis and Treatment System. 2015.
Osterberg L, Blaschke T. Adherence to Medication. N Engl J Med. 2005;353:487–97.
Sokol M, Mcguigan K, Verbrugge R, Epstein R. Impact of Medication Adherence on hospitalization risk and Healthcare cost. Med Care. 2005;43:521–30.
Poulter NR, Borghi C, Parati G, Pathak A, Toli D, Williams B, et al. Medication adherence in Hypertension. Journal of Hypertension; 2019.
He W, Bonner A, Anderson D. (2015). Patient reported adherence to Hypertension treatment: a revalidation study. Eur J Cardiovasc Nurs, 15.
Li J, Gao X, Lei X, Hu H. Influencing factors of Health-seeking behaviors in Primary Health Care Institutions among Middle-aged and aged patients with Hypertension:based on the Data of 2015 China Health and Retirement Longitudinal Study(CHARLS2015). Practical J Cardiac Cereb Pneumal Vascular Disease. 2020;28:89–93.
Feng L, Chen C, Hao X, Li S. Factors influencing on chronic Diseases in Community Elderly and their behaviors of receiving Medical Treatment and Drug Use. Chin Gen Pract. 2014;17:3477–9.
Jia H, Yuan S, Luo T. A cross-sectional study of elderly patients with Hypertension in Chongqing and suggestions for multidisciplinary diagnosis and treatment regimen. J Chongqing Med Univ. 2019;44:642–8.
Hu H, Li G, Arao T. (2013). Prevalence Rates of Self-Care Behaviors and Related Factors in a Rural Hypertension Population: A Questionnaire Survey. International Journal of Hypertension, 2013:526949.
Yue Z, Li C, Weilin Q, Bin W. (2015). Application of the Health Belief Model to improve the understanding of antihypertensive medication adherence among Chinese patients. Patient Educ Couns, 98.
Ma C. (2016). A cross-sectional survey of medication adherence and associated factors for rural patients with Hypertension. Appl Nurs Res, 31.
Shi S, Zhiying S, Duan Y, Ding S, Zhong Z. (2019). Association between Medication Literacy and Medication adherence among patients with Hypertension. Front Pharmacol, 10.
Pan J, Wu L, Wang H, Lei T, Hu B, Xue X, et al. Determinants of Hypertension treatment adherence among a Chinese population using the therapeutic adherence scale for hypertensive patients. Medicine. 2019;98:e16116.
Lee G, Wang H, Liu K, Cheung Y, Morisky D, Wong M. Determinants of Medication Adherence to Antihypertensive Medications among a Chinese Population using Morisky Medication Adherence Scale. PLoS ONE. 2013;8:e62775.
Liu J, Yang Y, Zhou J, Liu T, Zhang W, Wei L et al. (2020). Prevalence and Associated Factors of Compliance Behaviors among middle-aged and older hypertensive patients in China: results from the China Health and Retirement Longitudinal Study. Int J Environ Res Public Health, 17.
Hou Y, Zhang D, Gu J, Xue F, Sun Y, Wu Q, et al. The association between self-perceptions of aging and antihypertensive medication adherence in older Chinese adults. Aging Clinical and Experimental Research; 2016. p. 28.
Ahmad OB, Boschi Pinto C, Lopez A, Murray C, Lozano R, Inoue M. (2001). Age Standardization of Rates: A New WHO Standard. Gpe Discussion Paper Series, Eip/Gpe/Ebd, World Health Organization, No.31.
Wu F, Sheng Y. (2019). Differences in social isolation between young and old elderly in urban areas of Beijing, China: a cross-sectional study. Int J Nurs Sci, 7.
Andrade S, Kahler K, Frech F, Chan K. Methods for evaluation of Medication Adherence and Persistence using automated databases. Pharmacoepidemiol Drug Saf. 2006;15:565–74.
Peterson AM, Nau DP, Cramer JA, Benner J, Gwadry-Sridhar F, Nichol M. A Checklist for Medication Compliance and Persistence studies using Retrospective databases. Value in Health. 2007;10:3–12.
Hess L, Raebel M, Conner D, Malone D. Measurement of adherence in Pharmacy Administrative databases: a proposal for Standard definitions and Preferred measures. The Annals of Pharmacotherapy. 2006;40:1280–8.
Zeng Y, Wan Y, Yuan Z, Fang Y. Healthcare-seeking behavior among Chinese older adults: patterns and predictive factors. Int J Environ Res Public Health. 2021;18:2969.
Li W, Stewart A, Stotts N, Froelicher E. Cultural factors Associated with Antihypertensive Medication Adherence in Chinese immigrants. J Cardiovasc Nurs. 2006;21:354–62.
Uchmanowicz B, Jankowska E, Uchmanowicz I, Morisky D. (2019). Self-reported medication adherence measured with Morisky Medication Adherence scales and its determinants in hypertensive patients aged ≥ 60 years: a systematic review and Meta-analysis. Front Pharmacol, 10.
Li W, Wallhagen M, Froelicher E. Hypertension control, predictors for medication adherence and gender differences in older Chinese immigrants. J Adv Nurs. 2008;61:326–35.
Hsu Y, Mao C, Wey M. Antihypertensive medication adherence among Elderly Chinese americans. J Transcult Nurs. 2010;21:297–305.
Tang KL, Quan H, Rabi DM. Measuring medication adherence in patients with incident Hypertension: a retrospective cohort study. BMC Health Serv Res. 2017;17:135.
Gerdts E, Sudano I, Brouwers S, Borghi C, Bruno RM, Ceconi C, et al. Sex differences in arterial Hypertension. Eur Heart J. 2022;43:4777–88.
Acknowledgements
Not applicable.
Funding
This work was supported by The National Natural Science Foundation of China (72204169, 81825007), Beijing Outstanding Young Scientist Program (BJJWZYJH01201910025030), Capital’s Funds for Health Improvement and Research (2022-2-2045), National Key R&D Program of China (2022YFF1501500, 2022YFF1501501, 2022YFF1501502, 2022YFF1501503, 2022YFF1501504, 2022YFF1501505), Youth Beijing Scholar Program (010), Beijing Laboratory of Oral Health (PXM2021_014226_000041), Beijing Talent Project - Class A: Innovation and Development (2018A12), “National Ten-Thousand Talent Plan” - Leadership of Scientific and Technological Innovation, National Key R&D Program of China (2017YFC1307900, 2017YFC1307905).
Author information
Authors and Affiliations
Contributions
LL drafted the work and analyzed the data; PH acquired data; JL analyzed the data; RL interpreted the data; YW designed the work. All authors have read and approved the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was based on the project of “Study on the technical standard of capitation for chronic diseases” of Beijing Medical Insurance Bureau, and conducted in accordance with the Declaration of Helsinki. Beijing Medical Insurance Bureau granted permission to access the raw data used in this study and waived ethical approval for this project as it is administrative data. The data used in this study was anonymized before its use and this study does not report personal information. Therefore, informed consent has also been exempted.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary: Table S1
. Medical behaviors of hypertensive patients aged 60~74 in Beijing, China. Table S2. Medical behaviors of hypertensive patients aged 75~89 in Beijing, China. Table S3. Medical behaviors of hypertensive patients aged 90 or older in Beijing, China.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lan, L., Hai, P., Luo, J. et al. Medical behaviours and medication adherence of older hypertensive patients in different medical insurance programs in Beijing, China: a cross-sectional study. BMC Geriatr 23, 878 (2023). https://doi.org/10.1186/s12877-023-04476-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04476-y