Abstract
Background
Frailty increases the risks of hospitalization, injury, fall, psychological disorders, and death in older adults. Accurate estimation of the prevalence of frailty is crucial for promoting health in these individuals. Therefore, this study was conducted to estimate the prevalence of frailty and prefrailty in older adults residing in Indonesia.
Methods
In accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines, six electronic databases were searched (without any language restriction) for relevant articles from inception to February 2023. Studies on the prevalence of frailty and prefrailty in older adults (age ≥ 60 years) residing in Indonesia were included in the analysis. A random-effects model was selected a priori because of the expected high degree of heterogeneity in the study, followed by sensitivity analysis, subgroup analysis, and meta-regression. The protocol of this review study was registered in the PROSPERO database (CRD42022381132).
Results
A total of 79 studies were identified, of which 20 were finally included in the analysis. The pooled prevalence of frailty and prefrailty in older adults in Indonesia was 26.8% and 55.5%, respectively. The pooled prevalence of frailty and prefrailty was 37.9% and 44.8% in nursing homes, 26.3% and 61.4% in hospitals, and 21.1% and 59.6% in community settings, respectively. Furthermore, the pooled prevalence of frailty and prefrailty was 21.6% and 64.3%, 18.7% and 62%, and 27.8% and 59.8% in studies using the Frailty Index-40, FRAIL, and Fried Frailty Phenotype questionnaires, respectively. However, the parameters did not vary significantly across measurement tools or study settings. Publication bias was not detected while the year of data collection influenced the heterogeneity between the studies.
Conclusions
To the best of our knowledge, this study is the first meta-analysis to report the prevalence of frailty and prefrailty in older adults residing in Indonesia. The gradual increase in the number of older adults with frailty or prefrailty in Indonesia is concerning. Therefore, the government, private sectors, health-care professionals, and the community must jointly design effective strategies and policies to address this problem.
Similar content being viewed by others
Background
Frailty, a geriatric symptom, reduces older adults’ stress resistance and disturbs the body’s homeostatic balance. In addition, it reduces resistance to various harmful agents entering the body, elevates the risks of injury and immobility, and increases the rates of hospitalization and mortality in older adults [1]. Frailty is associated with several factors, such as age, sex, low education level, cohabitation (with family), comorbidities, polypharmacy, social isolation (limited engagement in activities outside the home), nonfunctional ambulation, and malnutrition [2].
The increase in the aging population worldwide is proportional to the incidence of degenerative and frailty-related diseases [3]. The estimated prevalence of frailty in the global population of older adults aged > 85 years is 25%–50%. However, the prevalence varies widely (range, 3%–47.2%) depending on age and sex. The prevalence of frailty varies across countries, with studies reporting the following prevalence percentages: China, 3.9%; Turkey, 39.2%; and Cuba, 51.4%. The prevalence of prefrailty also varies across countries, with studies reporting the following percentages: Tanzania, 13.4%; Turkey, 43.3%; and Brazil, 71.6% [2, 4]. In Singapore, which is the closest country to Indonesia, the prevalence of frailty in community-dwelling older adults is 5.7%–24.5% [5, 6]. In the countries neighboring Indonesia, such as Malaysia and Thailand, the prevalence of frailty in community-dwelling older adults is 8.9%–15.9% [7, 8] and 8.7%–22.1% [9, 10], respectively.
The modern world is facing an unprecedented challenge of aging populations. At least two-thirds of the global population of older adults reside in low-to-middle-income countries; the rate of population aging in these countries is expected to exceed the rate in high-income countries after 2025 [3]. The proportion of older adults in Indonesia increased to 10.7% (an increase of 5.2% over the last five decades) in 2020 and is projected to reach 19.9% by 2045 [11]. Concurrently, older adults’ health problems (e.g., frailty) have been increasing.
In Indonesia, the increase in the number and life expectancy of older adults has resulted in problems such as an increase in the number of older adults without any income who are forced to depend on others. The morbidity rate of such older adults in the community has been reported to be 25.05% [12]. In addition, the frailty condition experienced by older adults can exacerbate this burden on the community [13].
Indonesian have culturally strong family characteristics, this indirectly strengthens the social bond between older adults and their relatives. Social capital is one of the most important factors in strengthening biological and psychological perspectives in relation to the complexities of older adults’ health [5]. In the structure of Indonesian society, older adults are often considered a burden on society because they experience a decrease in intrinsic capacity such as physical, mental and cognitive capacity, thereby hampering functional abilities. The increasing number of vulnerable older adults can indirectly result in negative social and economic impacts on society [2]. Negative impacts that can occur include low community productivity, financial disruption, caregiver burden, and high costs of health services which could lead to a huge problem on the state [6].
Therefore, accurate country-specific prevalence data are essential for the implementation of priority interventions by the government and health workers to identify, manage, and prevent problems of related to the older population. To the best of our knowledge, no study has explored the prevalence of frailty in Indonesia. Therefore, this systematic review and meta-analysis was conducted to clarify the prevalence of frailty and prefrailty in older adults residing in Indonesia. Our findings regarding the overall prevalence of prefrailty and frailty in Indonesia may guide policies for reducing frailty-related problems in older adults.
Methods
Relevant articles were systematically identified in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [14]. The protocol of this review study was registered in the PROSPERO database (CRD42022381132).
Data sources and search strategy
PubMed, Cochrane Library, CINAHL, EMBASE, Ovid, and GARUDA web were searched (without any language restriction) for relevant articles from inception to November 2023. GARUDA web is an Indonesian science database containing Indonesian articles that have been published in Indonesian journals. The following Medical Subjective Heading terms were searched with an explosion function (if available): “frailty,” “prevalence,” or “epidemiology” and “Indonesia.” Articles containing a combination of the aforementioned keywords in the title and main text were retrieved. The year of publication was not limited because few studies have focused on frailty, particularly in Indonesia. No language restriction was imposed to avoid excluding articles likely to contribute positively to our analysis.
Selection criteria
The authors used the Population Intervention Comparison Outcomes (PICO) framework [15] as the basis for the method of the selection criteria as follows: (1) Population: the population was older adults aged > 60 years; (2) Intervention and Comparison were not included due to the prevalence study; and (3) Outcome: the reported outcome consists of frailty and/or prefrailty parameters. Studies on the prevalence of frailty and/or prefrailty in older adults (age ≥ 60 years) residing in the community, nursing homes or clinics, and hospitals in Indonesia were included. Studies involving older adults with comorbidities, and articles that were theses, abstract proceedings, literature reviews, editorials, and letters to the editor were excluded from our analysis. Two reviewers (AAP and SCL) screened the relevant articles on the basis of the inclusion and exclusion criteria.
Data extraction and methodological quality assessment
The following data were extracted by one reviewer (AAP) and independently confirmed by another reviewer (SCL): the participants (sample size and mean age), measurement tools (Fried frailty phenotype, Frailty Index-40 (FI-40) questionnaire, FRAIL questionnaire, Edmonton Frail Scale (EFS), and Survey of Health, and Ageing and Retirement in Europe (SHARE) frailty instrument], study settings (community, hospital, and nursing home), provincial locations, and outcomes (prevalence of frailty or prefrailty). Any disagreement between the two authors was resolved by a third author (HLC) through discussion.
Three reviewers (AAP, SCL, and HLC) critically appraised the included articles by using the risk of bias in nonrandomized studies of exposures (ROBINS-E) visualization tool, which can be used to evaluate the quality of study methodology across seven domains. They used the following seven domains of bias in the ROBINS-E tool: (1) risk of bias due to confounding, (2) risk of bias arising from the measurement of the exposure, (3) risk of bias in the selection of participants for the study, (4) risk of bias due to post-exposure interventions, (5) risk of bias due to missing data, (6) risk of bias arising from the measurement of the outcome, and (7) risk of bias in the selection of the reported result [16]. The ROBINS-E is designed primarily for use in systematic reviews, where it is used to measure the strength of evidence to determine the presence or nature of the potential effect of an exposure on an outcome.
Frailty measurement tools
Several measurement tools were used in the included studies: Fried frailty phenotype, FRAIL questionnaire, FI-40 questionnaire, EFS, and SHARE frailty instrument. Of them, the FRAIL and Fried scales mainly focus on the physical component of frailty, separating it from disability and comorbidity, namely, the ‘phenotype of frailty’ model, whereas the SHARE frailty instrument is based on conditions or disabilities, and it tends to emphasize the number rather than the nature of deficits, namely, the ‘accumulation of deficits’ model [17, 18]. The Fried frailty phenotype is a standardized protocol that categorizes older adults as having frailty based on five characteristics: (1) unintentional weight loss, (2) weakness, (3) exhaustion, (4) slowness, and (5) low activity level. Those with no frailty characteristics are considered robust, whereas those with one or two characteristics are hypothesized to be in an intermediate, possibly prefrail, stage clinically [19].
The Frail Scale comprises 5 questions (yes–no answer), and based on their total score, patients are categorized as robust (0 points), prefrail (1–2 points), and frail (> 3 points). The scale assesses the presence of fatigue, muscle resistance, aerobic capacity, disease burden, and weight loss [20]. The FI-40 questionnaire is a self-report measurement tool assessing symptoms, illness, health attitudes, and changes in function in community-dwelling older adults [21]. The EFS can be used by non-geriatricians. It comprises 10 domains; the maximum score is 17 and represents the highest level of frailty [22]. The SHARE frailty instrument is a special 4-criterion tool developed to help general practitioners assess frailty [23], but it requires further evaluation in larger studies for its widespread use in all settings [24].
Data analysis
A meta-analysis was performed after sufficient homogeneity was achieved across the included studies. I2 statistics were calculated to evaluate homogeneity across the studies; an I2 value of < 50% indicated low heterogeneity [25]. The transition rates of the included studies were pooled through a random-effects meta-analysis. A random-effects model was selected a priori because of the expected high degree of heterogeneity in the study populations, settings, and outcomes [25]. Sensitivity analysis was conducted to determine whether the study with a high risk of bias significantly affected the results of this study.
Publication bias was evaluated graphically by generating funnel plots to determine the level of heterogeneity of the included studies. An asymmetric funnel indicated a publication bias, which was statistically verified using Begg’s rank correlation test and Egger’s linear regression test. The Comprehensive Meta-Analysis tool was used for all analyses. Data are presented in terms of percentages and 95% confidence intervals (CIs). To obtain the pooled estimates of frailty and prefrailty prevalence, a subgroup meta-analysis was performed after the studies were stratified by their settings and measurement tools; the meta-regression analysis was performed considering p < 0.005 to determine whether covariates such as mean age, sample size, and data collection years can explain the between-study heterogeneity.
Results
Characteristics of the included studies
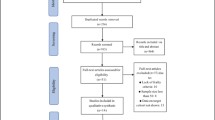
The literature search returned 79 articles, of which 20 articles (total participants = 6719; sample size = 27–2630) satisfied the inclusion criteria (Fig. 1). Seventeen articles were written in English, whereas three articles were in Indonesian. Frailty was assessed using the Fried Frailty Phenotype questionnaire in 12 studies (60%); the fatigue, resistance, aerobic, illness, and loss of weight (FRAIL) questionnaire in 3 studies (15%); the Frailty Index 40 (FI-40) questionnaire in 3 studies (15%); the Edmonton Frail Scale (EFS) in 1 study (5%); and the Survey of Health, Ageing and Retirement in Europe (SHARE) database in 1 study (5%). In terms of study settings, 8 (40%) studies were conducted in community settings, 7 (35%) were conducted in hospitals, and 5 (25%) were conducted in nursing homes. Fifteen articles reported the prevalence of both frailty and prefrailty in older adults, whereas five studies reported the prevalence of only frailty (Table 1).
The included studies covered 15 of 38 provinces in Indonesia (Fig. 2), representing the country’s major urban areas with high socioeconomic levels [35]. Eight of the studied provinces have a high proportion of older adults; these provinces are Yogyakarta, 15.52%; East Java, 14.53%; Central Java, 14.17%; North Sulawesi, 12.74%; Bali, 12.71%; South Sulawesi, 11.24%; Lampung, 10.22%; and West Java, 10.18% [11].
Assessment of quality
An assessment of the study quality (Fig. 3) revealed that 6 (30%) studies had high quality, 13 (65%) had some concerns, and 1 (5%) had low quality (high risk of bias). In most articles, the effects of key confounders were not adjusted for.
Pooled prevalence of frailty and prefrailty
Using a random-effects model, we performed meta-analyses for the prevalence of frailty and prefrailty, with 20 and 15 studies included, respectively. The prevalence of frailty ranged from 4.30% to 52.20%, whereas that of prefrailty ranged from 30.40% to 71%. As presented in Fig. 4, the pooled prevalence of frailty was 26.8% (95% CI: 20%–34.8%) and that of prefrailty was 55.5% in the Indonesian older adults (95% CI: 50.3%–60.6%). Publication bias was not detected (Fig. 5), and the results of the Begg-Mazumdar and Egger’s test were not significant (p = 0.9 and 0.06, respectively).
A high I2 value (I2 = 96.75%) was obtained, which indicated heterogeneity across the included studies. Therefore, sensitivity analysis, meta-regression, and subgroup analysis were performed for bias reduction. The sensitivity analysis revealed a similar prevalence of frailty (25.6%; CI = 19.1–33.4; I2 = 96.76, p < 0.001) and pre–frailty (57.5%; CI = 52.9–61.9; I2 = 90.39, p < 0.001) after one study with a high risk of bias [30] was excluded from the analysis. A meta-regression (Table 2) indicated that 1 year of data collection partly explained the heterogeneity observed in the prevalence of frailty (ꞵ = 0.33; p = 0.0007), whereas age (ꞵ = 0.07; p = 0.4257) and sample size (ꞵ = − 0.0016; p = 0.1729) could not explain the heterogeneity. Sub-group analysis was conducted on two variables, namely measurement tools and study settings (Table 3).
Prevalence of frailty and prefrailty in studies stratified by measurement tools
Because the EFS and SHARE databases were used in only one study each, the sample size was insufficient for meta-analysis. The remaining 18 studies were included in a subgroup analysis stratified by measurement tools. The results revealed that the prevalence of frailty and prefrailty in studies using the FI-40 questionnaire was 21.6% (95% CI: 15.5%–29.2%) and 64.3% (95% CI: 60.9%–67.6%), that in those using the FRAIL questionnaire was 18.7% (95% CI: 13.1%–25.9%) and 62% (95% CI: 58.9%–65%), and that in those using the Fried Frailty Phenotype questionnaire was 27.8% (95% CI: 17.2%–41.6%) and 59.8% (95% CI: 58.2%–61.4%), respectively (Fig. 6). However, no significant difference was noted across measurement tools for frailty (p = 0.403) or prefrailty (p = 0.214).
Prevalence of frailty and prefrailty in studies stratified by study settings
The prevalence of frailty and prefrailty in studies conducted in nursing homes was 37.9% (95% CI: 25.2%–52.6%) and 44.8% (95% CI: 33.5%–56.7%), that in those conducted in hospitals was 26.3% (95% CI: 21.4%–32%) and 61.4% (95% CI: 52.4%–69.6%), and that in those conducted in community settings was 21.1% (95% CI: 11.5%–35.6%) and 59.6% (95% CI: 55%–64.1%), respectively (Fig. 7). However, no significant difference was noted across study settings for frailty (p = 0.173) or prefrailty (p = 0.057).
Discussion
In this systematic review and meta-analysis, we investigated the overall prevalence of frailty and prefrailty in Indonesia. Our findings reveal that the pooled prevalence of frailty and prefrailty in Indonesian older adults was 26.8% and 55.5%, respectively. Stratified analysis revealed that the prevalence of frailty and prefrailty was 37.9% and 44.8%, 26.3% and 61.4%, and 21.1% and 59.6%, respectively, in studies conducted in nursing homes, hospitals, and community settings, respectively. The prevalence of frailty and prefrailty was 21.6% and 64.3%, 18.7% and 62%, and 27.8% and 59.8%, respectively, in studies using the FI-40, FRAIL, and Fried Frailty Phenotype questionnaire, respectively. However, no significant difference was observed across settings or measurement tools.
The lowest and highest prevalence was 4.30% and 52.20% for frailty and 30.40% and 71% for prefrailty, respectively. The reasons for the observed heterogeneity across the studies may be associated with differences in the study settings, population characteristics, and measurement tools. Information on the accurate prevalence of frailty is crucial for researchers involved in frailty research. Although Indonesia has a large population, the quality of its health services and the healthiness of the average person’s lifestyle in the country are not more favorable than those of developing or developed countries. Heterogeneity across regions in terms of health service distribution and a low level of health-related awareness among Indonesian individuals are the primary factors that have led to the country having a high rate of health problems, such as frailty [11].
The prevalence of frailty varies with the measurement tool used. Specifically, the multidimensional frailty tool (such as FI-40) provided a higher estimate of frailty than the physical dimensional frailty tool (such as Fried frailty phenotype and the FRAIL questionnaire) [4, 46,47,48]. However, we discovered no significant between-study differences in the results of measurement tools used for evaluating frailty and prefrailty prevalence in Indonesian older adults. Our data indicated a high prevalence of frailty assessed using the Fried Frailty Phenotype and different estimates of frailty prevalence from the two physical dimensional frailty tools (Fried frailty phenotype 27% vs FRAIL quesionnaire18%). These results are unexpected but are likely explained by the limited number of studies using the FI-40 and FRAIL scale in this review to define frailty.
The lowest, most moderate, and highest pooled prevalence of frailty was observed in community settings, hospitals, and nursing homes, respectively (21.1%, 26.3%, and 37.9%, respectively), the difference among the settings was nonsignificant; such an order of the prevalence of frailty in different study settings was also observed in a South American study (23.0%, 39.1%, and 55.8% in community settings, hospitals, and nursing homes, respectively; [49]. Studies have indicated that older adults recruited from hospitals and nursing homes had higher frailty levels than did those recruited from communities. For example, the prevalence of frailty in community-dwelling older adults has been reported to be 4%–59% [50, 51], that in hospital inpatients has been reported to be 20%–47.4% [52, 53], and that in nursing home residents has been reported to be 1.7%–76.3% [54, 55]. The older adults recruited from these institutions have various chronic medical health problems that affect their daily lives and lead to frailty [55]. Frailty in patients with various diseases can increase treatment costs [52].
The lowest, most moderate, and highest prevalence of prefrailty was 44.8% (nursing homes), 59.6% (community settings), and 61.4% (hospitals). Although no significant difference was discovered among the settings, such an order was also observed in a study conducted in South America, with the study reporting a prevalence of 29.8% in nursing homes, 47.6% in community settings, and 50.7% in hospitals [49]. The prevalence of prefrailty was the lowest in nursing homes, which might be because of the availability of adequate nursing home care for older adults in Indonesia and the fact that older adults tend to cohabitate with family rather than live in a nursing home or hospital. Notably, the pooled (all study settings) prevalence of prefrailty was higher in the present study than that reported in other studies, with other studies reporting a prevalence of 35% in nursing homes [54], 47.3% in community settings [50], and 25.8%–36.4% in hospitals [53, 55]. The high prevalence of prefrailty in Indonesia is concerning because it is an early but reversible sign of frailty, which can lead to negative health outcomes.
Most of the included studies were conducted in the urban areas of Indonesia. Older adults residing in urban areas often face challenges that may contribute to a disadvantaged status. They have inadequate access to opportunities for physical activity and limited social support from their families and communities [51, 56]. This observation is different from the prevailing notion and may be explained by the following reasons. First, Indonesian urban residents tend to be individualistic and spend most of their time working. Thus, older adults do not receive adequate family support. Second, urban developments in Indonesia are not centered on providing social facilities, such as parks and welfare agencies. Moreover, public transportation facilities fail to address the needs of older adults. Third, the complicated referral procedure and health services of Indonesia’s national health insurance systems and limited health-care facilities in urban areas are key barriers to accessing adequate support as well as social and health facilities for older adults. Similar findings have been reported by a study conducted in China [57].
The strength of the present study lies in the fact that we comprehensively searched six electronic databases to identify relevant regional articles. No date or language restriction was imposed during the literature search. Our study has some limitations. First, limited data are available regarding the prevalence of frailty and prefrailty in older adults residing in several Indonesian provinces, particularly those in the countryside, where the levels of frailty and prefrailty may be different from those in urban areas. This may introduce a bias in the estimation of the overall frailty burden in Indonesia. Second, the quality of study methodology was high in only 30% of the included studies. Some concerns were noted for the remaining studies; in fact, one study had a high level of bias. Third, some of the included studies had a small sample size (< 30 participants in 3 studies), which might not have been representative of the local populations of older adults with frailty. Finally, not all measurement tools have the category of prefrailty; however, determining the prefrailty status is crucial because a large proportion of older adults who are prefrail are likely to become frail; timely identification of this status can lead to timely intervention and potential recovery.
Conclusions
To the best of our knowledge, this study is the first meta-analysis to report the overall prevalence of frailty and prefrailty in older adults residing in Indonesia. The pooled prevalence of frailty and prefrailty in our study cohort was 26.8% and 55.5%, respectively. The prevalence did not vary significantly across study settings or measurement tools. The gradual increase in the number of older adults with frailty or prefrailty in Indonesia demands attention from the government, private sectors, health-care professionals, and the community. To address this problem, all stakeholders should jointly design effective strategies and policies by adopting a local cultural approach and enhancing the early detection and prevention of frailty and prefrailty in older adults residing in Indonesia.
Availability of data and materials
The datasets used and/or analyses during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CIs:
-
Confidence intervals
- FI-40:
-
Frailty Index 40
- FRAIL:
-
Fatigue, Resistance, Aerobic, Illness, and Loss of weight
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- SD:
-
Standard deviation
- SHARE:
-
Survey of Health, Ageing and Retirement in Europe
References
Castell M-V, Sánchez M, Julián R, Queipo R, Martín S, Otero Á. Frailty prevalence and slow walking speed in persons age 65 and older: implications for primary care. BMC Fam Pract. 2013;14(1):86.
Eyigor S, Kutsal YG, Duran E, Huner B, Paker N, Durmus B, et al. Frailty prevalence and related factors in the older adult—FrailTURK Project. Age. 2015;37(3):50.
He W, Muenchrath MN, Kowal PR. Shades of gray: a cross-country study of health and well-being of the older populations in SAGE countries, 2007–2010: US Department of Commerce. US: Economics and Statistics Administration; 2012.
Siriwardhana DD, Hardoon S, Rait G, Weerasinghe MC, Walters KR. Prevalence of frailty and prefrailty among community-dwelling older adults in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open. 2018;8(3):e018195.
Ge L, Yap CW, Heng BH. Prevalence of frailty and its association with depressive symptoms among older adults in Singapore. Aging Ment Health. 2019;23(3):319–24.
Vaingankar JA, Chong SA, Abdin E, Picco L, Chua BY, Shafie S, et al. Prevalence of frailty and its association with sociodemographic and clinical characteristics, and resource utilization in a population of Singaporean older adults. Geriatr Gerontol Int. 2017;17(10):1444–54.
Ahmad NS, Hairi NN, Said MA, Kamaruzzaman SB, Choo WY, Hairi F, et al. Prevalence, transitions and factors predicting transition between frailty states among rural community-dwelling older adults in Malaysia. PLoS One. 2018;13(11):e0206445.
Norazman CW, Adznam SNA, Jamaluddin R. Physical frailty among urban-living community-dwelling older adults in Malaysia. Int J Environ Res Public Health. 2020;17(18):6549.
Chittrakul J, Siviroj P, Sungkarat S, Sapbamrer R. Physical frailty and fall risk in community-dwelling older adults: a cross-sectional study. J Aging Res. 2020;2020:3964973.
Thinuan P, Siviroj P, Lerttrakarnnon P, Lorga T. Prevalence and potential predictors of frailty among community-dwelling older persons in Northern Thailand: a cross-sectional study. Int J Environ Res Public Health. 2020;17(11):4077.
Indonesian Central Statistics Agency. Elderly Population Statistics 2021. National Report. Jakarta: Indonesian Central Statistics Agency; 2021.
Undang-Undang Republik Indonesia Nomor 13 Tahun 1998 tentang Kesejahteraan Lanjut Usia (Law of the Republic of Indonesia Number 13 of 1998 concerning the Welfare of older adults); 1998.
Cawthon PM, Marshall LM, Michael Y, Dam T-T, Ensrud KE, Barrett-Connor E, et al. Frailty in older men: prevalence, progression, and relationship with mortality. J Am Geriatr Soc. 2007;55(8):1216–23.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9, w64.
Eriksen MB, Frandsen TF. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. J Med Libr Assoc. 2018;106(4):420–31.
ROBINS-E Development Group. Risk of Bias In Non-randomized Studies - of Exposure (ROBINS-E). 2022.
Dent E, Kowal P, Hoogendijk EO. Frailty measurement in research and clinical practice: a review. Eur J Intern Med. 2016;31:3–10.
Wei Y, McGrath PJ, Hayden J, Kutcher S. Measurement properties of tools measuring mental health knowledge: a systematic review. BMC Psychiatry. 2016;16(1):297.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56.
Aprahamian I, Cezar NOC, Izbicki R, Lin SM, Paulo DLV, Fattori A, et al. Screening for frailty with the FRAIL scale: a comparison with the phenotype criteria. J Am Med Dir Assoc. 2017;18(7):592–6.
Mitnitski AB, Song X, Rockwood K. The estimation of relative fitness and frailty in community-dwelling older adults using self-report data. J Gerontol A Biol Sci Med Sci. 2004;59(6):M627–32.
Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K. Validity and reliability of the Edmonton frail scale. Age Ageing. 2006;35(5):526–9.
Gilardi F, Capanna A, Ferraro M, Scarcella P, Marazzi MC, Palombi L, et al. Frailty screening and assessment tools: a review of characteristics and use in Public Health. Ann Ig. 2018;30(2):128–39.
Pialoux T, Goyard J, Lesourd B. Screening tools for frailty in primary health care: a systematic review. Geriatr Gerontol Int. 2012;12(2):189–97.
Borenstein M. Common Mistakes in Meta-Analysis and How to Avoid Them. New Jersey: Biostat, Inc.; 2019.
Aprianta IGA, Kuswardhani RT, Aryana IGPS. Hubungan Gangguan Pendengaran dan Frailty Pada Lansia Di Panti Sosial Tresna Werdha Wana Seraya Denpasar. Jurnal Penyakit Dalam Udayana. 2020;4(2):31–5.
Arjuna T, Soenen S, Hasnawati RA, Lange K, Chapman I, Luscombe-Marsh ND. A cross-sectional study of nutrient intake and health status among older adults in Yogyakarta Indonesia. Nutrients. 2017;9(11):1240.
Darwis Z, Safei I. Association between frailty and depression among elderly in nursing home. Surabaya Phys Med Rehabil J. 2022;4(2):55–62.
Faizah UZ, Widajanti N, Ichwani J. Two-year mortality profile in elderly with frailty: observational descriptive study in elderly health community in Surabaya, Indonesia. J Community Med Public Health Res. 2022;3(1):26–37.
Handajani YS, Widjaja NT, Turana Y. Frailty decreases physical health domain of quality of life in nursing home elderly. Universa Medicina. 2015;34(3):213–9.
Jayadi MJ, Udaya W, Sudarso A, Rasyid H, MakbulAman A, et al. Association between muscle mass with frailty state in elderly. Indian J Public Health Res Dev. 2020;11(6):1316–22.
Laksmi P, Ainun N, Setyohadi B, Setiati S, Ariane A, Tirtarahardja G. Association between the muscle mass index and physical frailty in geriatric outpatients. J Nat Sci Biol Med. 2019;10(3):103–8.
Ngestiningsih D, Sukmaningtyas H, Susanto TG, Probosari E. Relationship between body mass index, handgrip, and cognitive status on frailty status in elderly women. Bali Med J. 2020;9(3):859–62.
Ngestiningsih D, Dayanti JK, Batubara L. Relationship between IL-6, IL-1Î2, and vitamin D on frailty status in elderly women. Bali Med J. 2021;10(1):336–9.
Pengpid S, Peltzer K. Prevalence and associated factors of frailty in community-dwelling older adults in Indonesia, 2014–2015. Int J Environ Res Public Health. 2019;17(1):10.
Permatasari T, Sihombing B, Arianto P, editors. Frailty profile for geriatric patients in outpatient clinic of RSUP H. Adam Malik Medan. IOP Conference Series: Earth and Environmental Science. Bristol: IOP Publishing; 2018.
Rahmadani IR, Dwipa L, Pratiwi YS. Elderly characteristics with frailty syndrome by Frailty Index Questionnaire –40 (FI-40) at Bandung nursing home. J Med Health. 2018;2(2):756–63.
Rensa R, Setiati S, Laksmi PW, Rinaldi I. Factors associated with physical frailty in elderly women with low socioeconomic status in urban communities: a cross-sectional study. Acta Med Indones. 2019;51(3):220–9.
Rizka A, Indrarespati A, Dwimartutie N, Muhadi M. Frailty among older adults living in nursing homes in indonesia: prevalence and associated factors. Ann Geriatr Med Res. 2021;25(2):93.
Setiati S, Laksmi PW, Aryana IGPS, Sunarti S, Widajanti N, Dwipa L, et al. Frailty state among Indonesian elderly: prevalence, associated factors, and frailty state transition. BMC Geriatr. 2019;19(1):182.
Setiati S, Soejono CH, Harimurti K, Dwimartutie N, Aryana IGPS, Sunarti S, et al. Frailty and its associated risk factors: first phase analysis of multicentre Indonesia longitudinal aging study. Front Med. 2021;8:658580.
Seto E, Setiati S, Laksmi PW, Tamin TZ. Diagnostic test of a scoring system for frailty syndrome in the elderly according to cardiovascular health study, study of osteoporotic fracture and comprehensive geriatric assessment based frailty index compared with frailty index 40 items. Acta Med Indones. 2015;47(3):183–7.
Sunarti S, Hariyanti T. Physical activities, sitting time and frailty syndrome in elderly (A cross sectional study among elder person by Fried criteria). Malang Neurol J. 2018;4(2):59–64.
Triguna IPB, Kuswardhani RT, Purnami NKR. Correlation between body mass index and frailty in elderly men at Pemecutan Village, West Denpasar District. Bali J Penyakit Dalam Udayana. 2021;5(1):9–13.
Widajanti N, Ichwani J, Dharmanta RS, Firdausi H, Haryono Y, Yulianti E, et al. Sarcopenia and frailty profile in the elderly community of Surabaya: a descriptive study. Acta Med Indones. 2020;52(1):5–13.
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60(8):1487–92.
Da Mata FA, Pereira PP, Andrade KR, Figueiredo AC, Silva MT, Pereira MG. Prevalence of Frailty in Latin America and the Caribbean: a systematic review and meta-analysis. PLoS One. 2016;11(8):e0160019.
O’Caoimh R, Galluzzo L, Rodríguez-Laso Á, Van der Heyden J, Ranhoff AH, Lamprini-Koula M, et al. Prevalence of frailty at population level in European ADVANTAGE Joint Action Member States: a systematic review and meta-analysis. Ann Ist Super Sanita. 2018;54(3):226–38.
Coelho-Junior HJ, Marzetti E, Picca A, Calvani R, Cesari M, Uchida MC. Prevalence of prefrailty and frailty in South America: a systematic review of observational studies. J Frailty Aging. 2020;9(4):197–213.
Alqahtani BA, Alenazi AM, Alshehri MM, Osailan AM, Alsubaie SF, Alqahtani MA. Prevalence of frailty and associated factors among Saudi community-dwelling older adults: a cross-sectional study. BMC Geriatr. 2021;21(1):185.
Rivas-Ruiz F, Machón M, Contreras-Fernández E, Vrotsou K, Padilla-Ruiz M, Díez Ruiz AI, et al. Prevalence of frailty among community-dwelling elderly persons in Spain and factors associated with it. Eur J Gen Pract. 2019;25(4):190–6.
Bonjour T, Waeber G, Marques-Vidal P. Trends in prevalence and outcomes of frailty in a Swiss university hospital: a retrospective observational study. Age Ageing. 2021;50(4):1306–13.
Doody P, Asamane EA, Aunger JA, Swales B, Lord JM, Greig CA, et al. The prevalence of frailty and pre-frailty among geriatric hospital inpatients and its association with economic prosperity and healthcare expenditure: a systematic review and meta-analysis of 467,779 geriatric hospital inpatients. Ageing Res Rev. 2022;80:101666.
Cobden J, de Noronha M, Kingsley M. Prevalence of frailty and mobility disability in older people living in retirement villages. Australas J Ageing. 2022;41(2):222–8.
Veronese N, Custodero C, Cella A, Demurtas J, Zora S, Maggi S, et al. Prevalence of multidimensional frailty and pre-frailty in older people in different settings: a systematic review and meta-analysis. Ageing Res Rev. 2021;72:101498.
Ambagtsheer RC, Beilby J, Seiboth C, Dent E. Prevalence and associations of frailty in residents of Australian aged care facilities: findings from a retrospective cohort study. Aging Clin Exp Res. 2020;32(9):1849–56.
Llibre Rodriguez JJ, Prina AM, Acosta D, Guerra M, Huang Y, Jacob KS, et al. The prevalence and correlates of frailty in urban and rural populations in Latin America, China, and India: a 10/66 population-based survey. J Am Med Dir Assoc. 2018;19(4):287-95.e4.
Acknowledgements
Not applicable.
Funding
This study was partly supported by Taipei Medical University (PhD fellowship to AAP).
Author information
Authors and Affiliations
Contributions
A.A.P and S-C.L planned and designed the research study. AAP, S-C.L, and H–L.C carried out data collection and analysis. AAP, H–L.C and C-J.L drafted and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pradana, A.A., Chiu, HL., Lin, CJ. et al. Prevalence of frailty in Indonesia: a systematic review and meta-analysis. BMC Geriatr 23, 778 (2023). https://doi.org/10.1186/s12877-023-04468-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04468-y