Abstract
Background
The impact of multimorbidity on long-term care (LTC) use is understudied, despite its well-documented negative effects on functional disabilities. The current study aims to assess the association between multimorbidity and informal LTC use in China. We also explored the socioeconomic and regional disparities.
Methods
The study included 10,831 community-dwelling respondents aged 45 years and older from the China Health and Retirement Longitudinal Study in 2011, 2015, and 2018 for analysis. We used a two-part model with random effects to estimate the association between multimorbidity and informal LTC use. Heterogeneity of the association by socioeconomic position (education and income) and region was explored via a subgroup analysis. We further converted the change of informal LTC hours associated with multimorbidity into monetary value and calculated the 95% uncertainty interval (UI).
Results
The reported prevalence of multimorbidity was 60·0% (95% CI: 58·9%, 61·2%) in 2018. We found multimorbidity was associated with an increased likelihood of receiving informal LTC (OR = 2·13; 95% CI: 1·97, 2·30) and more hours of informal LTC received (IRR = 1·20; 95% CI: 1·06, 1·37), ceteris paribus. Participants in the highest income quintile received more hours of informal LTC care (IRR = 1·62; 95% CI: 1·31, 1·99). The estimated monetary value of increased informal LTC hours among participants with multimorbidity was equivalent to 3·7% (95% UI: 2·2%, 5·4%) of China’s GDP in 2018.
Conclusion
Our findings substantiate the threat of multimorbidity to LTC burden. It is imperative to strengthen LTC services provision, especially among older adults with multimorbidity and ensure equal access among those with lower income.
Similar content being viewed by others
Introduction
Multimorbidity, the coexistence of two or more chronic conditions, has become a prevalent global issue [1]. Ageing and relative socioeconomic deprivations are two leading determinants of multimorbidity [2]. The prevalence of multimorbidity increases with age and reaches over 50% among people aged 65 years or older globally [3]. Evidence in developed countries shows that those with higher socioeconomic status have a lower prevalence of multimorbidity [3,4,5]. People with multimorbidity often have poorer health outcomes [6, 7], driving increased utilisation of health services and expenditures in developed [8, 9] and developing countries [10,11,12]. Consequently, multimorbidity has become a global concern, given the accelerated pace of population ageing globally.
People with multimorbidity have also been found to have poorer functional outcomes [13, 14]. Physiologically, people with multimorbidity have been found to have elevated levels of blood inflammatory markers, which indicate a heightened susceptibility to functional disabilities, frailty, and premature death [15,16,17]. In addition, there is strong evidence that some non-communicable diseases (NCDs), such as stroke [18], arthritis [19, 20], dementia [21], and diabetes [22], can directly lead to or predict negative functional outcomes. Such evidence implies a high demand for long-term care (LTC), i.e., help with daily activities, especially among older people with multimorbidity. Studies thus far have focused on assessing whether having selected medical conditions, such as dementia and stroke, is associated with increased care dependency or increased LTC expenditures [23, 24]. A collection of studies conducted in Germany [25], Japan [26], and Scotland [27] considered whether multimorbidity is associated with higher LTC dependency, receipt of formal social care, or total formal LTC expenditures. Though available evidence shows a positive correlation, it has focused on formal LTC services and expenditures recorded by insurance claims data in developed countries. Informal care has been largely ignored, though it usually accounts for a larger proportion of the care provided to older people, especially in countries whose LTC systems are not fully established.
China has the largest older adult population in the world, faces a high burden of NCDs, and substantial regional disparities in economic development and health outcomes. The number of older people aged 60 and above reached 264 million and accounted for 18·70% of the total population in 2020 [28]. With regard to China’s health profile, the burden of NCDs has increased dramatically over recent decades, and NCDs contributed to around 85% of the total disease burden in 2019 [29]. Studies have found that the prevalence of multimorbidity is 40–70% among older people in China [11, 30,31,32]. There are tiered regional differences in terms of economic development and health outcomes between the eastern, central, and western provinces in China. For example, the 2020 gross domestic product (GDP) per capita in Beijing (east region) was 2·6 times that of Anhui (central region), and 4·6 times that of Gansu (west region) [33]. In 2015, the average healthy life expectancy was estimated to be around 78 years among males in Beijing, Tianjin, and Shanghai (eastern region), but only 69 years in Qinghai, Tibet, and Yunnan (western region) [34].
The Chinese government has started to work on establishing a comprehensive LTC system for accessible, affordable, and high-quality LTC for older people and outlined a three-tiered LTC system in 2011 in the 12th Five-Year Plan for National Economic and Social Development [35]. However, the LTC system in China is still in its infancy, with insufficient financing and workforce to provide formal LTC services [36]. Therefore, older people with disabilities primarily rely on informal LTC, defined as LTC provided by informal caregivers such as family members and relatives free of charge, for assistance with daily living activities [37]. However, the burden of informal LTC could be partially transferred to the LTC system once it is fully established and functioning. Considering the heavy burdens of NCDs and rapid population ageing in China, it is imperative that we understand how multimorbidity could impact the burdens of informal LTC. However, little evidence is available on the relationship between multimorbidity and informal LTC use in China.
In this study, we aim to assess the association between multimorbidity and informal LTC use in China and explore the socioeconomic and regional disparities. We used 8-year nationally representative household survey data collected by the China Health and Retirement Longitudinal Study (CHARLS) for analysis. We presented the prevalence of multimorbidity, analysed the association between multimorbidity and informal LTC use, and estimated the corresponding monetary value of the change in informal LTC hours. The heterogeneity of the effect driven by socioeconomic position (education and income) and region (economic development) was further explored via sub-group analysis.
Methods
Data and study participants
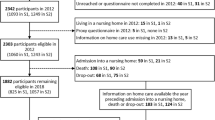
We used longitudinal survey data collected by the CHARLS in Waves 1, 3, and 4, conducted in 2011, 2015, and 2018, respectively, for analysis. The survey follows the design of the Health and Retirement Survey (HRS) in the US [38]. The CHARLS sample is a nationally representative sample of the population aged over 45 years living in households in China. The first wave of the survey was conducted in 28 provinces, and 17,708 participants responded [39]. More about the CHARLS design has been published elsewhere [40].
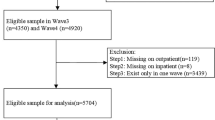
A total of 10,831 participants were included for analysis in the current study. We included participants with no missing values in key variables of interest and no loss to follow-up in Waves 3 and 4. Observations for Wave 2 were not included, as data on informal LTC use were not available. We further excluded respondents with abnormal values in informal LTC use (Figure S1 for the flowchart of study participants selection and Table S1 for the basic characteristics of the excluded participants).
Multimorbidity
Multimorbidity was defined as the coexistence of two or more chronic conditions. The CHARLS has measured 14 physical and mental chronic conditions, and we included all of them to measure multimorbidity in the current study. The 14 chronic conditions were hypertension, diabetes or high blood sugar, dyslipidaemia, heart disease, stroke, cancer, chronic lung disease, liver disease, digestive diseases, kidney disease, arthritis, asthma, psychiatric problems, and memory-related diseases.
Informal long-term care use
Informal LTC refers to LTC provided by informal caregivers free of charge. Informal LTC use was measured as self-reported hours of help/services received from informal caregivers to assist with activities of daily living (ADLs) or instrumental activities of daily living (IADLs) in the past month. Informal caregivers include spouses, children, grandchildren, and relatives. The hours of help/services provided by all recorded informal caregivers on ADL and IADL assistance were aggregated to generate the total hours of help/services received.
Covariates
We controlled for a set of covariates in the model to adjust for common socioeconomic determinants of health status and of receipt of informal LTC. Covariates included age, sex, marital status, socioeconomic position (education and income), region of residency, number of co-residents, urban or rural residence, and whether covered by public health insurance. Marital status was coded as a dichotomous variable: with a companion (married or partnered) or without a companion (separated, divorced, widowed, or never married).
We measured socioeconomic position by education and income, respectively. Each respondent’s highest education level obtained was coded using a scale with three tiers: (1) primary school or lower, (2) junior middle school, and (3) high school (vocational school) and above. To address the issue of underreported income, we used annual total household consumption per capita as a proxy and split this into quintiles to measure the relative socioeconomic deprivation by income.
We categorised the 28 provinces based on their GDP per capita in 2020 and ranked them in tertiles (see Appendix for specific provinces in the three groups) to measure regional disparities. The GDP per capita of the three regions was 7,404·6, 9,254·8, and 13,604·7 USD, respectively, in 2020 (exchange rate: 1 USD = 6·70 CNY).
Statistical analysis
We calculated the reported prevalence of multimorbidity by wave and, for each wave, by sex, age group, functional status, region, and socioeconomic position. We also conducted Chi-squared tests to assess the statistical difference among subgroups. In addition, we calculated the reported prevalence of the five leading chronic conditions among participants with multimorbidity to better understand their disease profiles.
We used a panel data analysis approach to estimate the association between multimorbidity and informal LTC use. To account for the zero-mass problem for informal LTC use, we chose a two-part model with random effects for analysis [41, 42]. Specifically, a logit model was used to estimate the probability of informal LTC use (0/1) for the first part. Conditioning on the use of informal LTC (for the first part), a negative binomial model was adopted to estimate the effect of multimorbidity on the intensity of informal LTC use (hours) for the second part. We treated the dependent variable, the hours of informal LTC use, as a count variable as the underlying data is discrete data that takes on countable and distinct values, and the distribution is highly skewed. Typically, modelling a dependent count variable with excessive zeros employs either Poisson or negative binomial models. We selected a negative binomial model, considering the over-dispersion issue of informal LTC use. Standard errors were clustered at the individual level to handle serial correlation. The model also controlled for covariates and period fixed effects (see Appendix for the econometric model). To explore the heterogeneity of the association driven by socioeconomic and regional disparities, we also conducted subgroup analysis by socioeconomic position and region, respectively, using the same model. Considering the mediating role of functional disabilities in the relationship between multimorbidity and informal LTC use, we further assessed the association between multimorbidity and functional disabilities for a better interpretation of the results (Appendix).
We reported odds ratios (OR) for the first part’s logit model results and incidence rate ratios (IRR) for the second part’s negative binomial model results, with 95% CI and statistical significance level. The proportion of missingness for the covariates was low (< 2%), except in the case of household consumption (14·1%, 30·4%, and 16·6% at Waves 1, 3, and 4, respectively). We therefore used the multivariate imputation by chained equations (MICE) approach to impute the missing values of household consumption for regression estimate based on key socioeconomic covariates (education, gender, and age) and 20 sets of imputations [43, 44]. We reported weighted results for multimorbidity prevalence and non-weighted results for regression analysis [31].
Sensitivity analysis
We conducted sensitivity analyses to check the robustness of the regression results. First, we used a Poisson model for the second part to re-estimate regression results. Second, we adjusted the measurement of multimorbidity to code it as the total number of chronic conditions. Third, we used non-medical household consumption per capita as a proxy for measuring income quintiles, considering total household consumption might be driven up by bad health. We performed the same imputation methods for non-medical household consumption to deal with missing data.
Economic burden estimation
We converted the change of hours of informal LTC received among older people with multimorbidity to monetary value through benchmarking the national average salaries of urban workers in health and social services (Appendix for calculation details and Table S2 for base case data inputs). The burden was further converted to a percentage of annual GDP for an intuitive understanding of its magnitude relative to the economy.
We performed uncertainty analysis to assess the impact of variables of interest on the economic burden. We allowed the three variables of interest to vary within set ranges (Appendix for the range of variables). The three variables were multimorbidity prevalence, average hours of informal LTC use among middle-aged and older people with multimorbidity, and average annual salaries for workers in health and social services. For each variable, we performed 1,000 random draws following a normal distribution, with its mean set at the base case scenario level within the range of the variable. The 95% uncertainty interval (UI) of the economic burden as a percentage of annual GDP was calculated, defined in terms of the respective estimates obtained from the 2.5th and 97.5th percentile of the estimated economic burden.
Results
For the 10,831 participants included in the analysis, the mean age was 64·1 in 2018. Females comprised 52·6% of the study sample, and 66·0% of the study sample received no education beyond the primary school level. Participants residing in rural areas comprised 64·6% of the sample. The percentages of participants residing in regions by tertile of economic development were 35·4% (most deprived), 33·4%, and 31·2% (most affluent), respectively. The percentages of participants with difficulties in ADLs and IADLs were 20·6% and 25·8%, respectively, in 2018 (Table 1).
In 2018, the reported prevalence of multimorbidity was 60·0% (95% CI: 58·9%, 61·2%) among study participants (Table 2). It was significantly higher among females, participants of older age, and those with disabilities (p < 0·001). Notably, the reported prevalence rose to 81% among those with disabilities in ADLs. Furthermore, we observed that the proportion was highest among participants at the lowest education level but highest among those in the top income quintile (p < 0·001). As for regional disparities, the reported prevalence was lowest in the most developed region but highest in the moderately developed region (p < 0·001). The top five contributors to multimorbidity were arthritis, hypertension, digestive diseases, dyslipidaemia, and heart diseases (Figure S2).
We found multimorbidity to be significantly associated with a higher likelihood of receiving informal LTC (OR = 2·13; 95% CI: 1·97, 2·30) and receipt of more hours of informal LTC (IRR = 1·20; 95% CI: 1·06, 1·37), ceteris paribus. Participants with companions (married or partnered) and living in rural areas were significantly more likely to receive informal LTC, though they received fewer hours of care. Participants with higher levels of education and those who lived in the most affluent region were also found to be less likely to receive informal LTC (P < 0·001), and those in the most affluent region received significantly fewer hours of care (IRR = 0·78, 95% CI: 0·66, 0·91). However, those in the highest quintile of income received significantly more hours of informal LTC than those in the lowest quintile (IRR = 1·62; 95% CI: 1·31, 1·99). In addition, age and number of co-residents were both strong, significantly positive predictors in both parts of the model (Table 3).
Overall, the subgroup analysis detected no significant heterogeneity of effect by socioeconomic position or region (Fig. 1). Multimorbidity was associated with a higher likelihood of receiving informal LTC at all levels of socioeconomic groups and in all regions. Nevertheless, the effect on the intensity of informal LTC did not persist at the higher level of income groups. In addition, the results of the sensitivity analyses yielded highly consistent results (Table S4, S5 and S6). The estimated economic burden associated with increased informal LTC among middle-aged and older adults with multimorbidity was 512·2 billion USD in 2018, equivalent to 3·7% (95% UI: 2·2%, 5·4%) of China’s 2018 GDP (Fig. 2).
Discussion
Despite the rich evidence on the impact of multimorbidity on health systems, this is, to our knowledge, the first study estimating the association between multimorbidity and informal LTC use in China. We find that the prevalence of multimorbidity was high and had risen fast among the study participants from 2011 to 2018. Overall, three of every five people aged 45 years or older in China reported multimorbidity. This is within the range of prevalence found in previous studies in China [11, 12, 30,31,32] but higher than the prevalence in developed countries [3]. Notably, the reported prevalence of multimorbidity rose to around 80% among participants with functional disabilities in 2018. The fast growth of reported multimorbidity prevalence can be attributed to worsened health conditions with ageing and improved diagnosis of NCDs due to strengthened NCDs control and management at the primary health care level. Strengthening the primary health care system is one focus of China’s health system reform, initiated in 2009; comprehensive control and management policies for multiple NCDs, strategies and projects have been implemented since then [45, 46]. Typical programs that facilitate NCD diagnosis include the nationwide Integrated NCD Prevention and Control Project and the take-up of free health checkups programs among older people [47, 48].
The results provide strong evidence that multimorbidity could increase the use of informal LTC, which in turn may have a profound impact on the LTC system, especially in terms of service delivery and financing when the LTC system begins to function well. Participants with multimorbidity are more likely to receive informal LTC and receive more hours of care. In addition, older participants and participants with a greater number of co-residents were significantly more likely to receive informal LTC and to receive more care. Those with a spouse or partner are more likely to receive informal LTC, though they receive fewer hours of informal LTC, as their functional abilities are better initially (Table S3). Notably, participants living in rural areas are also found to receive fewer hours of informal LTC, even though their functional abilities are worse than those of urban participants (Table S3). The annual economic burden due to increased informal LTC among people with multimorbidity is non-negligible, equivalent to 3·7% of China’s annual GDP in 2018. In comparison, total health expenditures, represented as a percentage of GDP, were 5·4% in 2018 [49]. This burden may be partially transferred to the LTC system, and it may make sustainable financing of the system even more challenging [36].
Socioeconomic position has been demonstrated to be an important determinant of health. Evidence shows it generally favours the less deprived in terms of access to and quality of health services utilised, as well as the health outcomes in Western countries [2, 4, 5, 50, 51]. Interestingly, our study finds that the socioeconomic disparities driven by income and education differ. First, the prevalence of multimorbidity increased with higher income but decreased with higher levels of education. One reasonable explanation is that people in the higher income groups are more likely to get diagnosed and to report it. In addition, our findings are consistent with those of previous studies conducted in China that the association between socioeconomic position and health could be mixed [11, 12]. The inverse association of multimorbidity by income and education could be driven by the difference in their interactions with unhealthy behaviours. For example, unhealthy behaviours such as smoking and high-frequency drinking were flat by wealth but are lower among older people with higher levels of education in China [52]. Second, participants in the highest income group received significantly more hours of informal LTC, though we found no significant difference in functional disabilities among participants in the different income groups (Table S3). Education, however, did not drive such differences in the hours of informal LTC received as income. This is consistent with previous studies showing that wealth is a stronger predictor of health services use and outcomes than education [51, 53].
We find regional disparities in terms of both the prevalence of multimorbidity and receipt of informal LTC. The reported prevalence of multimorbidity was lowest in the most developed region while highest in the moderately developed region, which consists primarily of central provinces. These findings are not surprising, as public health financing has been lowest for these provinces for years. In China, public health financing for provinces comes from a central government transfer fund, local government budgets, and a health insurance fund [45]. The most deprived provinces could receive the most central government transfers, while the most affluent provinces may utilise funding from their local budgets, leaving those provinces in the middle rank of economic development in the most disadvantageous positions in terms of health financing. For example, the 2018 total government health expenditures per capita in the three regions, from least to most developed, were 182·2, 163·3 and 207·5 USD (exchange rate: 1USD = 6·70 CNY, July 2022) [54]. The participants in the least affluent region were more likely to receive informal LTC and more hours of care, as participants in these provinces are found to have worse functional abilities compared to those in the most affluent region (Table S2).
This study’s findings carry important policy implications for chronic diseases and multimorbidity management in China. First and foremost, it is crucial to continue strengthening NCD prevention and control at the primary care level to reduce the prevalence of multimorbidity. Promoting healthy lifestyles is essential, and special attention should be paid to both the moderately and most deprived provinces, where the prevalence of multimorbidity is higher. Further, governments need to consider increasing health financing for these moderately developed provinces. Second, the management of NCDs should shift from targeting a single disease to multiple diseases, as has been widely pointed out [1, 2, 6, 11]. This is especially important in the case of older people, who are more prone to multimorbidity. Third, health and functional abilities are intercorrelated, and it is more efficient to integrate the provision of health and LTC services at the primary care level. For example, primary health centres should integrate timely and regular monitoring of functional abilities with health status for people with multimorbidity and take effective actions to restore or maintain these patients’ functional abilities. Fourth, resources should be purposively allocated to help the more socioeconomically deprived people, as measured by income, to receive health and LTC care in the important effort to reduce the socioeconomic inequalities which could be magnified in other aspects of people’s lives. The design of the public LTC insurance program should take this into consideration. Some of these implications may also apply to other developing countries with similar disease and demographic profiles.
The study admits to several limitations. First, we rely on the self-reported diagnoses by doctors from the CHARLS to measure multimorbidity, which might underestimate the multimorbidity prevalence as some participants, especially those in rural areas, might have limited access to timely diagnosis. Second, the numbers and types of chronic conditions measured in CHARLS are comprehensive though not exhaustive. Third, the measurement of multimorbidity focuses on the number of chronic conditions. Though standard and used extensively, it fails to capture the severity and interactions among different chronic conditions. Fourth, we excluded those lost to follow-up at Waves 3 and 4, which may lead to an underestimation of the results as they were generally older, had more difficulties in conducting ADLs and IADLs, and had a higher reported multimorbidity prevalence at baseline (Table S1). In addition, we only controlled marital status and the number of co-residents and were not able to include all the factors in our model that affect access to informal LTC, such as the willingness of family members to provide care, due to data availability. Further, the estimation of economic burdens is derived from the salaries of urban workers, which may overestimate the burden, despite our sensitivity analyses geared at partially offsetting this. The estimation also overlooks other sources of burden, such as the mental cost and the retirement savings foregone to caregivers, which may translate to other social burdens. Finally, future studies could explore the impact of multimorbidity on formal LTC burden when high-quality data become available.
Conclusion
Our findings substantiate the threat of multimorbidity to LTC burden and highlight the socioeconomic inequalities in receiving informal LTC driven by income. Urgent actions should be taken, as this study proposes, to strengthen LTC services provision, especially among older people with multimorbidity and ensure equal access among those with lower income.
Data availability
The CHARLS data and socioeconomic data from China Statistical Yearbooks are all publicly available to researchers. Researchers can access and download the CHARLS data from its website (http://charls.pku.edu.cn/en/) and China’s socioeconomic data from the National Bureau of Statistics of China (http://www.stats.gov.cn/english/Statisticaldata/AnnualData/).
References
Mercer S, Furler J, Moffat K, Fischbacher-Smith D, Sanci LA, World Health Organization. et al. Multimorbidity: Technical Series on Safer Primary Care. Geneva: World Health Organization; 2016.
Pearson-Stuttard J, Ezzati M, Gregg EW. Multimorbidity—a defining challenge for health systems. The Lancet Public Health. 2019;4(12):e599–600.
Nguyen H, Manolova G, Daskalopoulou C, Vitoratou S, Prince M, Prina AM. Prevalence of multimorbidity in community settings: a systematic review and meta-analysis of observational studies. J Comorb. 2019;9:2235042X1987093.
Dugravot A, Fayosse A, Dumurgier J, Bouillon K, Rayana TB, Schnitzler A, et al. Social inequalities in multimorbidity, frailty, disability, and transitions to mortality: a 24-year follow-up of the Whitehall II cohort study. The Lancet Public Health. 2020;5(1):e42–50.
Head A, Fleming K, Kypridemos C, Schofield P, Pearson-Stuttard J, O’Flaherty M. Inequalities in incident and prevalent multimorbidity in England, 2004–19: a population-based, descriptive study. The Lancet Healthy Longevity. 2021;2(8):e489–97.
Marengoni A, Vetrano DL. Multimorbidity: disease of society? The Lancet Healthy Longevity. 2021;2(8):e451–2.
Nunes BP, Flores TR, Mielke GI, Thumé E, Facchini LA. Multimorbidity and mortality in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2016;67:130–8.
Fleishman JA, Cohen JW. Using information on clinical conditions to predict high-cost patients. Health Serv Res. 2010;45(2):532–52.
Hazra NC, Rudisill C, Gulliford MC. Determinants of health care costs in the senior elderly: age, comorbidity, impairment, or proximity to death? Eur J Health Econ. 2018;19(6):831–42.
Lee JT, Hamid F, Pati S, Atun R, Millett C. Impact of Noncommunicable Disease Multimorbidity on Healthcare Utilisation and Out-Of-Pocket Expenditures in Middle-Income Countries: Cross Sectional Analysis. Correa-Velez I, editor. PLoS ONE. 2015;10(7):e0127199.
Zhao Y, Atun R, Oldenburg B, McPake B, Tang S, Mercer SW, et al. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: an analysis of population-based panel data. The Lancet Global Health. 2020;8(6):e840–9.
Zhao Y, Atun R, Anindya K, McPake B, Marthias T, Pan T, et al. Medical costs and out-of-pocket expenditures associated with multimorbidity in China: quantile regression analysis. BMJ Glob Health. 2021;6(2):e004042.
Ryan A, Wallace E, O’Hara P, Smith SM. Multimorbidity and functional decline in community-dwelling adults: a systematic review. Health Qual Life Outcomes. 2015;13(1):168.
Vetrano DL, Palmer K, Marengoni A, Marzetti E, Lattanzio F, Roller-Wirnsberger R, et al. Frailty and Multimorbidity: a systematic review and Meta-analysis. The Journals of Gerontology: Series A. 2019;74(5):659–66.
Ferrucci L, Fabbri E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol. 2018;15(9):505–22.
Friedman E, Shorey C. Inflammation in multimorbidity and disability: an integrative review. Health Psychol. 2019;38(9):791–801.
Friedman EM, Mroczek DK, Christ SL. Multimorbidity, inflammation, and disability: a longitudinal mediational analysis. Therapeutic Adv Chronic Disease. 2019;10:2040622318806848.
KWAKKEL G, WAGENAAR RC, KOLLEN BJ. Predicting disability in Stroke—A critical review of the literature. Age Ageing. 1996;25(6):479–89.
Yelin E, Meenan R, Nevitt M, Epstein W. Work disability in rheumatoid arthritis: Effects of Disease, Social, and work factors. Ann Intern Med. 1980;93(4):551–6.
Sherrer YS, Bloch DA, Mitchell DM, Young DY, Fries JF. The development of disability in rheumatoid arthritis. Arthr Rhuem. 1986;29(4):494–500.
Sauvaget C, Yamada M, Fujiwara S, Sasaki H, Mimori Y. Dementia as a predictor of functional disability: a Four-Year Follow-Up study. GER. 2002;48(4):226–33.
Wong E, Backholer K, Gearon E, Harding J, Freak-Poli R, Stevenson C, et al. Diabetes and risk of physical disability in adults: a systematic review and meta-analysis. The Lancet Diabetes & Endocrinology. 2013;1(2):106–14.
Schwarzkopf L, Menn P, Leidl R, Wunder S, Mehlig H, Marx P, et al. Excess costs of dementia disorders and the role of age and gender - an analysis of german health and long-term care insurance claims data. BMC Health Serv Res. 2012;12(1):165.
Ferri CP, Schoenborn C, Kalra L, Acosta D, Guerra M, Huang Y, et al. Prevalence of stroke and related burden among older people living in Latin America, India and China. J Neurol Neurosurg Psychiatry. 2011;82(10):1074–82.
Koller D, Schön G, Schäfer I, Glaeske G, van den Bussche H, Hansen H. Multimorbidity and long-term care dependency—a five-year follow-up. BMC Geriatr. 2014;14(1):70.
Mori T, Hamada S, Yoshie S, Jeon B, Jin X, Takahashi H, et al. The associations of multimorbidity with the sum of annual medical and long-term care expenditures in Japan. BMC Geriatr. 2019;19(1):69.
Henderson DAG, Atherton I, McCowan C, Mercer SW, Bailey N. Linkage of national health and social care data: a cross-sectional study of multimorbidity and social care use in people aged over 65 years in Scotland. Age Ageing. 2021;50(1):176–82.
National Bureau of Statistics. Public Report of the Seventh National Census (No.5) [Internet]. 2021 [cited 2021 Aug 9]. Available from: http://www.stats.gov.cn/tjsj/tjgb/rkpcgb/qgrkpcgb/202106/t20210628_1818824.html.
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. [Internet]. 2020 [cited 2021 Aug 10]. Available from: http://ghdx.healthdata.org/gbd-results-tool.
Ma X, He Y, Xu J. Urban–rural disparity in prevalence of multimorbidity in China: a cross-sectional nationally representative study. BMJ Open. 2020;10(11):e038404.
Yao SS, Cao GY, Han L, Chen ZS, Huang ZT, Gong P et al. Prevalence and Patterns of Multimorbidity in a Nationally Representative Sample of Older Chinese: Results From the China Health and Retirement Longitudinal Study. Newman A, editor. The Journals of Gerontology: Series A. 2020;75(10):1974–80.
Zhang Y, Zhou L, Liu S, Qiao Y, Wu Y, Ke C, et al. Prevalence, correlates and outcomes of multimorbidity among the middle-aged and elderly: findings from the China Health and Retirement Longitudinal Study. Arch Gerontol Geriatr. 2020;90:104135.
National Bureau of Statistics, China. National data [Internet]. 2020 [cited 2021 Aug 12]. Available from: https://data.stats.gov.cn/easyquery.htm?cn=E0103.
Li H, Hanewald K, Wu S. Healthy life expectancy in China: Modelling and implications for public and private insurance. Annals of Actuarial Science. 2021;15(1):40–56.
The State Council. Notice of the State Council on Printing and Distributing the “Twelfth Five-Year Plan” for the Development of China’s Aging Care Section [Internet]. 2011 [cited 2021 Aug 10]. Available from: http://www.gov.cn/zwgk/2011-09/23/content_1954782.htm.
Feng Z, Glinskaya E, Chen H, Gong S, Qiu Y, Xu J, et al. Long-term care system for older adults in China: policy landscape, challenges, and future prospects. The Lancet. 2020;396(10259):1362–72.
Yang W, Tan SY. Is informal care sufficient to meet the long-term care needs of older people with disabilities in China? Evidence from the China Health and Retirement Longitudinal Survey. Ageing Soc. 2021;41(5):980–99.
Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR. Cohort Profile: the Health and Retirement Study (HRS). Int J Epidemiol. 2014;43(2):576–85.
Zhao Y, Stauss J, Yang G, Giles J, Hu P (Perry), Hu Y China Health and Retirement Longitudinal Study, et al. editors. 2011–2012 National Baseline User’s Guide [Internet]. National School of Development, Peking University.; 2013. Available from: http://charls.pku.edu.cn/Public/ashelf/public/uploads/document/2011-charls-wave1/application/CHARLS_nationalbaseline_users_guide.pdf.
Zhao Y, Stauss J, Chen X, Wang Y, Gong J, Meng Q et al. China Health and Retirement Longitudinal Study Wave 4 User’s Guide [Internet]. National School of Development, Peking University.; 2020. Available from: http://charls.pku.edu.cn/Public/ashelf/public/uploads/document/2018-charls-wave4/application/CHARLS_2018_Users_Guide.pdf.
Farewell VT, Long DL, Tom BDM, Yiu S, Su L. Two-part and related regression models for Longitudinal Data. Annu Rev Stat Appl. 2017;4:283–315.
Neelon B, O’Malley AJ, Smith VA. Modeling zero-modified count and semicontinuous data in health services research part 1: background and overview: modeling zero-modified count and semicontinuous data in health services research part 1: background and overview. Statist Med. 2016;35(27):5070–93.
Royston P, White IR. Multiple imputation by chained equations (MICE): implementation in Stata. J Stat Softw. 2011;45:1–20.
Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20(1):40–9.
Yip W, Fu H, Chen AT, Zhai T, Jian W, Xu R, et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. The Lancet. 2019;394(10204):1192–204.
Meng Q, Mills A, Wang L, Han Q. What can we learn from China’s health system reform? BMJ. 2019;365:l2349.
Liu S, Chen Z, Han L, Dong W, Li H, Koplan J, et al. Integrated multisectoral non-communicable disease prevention and control in China: a review of agencies and policies. J Glob Health. 2020;10(2):020304.
Du B, Mu Y, The Relationship Between Health Changes and Community Health Screening Participation Among Older People. Frontiers in Public Health [Internet]. 2022 [cited 2022 May 15];10. Available from: https://www.frontiersin.org/article/https://doi.org/10.3389/fpubh.2022.870157.
World Bank. Current health expenditure (% of GDP) | Data [Internet]. 2022 [cited 2022 May 18]. Available from: https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS.
Davies JM, Sleeman KE, Leniz J, Wilson R, Higginson IJ, Verne J, et al. Socioeconomic position and use of healthcare in the last year of life: a systematic review and meta-analysis. PLoS Med. 2019;16(4):e1002782.
Davies JM, Maddocks M, Chua KC, Demakakos P, Sleeman KE, Murtagh FEM. Socioeconomic position and use of hospital-based care towards the end of life: a mediation analysis using the English Longitudinal Study of Ageing. The Lancet Public Health. 2021;6(3):e155–63.
Huang R, Grol-Prokopczyk H. Health and health behaviors in China: anomalies in the SES-health gradient? SSM - Population Health. 2022;17:101069.
Demakakos P, Biddulph JP, Bobak M, Marmot MG. Wealth and mortality at older ages: a prospective cohort study. J Epidemiol Community Health. 2016;70(4):346–53.
National Health and Family Planning Commission. China Health and Family Planning Statistical Yearbook 2019. Beijing: Peking Union Medical College Press; 2019.
Acknowledgements
We thank the China Health and Retirement Longitudinal Study team for designing, collecting, and sharing the data. We also thank Prof. Michael Keane, UNSW, for his valuable technical suggestions on the econometric methods used in this study, and Mr Lei Guo, Duke Global Health Institute, for his help with the figures in this paper.
This analysis uses data or information from the Harmonized CHARLS dataset and Codebook, Version D, as of June 2021, developed by the Gateway to Global Aging Data. The development of the Harmonised CHARLS was funded by the National Institute on Aging (R01 AG030153, RC2 AG036619, R03 AG043052). For more information, please refer to https://g2aging.org/.
Funding
This work was supported by the UNSW Sydney and the ARC Centre of Excellence in Population Ageing Research (CEPAR), Australia.
Author information
Authors and Affiliations
Contributions
SC designed the study under the supervision of KH, BL, and HB. SC extracted the data, conducted statistical analyses in Stata, formulated tables and figures, and drafted the manuscript. SC and YS verified the data used in the study. All authors contributed to commenting, editing, and approval of the final manuscript. All accept responsibility for submitting for publication.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The conduct of the study is in accordance with the Declaration of Helsinki. The CHARLS received ethical approval from the Biomedical Ethics Review Committee of Peking University, China (IRB00001052-11015), and all participants were required to provide written informed consent. Our study obtained further ethical approval from the Human Research Ethics Committee of the University of New South Wales, Australia (HC 210795).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, S., Si, Y., Hanewald, K. et al. Association between multimorbidity and informal long-term care use in China: a nationwide cohort study. BMC Geriatr 23, 700 (2023). https://doi.org/10.1186/s12877-023-04371-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04371-6