Abstract
Background
Chronic pain (CP) may increase the risk of acute coronary syndrome (ACS); however, this issue in the older population remains unclear. Therefore, this study was conducted to clarify it.
Methods
We used the Taiwan National Health Insurance Research Database to identify older patients with CP between 2001 and 2005 as the study cohort. Comparison cohort was the older patients without CP by matching age, sex, and index date at 1:1 ratio with the study cohort in the same period. We also included common underlying comorbidities in the analyses. The risk of ACS was compared between the two cohorts by following up until 2015.
Results
A total of 17241 older patients with CP and 17241 older patients without CP were included in this study. In both cohorts, the mean age (± standard deviation) and female percentage were 73.5 (± 5.7) years and 55.4%, respectively. Spinal disorders (31.9%) and osteoarthritis (27.0%) were the most common causes of CP. Older patients with CP had an increased risk for ACS compared to those without CP after adjusting for all underlying comorbidities (adjusted sub-distribution hazard ratio [sHR] 1.18; 95% confidence interval: 1.07–1.30). The increasement of risk of ACS was more when the follow-up period was longer (adjusted sHR of < 3 years: 1.8 vs. <2 years: 1.75 vs. <1 year: 1.55).
Conclusions
CP was associated with an increased risk of ACS in the older population, and the association was more prominent when the follow-up period was longer. Early detection and intervention for CP are suggested in this population.
Similar content being viewed by others
Background
Chronic pain (CP) is one of the major healthcare problems worldwide, which is defined as a persistent or recurrent pain lasting longer than 3 months by the International Association for the Study of Pain [1, 2]. Previous studies have reported that the prevalence rate of CP ranged from 8.7 to 64.4% [3] and is more prominent in the female population and older people [4]. In addition to the original cause of CP, CP may contribute to impaired functional status, disability, decreased quality of life, increased comorbidities, death, and increased social and economic burdens [5,6,7,8].
CP is a stress on the human body, which may increase the risk of the acute coronary syndrome (ACS) [9,10,11]. A previous study reported that CP increased the rate of ACS events in non-older adults (< 65 years) (adjusted hazard ratio [AHR] 1.2; 95% confidence interval [CI] 1.0 − 1.4) [9]. Older people have a higher risk of CP than the younger population because of multiple comorbidities, including osteoarthritis, spinal disorders, peripheral vascular diseases, osteoporosis, and malignancy [12, 13]. The risk of ACS in older people with CP may be different from that in the younger population. However, the association between CP and ACS in this population remains unclear. Therefore, this study was conducted to clarify it and fill the data gap.
Methods
Data source
This nationwide population-based cohort study was conducted using Taiwan’s National Health Insurance Research Database (NHIRD) [14], which is one of the biggest health databases worldwide. The Taiwan National Health Insurance (NHI) program was launched in 1995, providing coverage to almost the entire Taiwanese population. Hence, the NHIRD can be regarded as representative of the general population in Taiwan [14]. The NHIRD contains complete data of all medical claims covered by the NHI, including outpatient, inpatient, and emergency department services. Many studies based on the NHIRD have provided useful information for clinical care [15]. In addition, the NHIRD provides real-world big data for researchers to investigate many important issues that are difficult to conduct by randomized controlled trials [15].
Study Design, setting, and participants
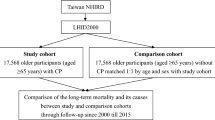
After exclusion of patients with a history of ACS, we identified all older patients (≥ 65 years) with CP between 2001 and 2005 as the study cohort (Fig. 1). The diagnosis of CP was defined as the patient who has used analgesics, including non-steroidal anti-inflammatory drugs (excluding aspirin), acetaminophen, and opioids for more than 3 months [8, 9, 12, 16]. The index date was defined as the date when patients fit the diagnostic criteria for CP, specifically the date when they had used analgesics for a minimum of three months. We identified older patients without CP as the comparison cohort by matching age, sex, and index date with the study cohort at a ratio of 1:1 through sampling without replacement [17]. In consideration of examining more variables, we made the decision to minimize the matched variables, focusing on age, sex, and index date as the key matching criteria. For the subgroup analyses, we employed adjustments for all baseline characteristics presented in Table 1 in the multivariable model to minimize any potential confounding effects. In clinical decision making, it is essential to have information about the difference in ACS risk between older patients with and without CP. This knowledge helps clinicians determine whether to pay more attention to identifying CP and prescribing more intensive pain treatment. Therefore, this study was designed to compare the ACS risk between older patients with CP and those without CP, as it has more practical implications for decision making than knowing the absolute risk.
Definitions of variables
We categorized older patients into three distinct subgroups based on age: 65–74 years (youngest-old), 75–84 years (middle-old), and ≥ 85 years (oldest-old). This classification aligns with the categorization commonly used in the field of geriatric medicine [12, 18, 19]. The underlying comorbidities were identified according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes, as the follows: hypertension (ICD-9-CM: 401–405), diabetes (ICD-9-CM: 250), hyperlipidemia (ICD-9-CM: 272), coronary artery disease (ICD-9-CM: 410–414), malignancy (ICD-9-CM: 140–208), stroke (ICD-9-CM: 436–438), dementia (ICD-9-CM: 290), congestive heart failure (ICD-9-CM: 428), chronic obstructive pulmonary disease (ICD-9-CM: 496), liver disease (ICD-9-CM: 570–576), renal disease (ICD-9-CM: 580–593), connective tissue disease (ICD-9-CM: 710), and mental disorder (ICD-9-CM: 290–302 and 306–319). The causes of CP were spinal disorders (ICD-9-CM: 756.11, 756.12, 720–725, and 737.1–737.4), osteoarthritis (ICD-9-CM: 715), peripheral vascular diseases (ICD-9-CM: 443.8–444.9), gout (ICD-9-CM: 274), osteoporosis (ICD-9-CM: 733.0), headache (ICD-9-CM: 307.81, 784.0, and 346), malignancy (ICD-9-CM: 140–208), diabetic neuropathy (ICD-9-CM: 250.6 and 357.2), rheumatoid arthritis (ICD-9-CM: 714), and pressure ulcer (ICD-9-CM: 707). The underlying comorbidities and causes of CP were defined as diseases with at least one hospitalization or three outpatient visits within the year prior to the index date.
Outcome measures
The primary outcome measure was defined as ACS development during the follow-up period. ACS was identified using the ICD-9-CM of 410 or 411 with at least one hospitalization [12]. All patients were followed from the index date until the development of the ACS, death, or until December 31, 2015 (last date in the database).
Ethical statements
The study was conducted in accordance with the World Medical Association Declaration of Helsinki. This study was approved by the Institutional Review Board of Chi Mei Medical Center, Tainan, Taiwan (Applicant’s No: 11105-E01). Because NHIRD data have been de-identified, the need for written informed consent was waived. The waiver does not affect the rights and welfare of the participants.
Statistical analyses
We used the standardized difference to compare baseline characteristics between the two cohorts [20, 21]. An absolute standardized difference of > 0.10 was considered to indicate imbalance [21]. Based on the non-parametric statistic of Kaplan-Meier methods, we estimated the probabilities of ACS during the follow-up period and performed log-rank tests to compare cumulative incidence curves between the two cohorts. To account for survival bias, we used the Fine and Gray competing risk models to calculate the sub-distribution hazard ratios (sHRs) and corresponding 95% confidence intervals (CIs) of the risk of ACS between the cohorts [22]. We adjusted for potential confounders, including sex, age subgroups, and underlying comorbidities as listed in Table 1 in the multivariable models [23]. Stratified analyses were conducted to investigate potential effect modification across different age subgroups, sex, underlying comorbidities, and follow-up periods. Statistical analyses were performed using SAS 9.4 for Windows (SAS Institute, Inc., Cary, NC, USA). A two-tailed p-value < 0.05 was considered significant.
Results
Patient characteristics
A total of 17241 older patients with CP and the same number of older patients without CP were identified in this study (Table 1). Following matching, no significant difference was found in the age and sex between the two cohorts. The mean age (± standard deviation) was 73.5 (± 5.7) years. The percentage of the subgroup aged 65–74 years was the highest (58.6%), followed by the subgroups aged 75–84 years (36.9%) and ≥ 85 years (4.6%). Among older patients with CP, there were more women than men (55.4% vs. 44.6%). Compared with older patients without CP, older patients with CP had a higher prevalence of underlying comorbidities, including hypertension, diabetes, hyperlipidemia, coronary artery disease, malignancy, stroke, congestive heart failure, chronic obstructive pulmonary disease, liver diseases, renal diseases, and mental disorders (standardized difference > 0.10).
Causes of CP
The most common cause of CP was spinal disorders (31.9%), followed by osteoarthritis (27.0%), peripheral vascular diseases (17.2.%), gout (10.9%), osteoporosis (10.4%), headache (8.8%), and malignancy (5.9%) (Table 2). The subgroup aged ≥ 85 years had a higher prevalence of peripheral vascular diseases, osteoporosis, and pressure ulcer, but a lower prevalence of spinal disorders, headache, diabetic neuropathy, and rheumatoid arthritis than younger patients.
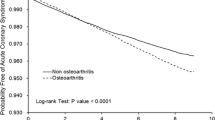
Comparison of subsequent ACS between the two cohorts
The Kaplan–Meier method revealed that the cumulative incidence of ACS in older patients with CP was significantly higher than in those without CP during the follow-up period (log-rank test, p < 0.0001) (Fig. 2). The competing risk survival analysis revealed that older patients with CP had a higher rate of developing ACS than those without CP in both univariable (crude sHR 1.33; 95% CI 1.21–1.46) and multivariable models (adjusted sHR 1.18; 95% CI 1.07–1.30) (Table 3). Stratified analyses revealed that the elevated risk of ACS in older patients with CP was more prominent in the subgroup aged 65–74 years (adjusted sHR 1.21; 95% CI 1.06–1.39) compared to the subgroups aged 75–84 years (adjusted sHR 1.13; 95% CI 0.97–1.31) and ≥ 85 years (adjusted sHR 1.06; 95% CI 0.66 − 1.70). Furthermore, the increased rate of ACS events was statistically significant in both male (adjusted sHR 1.15; 95% CI 1.00 − 1.32) and female (adjusted sHR 1.21; 95% CI 1.05 − 1.39) patients. Additionally, patients with comorbidities of hypertension showed a heightened risk of ACS (adjusted sHR 1.18; 95% CI 1.04 − 1.34), as did those with chronic obstructive pulmonary disease (adjusted sHR 1.32; 95% CI 1.04 − 1.68). The risk of ACS increased with longer follow-up periods (adjusted sHR 1.80 for follow-up < 3 years vs. adjusted sHR 1.75 for follow-up < 2 years vs. adjusted sHR 1.55 for follow-up < 1 year).
Discussion
This nationwide population-based cohort study reported that older patients with CP were at a higher risk of subsequent ACS than those without CP, similar to that in a previous study of the non-older population [9]. The increased risk of ACS was more prominent in the subgroup aged 65 − 74 years than in older age subgroups and in the group with a longer follow-up period than in those with a shorter follow-up period.
Our data fills the gap for older population about the association between CP and ACS in the literature. In addition, our study presented that the increased risk of ACS was more prominent in the group with a longer follow-up period, which indicates a possible dose–response relationship. A population-based cross-sectional study in New Zealand reported that cardiovascular diseases, including heart attack, heart failure, and other heart diseases, were independently associated with CP after adjusting for demographic factors and chronic physical conditions (odds ratio [OR] 1.6; 95% CI 1.3–1.9) [24]. Another large-scale population-based cohort study of extended families in Scotland also reported an increased co-occurrence of CP and cardiovascular disease (OR 4.19; 95% CI 3.64 − 4.82) [25]. A population-based cohort of adults aged < 65 years in Taiwan reported a significant association between CP and the risk of acute myocardial infarction (AHR 1.2; 95% CI 1.0 − 1.4). However, these aforementioned studies did not investigate the risk of ACS in older people. Our results were compatible with the findings of those studies and help complete a whole picture of CP and ACS in the total population.
One of the possible mechanisms for the increased risk of ACS is the effect of stress from CP. In response to stress, the hypothalamic–pituitary–adrenal (HPA) axis and the sympathetic nervous system release cortisol and catecholamines, which produce a negative effect on the vascular system by inducing high blood pressure, inflammation, and endothelial dysfunction [11, 26]. The dysregulation of the HPA axis may contribute to cardiovascular disorders, including ACS, left ventricular dysfunction, dysrhythmia, and atherosclerosis [10]. Furthermore, CP may cause a reduction of daily activities, sleep disturbance, depression, and cognitive decline [16, 27,28,29], which are also associated with increased cardiovascular diseases and death. However, the relationship between CP and cardiovascular diseases is complex and interdependent because of multiple physiologic, psychological, and even social factors [27]. Further studies are necessary to examine the exact underlying mechanisms.
In our study, we found that the increased risk for ACS was more prominent in the subgroup aged 65 − 74 years than in the subgroups aged 75 − 84 and ≥ 85 years. The possible explanation for the difference is that older people have more underlying comorbidities, such as hypertension, diabetes, and hyperlipidemia, responsible for cardiovascular diseases. Therefore, the combined effect decreases the role of CP played in the development of ACS.
This study has demonstrated that, while not all comorbidities significantly influence the association between CP and the risk of ACS, hypertension and chronic obstructive pulmonary disease do. These results suggest that individuals with hypertension or chronic obstructive pulmonary disease and CP may face a heightened risk of ACS compared to those with other comorbidities. The potential interaction between hypertension, chronic obstructive pulmonary disease, CP, and ACS has emerged as a novel finding, warranting further investigation into the underlying mechanisms.
The major strength of this study is attributed to its nationwide population-based design with a large sample size. In addition, this study, for the first time, clarified the association between CP and ACS in the older population. Despite the aforementioned strengths, it has some limitations. First, the claims-based database could not provide clinical information on some potential confounding factors, such as lifestyle, body mass index, smoking, and results of clinical tests. Nevertheless, we adjusted common underlying comorbidities related to these potential confounders to minimize the confounding effects. Second, there was no defined diagnostic code of CP in the NHIRD, so we used “analgesics usage for more than 3 months” as our criteria to identify CP. The diagnosis of CP may be underestimated, and the duration and severity of CP could not be further analyzed. Third, although we defined the use of analgesics as a criterion for CP, it is important to note that different types of analgesics may be associated with an increased risk of ACS. Previous epidemiological research conducted by our team on the older population with CP in Taiwan revealed that the most used analgesics were NSAIDs (89.1%), acetaminophen (77.5%), and opioids (10.2%) [12]. However, due to the frequent combination or alternation of analgesics, it becomes challenging to analyze the specific impact of a single type of analgesic on outcomes. As the primary aim of this study was to investigate the influence of CP on the risk of ACS in older patients, exploring the relationship between analgesics and ACS, including their specific types, may deviate from the focus of this study. Nevertheless, we acknowledge the importance of this aspect and plan to investigate the association between analgesic types and ACS in future research. Forth, the results may not be generalized to other nations because of the differences in race, culture, and medical insurance. Finally, we could not establish a causal relationship between CP and ACS because of the complex interactions and the observational study design. Further studies are warranted to delineate the issues mentioned above in the future.
Conclusions
This nationwide population-based cohort study revealed a positive association between CP and ACS in the older population, especially in the longer follow-up period. The result fills the gap for older people in this issue. Possible mechanisms are as follows: CP causes stress, reduced daily activities, sleep disturbance, depression, and cognitive decline, which contributes to the increased risk of ACS. Therefore, we suggest a more aggressive control of CP in the older population to decrease the risk of subsequent ACS. Further studies, including recruiting more possible confounders, more precise diagnosis criteria of CP, and validation in other nations, are warranted in the future.
Data Availability
Data are available from the NHIRD published by the Taiwan NHI Bureau. Due to legal restrictions imposed by the government of Taiwan in relation to the “Personal Information Protection Act,” data cannot be made publicly available. Requests for data can be sent as a formal proposal to the NHIRD (http://nhird.nhri.org.tw).
Abbreviations
- CP:
-
chronic pain
- ACS:
-
acute coronary syndrome
- AHR:
-
adjusted hazard ratio
- sHR:
-
sub-distribution hazard ratio
- CI:
-
confidence interval
- NHIRD:
-
National Health Insurance Research Database
- NHI:
-
National Health Insurance
- ICD-9-CM:
-
International Classification of Diseases, Ninth Revision, Clinical Modification
- OR:
-
odds ratio
- HPA:
-
hypothalamic–pituitary–adrenal
References
Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, Keefe FJ, Mogil JS, Ringkamp M, Sluka KA, et al. The revised International Association for the study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976–82.
Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, Cohen M, Evers S, Finnerup NB, First MB, et al. A classification of chronic pain for ICD-11. Pain. 2015;156(6):1003–7.
Steingrimsdottir OA, Landmark T, Macfarlane GJ, Nielsen CS. Defining chronic pain in epidemiological studies: a systematic review and meta-analysis. Pain. 2017;158(11):2092–107.
Fayaz A, Croft P, Langford RM, Donaldson LJ, Jones GT. Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open. 2016;6(6):e010364.
Mayer S, Spickschen J, Stein KV, Crevenna R, Dorner TE, Simon J. The societal costs of chronic pain and its determinants: the case of Austria. PLoS ONE. 2019;14(3):e0213889.
Stockbridge EL, Suzuki S, Pagan JA. Chronic pain and health care spending: an analysis of longitudinal data from the Medical Expenditure Panel Survey. Health Serv Res. 2015;50(3):847–70.
Smith D, Wilkie R, Uthman O, Jordan JL, McBeth J. Chronic pain and mortality: a systematic review. PLoS ONE. 2014;9(6):e99048.
Tsai MH, Tsay WI, Her SH, Ho CH, Chen YC, Hsu CC, Wang JJ, Huang CC. Long-term mortality in older adults with chronic pain: a nationwide population-based study in Taiwan. Eur Geriatr Med. 2019;10(5):777–84.
Chung KM, Ho CH, Chen YC, Hsu CC, Chiu CC, Lin HJ, Wang JJ, Huang CC. Chronic Pain increases the risk for major adverse Cardiac and cerebrovascular events: a Nationwide Population-Based study in Asia. Pain Med. 2020;21(9):1985–90.
Brotman DJ, Golden SH, Wittstein IS. The cardiovascular toll of stress. Lancet. 2007;370(9592):1089–100.
McBeth J, Chiu YH, Silman AJ, Ray D, Morriss R, Dickens C, Gupta A, Macfarlane GJ. Hypothalamic-pituitary-adrenal stress axis function and the relationship with chronic widespread pain and its antecedents. Arthritis Res Ther. 2005;7(5):R992–r1000.
Huang YL, Tsay WI, Her SH, Ho CH, Tsai KT, Hsu CC, Wang JJ, Huang CC. Chronic pain and use of analgesics in the elderly: a nationwide population-based study. Arch Med Sci. 2020;16(3):627–34.
Reid MC, Eccleston C, Pillemer K. Management of chronic pain in older adults. BMJ. 2015;350:h532.
Sung SF, Hsieh CY, Hu YH. Two decades of Research using Taiwan’s National Health Insurance Claims Data: bibliometric and text mining analysis on PubMed. J Med Internet Res. 2020;22(6):e18457.
Hsieh CY, Su CC, Shao SC, Sung SF, Lin SJ, Kao Yang YH, Lai EC. Taiwan’s National Health Insurance Research Database: past and future. Clin Epidemiol. 2019;11:349–58.
Kao PH, Jang FL, Ho CH, Chen YC, Hsu CC, Lin HJ, Wang JJ, Huang CC. Chronic Pain increases the risk of dementia: a Nationwide Population-Based Cohort Study. Pain Physician. 2021;24(6):E849–e856.
Heide-Jørgensen U, Adelborg K, Kahlert J, Sørensen HT, Pedersen L. Sampling strategies for selecting general population comparison cohorts. Clin Epidemiol. 2018;10:1325–37.
Alterovitz SS, Mendelsohn GA. Relationship goals of middle-aged, young-old, and old-old internet daters: an analysis of online personal ads. J Aging Stud. 2013;27(2):159–65.
Lee SB, Oh JH, Park JH, Choi SP, Wee JH. Differences in youngest-old, middle-old, and oldest-old patients who visit the emergency department. Clin Exp Emerg Med. 2018;5(4):249–55.
Schober P, Bossers SM, Schwarte LA. Statistical significance Versus clinical importance of observed effect sizes: what do P values and confidence intervals really represent? Anesth Analg. 2018;126(3):1068–72.
Schulte PJ, Mascha EJ. Propensity score methods: theory and practice for Anesthesia Research. Anesth Analg. 2018;127(4):1074–84.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509.
Sjölander A, Greenland S. Ignoring the matching variables in cohort studies - when is it valid and why? Stat Med. 2013;32(27):4696–708.
Dominick CH, Blyth FM, Nicholas MK. Unpacking the burden: understanding the relationships between chronic pain and comorbidity in the general population. Pain. 2012;153(2):293–304.
van Hecke O, Hocking LJ, Torrance N, Campbell A, Padmanabhan S, Porteous DJ, McIntosh AM, Burri AV, Tanaka H, Williams FM, et al. Chronic pain, depression and cardiovascular disease linked through a shared genetic predisposition: analysis of a family-based cohort and twin study. PLoS ONE. 2017;12(2):e0170653.
Keller-Wood M. Hypothalamic-pituitary–adrenal Axis-Feedback Control. Compr Physiol. 2015;5(3):1161–82.
Da Silva JAP, Geenen R, Jacobs JWG. Chronic widespread pain and increased mortality: biopsychosocial interconnections. Ann Rheum Dis. 2018;77(6):790–2.
Macfarlane GJ, Barnish MS, Jones GT. Persons with chronic widespread pain experience excess mortality: longitudinal results from UK Biobank and meta-analysis. Ann Rheum Dis. 2017;76(11):1815–22.
Meijer A, Conradi HJ, Bos EH, Anselmino M, Carney RM, Denollet J, Doyle F, Freedland KE, Grace SL, Hosseini SH, et al. Adjusted prognostic association of depression following myocardial infarction with mortality and cardiovascular events: individual patient data meta-analysis. Br J Psychiatry. 2013;203(2):90–102.
Acknowledgements
We thank Enago for the English revision.
Funding
This study was supported by the Grant Physician-Scientist 11001, Grant CMFHR10978, and Grant CMHCR112029 from the Chi Mei Medical Center.
Author information
Authors and Affiliations
Contributions
YCL, CTW, and CC Huang designed and conceived this study. CHH and YCC performed the statistical analysis. CC Hsu and HJL provided professional suggestions. All authors wrote the manuscript and also read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
This study was approved by the Institutional Review Board of Chi Mei Medical Center, Tainan, Taiwan (Applicant’s No: 11105-E01). Because NHIRD data have been de-identified, the need for written informed consent was waived. The waiver does not affect the rights and welfare of the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, YC., Ho, CH., Chen, YC. et al. Association between chronic pain and acute coronary syndrome in the older population: a nationwide population-based cohort study. BMC Geriatr 23, 708 (2023). https://doi.org/10.1186/s12877-023-04368-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04368-1