Abstract
Background
Unhealthy lifestyle behaviours such as smoking, high alcohol consumption, poor diet or low physical activity are associated with morbidity and mortality. Public health guidelines provide recommendations for adherence to these four factors, however, their relationship to the health of older people is less certain.
Methods
The study involved 11,340 Australian participants (median age 7.39 [Interquartile Range (IQR) 71.7, 77.3]) from the ASPirin in Reducing Events in the Elderly study, followed for a median of 6.8 years (IQR: 5.7, 7.9). We investigated whether a point-based lifestyle score based on adherence to guidelines for a healthy diet, physical activity, non-smoking and moderate alcohol consumption was associated with subsequent all-cause and cause-specific mortality.
Results
In multivariable adjusted models, compared to those in the unfavourable lifestyle group, individuals in the moderate lifestyle group (Hazard Ratio (HR) 0.73 [95% CI 0.61, 0.88]) and favourable lifestyle group (HR 0.68 [95% CI 0.56, 0.83]) had lower risk of all-cause mortality. A similar pattern was observed for cardiovascular related mortality and non-cancer/non-cardiovascular related mortality. There was no association of lifestyle with cancer-related mortality.
Conclusions
In a large cohort of initially healthy older people, reported adherence to a healthy lifestyle is associated with reduced risk of all-cause and cause-specific mortality. Adherence to all four lifestyle factors resulted in the strongest protection.
Similar content being viewed by others
Introduction
Common unhealthy lifestyle behaviours, such as smoking [1], high alcohol consumption [2], poor dietary patterns [3] or low physical activity [4], have each been associated with mortality in middle to older-aged adults [5]. As a result, public health authorities in various countries have provided recommendations related to these behaviours in order to preserve good health. However, it is less certain whether reported adherence to these recommendations is associated with appreciable benefit among older people [6].
Previous studies have suggested that a combination of healthy lifestyle behaviours is associated with the strongest improvement in healthy longevity [7] and reduced risk of future mortality [8]. A meta-analysis of 15 studies including 531,804 participants from the United States, Europe, China and Japan (mean follow-up 13.24 years) reported that up to 66% of deaths could be attributable to a combination of unhealthy lifestyle characteristics including smoking, high alcohol consumption, physical inactivity and a poor diet [8,9,10,11].
Currently, the studies underpinning health guidelines and lifestyle recommendations for the wider population are mainly derived from middle-aged cohorts (≥ 40 to < 60 ± 5 years at baseline). The few studies focussing exclusively on older people (i.e. ≥ 70 ± 5 years) have limited sample-sizes and/or focussed exclusively on all-cause mortality while not reporting the relationship to cause specific mortality [10, 12, 13]. Clarifying the relationship between adherence and advice concerning lifestyle behaviours and mortality may help prioritise preventive advice and policy recommendations among progressively aging populations.
The Aspirin in Reducing Events in the Elderly (ASPREE) study, a cohort of initially healthy older people, is uniquely suited to investigate whether a combination of current healthy lifestyle behaviours in community-dwelling older people is associated with a prolonged life span and reduced cause specific mortality [14].
Methods
Study population and trial design
This analysis is based on data from Australian participants in the ASPREE (n = 16,703), and ASPREE trial sub-sets: the ASPREE-eXTension (ASPREE-XT) study (n = 14,849) [14,15,16] and the ASPREE Longitudinal Study of Older Persons (ALSOP) sub-study (n = 14,892) [17]. ASPREE was a large, randomised, double-blind, placebo-controlled trial investigating the efficacy of 100 mg of aspirin on disability free survival in healthy men and women who were 70 years of age or older. Details of ASPREE and the primary results of the study have been published previously [14,15,16]. Briefly, all participants were required to be in good health, with no prior cardiovascular disease events, dementia or major physical disability and expected to survive for at least five years at the time of enrolment. All participants provided written informed consent.
Following completion of the ASPREE clinical trial (2010 – June 2017), the ASPREE-XT observation follow-up period commenced (ongoing). Data in this analysis includes that collected up to the participants’ second annual ASPREE-XT visit (2020). Baseline was defined by the completion date of the ASPREE baseline questionnaire which took place between March 2010 to December 2014. ASPREE and ASPREE-XT were approved by the local ethics committees and is registered on clinicaltrials.gov on 24/12/2009 (NCT01038583).
The ALSOP sub-study is a longitudinal cohort study involving approximately 90% of the Australian participants in ASPREE and ASPREE-XT. Details of the ALSOP study methodology and baseline characteristics have been published elsewhere [17]. Participation involved voluntary completion of a set of medical and social questionnaires, administered within three to six months (May 2010 – March 2015) of ASPREE study enrolment, and again after three years of ASPREE participation.
Lifestyle score
The lifestyle score was constructed based on four modifiable lifestyle factors (alcohol consumption, smoking status, physical activity and diet) known to be associated with chronic disease onset [10, 18,19,20,21,22]. The score was created by allocating one-point for adherence to each of the 4 lifestyle behaviours defined on the basis of national and international recommendations (Table S1). The lifestyle score ranged from 0 to 4, with higher scores indicating higher adherence to healthy lifestyle recommendations. The lifestyle score was also subsequently categorised in 3 groups, as unfavourable (lifestyle score ≤ 1), moderate (lifestyle score = 2), and favourable (lifestyle score ≥ 3).
Assessment of lifestyle factors
Full details of the assessment of the lifestyle factors and classification is described in detail in Table S1. Briefly, baseline smoking status was categorised as either current or no current smoking (including former smokers). A previous study using ASPREE data found that moderate alcohol consumption was associated with a reduced risk of CVD and all-cause mortality when compared to those reporting low/none or high levels, as reported previously [2, 23]. In the current analyses, participants were therefore categorised as either having moderate alcohol consumption or not. Cut-off’s were defined by those reporting between 51–100 g of alcohol per week (approximating to an average of 0.7 to 1.4 standard Australian alcoholic beverages a day) at baseline, synonymous to previous cut-offs [23] and cut-offs informed by current NHMRC guidelines of “no more than 10 standard drinks a week or no more than 4 standard drinks on any one day” [24]. Current NHMRC guidelines also state “the less you drink, the lower your risk of harm from alcohol”, hence, we acknowledge that cut-offs for alcohol consumption used here do not strictly align with the current guidelines. For physical activity, the World Health Organization (WHO) and Australian government guidelines for adults aged ≥ 65 years recommend at least 30 min of moderate activity at least five days per week [25, 26]. Therefore, participants were categorised into either engaging in ‘no or light activity’; or 'moderate or vigorous activity’ based on their questionnaire responses at baseline. Dietary data was not available at baseline; therefore, year-three diet was utilised instead. This was assessed by a 49-item simple food frequency questionnaire, covering major food groups. Consumption was assessed over five predefined categories of responses ranging from “never/rarely” to “every day or several times a day”. A healthy diet was based on the consumption of at least four of seven commonly eaten food groups, following recommendations on dietary priorities for cardiometabolic health [27], and previously used elsewhere [21].
Outcomes
Methodological details on the ascertainment of all-cause and categorisation of cause-specific mortality have been published [15, 16] and further detail is provided in Table S2. Briefly, all deaths and underlying cause were adjudicated by clinicians masked to treatment allocation and confirmed by review of at least two independent sources such as family report, clinical record or public death notice, and via a final cross check through linkage with the National Death Indices. The primary outcome was all-cause mortality. Secondary outcomes included cancer-related mortality, CVD-related mortality (including stroke, coronary and cardiovascular related death) and non-CVD/non-cancer mortality (the latter referred to as ‘other’ mortality).
Statistical analyses
Participants were included in the current analysis if they had completed both baseline and year-three ALSOP questionnaires (Fig. 1). Baseline characteristics were reported using descriptive statistics and stratified by the lifestyle score categories (unfavourable, moderate, favourable). Comparison of baseline characteristics across categories was made using the χ2 test, analysis of variance (ANOVA) or Kruskal–Wallis test, as appropriate.
Cox proportional hazards models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between the lifestyle score and all-cause and cause-specific HRs for each of cancer, CVD and ‘Other’ mortality. Competing risk Kaplan–Meier curves were plotted to illustrate the cumulative effect of lifestyle categories on all-cause and cause-specific mortality. Analyses were adjusted for age (continuous), sex (male/female), aspirin treatment allocation (100 mg enteric coated aspirin/placebo) (model 1), education (≥ 12-years/ < 12-years), living status (alone/with others), and socioeconomic status (IRSAD deciles, continuous) (model 2). Full details on the ascertainment of these study measurements have been described in detail previously [14, 17].
To investigate whether a priori selected factors modified the association between the lifestyle score and all-cause mortality, we performed analyses stratified by median age (≥ 74/ < 74 years), sex (male/female), education (≥ 12-years/ < 12-years), Body Mass Index (BMI) (≥ 25 vs < 25 kg/m2), baseline diagnosis of type-2 diabetes (yes/no) and baseline diagnosis of hypertension (yes/no) and aspirin treatment allocation. Interaction was tested by including a cross-product term along with the main effect terms in the models. In exploratory analyses, we investigated the association between the individual lifestyle factors with all-cause and cause-specific mortality and combinations of individual lifestyle factors with all-cause mortality.
In sensitivity analyses we explored alternative definitions of adherence to the lifestyle factors to assess whether significant differences in associations with all-cause mortality would result. For example, there is debate over whether the ‘protective’ effect of moderate alcohol consumption is real or spurious due to residual confounding [28]. Therefore, we created an alternative variable, allocating participants to either moderate/low/never vs high. This variable was associated with all-cause mortality alone and as part of the lifestyle score. Second, we excluded former alcohol consumers and former smokers (who quit < 15-years ago), who may have stopped due to various health reasons, possibly introducing bias from reverse causality. Third, owing to the need to use the ‘year 3’ diet questionnaire in the principal analysis, in sensitivity analyses we tested the association between the same lifestyle score, but now including year-three smoking, alcohol, physical activity and diet, again with all-cause mortality. Finally, as 1,122 participants were excluded due to missing or incorrectly completed physical activity data, we compared differences in key characteristics (age, sex, education, BMI, T2D, hypertension, aspirin treatment allocation, living status, socioeconomic status and frailty), between these individuals and those included in the final study sample.
Statistical analyses were conducted using Stata (version 17; College Station, TX: StataCorp LLC). A two-sided p-value of ≤ 0.05 was considered statistically significant. The proportional hazards assumption was assessed and met using log–log Kaplan–Meier survival plots.
Results
A total of 11,340 Australian participants were included in the current analysis, and followed for a median of 6.8 years (IQR: 5.7, 7.9) years. At study entry, the median age was 73.9 (IQR 71.7–77.3) years and 54.2% were female. A total of 702 (6.2%) participants died during the follow-up period.
Baseline characteristics
Baseline characteristics of included participants according to the lifestyle score categories as well as by all-cause mortality are shown in Table 1 and Table S3, respectively. Overall, 20.4% of participants adhered to one or no lifestyle factors (unfavourable lifestyle), 44.2% of participants adhered to two lifestyle factors (moderate lifestyle) and 35.3% adhered to three or four lifestyle factors (favourable lifestyle). There was a significantly higher proportion of younger participants, females, those living with others and those with a higher education in the favourable lifestyle group. When compared to the overall ASPREE cohort there were a higher proportion of those who were frail, reporting depressive symptoms and on statins (Table S3).
A higher proportion of individuals with vascular risk factors (i.e. hypertension, diabetes, dyslipidaemia), who were on antihypertensives and statins, who were pre-frail/frail, with depressive symptoms and/or higher BMI, waist circumference and systolic blood pressure were in the unfavourable lifestyle group. There were no differences across lifestyle groups based on aspirin treatment allocation. Description and prevalence of the lifestyle factors in the population are shown in Table S1. With regard to adherence to healthy lifestyle factors, 97.5% reported no current smoking, 22.3% reported moderate alcohol consumption, 33.3% met the ‘healthy diet’ criteria and 66.9% of participants reported engagement in weekly moderate/vigorous physical activity.
Association between lifestyle and mortality
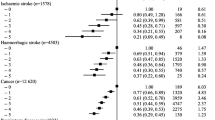
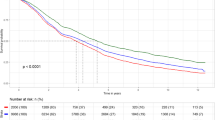
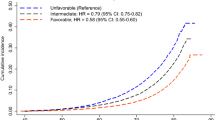
Rates of all-cause mortality and cause-specific mortality are shown in Tables 2, 3 and Fig. 2. For all-cause mortality, compared to participants with no or one healthy lifestyle factors, the multivariable adjusted HRs were 0.73 (95% CI 0.61, 0.88) for two factors, 0.70 (95% CI 0.57, 0.86) for three factors, and 0.56 (95% CI 0.37, 0.86) for four factors, p-trend < 0.0001 (Table 2; Fig. 2A). When evaluated as a continuous variable, each additional lifestyle factor was associated with a 16% lower risk of all-cause mortality (HR for a one-point increase: 0.84 [95% CI 0.76, 0.92]). A similar association was observed for CVD-related (Table 3, Fig. 2B) and ‘Other’ mortality (Table 3, Fig. 2C).
Cumulative Incidence of all-cause and cause specific mortality by lifestyle categories. Shown is the cumulative incidence of death due to any cause and death according to major underlying causes (cancer, cardiovascular disease and ‘other’ non-CVD/non-cancer cause). For each cause of death, the cumulative incidence was based on a competing-risks model, stratified by lifestyle categories, with the remaining causes of death as competing events. Abbreviations: Unfav., unfavourable lifestyle category; Mod., moderate lifestyle category; Fav., favourable lifestyle category. Years = years since baseline visit
The same dose–response association was observed when the lifestyle scores were divided into three categories as shown in Table 2, Fig. 2A (all-cause mortality) and Table 3, Fig. 2B-C (cause-specific mortality). In multivariable adjusted models, compared with those in the unfavourable lifestyle group, individuals in the moderate lifestyle group had a 27% lower risk of all-cause mortality [HR 0.73 (95% CI 0.61, 0.88]), and individuals in the favourable lifestyle group had a 32% lower risk of all-cause mortality (HR 0.68 [95% CI 0.56, 0.83]), p-trend < 0.001 (Table 2; Fig. 2A). In absolute terms, among 1000 individuals in the unfavourable lifestyle group, 39 more deaths occurred during the median follow-up period of 6.8 years compared with the favourable lifestyle group.
With regard to risk of CVD and ‘Other’ mortality, the same dose–response association was observed, with larger effect size for CVD mortality (Table 3; Fig. 2B-C). There was no association between lifestyle groups and cancer-related mortality (Table 3; Fig. 2D).
Additional analyses
Additional analyses of specific lifestyle characteristics are presented in Tables S4-S7. Each individual lifestyle factor was associated with a lower risk of all-cause mortality, CVD mortality, cancer mortality and ‘Other’ mortality. Specifically, effect sizes of each lifestyle factor on risk of all-cause mortality were highest and statistically significant for smoking status (HR 0.42 [95% CI 0.30, 0.59]) and physical activity (HR 0.84 [95% CI 0.72, 0.98]), with non-significant trends for alcohol consumption (HR 0.92 [95% CI 0.62, 1.37]) and diet (HR 0.90 [95% CI 0.76, 1.06]). Similar trends were observed for cause-specific mortality.
Further analyses according to different combinations of two, three and four healthy lifestyle factors prevalent in at least 2% of the population compared to no or one healthy lifestyle factors are shown in Table S8. None of the observed associations were as protective of all-cause mortality as the combination of 4 factors (HR 0.57 [95% CI 0.37, 0.86]).
Table S9 shows results of the stratified analyses by selected health, demographic and anthropometric factors on the association between the lifestyle score categories and all-cause mortality. No statistically significant differences were observed in the associations between the healthy lifestyle score categories and all-cause mortality by age, sex, education, BMI, diabetes, hypertension and aspirin treatment.
Sensitivity analyses
Results from the various sensitivity analyses are presented in the Tables S10-S13, and page 14 of the supplement. Briefly, excluding former smokers/drinkers (Table S10), the alternative categorisation of alcohol consumption (supplement p 14) and the alternative lifestyle score (Table S11 and S13) did not alter the results for all-cause mortality Multivariable adjusted HRs on the association between the year-three lifestyle score categories and risk of all-cause mortality remained equivalent (Table S13). There were no differences in characteristics between those with missing physical activity data (n = 1,122) and the included sample (not reported).
Discussion
In this cohort of 11,340 community dwelling healthy older Australians, we examined the association between a healthy lifestyle score and all-cause mortality, cancer-related mortality, CVD-related mortality and ‘other’ causes over a median follow-up time of 6.8 years (IQR: 5.7, 7.9). We found that a healthy lifestyle score at baseline, comprising of four common and potentially modifiable lifestyle factors (non-smoking, moderate alcohol consumption, a healthy dietary pattern and physical activity) was associated with prolonged lifespan in a dose–response relationship, such that each additional lifestyle factor was associated with a 16% lower risk of all-cause mortality, 25% lower risk of CVD mortality and 22% lower risk of ‘Other’ mortality. The current data found no association between lifestyle groups and cancer-related mortality.
This is one of the largest and most comprehensive studies, conducted exclusively within community dwelling older people, reporting the association between a lifestyle composite score based on adherence to international health behaviour recommendations and all-cause plus cause-specific mortality. The results are largely in agreement with previous reports investigating different combinations of healthy lifestyle characteristics. A similar study of older Chinese people (n = 11,224, aged 65–90 years) reported that, compared to those without any unhealthy factors, those who had a high BMI, poor sleep, unhealthy diet, no physical activity, consumed alcohol and currently smoked were 1.34 (95% CI 1.02, 1.76) times more likely to die from any cause over a ten-year follow-up period [13]. Another 18-year follow-up study of Swedish older adults (75 + years of age; n = 1,810) reported a median additional survival of 5.4 years among those who had a healthy BMI, never smoked or drank alcohol, engaged in leisure activities and moderate levels of physical activity versus those who did not [12]. “The healthy aging: a longitudinal study in Europe” (HALE) study (n = 1,507) reported that 70 to 90-year-old community-dwelling people who did not smoke, consumed a Mediterranean diet, reported moderate alcohol consumption and was physically active had a 50% lower rate of all-cause and cause-specific mortality over 10-years, including CVD and cancer-related mortality [10]. Similar protective effects of a composite lifestyle score, typically including at least diet, physical activity, smoking and alcohol, have been reported among middle-aged cohorts from different counties including Japan [29], China [11], United States of America (USA) [9], Australia [30] and the United Kingdom (UK) [31].
Results reported here and previously, provide compelling evidence to suggest that individuals reporting a healthy lifestyle in older age have a significantly reduced risk of earlier mortality. The results also demonstrate that current international recommendations for moderate physical activity, no smoking, a healthy dietary pattern and moderate alcohol consumption may still provide a useful predictor of longevity among this older aged cohort.
We found no relationship between a healthy lifestyle on risk of overall cancer-related death, which is contrary to findings previously reported in the HALE study as well as among studies of younger cohorts [10]. Nonetheless, the HALE study was conducted via survey only and among a demographic born up to 40-years earlier than ASPREE participants. It is possible that the lack of a broader link with cancer reflects the very small percentage of current smokers in ASPREE. Should a larger proportion of ASPREE participants be current smokers, we may observe a larger effect size on the association between the lifestyle score and cancer-related mortality. A longer follow-up time, or considering earlier smoking behaviour, could also reveal stronger effects of lifestyle on cancer-related mortality.
Some methodological points may impact the conclusions of this study. In order to construct the healthy lifestyle score, we dichotomised each lifestyle factor according to pre-defined cut-off points. Different threshold values may have resulted in different risk estimates, being especially relevant to cause specific mortality. Indeed, one study reported an association between vigorous physical activity and reduced risk of cancer related death, whereas, moderate activity was associated with CVD related death [32]. Nonetheless, the choice of cut-off was largely based on national and international public health recommendations [24,25,26,27]. In sensitivity analyses we trialled different cut-offs and multi-levels in association with all-cause mortality but the results remained largely unchanged (Tables S11, S12 and supplement p 14). The approach of designating compliance versus non-compliance allows a simple objective classification to assess the health impact of lifestyle and can inform a clear public health message. Future modifications of this approach may involve differential weighting of the health impact of each lifestyle measure, considering both mid-life and later-life behaviour while exploring alternative risk cut-off’s for cause specific mortality.
Our categorisation of moderate alcohol consumption was only partly based on the NHMRC guidelines stating no more than 10 standard drinks per week and no more than 4 standard drinks in one day. The guidelines also state that “the less you drink, the lower your risk of harm for alcohol”. We acknowledge our score does not fully encompass those falling within the current recommendations (i.e. we have categorised those reporting low/no consumption as higher risk). Nonetheless, the score is informed by recent data indicating a ‘U’ shaped association between alcohol consumption and mortality in older adults, as also reported within ASPREE.
Owing to the absence of baseline dietary data, we utilised year-three dietary data as an alternative replacement within the baseline lifestyle score. It is not certain whether dietary behavior had significantly changed over this three-year period. Dietary changes can occur in older people due to factors such as oral health, income, marital status, medication or change of residence [33]. Nonetheless, as healthy lifestyle habits are characteristic of a person’s way of living, and given ASPREE is an especially healthy cohort, majority of participants were unlikely to show a substantial change in general dietary habits over a three-year period [34]. Furthermore, the year-three lifestyle score was associated with all-cause and cause-specific mortality with similar effect size to associations between baseline lifestyle and mortality, sanctioning this assumption.
Finally, given we do not have detailed information about mid-life lifestyle behaviour in the ASPREE cohort, we cannot confirm whether observed mortality risks are determined by behaviour earlier in life. Healthy lifestyle behaviours in older age may reflect a long-standing approach to healthy living which, in turn, may be driving these observations. Our results still, however, highlight the relevance of identifying healthy lifestyle factors as predictors of likely future mortality, even among already healthy older people.
Strengths and limitations
There are several strengths of our study. ASPREE is a well characterised, large and contemporary cohort of older people who had reached age 70-years or more in relatively good health [17]. Furthermore, rigorous methods for the ascertainment of cause-specific mortality ensured highly accurate endpoints. The investigation of not only all-cause but cause-specific mortality is a further strength.
There are also several potential limitations. First, the ASPREE cohort is comprised of initially healthy volunteers for a clinical trial who are more likely to be attentive to maintaining a healthy lifestyle, hence, is likely to represent a healthier sample of older people compared with the general population. Second, the cohort is largely Caucasian, educated and drawn from communities with access to universal healthcare as reflected by the extensive use of preventive medications including statins (in 30%) and antihypertensive agents (in 51%). Therefore, our results may not be applicable among other socioeconomic and ethnic groups as well as among those residing in lower- to middle-income countries.
Third, due to the progressive nature of noncommunicable disease leading to death, with declining function often preceding and possibly influencing lifestyle behaviour, we cannot rule out reverse causality as a partial explanation for these observations.
Fourth, the use of subjective measures will incur some risk of self-reporting bias and a onetime assessment may not accurately represent one’s habitual lifestyle. Fifth, the questions used to measure physical activity did not provide in-depth detail on duration and frequency (i.e. how many times per week and for how long). This information may be especially relevant when investigating cause-specific mortality [32]. Although it is beyond the scope of the current study, differential risk thresholds for cause-specific mortality warrants further evaluation.
Finally, although potential confounders were considered in multivariable analyses, residual confounding cannot be ruled out. Furthermore, other unmeasured lifestyle and environmental factors may also play a role in determining risk of death. Nonetheless, demonstrating that these four common lifestyle behaviors are associated with prolongation of an individual’s lifespan remains an important public health message.
Conclusion
In a well-characterised population of healthy older people, moderate exercise, a healthy dietary pattern, moderate alcohol consumption and non-smoking was associated with 44% reduced risk of all-cause mortality, when compared to those complying to ≤ 1 healthy lifestyle factor. Previous multi-lifestyle interventions among healthy older people has proven beneficial in reducing risk for CVD and cognitive decline [35,36,37], whereas evidence from single domain lifestyle interventions are less convincing [38]. Furthermore, these studies, plus others [39], suggest that simple and effective methods for lifestyle modification may be possible among older people. Our findings suggest the likely value of engaging or continuing to engage in multiple healthy lifestyle behaviours in older age and may encourage further multi-lifestyle interventions at both the population level as well as on an individual level.
Availability of data and materials
Data can be made available upon official request with the support of the study Principle Investigator (Professor John McNeil).
Abbreviations
- HR:
-
Hazard Ratio
- IQR:
-
Interquartile range
- SD:
-
Standard Deviation
- CI:
-
Confidence Interval
- CVD:
-
Cardiovascular Disease
- ASPREE:
-
Aspirin in Reducing Events in the Elderly study
- ASPREE-XT:
-
ASPREE-eXTension study
- ALSOP:
-
ASPREE Longitudinal Study of Older Persons sub-study
- WHO:
-
World Health Organisation
- ANOVA:
-
Analysis of Variance
- IRSAD:
-
Index of Relative Socio-economic Advantage and Disadvantage
- BMI:
-
Body Mass Index
- HALE:
-
Healthy Aging: a Longitudinal study in Europe
- USA:
-
United States of America
- UK:
-
United Kingdom
- eGFR:
-
Estimated Glomerular Filtration Rate
- BP:
-
Blood pressure
References
Banks E, Joshy G, Weber MF, Liu B, Grenfell R, Egger S, et al. Tobacco smoking and all-cause mortality in a large Australian cohort study: findings from a mature epidemic with current low smoking prevalence. BMC Med. 2015;13:38.
Wood AM, Kaptoge S, Butterworth AS, Willeit P, Warnakula S, Bolton T, et al. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet. 2018;391(10129):1513–23.
English LK, Ard JD, Bailey RL, Bates M, Bazzano LA, Boushey CJ, et al. Evaluation of dietary patterns and all-cause mortality: a systematic review. JAMA Netw Open. 2021;4(8):e2122277.
Zhao M, Veeranki SP, Magnussen CG, Xi B. Recommended physical activity and all cause and cause specific mortality in US adults: prospective cohort study. BMJ. 2020;370:m2031.
Collaborators GBDRF. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659–724.
McLaughlin D, Adams J, Almeida OP, Brown W, Byles J, Dobson A, et al. Are the national guidelines for health behaviour appropriate for older Australians? Evidence from the men, women and ageing project. Australas J Ageing. 2011;30(2):13–6.
Jacob ME, Yee LM, Diehr PH, Arnold AM, Thielke SM, Chaves PH, et al. Can a healthy lifestyle compress the disabled period in older adults? J Am Geriatr Soc. 2016;64(10):1952–61.
Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med. 2012;55(3):163–70.
Li Y, Pan A, Wang DD, Liu X, Dhana K, Franco OH, et al. Impact of healthy lifestyle factors on life expectancies in the US population. Circulation. 2018;138(4):345–55.
Knoops KT, de Groot LC, Kromhout D, Perrin AE, Moreiras-Varela O, Menotti A, et al. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004;292(12):1433–9.
Wu MY, Wang JB, Zhu Y, Lu JM, Li D, Yu ZB, et al. Impact of individual and combined lifestyle factors on mortality in china: a cohort study. Am J Prev Med. 2020;59(3):461–8.
Rizzuto D, Orsini N, Qiu C, Wang HX, Fratiglioni L. Lifestyle, social factors, and survival after age 75: population based study. BMJ. 2012;345:e5568.
Sun C, Liu H, Xu F, Qin Y, Wang P, Zhou Q, et al. Combined lifestyle factors on mortality among the elder population: evidence from a Chinese cohort study. BMC Geriatr. 2022;22(1):474.
McNeil JJ, Woods RL, Nelson MR, Murray AM, Reid CM, Kirpach B, et al. Baseline characteristics of participants in the ASPREE (ASPirin in Reducing Events in the Elderly) study. J Gerontol A Biol Sci Med Sci. 2017;72(11):1586–93.
McNeil JJ, Nelson MR, Woods RL, Lockery JE, Wolfe R, Reid CM, et al. Effect of Aspirin on All-Cause Mortality in the Healthy Elderly. N Engl J Med. 2018;379(16):1519–28.
McNeil JJ, Woods RL, Nelson MR, Reid CM, Kirpach B, Wolfe R, et al. Effect of aspirin on disability-free survival in the healthy elderly. N Engl J Med. 2018;379(16):1499–508.
McNeil JJ, Woods RL, Ward SA, Britt CJ, Lockery JE, Beilin LJ, et al. Cohort profile: the ASPREE longitudinal study of older persons (ALSOP). Int J Epidemiol. 2019;48(4):1048–9.
Artaud F, Dugravot A, Sabia S, Singh-Manoux A, Tzourio C, Elbaz A. Unhealthy behaviours and disability in older adults: three-City Dijon cohort study. BMJ. 2013;347: f4240.
Carr PR, Weigl K, Jansen L, Walter V, Erben V, Chang-Claude J, et al. Healthy lifestyle factors associated with lower risk of colorectal cancer irrespective of genetic risk. Gastroenterology. 2018;155(6):1805–15.
Chakravarty EF, Hubert HB, Krishnan E, Bruce BB, Lingala VB, Fries JF. Lifestyle risk factors predict disability and death in healthy aging adults. Am J Med. 2012;125(2):190–7.
Lourida I, Hannon E, Littlejohns TJ, Langa KM, Hypponen E, Kuzma E, et al. Association of lifestyle and genetic risk with incidence of dementia. JAMA. 2019;322(5):430–7.
Brinkman S, Voortman T, Kiefte-de Jong JC, van Rooij FJA, Ikram MA, Rivadeneira F, et al. The association between lifestyle and overall health, using the frailty index. Arch Gerontol Geriatr. 2018;76:85–91.
Neumann JT, Freak-Poli R, Orchard SG, Wolfe R, Reid CM, Tonkin AM, et al. Alcohol consumption and risks of cardiovascular disease and all-cause mortality in healthy older adults. Eur J Prev Cardiol. 2022;29(6):e230–2.
National Health and Medical Research Council. (2020). Australian guidelines to reduce health risks from drinking alcohol. Retrieved from https://www.nhmrc.gov.au/health-advice/alcohol.
Department of Health and Aged Care. (2021). Physical activity and exercise guidelines for all Australians. Retrieved from https://www.health.gov.au/health-topics/physical-activity-and-exercise/physical-activity-and-exercise-guidelines-for-all-australians.
World Health Organistation. (2020). WHO guidelines on physical activity and sedentary behaviour. Retrieved from https://www.who.int/publications/i/item/9789240015128.
Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation. 2016;133(2):187–225.
Biddinger KJ, Emdin CA, Haas ME, Wang M, Hindy G, Ellinor PT, et al. Association of habitual alcohol intake with risk of cardiovascular disease. JAMA Netw Open. 2022;5(3): e223849.
Sakaniwa R, Noguchi M, Imano H, Shirai K, Tamakoshi A, Iso H, et al. Impact of modifiable healthy lifestyle adoption on lifetime gain from middle to older age. Age Ageing. 2022;51(5).
Ding D, Rogers K, van der Ploeg H, Stamatakis E, Bauman AE. Traditional and emerging lifestyle risk behaviors and all-cause mortality in middle-aged and older adults: evidence from a large population-based Australian cohort. PLoS Med. 2015;12(12):e1001917.
Foster HME, Celis-Morales CA, Nicholl BI, Petermann-Rocha F, Pell JP, Gill JMR, et al. The effect of socioeconomic deprivation on the association between an extended measurement of unhealthy lifestyle factors and health outcomes: a prospective analysis of the UK Biobank cohort. Lancet Public Health. 2018;3(12):e576–85.
Hsu B, Merom D, Blyth FM, Naganathan V, Hirani V, Le Couteur DG, et al. Total physical activity, exercise intensity, and walking speed as predictors of all-cause and cause-specific mortality over 7 years in older men: the concord health and aging in men project. J Am Med Dir Assoc. 2018;19(3):216–22.
Drewnowski A, Shultz JM. Impact of aging on eating behaviors, food choices, nutrition, and health status. J Nutr Health Aging. 2001;5(2):75–9.
Koehler J, Leonhaeuser IU. Changes in food preferences during aging. Ann Nutr Metab. 2008;52(1):15–9.
Moll Charante van EP, Richard E, Eurelings LS, Dalen van JW, Ligthart SA, Bussel van EF, et al. Effectiveness of a 6-year multidomain vascular care intervention to prevent dementia (preDIVA): a cluster-randomised controlled trial. Lancet. 2016;388(10046):797–805.
Ngandu T, Lehtisalo J, Solomon A, Levalahti E, Ahtiluoto S, Antikainen R, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet. 2015;385(9984):2255–63.
Rolland Y, Barreto PS, Maltais M, Guyonnet S, Cantet C, Andrieu S, et al. Effect of long-term omega 3 polyunsaturated fatty acid supplementation with or without multidomain lifestyle intervention on muscle strength in older adults: secondary analysis of the Multidomain Alzheimer Preventive Trial (MAPT). Nutrients. 2019;11(8):1931.
Newman AB, Dodson JA, Church TS, Buford TW, Fielding RA, Kritchevsky S, et al. Cardiovascular events in a physical activity intervention compared with a successful aging intervention: the life study randomized trial. JAMA Cardiol. 2016;1(5):568–74.
Cheng J, Burke LE, Venditti EM, Sereika SM, Glynn NW, Albert SM, et al. Diet improvements in community-dwelling older adults in the mobility and vitality lifestyle program. J Appl Gerontol. 2022;41(5):1480–4.
Acknowledgements
We thank the ASPREE trial staff, participants, and general practitioners involved in the study.
Data sharing
Upon official request and submission of an expression of interest to the ASPREE data management team, with support from the PI (Professor John McNeil), data may be made available. Deidentified participant data would be accessed via a secure remote server with an accompanying data dictionary and manual including all source data worksheets. Upon submission of the expression of interest, data can be made available within a timely manner.
Funding
This work was supported by the National Institute on Aging and the National Cancer Institute at the National Institutes of Health [grant numbers U01AG029824, U19AG062682]; the National Health and Medical Research Council of Australia [grant numbers 334047, 1127060]; Monash University; and the Victorian Cancer Agency. J.McN. is supported through an NHMRC Leadership Fellowship [IG 1173690]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Author information
Authors and Affiliations
Contributions
CR was involved in study conceptualisation, data cleaning and analysis, interpretation of findings, and drafting of the manuscript. PRC and JB were involved in study conceptualisation, data cleaning, interpretation of findings, and review of the manuscript. JMN was involved in study conceptualisation, interpretation of findings and review of the manuscript. AO, LJB, ABN, MRN, CMR, SGO, JTN, AMT and RW were involved in review of the manuscript. PRC and JB had full access to the data and verified the underlying data.
Corresponding author
Ethics declarations
Ethics approvals and consent to participate
In Australia ethics approvals were obtained from the Monash University Human Research Ethics Committee, RACGP Ethics Committee, University of Tasmania Ethics Committee, Australian National University Human Research Ethics Committee, ACT Health Human Research Ethics Committee, and the University of Adelaide Ethics Committee. Informed consent was obtained from all the participants. All methods were carried out in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
A.M.T has received honoraria from Amgen, Boehinger-Ingelheim, Merck, Novartis and Pfizer. M.R.N served on a Novartis lipids advisory board. All other authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Table 1. Description and prevalence of lifestyle factors in the study population. Table S2. Description of the ascertainment of all-cause and cause specific mortality. Table S3. Baseline characteristics of the study participants by all-cause mortality. Table S4. Hazard ratios of all-cause mortality in relation to individual lifestyle factors (n=11,340). Table S5. Hazard ratios of CVD mortality in relation to individual lifestyle factors (n=11,340). Table S6. Hazard ratios of other mortality in relation to individual lifestyle factors (n=11,340). Table S7. Hazard ratios of cancer mortality in relation to individual lifestyle factors (n=11,340). Table S8. Hazard ratios of all-cause mortality according to combinations of healthy lifestyle factors. Table S9. Hazard ratios of all-cause mortality according to lifestyle categories within demographic, anthropometric and health subgroups. Table S10. Hazard ratios of all-cause mortality according to healthy lifestyle score (excluding former smoker and former drinker). Table S11. Description of an alternative lifestyle score containing multiple levels. Table S12. Hazard ratios of all-cause mortality according to the alternative healthy lifestyle score. Table S13. Hazard ratios of all-cause mortality according to the year-3 healthy lifestyle score.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Robb, C., Carr, P.R., Ball, J. et al. Association of a healthy lifestyle with mortality in older people. BMC Geriatr 23, 646 (2023). https://doi.org/10.1186/s12877-023-04247-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04247-9