Abstract
Background
Drugs with anticholinergic properties are associated with cognitive adverse effects, especially in patients vulnerable to central muscarinic antagonism. A variety of drugs show weak, moderate or strong anticholinergic effects. Therefore, the cumulative anticholinergic burden should be considered in patients with cognitive impairment. This study aimed to develop a Swedish Anticholinergic Burden Scale (Swe-ABS) to be used in health care and research.
Methods
A systematic literature review was conducted in PubMed and Ovid Embase to identify previously published tools quantifying anticholinergic drug burden (i.e., exposure). Drugs and grading scores (0–3, no to high anticholinergic activity) were extracted from identified lists. Enteral and parenteral drugs authorized in Sweden were included. Drugs with conflicting scores in the existing lists were assessed by an expert group. Two drugs that were not previously assessed were also added to the evaluation process.
Results
The systematic literature search identified the following nine anticholinergic burden scales: Anticholinergic Activity Scale, Anticholinergic Burden Classification, updated Anticholinergic Cognitive Burden scale, Anticholinergic Drug Scale, Anticholinergic Load Scale, Anticholinergic Risk Scale, updated Clinician-rated Anticholinergic Scale, German Anticholinergic Burden Scale and Korean Anticholinergic Burden Scale. A list of drugs with significant anticholinergic effects provided by The Swedish National Board of Health and Welfare was included in the process. The suggested Swe-ABS consists of 104 drugs scored as having weak, moderate or strong anticholinergic effects. Two hundred and fifty-six drugs were listed as having no anticholinergic effects based on evaluation in previous scales. In total, 62 drugs were assessed by the expert group.
Conclusions
Swe-ABS is a simplified method to quantify the anticholinergic burden and is easy to use in clinical practice. Publication of this scale might make clinicians more aware of drugs with anticholinergic properties and patients’ total anticholinergic burden. Further research is needed to validate the Swe-ABS and evaluate anticholinergic exposure versus clinically significant outcomes.
Similar content being viewed by others
Background
Acetylcholine is a neurotransmitter used by all cholinergic neurons in the central and peripheral nervous systems. It plays an important role in cognitive functions, such as memory processes [1]. Medications with anticholinergic properties (i.e. muscarinic cholinergic antagonists) are associated with a high risk of both central adverse effects, such as cognitive impairment, and peripheral adverse effects, such as dryness of the mouth and urinary retention [2]. These adverse effects may occur when anticholinergic drugs block acetylcholine binding to muscarinic receptors M1–M5, all of which have similar structures at their ligand-binding sites. The development of subtype-selective antagonists is one approach to diminish these adverse effects. Hence, the introduction of M3-selective urinary spasmolytics such as solifenacin and darifenacin has improved the treatment of urinary incontinence as they exert less central anticholinergic effects. Beyond urinary incontinence drugs with anticholinergic properties are used to treat a wide variety of medical conditions, including pain, sleep disorders, parkinsonism and depression [3].
Besides medications used particularly for their anticholinergic properties, there are medications with varying degrees of anticholinergic activity (AA), leading to non-intended anticholinergic effects. The cumulative effect of taking multiple medications with AA is known as anticholinergic burden and is associated with an increased risk of significant anticholinergic adverse drug reactions [4, 5].
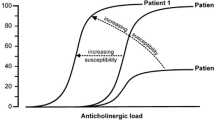
Drugs with high anticholinergic potency are regarded as potentially inappropriate in treating older people, especially those with Alzheimer’s or other neurodegenerative diseases, because of conditions such as degeneration of cholinergic neurons in the basal forebrain or increased permeability of the blood–brain barrier [6]. However, recent studies suggested that even individuals aged ≤75 years [7], younger patients with Parkinson’s disease [8] and middle-aged people with Alzheimer’s disease [9] are at increased risk of anticholinergic adverse effects. Hence, individual vulnerability pertaining to neurodegenerative diseases, besides age, might play an important role in the risk of anticholinergic adverse effects [10].
The Swedish National Board of Health and Welfare has issued a list of drugs with significant anticholinergic effects that should be avoided in treating the elderly [11]. The total prescription of these listed drugs has decreased radically among the elderly in Sweden. Nevertheless, 3.8% of people aged ≥75 are prescribed these medications [12].
Currently, the following two major methods to assess a patient’s anticholinergic burden are available: (1) serum radioreceptor anticholinergic activity assay and (2) using expert-based lists of medications with anticholinergic properties [13]. The latter method has been suggested as the only clinically useful method [14]. Summer’s method using the drug risk number, which estimated the risk of drug-induced delirium, was the first clinical research method to be published [15]. Over the years, several expert-based lists have been developed, with most of them categorizing anticholinergic medications into groups based on their level of AA. However, they differ in the number and selection of included drugs as well as in the rating of AA [16].
In 2013, Duran et al. developed the first comprehensive list of drugs with anticholinergic properties based on seven published risk scales [17]. This method was later used to develop drug lists for countries such as Germany and South Korea [18, 19]. Adapting lists for specific countries is important because medication availability and prescribing patterns differ among countries [16].
Therefore, we aimed to develop a scale with drugs authorized and available in Sweden, using the experiences gained elsewhere. To our knowledge, a Swedish version of a scale for quantifying anticholinergic burden has not yet been introduced. However, a web-based risk assessment tool, Janusmed®, was available for two specific regions in Sweden at the start of the present study. Nevertheless, no Swedish expert-based list was available to us.
Methods
Search strategy and selection criteria
PubMed was searched for systematic reviews of previously published tools quantifying anticholinergic drug burden (i.e., exposure). To be classified as a systematic review, the study had to be planned and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement [20, 21]. The search was conducted in April 2020 with no date restriction. The search terms were as follows: anticholinergic [Title/Abstract] AND burden [Title/Abstract] AND scale [Title/Abstract] OR list [Title/Abstract] OR score [Title/Abstract] OR tool [Title/Abstract] AND review. The same procedure was used for Ovid Embase to ensure that all relevant reviews were found. In addition, the reference lists of the selected studies were searched manually for more studies. Furthermore, studies were included if they were (1) systematic reviews on tools to quantify anticholinergic drug burden or original research papers presenting anticholinergic risk scales and (2) written in English. Tools were included if they (1) provided medication lists with grading scores to quantify anticholinergic burden; (2) were based on clinical expert opinions and included drugs authorized in Sweden not previously assessed and (3) provided lists that were comparable to other lists. Tools based on equations were not included. The titles and abstracts of the identified studies were screened, and full-text articles were evaluated in case of uncertainty. To find any new lists with drugs not previously assessed, the search was updated in March 2022.
Data extraction
The method established by Duran et al. and adapted by Kiesel et al. was used to construct a Swedish anticholinergic burden scale [17, 18]. Enteral and parenteral drugs were included. Drugs authorized and available in Sweden at the start of the present study (April 2020) were included. In addition, two clinically relevant substances, propiomazine and vortioxetine, were added.
Each drug was generally assigned a score from 0 (no AA) to 3 (high AA) in the identified lists why this gradation was chosen for this scale. However, the grading system differed in one list, the Anticholinergic Activity Scale, where a 5-point grading system (0–4) was used [22]. Therefore, this list was modified to 0–3 in accordance with Duran et al.’s methodology [17].
The agreement of the scores for each drug was evaluated. The algorithm employed by Kiesel et al. was used. If a drug was scored by ≥2 lists and there was agreement among the list scores, the drug was assigned that score. If a drug was scored by ≥2 lists with only a 1-point difference, the drug was assigned the higher score. If a drug was scored exclusively 0 in at least one existing list, the drug was scored 0. Further evaluation was needed (1) when the scores differed by ≥2 points between the lists and (2) if the drug was evaluated and scored 1–3 in only one list [18]. In addition, further evaluation was needed when (1) a drug was scored unanimously 3 by ≥2 lists but was not included on the list of medications with significant anticholinergic effects provided by the National Board of Health and Welfare [11] and (2) a drug was included on the abovementioned list but not included or scored 0–2 in the identified lists.
An expert group consisting of four physicians (two senior neuropsychiatrists, a senior general practitioner and a resident in both clinical pharmacology and psychiatry) and one clinical pharmacist was formed to further evaluate the selected drugs. To rate the mechanism of action of the drugs, central and peripheral anticholinergic adverse effects reported by Tune [4] were retrieved from the online version of DRUGDEX®. Any information about the muscarinic binding affinity of the drugs was retrieved from the Psychoactive Drug Screening Program Ki Database® and DrugBank Online®, while Chew’s list was used for any information about a drug’s serum AA [23]. Additional sources of information, such as UpToDate® and Martindale®, were used if information about a drug was absent, poor or outdated in DRUGDEX®. The Swedish summary of product characteristics for each drug was searched for contraindicated medical conditions, such as glaucoma, myasthenia gravis and benign prostatic hyperplasia. A score of 0 to 3 was assigned for each drug individually by the experts based on the mechanism of action, contraindications, frequency of adverse effects and type of adverse effects. The scoring was then discussed in the expert group leading to consensus and a final anticholinergic score. Information regarding the muscarinic binding affinity of the drugs was considered in the final discussion when available. In case of disagreement in the expert group, other physicians were consulted. The clinical experience of the expert group was considered in the rating process.
Results
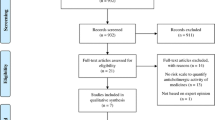
The search in PubMed and Ovid Embase resulted in seven systematic reviews [17, 20, 24,25,26,27,28] and two original research articles [19, 29]. The following nine anticholinergic risk scales met the inclusion criteria: Anticholinergic Activity Scale, Anticholinergic Burden Classification, updated Anticholinergic Cognitive Burden scale, Anticholinergic Drug Scale, Anticholinergic Load Scale, Anticholinergic Risk Scale, updated Clinician-rated Anticholinergic Scale, German Anticholinergic Burden Scale and Korean Anticholinergic Burden Scale [18, 19, 22, 30,31,32,33,34,35]. A flowchart of the selection strategy is presented in Fig. 1 [21]. The list of medications with significant anticholinergic effects provided by the National Board of Health and Welfare was then added to these scales [11]. Excluded tools with the reasons for exclusion are presented in Table 1.
An additional database search with a time restriction of 1 May 2020 to 31 March 2022 yielded two new reviews [13, 36], one new original research article [37] and four additional scales (the Delirogenic Risk Scale [38], modified Anticholinergic Burden Scale [39], Anticholinergic Toxicity Score [40] and CRIDECO Anticholinergic Load Scale [37]; Fig. 1). The Delirogenic Risk Scale and the Anticholinergic Toxicity Score were not comparable with other scales [38, 40]. The modified Anticholinergic Burden Scale was produced by combining pre-existing scales without any evaluation of new drugs [39]. The CRIDECO Anticholinergic Load Scale was based on risk scales already included in the assessment. However, it included one enteral drug authorized in Sweden previously not evaluated in the existing scales [37]. This drug was assessed by the expert group.
A total of 234 drugs scored 1–3 were extracted from the existing lists and the list of drugs with definite anticholinergic effects provided by the National Board of Health and Welfare. Of these, 107 drugs were excluded because they were not authorized in Sweden (Additional file 1 Table 1). Furthermore, nine drugs were excluded due to other modes of administration than enteral or parenteral (Additional file 1 Table 2). Six drugs were then added: two of them were previously not rated (propiomazine and vortioxetine) and four of them scored 0 in previous scales (chlorzoxazone, melperone, memantine and sertindole). A summary of the remaining 124 drugs is presented in Table 2.
In total, 62 drugs, including two drugs previously not assessed and one drug from the second database search, were evaluated by the expert group. The rating was reconsidered for some drugs within the same drug class, based on the Anatomical Therapeutic Chemical Classification by the World Health Organization, that were scored differently [18]. The rating could also be reconsidered for structurally alike drugs that were assigned different scores.
Twenty-one drugs were assessed by the expert group as having no anticholinergic effects (score 0; Table 3), while 256 drugs were listed as having no anticholinergic effects based on their assessment in previous scales [18] (Additional file 1 Table 3).
The suggested final Swedish Anticholinergic Burden Scale (Swe-ABS) is presented in Table 4. It presents 23 drugs with strong anticholinergic effects (score 3), 16 drugs with moderate anticholinergic effects (score 2) and 65 drugs with low anticholinergic effects (score 1).
Discussion
Several anticholinergic burden scales have been published. However, no international standard scale has been recommended for the quantification of anticholinergic burden [36]. The Swe-ABS was developed from nine existing anticholinergic risk scales [18, 19, 22, 30,31,32,33,34,35] and the list of medications with significant anticholinergic effects provided by the National Board of Health and Welfare [11]. Although grey literature was not searched for possible unpublished anticholinergic risk scales, several published systematic reviews have been reviewed in this study to reduce the risk of missing existing scales. Most of the included scales are over a decade old and lack drugs marketed after the publication of the scales [22, 30,31,32,33,34,35]. However, two of the scales were newly published and updated with new drugs [18, 19], which makes the Swe-ABS up to date. Furthermore, drugs not authorized in Sweden were excluded and two new drugs were added to adapt the scale to the Swedish market.
In the scoring process, the algorithm employed by Kiesel et al. to develop the German Anticholinergic Burden Score was used [18]. In a study assessing the quality of published anticholinergic burden scales, the German scale achieved the highest percentage in quality, together with the updated Anticholinergic Cognitive Burden scale [13]. Furthermore, a newly published study showed that the German Anticholinergic Burden Score appears to be comparable with the validated Anticholinergic Drug Scale regarding the effect of an anticholinergic burden on cognitive function [50]. Contrary to Kiesel et al., the authors of this study also considered muscarinic binding affinity in the assessment of drugs that needed further evaluation.
The present study has some limitations. First, the dependability of the reported adverse effects as a measure is contingent on both frequency and reliability. For example, an absence of reported anticholinergic adverse effects may be because they are absent or underreported. Other issues include how anticholinergic and antihistaminic effects should be distinguished and the challenging differentiation between anticholinergic side effects and the mechanism of action of an assessed drug. Moreover, information about the muscarinic binding affinity was lacking for several drugs and for others, the reported dissociation constant differed significantly between studies. The expert group consisted of people with extensive clinical experience from pharmaceutical-intensive specialties contributing to a multifaceted assessment. However, making a completely impartial assessment regarding anticholinergic adverse effects based on expert clinical opinion may not be possible [48].
Second, in cases where a drug had been assessed using ≥2 scales and the scores differed by only 1 point, the drug was automatically assigned the higher score based on Kiesel et al.’s methodology [18]. This might have resulted in an overestimation of the AA of the drug [19]. However, the risk of missing any drug with anticholinergic properties was reduced [18]. Furthermore, if a drug was scored by ≥2 lists and there was agreement among the list scores, the drug was assigned that score. This might have resulted in repetition of incorrectly assessed drugs. The gradation 0–3 was selected to make this scale comparable with several existing scales. A wider scoring range might have been valuable in distinguishing the drugs even more [24]. On the other hand, this could create an illusion of that it is a more precise measure of anticholinergic effects than it is.
Third, as in the case of many previously published scales, this scale does not consider dosage even though anticholinergic effects are considered dose-dependent [6, 23, 41, 51]. Whether an equal anticholinergic score results in the same effect has been questioned. For example, whether three drugs with an anticholinergic score of 1 are equivalent to one drug with an anticholinergic score of 3 [26]. This limits the application in clinical practice. Moreover, there is no advice on how to apply the scale in relation to changes in medication at a specific cut off value for high anticholinergic burden [6]. It is also recommended that individual vulnerability is to be considered, which adds a further level of complexity and uncertainty. Furthermore, variables such as drug–drug interactions and possible development of tolerance for anticholinergic drug effects are yet to be considered [6].
Fourth, this list is not comprehensive. Drugs with routes of administration other than enteral or parenteral were not included in this list due to incomplete data on systemic effects, and the list does not include all drugs marketed in Sweden. This scale is proposed to be used as a guideline when evaluating anticholinergic burden in patients, especially in those vulnerable to central muscarinic antagonism. Nevertheless, both central and peripheral anticholinergic adverse effects have been assessed in this study due to increased permeability of the blood–brain barrier in the elderly and individuals with neurodegenerative diseases [6, 52].
The authors encourage a possible adaptation of Swe-ABS for the other Nordic countries with comparable treatment guidelines and medication availability. To avoid repetition of previous assessment, the Swe-ABS could be modified for medications approved in other Nordic countries. This approach would be timesaving, although also involve a significant risk that the list does not cover approved drugs in the country for which it is intended. In the adaptation process we therefore also recommend review of excluded drugs in this paper (Additional file 1 Table 1). We encourage a Nordic cross-national collaboration regarding validation studies in different clinical settings and assessment of new drugs on the market. The use of an adapted Swe-ABS in other Nordic countries with similar healthcare systems could contribute to increased awareness of drugs with anticholinergic properties and reduce the overall anticholinergic burden. However, mentioned limitations, specifically the lack of dose-related information must be considered.
During the finalization of this article, the web-based risk assessment tool Janusmed®, which was earlier available in two county councils in Sweden, became available throughout Sweden. In the future, it would be useful to review the coherence between these two tools. Swe-ABS will be validated in an ongoing study conducted at a memory clinic in southern Sweden. We aim to establish a continuously updated tool for quantifying anticholinergic burden that is clinically relevant. An eHealth application integrated with electronic medical record systems could be one way to automize the use of this scale.
Conclusions
The Swe-ABS is a simplified method to quantify anticholinergic burden and it is easy to use in clinical practice. Publication of this scale might make clinicians more aware of drugs with anticholinergic properties and patients’ total anticholinergic burden. Further research is needed to validate the Swe-ABS and evaluate anticholinergic exposure versus clinically significant outcomes.
Data Availability
All data generated or analysed during this study are included in this published article (and its additional files).
Abbreviations
- AA:
-
Anticholinergic activity
- Swe-ABS:
-
Swedish Anticholinergic Burden Scale
References
Ferreira-Vieira TH, Guimaraes IM, Silva FR, Ribeiro FM. Alzheimer’s disease: targeting the Cholinergic System. Curr Neuropharmacol. 2016;14(1):101–15.
Fox C, Smith T, Maidment I, Chan WY, Bua N, Myint PK, et al. Effect of medications with anti-cholinergic properties on cognitive function, delirium, physical function and mortality: a systematic review. Age Ageing. 2014;43(5):604–15.
Nestler EJKP, Russo SJ, Schaefer A, Nestler. Hyman and Malenka’s Molecular Neuropharmacology: A Foundation for Clinical Neuroscience, 4e. 4th ed; 2020. ISBN 978-1-260-45690-5.
Tune LE. Anticholinergic effects of medication in elderly patients. J Clin Psychiatry. 2001;62 Suppl 21:11 – 4.
Boustani MA, Campbell NL, Munger S, Maidment ID, Fox C. Impact of anticholinergics on the aging brain: a review and practical application. Aging Health. 2008;4:311–20.
Kersten H, Wyller TB. Anticholinergic drug burden in older people’s brain - how well is it measured? Basic Clin Pharmacol Toxicol. 2014;114(2):151–9.
Welk B, McArthur E. Increased risk of dementia among patients with overactive bladder treated with an anticholinergic medication compared to a beta-3 agonist: a population-based cohort study. BJU Int. 2020;126(1):183–90.
Rajan R, Saini A, Verma B, Choudhary N, Gupta A, Vishnu VY, et al. Anticholinergics may carry significant cognitive and Gait Burden in Parkinson’s Disease. Mov Disord Clin Pract. 2020;7(7):803–9.
Coupland CAC, Hill T, Dening T, Morriss R, Moore M, Hippisley-Cox J. Anticholinergic drug exposure and the risk of dementia: a nested case-control study. JAMA Intern Med. 2019;179(8):1084–93.
Reinold J, Braitmaier M, Riedel O, Haug U. Anticholinergic burden: first comprehensive analysis using claims data shows large variation by age and sex. PLoS ONE. 2021;16(6):e0253336.
Swedish National Board of Health and Welfare. [Indikatorer for god lakemedelsterapi hos alder] 2017-6-7. 2017-6-7 ed. Stockholm2017.
Swedish National Board of Health. and Welfare.[Vard och omsorg for aldre. Lagesrapport 2021] 2021-3-7249. 2021-3-7249 ed. Stockholm2021.
Lisibach A, Benelli V, Ceppi MG, Waldner-Knogler K, Csajka C, Lutters M. Quality of anticholinergic burden scales and their impact on clinical outcomes: a systematic review. Eur J Clin Pharmacol. 2021;77(2):147–62.
Rudd KM, Raehl CL, Bond CA, Abbruscato TJ, Stenhouse AC. Methods for assessing drug-related anticholinergic activity. Pharmacotherapy. 2005;25(11):1592–601.
Summers WK. A clinical method of estimating risk of drug induced delirium. Life Sci. 1978;22(17):1511–6.
Lertxundi U, Domingo-Echaburu S, Hernandez R, Peral J, Medrano J. Expert-based drug lists to measure anticholinergic burden: similar names, different results. Psychogeriatrics. 2013;13(1):17–24.
Duran CE, Azermai M, Vander Stichele RH. Systematic review of anticholinergic risk scales in older adults. Eur J Clin Pharmacol. 2013;69(7):1485–96.
Kiesel EK, Hopf YM, Drey M. An anticholinergic burden score for german prescribers: score development. BMC Geriatr. 2018;18(1):239.
Jun K, Hwang S, Ah YM, Suh Y, Lee JY. Development of an anticholinergic Burden Scale specific for korean older adults. Geriatr Gerontol Int. 2019;19(7):628–34.
Welsh TJ, van der Wardt V, Ojo G, Gordon AL, Gladman JRF. Anticholinergic drug Burden Tools/Scales and adverse outcomes in different clinical settings: a systematic review of reviews. Drugs Aging. 2018;35(6):523–38.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Ehrt U, Broich K, Larsen JP, Ballard C, Aarsland D. Use of drugs with anticholinergic effect and impact on cognition in Parkinson’s disease: a cohort study. J Neurol Neurosurg Psychiatry. 2010;81(2):160–5.
Chew ML, Mulsant BH, Pollock BG, Lehman ME, Greenspan A, Mahmoud RA, et al. Anticholinergic activity of 107 medications commonly used by older adults. J Am Geriatr Soc. 2008;56(7):1333–41.
Salahudeen MS, Duffull SB, Nishtala PS. Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: a systematic review. BMC Geriatr. 2015;15:31.
Lozano-Ortega G, Johnston KM, Cheung A, Wagg A, Campbell NL, Dmochowski RR, et al. A review of published anticholinergic scales and measures and their applicability in database analyses. Arch Gerontol Geriatr. 2020;87:103885.
Villalba-Moreno AM, Alfaro-Lara ER, Perez-Guerrero MC, Nieto-Martin MD, Santos-Ramos B. Systematic review on the use of anticholinergic scales in poly pathological patients. Arch Gerontol Geriatr. 2016;62:1–8.
Cardwell K, Hughes CM, Ryan C. The Association between Anticholinergic Medication Burden and Health related outcomes in the ‘Oldest Old’: a systematic review of the literature. Drugs Aging. 2015;32(10):835–48.
Mayer T, Haefeli WE, Seidling HM. Different methods, different results-how do available methods link a patient’s anticholinergic load with adverse outcomes? Eur J Clin Pharmacol. 2015;71(11):1299–314.
Nery RT, Reis AMM. Development of a brazilian anticholinergic activity drug scale. Einstein (Sao Paulo). 2019;17(2):eAO4435.
Carnahan RM, Lund BC, Perry PJ, Pollock BG, Culp KR. The anticholinergic drug Scale as a measure of drug-related anticholinergic burden: associations with serum anticholinergic activity. J Clin Pharmacol. 2006;46(12):1481–6.
Ancelin ML, Artero S, Portet F, Dupuy AM, Touchon J, Ritchie K. Non-degenerative mild cognitive impairment in elderly people and use of anticholinergic drugs: longitudinal cohort study. BMJ. 2006;332(7539):455–9.
Han L, Agostini JV, Allore HG. Cumulative anticholinergic exposure is associated with poor memory and executive function in older men. J Am Geriatr Soc. 2008;56(12):2203–10.
Sittironnarit G, Ames D, Bush AI, Faux N, Flicker L, Foster J, et al. Effects of anticholinergic drugs on cognitive function in older Australians: results from the AIBL study. Dement Geriatr Cogn Disord. 2011;31(3):173–8.
Aging Brain Care. Aging Brain Program: Anticholinergic Cognitive Burden Scale 2012 Update. 2012. https://gwep.med.ucla.edu/files/view/docs/initiative2/conferences/Anticholinergic-Burden-Scale.pdf. Accessed 31 Mar 2022.
Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med. 2008;168(5):508–13.
Al Rihani SB, Deodhar M, Darakjian LI, Dow P, Smith MK, Bikmetov R, et al. Quantifying anticholinergic burden and sedative load in older adults with polypharmacy: a systematic review of risk scales and models. Drugs Aging. 2021;38(11):977–94.
Ramos H, Moreno L, Perez-Tur J, Chafer-Pericas C, Garcia-Lluch G, Pardo J. CRIDECO anticholinergic load scale: an updated anticholinergic Burden Scale. Comparison with the ACB Scale in Spanish individuals with subjective memory complaints. J Pers Med. 2022;12(2).
Hefner G, Shams MEE, Wenzel-Seifert K, Fellgiebel A, Falter T, Haen E, et al. Rating the delirogenic potential of drugs for Prediction of Side Effects in Elderly Psychiatric Inpatients. J J Pharma Pharmacovigilance. 2015;1(3):1–3.
Kable A, Fullerton A, Fraser S, Palazzi K, Hullick C, Oldmeadow C et al. Comparison of potentially inappropriate medications for people with dementia at admission and discharge during an unplanned admission to hospital: results from the SMS dementia study. Healthc (Basel). 2019;7(1).
Xu D, Anderson HD, Tao A, Hannah KL, Linnebur SA, Valuck RJ, et al. Assessing and predicting drug-induced anticholinergic risks: an integrated computational approach. Ther Adv Drug Saf. 2017;8(11):361–70.
Klamer TT, Wauters M, Azermai M, Duran C, Christiaens T, Elseviers M, et al. A novel scale linking potency and dosage to Estimate Anticholinergic exposure in older adults: the muscarinic acetylcholinergic receptor ANTagonist exposure scale. Basic Clin Pharmacol Toxicol. 2017;120(6):582–90.
Hilmer SN, Mager DE, Simonsick EM, Cao Y, Ling SM, Windham BG, et al. A drug Burden Index to define the functional burden of medications in older people. Arch Intern Med. 2007;167(8):781–7.
Hilmer SN, Mager DE, Simonsick EM, Ling SM, Windham BG, Harris TB, et al. Drug burden index score and functional decline in older people. Am J Med. 2009;122(12):1142–9e1.
Aizenberg D, Sigler M, Weizman A, Barak Y. Anticholinergic burden and the risk of falls among elderly psychiatric inpatients: a 4-year case-control study. Int Psychogeriatr. 2002;14(3):307–10.
Cancelli I, Valentinis L, Merlino G, Valente M, Gigli GL. Drugs with anticholinergic properties as a risk factor for psychosis in patients affected by Alzheimer’s disease. Clin Pharmacol Ther. 2008;84(1):63–8.
Whalley LJ, Sharma S, Fox HC, Murray AD, Staff RT, Duthie AC, et al. Anticholinergic drugs in late life: adverse effects on cognition but not on progress to dementia. J Alzheimers Dis. 2012;30(2):253–61.
Han L, McCusker J, Cole M, Abrahamowicz M, Primeau F, Elie M. Use of medications with anticholinergic effect predicts clinical severity of delirium symptoms in older medical inpatients. Arch Intern Med. 2001;161(8):1099–105.
Bishara D, Harwood D, Sauer J, Taylor DM. Anticholinergic effect on cognition (AEC) of drugs commonly used in older people. Int J Geriatr Psychiatry. 2017;32(6):650–6.
Minzenberg MJ, Poole JH, Benton C, Vinogradov S. Association of anticholinergic load with impairment of complex attention and memory in schizophrenia. Am J Psychiatry. 2004;161(1):116–24.
Kruger C, Schafer I, van den Bussche H, Bickel H, Fuchs A, Gensichen J, et al. Anticholinergic drug burden according to the anticholinergic drug scale and the german anticholinergic burden and their impact on cognitive function in multimorbid elderly german people: a multicentre observational study. BMJ Open. 2021;11(3):e044230.
Wauters M, Klamer T, Elseviers M, Vaes B, Dalleur O, Degryse J, et al. Anticholinergic exposure in a cohort of adults aged 80 years and over: Associations of the MARANTE scale with mortality and hospitalization. Basic Clin Pharmacol Toxicol. 2017;120(6):591–600.
Chancellor MB, Staskin DR, Kay GG, Sandage BW, Oefelein MG, Tsao JW. Blood-brain barrier permeation and efflux exclusion of anticholinergics used in the treatment of overactive bladder. Drugs Aging. 2012;29(4):259–73.
Acknowledgements
Not applicable.
Funding
This study has received research funding from The Elly Berggrens Foundation and The Kockska Foundation for Medical Research.
Open access funding provided by Lund University.
Author information
Authors and Affiliations
Contributions
T.R. designed the study with support from P.J. T.R. conducted the database searches and extracted and summarized existing scores. A.E. retrieved the information from DRUGDEX. T.R. drafted the manuscript. All authors (T.R., A.E., E.L., S.M. and P.J.) participated in the assessment of drugs and made contributions to the manuscript and its conclusions. All authors reviewed the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rube, T., Ecorcheville, A., Londos, E. et al. Development of the Swedish anticholinergic burden scale (Swe-ABS). BMC Geriatr 23, 518 (2023). https://doi.org/10.1186/s12877-023-04225-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04225-1