Abstract
Background
Walking is an important factor in daily life. Among older adults, gait function declines with age. In contrast to the many studies revealing gait differences between young adults and older adults, few studies have further divided older adults into groups. The purpose of this study was to subdivide an older adult population by age to identify age-related differences in functional evaluation, gait characteristics and cardiopulmonary metabolic energy consumption while walking.
Methods
This was a cross-sectional study of 62 old adult participants who were classified into two age groups of 31 participants each as follows: young-old (65–74 years) and old-old (75–84 years) group. Physical functions, activities of daily living, mood state, cognitive function, quality of life, and fall efficacy were evaluated using the Short Physical Performance Battery (SPPB), Four-square Step Test (FSST), Timed Up and Go Test (TUG), Korean Version of the Modified Barthel Index, Geriatric Depression Scale (GDS), Korean Mini-mental State Examination, EuroQol-5 Dimensions (EQ-5D) questionnaire, and the Korean version of the Fall Efficacy Scale. A three-dimensional motion capture system (Kestrel Digital RealTime System®; Motion Analysis Corporation, Santa Rosa, CA, USA) and two force plates (TF-4060-B; Tec Gihan, Kyoto, Japan) were used to investigate spatiotemporal gait parameters (velocity, cadence, stride length, stride width, step length, single support, stance phase, and swing phase), kinematic variables (hip, knee, and ankle joint angles), and kinetic variables (hip, knee, and ankle joint moment and power) of gait. A portable cardiopulmonary metabolic system (K5; Cosmed, Rome, Italy) was used to measure cardiopulmonary energy consumption.
Results
The old-old group showed significantly lower SPPB, FSST, TUG, GDS-SF, and EQ-5D scores (p < 0.05). Among spatiotemporal gait parameters, velocity, stride length, and step length were significantly lower in the old-old group than in the young-old group (p < 0.05). Among the kinematic variables, the knee joint flexion angles during initial contact and terminal swing phase were significantly higher in the old-old than the young-old group (P < 0.05). The old-old group also showed a significantly lower ankle joint plantarflexion angle during the pre- and initial swing phases (P < 0.05). Among the kinetic variables, the hip joint flexion moment and knee joint absorption power in the pre-swing phase were significantly lower in the old-old than the young-old group (P < 0.05).
Conclusion
This study demonstrated that participants 75–84 years of age had less functional gaits than their young-old counterparts (65–74 years old). As the walking pace of old-old people diminishes, driving strength to move ahead and pressure on the knee joint also tend to decrease together with stride length. These differences in gait characteristics according to age among older adults could improve our understanding of how aging causes variations in gait that increase the risk of falls. Older adults of different ages may require customized intervention plans, such as gait training methods, to prevent age-related falls.
Trial registration
Clinical trials registration information: ClinicalTrials.gov Identifier: NCT04723927 (26/01/2021).
Similar content being viewed by others
Background
The size of the global older adult population is rapidly increasing [1]. The current age at which a person is considered old is 65 years or older. In Japan, which has the world's largest aging population, researchers have called for ‘senior’ to be redefined as age 75 or older [2]. Previous research has shown that age-related body function changes such as slowing of movement and grip weakening occur 5 to 10 years later in life than they did 10 to 20 years ago, resulting in a ‘rejuvenation’ phenomenon [3]. Furthermore, people aged 65–74 years have better mental and physical health than previous generations at that age range, and they engage in more social activities than people older than 75 years. Some geriatric studies have compared the characteristics of people aged 65–74 years (young-old) with those of people aged 75–84 years (old-old) [4, 5]. For example, compared with young-old individuals, old-old people showed increased depression [6] and decreased health-promoting behavior and self-esteem [7]. In physical health, old-old people show pronounced decreases in gait function, such as increased muscle weakness in the lower extremities and increased gait disturbances, compared with young-old people [8, 9].
Among studies dealing with changes in older adults due to aging, gait studies are important because they can identify or predict clinical abnormalities related to aging [10]. In gait research, functional evaluation plays an important role in patient treatment planning and prognosis prediction [11]. Furthermore, kinematic and kinetic variables provide important information on the underlying causes of the gait impairment and can help guide treatment and intervention strategies among older adults [12]. In addition, cardiopulmonary metabolic energy efficiency testing is important for evaluating human exercise capacity and predicting disease outcomes [13], and research has confirmed that older people use energy less efficiently than younger adults during walking [14]. As such, functional assessment, gait analysis, and cardiopulmonary metabolic energy efficiency testing are important measures of mobility quality and functional capacity in older adults [15, 16]. Several previous studies have shown variations in function [17, 18], gait patterns [19,20,21,22,23], and age-related cardiopulmonary metabolic efficiency [24,25,26] between healthy older adults and younger adults. However, few studies have divided older adult participants into two age groups and evaluated function, gait, and cardiopulmonary metabolic energy use in a laboratory setting.
The purpose of this study was to investigate differences in gait measures among participants divided into young-old (65–74 years) and old-old groups (75–84 years) within a single laboratory environment. Results are intended to be used as strategic data for creating elderly-specific interventions to prevent the risks associated with aging, such as falls. Three main hypotheses of this study are: 1) physical performance assessments and participant-reported outcomes differ between the young-old and old-old groups; 2) spatiotemporal gait parameters, kinematics, and kinetics differ between the young-old and old-old groups; 3) cardiopulmonary metabolic energy efficiency differ between the young-old and old-old groups.
Materials and methods
Participants
This cross-sectional study included 62 older adult people without a history of neurological or psychiatric complaints ranging in age from 65–84 years (mean age, 74.16 ± 4.26 years; 29 males). They were split into two groups based on their ages, as follows: young-old (65–74 years; mean age, 70.6 ± 2.4 years; n = 31; 12 males) and old-old (75–84 years; mean age, 77.74 ± 2.07 years; n = 31; 17 males). Participants were excluded if they (1) experienced difficulty walking on their own due to issues such as visual field loss, (2) had severe dizziness that might cause a fall, or (3) demonstrated severe cognitive decline with a score of < = 10 points on the Korean Mini-mental State Exam (K-MMSE) [27]. Samsung Medical Center's 'IRB number: 2020–09-172' Institutional Review Board approved this study protocol after receiving the informed consent of all subjects.
Experimental protocol
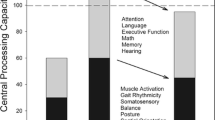
All study participants who consented to participate provided their sociodemographic information (age, sex, and educational attainment), height, weight, body mass index, and medical history (Table 1). Functional assessments were used to assess the differences of the participant's physical performance assessments and participant-reported outcomes. A three-dimensional (3D) motion capture system (Kestrel Digital RealTime System®; Motion Analysis Corporation, Santa Rosa, CA, USA) and two force plates (TF-4060-B; Tec Gihan, Kyoto, Japan) were used to investigate spatiotemporal, kinematic, and kinetic aspects of gait. The participants were asked to walk along a 10-m walkway at their preferred walking speed (Fig. 1). The spatiotemporal gait parameter variables were velocity (cm/s), cadence (step/min), stride length (cm), step length (cm), single support (% cycle), stance phase (% cycle), and swing phase (% cycle) [28] (Fig. 2). Gait kinematic variables were the hip, knee, and ankle joint angles (degree) in the sagittal plane during walking. Kinetic variables were sagittal plane, the hip, knee, and ankle joint moments (N·m/kg·m) and power (W/kg·m). Gait data were obtained subjectively through a walkway test in a motion analysis laboratory. While the participants were attached to a portable cardiopulmonary metabolic system (K5; Cosmed, Rome, Italy), baseline values were determined by measuring cardiopulmonary metabolic energy consumption data while standing comfortably for three minutes. Then, their metabolic rate was measured as they walked on a treadmill for six minutes at preferred walking speed. Three variables measured when evaluating cardiopulmonary metabolic consumption: The net cardiopulmonary metabolic energy cost (net VO2) is the energy expended by the body while walking a certain distance [29]. The energy expenditure measurement (EEm) is the total energy cost of maintaining constant conditions in the body plus the energy cost of physical activities [30]. The metabolic equivalent (MET) is an objective measure of the ratio between the rate at which a person expends energy while performing some specific physical activity and the mass of that person compared to a reference that is set by convention at 3.5 mL of oxygen per kilogram per minute, which is roughly equivalent to the energy expended when sitting quietly [31].
Measurements
The physical performance assessments were as follows. The Short Physical Performance Battery (SPPB) [32] evaluates balance, lower limb muscle strength, and mobility by assessing three tasks: balancing, performing five sit-to-stand cycles, and walking at a normal pace. Each task is rated on a scale from 0 (worst) to 4 (best), and the overall summary score ranges from 0 (worst performers) to 12 (best performers), providing an objective measure of an individual's physical performance. The Four-Square Step Test (FSST) [33] evaluates dynamic stability and coordination by measuring the time it takes for a subject to step clockwise, then counterclockwise, through each quadrant. Subjects are instructed to face forward during the entire sequence, if possible. The Timed Up and Go Test (TUG) [34] assesses balance and functional exercise ability to predict the risk of falling. To assess TUG, participants are seated on a chair positioned against a wall, after which they are directed to rise from the chair, walk along a 3-m pathway at their normal pace, turn around, come back, and sit down once again. The timing of the task begins with the command "go" and concludes when the participant sits down again. The questionnaires used for participant-reported outcomes were as follows. The K-MMSE is a quick way to evaluate cognitive function and the participant's current state, with scores ranging from 0 to 30. A score of 24 points or more is considered 'normal', a score of 20 to 23 is 'suspected dementia', and a score of 19 points or less is 'definite dementia'. The Korean-Modified Barthel Index (K-MBI) [35] assesses the degree of independence in daily life through 10 items which has a five level scoring system according to the degree of help and direct observation/interview. The degree of dependence is evaluated on a scale from complete independence (100 points) to complete dependence (0 points). A score of 24 points or less is considered 'total dependence', a score of 25 to 49 is 'severe dependence', a score of 50 to 74 is 'moderate dependence', a score of 75 to 90 is 'mild dependence', and a score of 91 points or more is 'minimal dependence'. The Fall Efficacy Scale-Korea (FES-K) [36] assesses a subject's self-confidence in performing daily activities without falling. Participants express their fear of performing 10 activities on a scale from 1 point being ‘not at all confident’ and 10 points being ‘very confident’, with lower scores indicating greater fear of falling. The Geriatric Depression.
Scale Short Form (GDS-SF) [37] is an effective screening instrument for monitoring mood status and evaluating depression, which includes 15 yes/no questions. A score of 0 to 5 is 'normal’, a score 6 to 9 suggests 'depression', and a score 10 or more is almost always indicative of depression. The EuroQol-5 Dimension (EQ-5D) [38] consists of five domains, mobility (M), self-care (SC), usual activities (UA), pain/discomfort (PD), and anxiety/depression (AD), and each domain is scored as follows: no problem = level 1, some/moderate problems = level 2, extreme problem = level 3. According to the EQ-5D index: \(1-(0.05+0.096\times \mathrm{M}2+0.418\times \mathrm{M}3+0.046\times \mathrm{SC}2+0.136\times \mathrm{SC}3+0.051\times \mathrm{UA}2+0.208\times \mathrm{UA}3+0.037\times \mathrm{PD}2+0.151\times \mathrm{PD}3+0.043\times \mathrm{AD}2+0.158\times \mathrm{AD}3+0.050\times \mathrm{N}3)\), if there is no problem in any of the five areas, the EQ-5D index = 0.95. When the EQ-5D index is divided into quintiles, 20% or less is 'very bad' and 20 to 40% is 'bad', 40 to 60% is 'average', 60 to 80% is 'good', and 80% or more is 'very good'. All assessments were performed by trained physical therapists blinded to the intervention task. A 3D motion capture system consisting of eight infrared cameras was used to measure spatiotemporal and kinematic data. Additionally, two force plates (TF-4060-B, Tec Gihan, Kyoto, Japan) embedded midway along the walkway were used to collect kinetic data. The Helen Hayes marker model was used to collect the trajectories of 15 markers placed on anatomical landmarks [39]. The motion capture system was able to define each marker during collection, allowing for real-time recording of marker position (Fig. 1). Markers were applied to the bilateral anterior superior iliac spine, sacrum, bilateral thigh, knee, shank, ankle, toe, and heel to enable 3D motion capture. Standing calibration was used to obtain a rotation matrix for each limb segment [40,41,42]. The Cosmed K5 wearable metabolic system was used to measure cardiopulmonary energy consumption. The Cosmed K5 portable cardiopulmonary metabolic system was placed on the upper body before respiratory metabolism measurement started, and each participant wore a face mask to ensure that breathing analysis was precise. This system works by using combined breath-by-breath technology to measure oxygen consumption (VO2, L/min) and carbon dioxide production (VCO2, L/min) and thereby evaluates physical performance to support clinical diagnoses. Specifically, it measures the flow, quantity, and volume of oxygen and carbon dioxide in exhaled breath. Broadly, the equipment senses the amount of respiration sent to it by a sample line attached to a turbine when the exhaled gas is discharged through the turbine. Sensors within the device analyze the data. Prior to each experiment, the flow turbine and gas analyzer of the Cosmed K5 analyzer unit were calibrated using a 3-L calibration syringe, gas, and regulator.
Data processing and analysis
Data were automatically converted to 3D coordinates using CORTEX motion capture software version 5.5.0 (Motion Analysis Corporation, Santa Rosa, CA, USA), which has a sampling rate of up to 2000 Hz for cameras and up to 5000 Hz for force plates. A low-band pass filter was used to remove unnecessary noise and better observe the changes according to gait cycle. All data were calculated for each gait cycle using Ortho Track 6.6.4 software (Motion Analysis Corporation). The net cardiopulmonary metabolic energy costs during standing and walking were calculated using the Brockway equation as follows: \(16.58\mathrm{VO}2 + 4.51\mathrm{VCO}2 - 5.90\mathrm{N}\) [43], which subtracts the mean data from the last minute of walking from the mean data from the last minute of baseline measurement [44]. EEm and METs were calculated from the average data in the last minute of walking.
Statistical analysis
All statistical analyses were performed using SPSS version 22.0 (IBM Corporation, Armonk, NY, USA), and the significance level was set at 0.05. Results were calculated as the mean value with standard deviation. To determine the appropriate statistical tests to apply, we checked the distribution of the data for normality. Differences in demographic characteristics between the young-old and old-old were investigated using independent t-tests and chi-square tests. Significant variations in functional assessments, spatiotemporal gait parameters, kinematics and kinetics of gait, and cardiopulmonary metabolic energy efficiency were compared using paired t tests or the Mann–Whitney U test to determine statistically significant differences among groups.
Results
Differences in functional assessments between the young-old and old-old groups
Table 2 presents the functional differences observed between the two groups. The results show that the old-old group had significantly poorer gait and balance function than the young-old group on the SPPB, FSST, and TUG tests (P < 0.01). Moreover, the quality of life (EQ-5D) and mood state (GDS) of the old-old group were significantly lower than those of the young-old group (P < 0.05). However, there were no significant differences between the two groups in K-MMSE, K-MBI, and FES-K scores.
Gait characteristics and differences between older adult groups
Gait characteristics based on spatiotemporal gait parameters were compared and analyzed between the young-old and old-old groups. Results showed that the old-old group had significantly poorer gait function than the young-old group in terms of velocity, stride length, and step length (P < 0.05) (Fig. 3). The groups did not differ in their cadence, stride width, single support, stance, or swing. The results of the comparative analysis of kinematic gait characteristics between groups can be seen in Fig. 4. The hip joint angle during the gait cycle did not differ significantly between groups, but the knee and ankle joint angle were significantly different (Supplementary Table S1). The knee joint angle was more flexed during the initial contact and terminal swing phases in the old-old group than in the young-old group (P < 0.05). The ankle joint angle was less plantarflexed during the pre- and initial-swing phases of the gait cycle in the old-old group than in the young-old group (P < 0.01). The results of comparative analysis of kinetic moment and power gait characteristics of the two groups can be seen in Fig. 4, Supplementary Table S2, and Supplementary Table S3. In the pre-swing phase, the hip joint flexion moment and knee joint absorption power were significantly different between groups. At the peak of the hip joint flexion moment in the pre-swing phase, the old-old group exhibited a significantly less flexed moment than the young-old group (P < 0.05). Knee and ankle moments did not differ significantly between groups. There was a difference between the young-old and old-old groups in peak knee joint power in the pre-swing phase; the old-old group used significantly less absorption power than the young-old group (P < 0.05). Hip and ankle power did not exhibit any substantial differences between groups. The peak ground reaction force during the gait cycle did not differ significantly between groups (Supplementary Fig. S1).
a Joint angles over a gait cycle in the young-old and old-old groups, which differed in knee joint angle during the initial contact and terminal swing phases and ankle joint plantarflexion during the pre- and initial swing phases. b Peak joint moments and power over a gait cycle in the young-old and old-old groups, which differed significantly in hip joint flexion moment and knee joint absorption power in the pre-swing phase. Red rectangular lines represent significant differences (paired t-test, P < 0.05) between groups. Yellow circles represent significant differences (paired t-test, P < 0.05) between groups
Cardiopulmonary metabolic energy consumption during walking
Table 3 shows no significant differences in net VO2, EEm, and MET between the young-old and old-old groups.Preferred treadmill walking speed and distance are presented in Supplementary Table S4. Figure 5 demonstrates that the net cardiopulmonary metabolic energy cost by speed was slightly higher for the old-old group during walking compared to the young-old group, although this difference did not reach statistical significance.
Discussion
In this study, we investigated differences in gait characteristics and cardiopulmonary metabolic energy consumption during walking between young-old (65–74 years) and old-old (75–84 years) participants using a 3D motion capture system and a wearable cardiopulmonary energy measurement system.
Physical performance according to SPPB score was lower in the old-old group than the young-old group, and the FSST and TUG results were slower in the old-old group than the young-old group. In the mood state and quality of life assessments, the GDS-SF score of the old-old group was higher and the EQ-5D score significantly lower than those in the young-old group. Older people with a slower gait speed move at a slow pace when performing daily tasks such as moving from sitting in a chair to standing and walking. Those changes are caused by a decline in muscle strength, reduced physical exercise, joint pain, and fear of falling [45,46,47,48]. Previous research has demonstrated that decreased physical function causes depression to worsen [49], and poorer physical function also causes a decline in social activities, which in turn causes a decrease in quality of life [50]. The results of this study support an impact of decreased physical function in the old-old group based on GDS-SF and EQ-5D scores.
Analysis of spatiotemporal gait parameters showed that the old-old group tended to walk at a slower speed and use shorter step length and stride length than the young-old group. Research suggests that walking speed has a positive correlation with step length and stride length in older adults [51]. Older adults tend to move at slower speeds with shorter strides because of reduced muscle strength and limited ability to control the balance, which affects fall risk [52]. The analysis of spatiotemporal gait parameters in this study revealed that the old-old group walked at a slower speed and used shorter step length and stride length than the young-old group, indicating a higher risk of falls in the older participants. These results suggest various methods such as gait rehabilitation exercises and walking programs be used to improve older people walking ability and reduce the risk of falls to improve quality of life and safety of old adults.
The study's kinematic findings indicated that the old-old group tended to have greater knee flexion upon heel contact than the young-old group. A prior study suggested that a reduced extension angle of the knee joint during initial contact in older adults is linked to weaker quadriceps muscles, knee pain, and slower walking speed [53, 54]. Not extending the knees fully while walking can lead to increased weight load on the knees, which can result in pain and increase the risk of falling [55]. The results suggest that a decrease in the extension angle of the knee joint could potentially serve as an early indication of knee issues associated with aging. The angle of plantarflexion at the ankle usually decreases as people age due to weakened lower limb muscles and reduced power to lift them, leading to slower gait speed [56, 57]. The results of the current study were consistent with previous research, with the old-old group utilizing less plantarflexion in their ankle than the young-old group during the initial swing phase.
Aging reduces the hip extension moment during the loading response phase [58]. In this study, a similar trend was observed, but no significant differences were found between groups. Additionally, the old-old group exhibited significantly lower hip joint maximum flexion moment, which indicates weakness in swinging and kicking the lower limbs to generate forward propulsive force while walking [59]. This is related to decreased absorption force in the knee joint, which results in greater pressure being exerted on the knee joints without effectively absorbing the repelling force when compared to the young-old group [60]. Overall, this means that the joints absorb rather than generate energy at different stages of the gait cycle. This can lead to changes in gait to compensate for joint pain or stiffness with decreased muscle strength, especially in the hip and knee joints, with increased dependence on joint absorption during the preswing phase. These results suggest that eccentric training of the quadriceps muscles might enhance power absorption and alleviate knee joint pain or dysfunction in old-old people.
In cardiopulmonary metabolic energy consumption, despite walking slower than the young-old group, the old-old group used a similar amount of energy in terms of net VO2, EEm, and MET during preferred walking speeds on the treadmill. One possible explanation for the lack of statistically significant difference between the groups is that the average age of the old-old group was 77.74 years, which isn’t much older than 75; another possible reason is that this study recruited very healthy old-old participants.
This study has some limitations. First, although aging affects both gait pattern and muscle activity, this study did not measure muscle activity. In a future study, muscle activation of the lower limbs should be measured alongside kinematic and kinetic data. Second, this study did not calculate rigid body model and COM variables. Therefore, future studies should consider specific variables that describe the essential characteristics of movement. In addition, data should be collected for young adults and the oldest-old population (85 +) to compare age-related gait changes more comprehensively.
Conclusions
In this study, the old-old group had lower functional assessment scores, increased knee flexion angle, impaired ankle joint motion, and insufficient hip and knee joint kinetic values while walking compared to the young-old group. These results will contribute to the development of personalized intervention plans for older adult individuals of varying age to prevent age-related gait issues like falls.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body Mass Index
- SPPB:
-
Short Physical Performance Battery
- FSST:
-
Four-Square Step Test
- TUG:
-
Timed Up and Go
- K-MBI:
-
Korean version of the Modified Barthel Index
- GDS-SF:
-
Geriatric Depression Scale Short Form
- K-MMSE:
-
Korean Mini-mental State Examination
- EQ-5D:
-
EuroQol-5 Dimensions
- FES-K:
-
Fall Efficacy Scale-Korea
References
He W, Goodkind D, Kowal PR. An aging world: 2015. Washington, DC: United States Census Bureau; 2016.
Ouchi Y, et al. Redefining the elderly as aged 75 years and older: Proposal from the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society. Geriatr Gerontol Int. 2017;17(7):1045–7.
Suzuki T. Cross sectional and longitudinal study on the health status among the Japanese elderly from prospective cohort study. Jpn J Health Welfare. 2006;53:1.
Back CY, Joo JY, Kim YK. Association between muscular strengths and gait characteristics of elderly people aged 65 to 74 and 75 and above. J Korea Acad Ind Coop Soc. 2020;21(2):415–22.
Forrest KY, Zmuda JM, Cauley JA. Patterns and correlates of muscle strength loss in older women. Gerontology. 2007;53(3):140–7.
Fujii K, et al. Straight and curved walking abilities and walking self-efficacy in community-dwelling older women with high social functioning: comparison of young-old and old-old adults. Int J Gerontol. 2020;14(3):190–5.
Choi Y-H. A comparative study on health-promoting behavior, life satisfaction and self-esteem of the young and old old. J Korean Acad Community Health Nurs. 2001;12(2):428–36.
Gimmon Y, et al. Gait coordination deteriorates in independent old-old adults. J Aging Phys Act. 2018;26(3):382–9.
Thaler-Kall K, et al. Description of spatio-temporal gait parameters in elderly people and their association with history of falls: results of the population-based cross-sectional KORA-Age study. BMC Geriatr. 2015;15:1–8.
Studenski S, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50–8.
Ito T. Comprehensive physical function assessment in elderly people. Clin Phys Ther. 2017;28:2572–9.
Rasmussen HM, et al. Gait analysis for individually tailored interdisciplinary interventions in children with cerebral palsy: a randomized controlled trial. Dev Med Child Neurol. 2019;61(10):1189–95.
Tung KD, Franz JR, Kram R. A test of the metabolic cost of cushioning hypothesis during unshod and shod running. Med Sci Sports Exerc. 2014;46(2):324–9.
Ortega JD, Farley CT. Individual limb work does not explain the greater metabolic cost of walking in elderly adults. J Appl Physiol. 2007;102(6):2266–73.
Bridenbaugh SA, Kressig RW. Laboratory review: the role of gait analysis in seniors’ mobility and fall prevention. Gerontology. 2011;57(3):256–64.
Patrizio E, et al. Physical functional assessment in older adults. J Frailty Aging. 2021;10:141–9.
Sousa LB, et al. The adults and older adults functional assessment inventory: a rasch model analysis. Res Aging. 2015;37(8):787–814.
McPhee JS, et al. Physiological and functional evaluation of healthy young and older men and women: design of the European MyoAge study. Biogerontology. 2013;14:325–37.
Anderson DE, Madigan ML. Healthy older adults have insufficient hip range of motion and plantar flexor strength to walk like healthy young adults. J Biomech. 2014;47(5):1104–9.
Arnold JB, et al. Differences in foot kinematics between young and older adults during walking. Gait Posture. 2014;39(2):689–94.
Kim B, et al. Characteristics of gait variability in the elderly while walking on a treadmill with gait speed variation. Int J Environ Res Public Health. 2021;18(9):4704.
Noh B, et al. Age-specific differences in gait domains and global cognitive function in older women: Gait characteristics based on gait speed modification. PeerJ. 2020;8:e8820.
Noh B, et al. Associating gait phase and physical fitness with global cognitive function in the aged. Int J Environ Res Public Health. 2020;17(13):4786.
Das Gupta S, et al. Metabolic cost in healthy fit older adults and young adults during overground and treadmill walking. Eur J Appl Physiol. 2021;121(10):2787–97.
Looney DP, et al. Metabolic costs of standing and walking in healthy military-age adults: a meta-regression. Med Sci Sports Exerc. 2019;51(2):346–51.
Van de Walle P, et al. Age-related changes in mechanical and metabolic energy during typical gait. Gait Posture. 2010;31(4):495–501.
LEE D-Y, et al. A normative study of the mini-mental state examination in the Korean elderly. J Korean Neuropsychiatr Assoc. 2002;41(3):508-25.
Hollman JH, McDade EM, Petersen RC. Normative spatiotemporal gait parameters in older adults. Gait Posture. 2011;34(1):111–8.
Berryman N, et al. Comparison of the metabolic energy cost of overground and treadmill walking in older adults. Eur J Appl Physiol. 2012;112(5):1613–20.
Levine JA. Measurement of energy expenditure. Public Health Nutr. 2005;8(7a):1123–32.
Franklin BA, et al. Using metabolic equivalents in clinical practice. Am J Cardiol. 2018;121(3):382–7.
Guralnik JM, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94.
Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil. 2002;83(11):1566–71.
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8.
Jung HY, et al. Development of the Korean version of Modified Barthel Index (K-MBI): multi-center study for subjects with stroke. J Korean Acad Rehabil Med. 2007;31(3):283–97.
Huh J, Lim S, Lee D. Development of the Korean Falls Efficacy Scale (FES-K) for the elderly. Korean J Phys Educ. 2010;49(3):193–201.
Alden D, Austin C, Sturgeon R. A correlation between the Geriatric Depression Scale long and short forms. J Gerontol. 1989;44(4):P124–5.
Balestroni G, Bertolotti G. EuroQol-5D (EQ-5D): an instrument for measuring quality of life. Monaldi Arch Chest Dis. 2012;78(3):155–9.
Kadaba MP, Ramakrishnan H, Wootten M. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8(3):383–92.
Lee HJ, et al. A wearable hip assist robot can improve gait function and cardiopulmonary metabolic efficiency in elderly adults. IEEE Trans Neural Syst Rehabil Eng. 2017;25(9):1549–57.
Lee SH, et al. Exercise with wearable hip-assist robot improved physical function and walking efficiency in older adults. 2022.
Lee SH, et al. Gait performance and foot pressure distribution during wearable robot-assisted gait in elderly adults. J Neuroeng Rehabil. 2017;14(1):1–10.
Brockway J. Derivation of formulae used to calculate energy expenditure in man. Hum Nutr Clin Nutr. 1987;41(6):463–71.
Brehm MA, Becher J, Harlaar J. Reproducibility evaluation of gross and net walking efficiency in children with cerebral palsy. Dev Med Child Neurol. 2007;49(1):45–8.
Angulo J, et al. Physical activity and exercise: strategies to manage frailty. Redox Biol. 2020;35:101513.
Bindawas SM. Relationship between frequent knee pain, obesity, and gait speed in older adults: data from the Osteoarthritis Initiative. Clin Interv Aging. 2016;11:237–44.
Jahn K, Zwergal A, Schniepp R. Gait disturbances in old age: classification, diagnosis, and treatment from a neurological perspective. Dtsch Arztebl Int. 2010;107(17):306–15; quiz 316.
Marcucci L, Reggiani C. Increase of resting muscle stiffness, a less considered component of age-related skeletal muscle impairment. Eur J Transl Myol. 2020;30(2):8982.
Heesch KC, et al. Physical activity, walking, and quality of life in women with depressive symptoms. Am J Prev Med. 2015;48(3):281–91.
Stahl ST, et al. The effects of gait speed and psychomotor speed on risk for depression and anxiety in older adults with medical comorbidities. J Am Geriatr Soc. 2021;69(5):1265–71.
Espy DD, et al. Independent influence of gait speed and step length on stability and fall risk. Gait Posture. 2010;32(3):378–82.
Ribeiro F, Oliveira J. Aging effects on joint proprioception: the role of physical activity in proprioception preservation. Eur Rev Aging Phys Act. 2007;4(2):71–6.
Holm B, et al. Loss of knee-extension strength is related to knee swelling after total knee arthroplasty. Arch Phys Med Rehabil. 2010;91(11):1770–6.
Kwon JW, Son SM, Lee NK. Changes of kinematic parameters of lower extremities with gait speed: a 3D motion analysis study. J Phys Ther Sci. 2015;27(2):477–9.
Hicks C, et al. Reduced strength, poor balance and concern about falls mediate the relationship between knee pain and fall risk in older people. BMC Geriatr. 2020;20(1):1–8.
Bok SK, Lee TH, Lee SS. The effects of changes of ankle strength and range of motion according to aging on balance. Ann Rehabil Med. 2013;37(1):10–6.
Afiah IN, et al. An exploratory investigation of changes in gait parameters with age in elderly Japanese women. Springerplus. 2016;5(1):1–14.
Kim WS, Kim EY. Comparing self-selected speed walking of the elderly with self-selected slow, moderate, and fast speed walking of young adults. Ann Rehabil Med. 2014;38(1):101–8.
Kato K, Hatanaka Y. The influence of trunk muscle strength on walking velocity in elderly people with sarcopenia. J Phys Ther Sci. 2020;32(2):166–72.
Nagano H, et al. Modelling knee flexion effects on joint power absorption and adduction moment. Knee. 2015;22(6):490–3.
Acknowledgements
We thank all participants for enrolling in this study.
Funding
This study was supported by the MSIT (Ministry of Science and ICT), Korea, under the ICT Creative Consilience program (IITP-2021–2020-0–01821) supervised by the IITP (Institute for Information & Communications Technology Planning & Evaluation), and the Korea Medical Device Development Fund grant funded by the Korean government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, the Ministry of Food and Drug Safety) (KMDF-RS-2022–00140478).
Author information
Authors and Affiliations
Contributions
EHC contributed to the experimental design, experimental progress, data analysis, and drafting of the manuscript. SHL and HJL contributed to the experimental design, setting up of the experiment, and data collection. YHK contributed to the experimental design, data interpretation, and manuscript revision. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants recruited through Samsung Medical Center provided informed consent before participating in the present study. This study protocol was approved by the ethics committee of the Samsung Medical Center Institutional Review Board and was performed in accordance with the Declaration of Helsinki.
Consent for publication
Informed consent for publication of identifiable information/ images in open access journal was obtained from all study participants and/or their legal guardian(s).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table S1.
Kinematic joint angle differences between the young-old and old-old groups. Supplementary Table S2. Kinetic peak joint moment differences between the young-old and old-old groups. Supplementary Table S3. Kinetic peak joint power differences between the young-old and old-old groups. Supplementary Table S4. Self-selected treadmill walking speed and distance in the young-old and old-old groups. Supplementally Figure S1. Peak ground reaction force over a gait cycle did not differ significantly between the young-old and old-old groups. IC: Initial contact (0–2%), LR: Loading response (2–12%), MS: Mid-stance (12–31%), TS: Terminal stance (31–50%), PSw: Pre-swing (50–62%), ISw: Initial swing (62–73%), MSw: Mid-swing (73–87%), TSw: Terminal swing (87–100%).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chung, E., Lee, SH., Lee, HJ. et al. Comparative study of young-old and old-old people using functional evaluation, gait characteristics, and cardiopulmonary metabolic energy consumption. BMC Geriatr 23, 400 (2023). https://doi.org/10.1186/s12877-023-04088-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04088-6