Abstract
Background
Around the world, advances in public health and changes in clinical interventions have resulted in increased life expectancy. Multimorbidity is becoming more of an issue, particularly in countries where the population is rapidly ageing. We aimed to determine the prevalence of multimorbidity and disease-specific multimorbidity and examine its association with demographic and socioeconomic characteristics among older adults in India and its states.
Methods
The individual data from the longitudinal ageing study in India (LASI) were used for this study, with 11 common chronic conditions among older adults aged 60 and above years (N = 31,464). Descriptive statistics were used to report the overall prevalence of multimorbidity and disease-specific burden of multimorbidity. Multinomial logistic regression has been used to explore the factors associated with multimorbidity.
Results
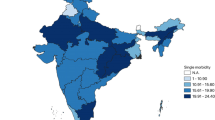
Prevalence of single morbidity was 30.3%, and multimorbidity was 32.1% among older people in India. Multimorbidity was higher among females and in urban areas and increased with age and among those living alone. Hypertension, arthritis and thyroid were highly prevalent among females and chronic lung diseases and stroke were highly prevalent among males. The older people in the state of Kerala had a high prevalence of multimorbidity (59.2%). Multimorbidity was found to be more likely in older age groups of 75–79 years (RR-1.69; CI: 1.53–1.87) and 80 years and above (RR-1.40; CI: 1.27–1.56) and in the Western (RR-2.16; CI: 1.90–2.44) and Southern regions (RR-2.89; CI: 2.57–3.24). Those who were living with a spouse (RR-1.60; CI: 1.15–2.23) were more likely to have multimorbidity. Disease-specific multimorbidity was high in chronic heart disease (91%) and low in angina (64.8%).
Conclusions
The findings suggest that multimorbidity has a positive relationship with advancing age, and disease-specific burden of multimorbidity is higher among chronic heart patients. Comorbidity, especially among those who already have chronic heart disease, stroke, cholesterol or thyroid disorder can have severe consequences on physical functioning, therefore, disease-specific health management needs to be enhanced.
Similar content being viewed by others
Background
Around the world, advances in public health and changes in clinical interventions have resulted in increased life expectancy. Significant demographic shifts have already occurred, and this trend will continue [1]. Still, the quality of life and functional capability have deteriorated due to non-communicable diseases that are strongly linked to ageing [2]. Worldwide, the population of people aged 60 and older is expected almost to double between 2015 and 2050, reaching around 2.1 billion [3]. The burden of chronic diseases has become a public health concern in low and middle income countries, with severe implications for primary and secondary care providers [4]. As a result of higher lifespan and higher exposure to risk factors for chronic diseases, the burden of multimorbidity is quickly rising in India. [5, 6] Multimorbidity, identified as two or more chronic conditions occurring in the same individual at the same time, is becoming more of an issue, particularly in countries where the population is rapidly ageing [7, 8], and it has been linked to a decrease in physical and mental functioning [7, 9] and reduced quality of life [10].
Assuming that a particularly prevalent chronic health problem, such as cardiovascular disease (CVD) or diabetes, may share various related risk factors, it is not uncommon for a single person to have more than one chronic illness. Studies in in western countries report that many people live with two or more chronic diseases due to an increase in life expectancy [11]. Similarly, multimorbidity (62.6%) is shown to be very common than single (18.8%) morbidity among middle-aged and older adult in India (age 45 years and above) [12] Rather than being the exception, multimorbidity is becoming normal [13]. However, several factors such as socioeconomic and demographic characteristics, alongside health and behavioural aspects are considered critical determinants of multimorbidity [7, 14]. In addition, a study shows a direct relationship between unhealthy dietary patterns, chronic disease risk factors and multimorbidity among women [15].
Further, multimorbidity shows a positive relationship with mental comorbidities, increasing with age in women and lower socioeconomic groups in Asian countries [16]. A previous study conducted in the Indian state of West Bengal found a 44% prevalence of multimorbidity [17], another study across the states of India found 42% multimorbidity prevalent in Kerala and 36% in Punjab [18]. Multimorbidity is more strongly predicted by age, economic independence, and lifestyle characteristics in the rural population in a study conducted in Bargarh district of Odisha [19].
There is substantial evidence on the regional variations in the prevalence of multimorbidity in India, attributed to differential healthcare access, utilization, under-reporting and under-diagnosis [20,21,22]. However, the burden of disease-specific multimorbidity and its state-wise prevalence and associated socio-demographic factors is an unexplored arena in India. In the current study, we aimed to assess the prevalence of multimorbidity and disease-specific multimorbidity and examine its association with demographic and socioeconomic characteristics in the older population. Disease-specific burden of multimorbidity was also estimated among older adults in India and its states by selected socio-demographic characteristics.
Data and methodology
This study used data from the Longitudinal Ageing Study in India (LASI), which is a comprehensive nationwide survey that examines the health, economic, and social factors and effects of population ageing in India. The LASI collected data on the functional health, social and economic wellbeing, healthcare, burden of disease of older adults This survey is nationally representative of middle aged and older population in India and its states and union territories (UTs). Major states are considered to have more than 10 million per Census 2011. The LASI comprised a sample of 72,250 individuals aged 45 and above and their spouses from 35 Indian states and UTs, including 31,464 older people aged 60 and above and 6,749 oldest-old people aged 75 and above (excluding Sikkim). It is harmonized internationally with the Health and Retirement Study (HRS) and its sister studies across the world allow cross-national comparisons [23]. The data is publicly available and can be accessed by registration at https://iipsindia.ac.in/sites/default/files/LASI_DataRequestForm_0.pdf.
Variable description
Outcome variable
In this study, outcome variable was chronic morbidity which is recorded as: no morbidity, single morbidity and two and above morbidity. Multimorbidity is the presence of two or more chronic conditions in the same individuals. For the current analysis, the following eleven chronic health conditions were included: hypertension, diabetes, cancer, chronic lung disease, chronic heart disease, stroke, arthritis, depression, cholesterol, thyroid and angina. In LASI, chronic disease was defined by self-report, the self-reported conditions were assessed based on responses to the question, “Have you ever been diagnosed with the following diseases?”.
Independent variables
The control variables were taken into consideration after extensive literature review. Sex of the respondent was available as male and female. Age-group was categorised into 60–64, 65–69,70–74, 75–79 and 80 years and above. Education was categorized into illiterate, primary, secondary and higher. Place of residence was available as rural and urban residence. Marital status was categorized into currently married and others (unmarried, divorced/ separated/ widow). Religion was categorized into Hindu, Muslim and others. Caste was categorized into SC/ST (Scheduled Caste/Schedule Tribe), OBC (Other Backward Classes) and others (including upper caste). Wealth quantile was categorized into five categories: poorest, poorer, middle, richer and richest. The geographical region was categorized into: north, south, east, west, north-east and central region. Tobacco use /smoking was categorised into yes/no. Living arrangement was categorized as living alone, living with spouse, living with children and living with others.
Statistical analysis
Descriptive analysis was conducted to report the prevalence and pattern of morbidity among older participants with different background characteristics. Chi-square test was used to examine the significance of the associations between sociodemographic variables and multimorbidity. A multivariate multinomial logistic regression models are performed to adjust for the possibly confounding impacts of other indicators (Fig. 1). In multivariate analysis, a multinomial logistic regression (MLR) [24] has been used to find out the factors associated with single and multimorbidity.
In MLR model, the estimate for the parameter can be identified compared to a baseline category. The logit models pair each response category with a baseline category, often the most common model is:
The equation simultaneously describes the effects of X (independent variables) on the response categories, the effects vary according to the response paired with the baseline. The probability of each category can be calculated by the following equations:
where, P is the probability; \({b}_{0}\) denotes to the constant; \({b}_{1}\) and \({b}_{n}\) denote to the coefficients; and \({x}_{1}\) and \({x}_{n}\) denote to the number of independent variables.
The estimates of multinomial logistic regression in this study are presented in the form of Relative Risk (RR) and P is the probability of occurrences in the equation. Multinomial logistic regression was used with three categories of multimorbidity: i) no morbidity, ii) single morbidity and iii) multimorbidity. No morbidity was taken as base category and first category of independent variables was taken as the base category. The analysis was carried out in STATA-16 software. We further created a hierarchical heat cluster map and dendrogram using Origin software, to illustrate the disease-specific burden of multimorbidity across the states of India. Hierarchically-clustered heat map is a graphical representation of data, that uses colours to indicate values. The colour band of the cluster map gives information about the cluster map, such as the lower colour band indicating the lowest value of variable and the higher colour band indicating the greatest value of variable. The graph which is produced after doing agglomerative clustering on the data is called a dendrogram. The dendrograms on the sides demonstrate the independent clustering of the rows and the columns.
Results
Table 1: The percentage distribution of sociodemographic characteristics among older adults in India was, over half (52.6%) of the older participants were females. A total of 70.6% of older adults belonged to rural areas. More than 50% of older adults were from the age group of 60–70-year. More than 50% of older adults were illiterate, 22% were primarily educated, 17% were secondary educated, and 3% were highly educated. Around 60% of older adults were currently married. The association of sociodemographic characteristics with morbidity among older adults. All of the sociodemographic characteristics were showing a significant relationship with multimorbidity. Multimorbidity was higher in females than males and higher in the urban area (42.7%) than in rural area (27.7%). The prevalence of multimorbidity and single morbidity increased with age, while slightly decreased in 80 and above age group. Single morbidity decreased with education while slightly increased in higher education. Multimorbidity increased with education while slightly decreased in higher education. Currently married women had less morbidity than others groups. Hindu and others religion had less multimorbidity than those from Muslim religion. SC/ST (24.7%) category had less multimorbidity than OBC (33.7%) and others category (39.7%). No much variation was observed in wealth groups for single morbidity but, multimorbidity increased in higher wealth quintiles. People from the north-east (35%) had high and those from the East (28.6%) had less single morbidity while, those from the south region (40.1%S) had high and those from central region (21.9%) had less multimorbidity. Those living alone had high (35.6%) and those living with others (29.4%) had less single morbidity while older adults living with children (34.5%) had high multimorbidity.
Table 2: The factors associated with multimorbidity are shown in Table 3. No morbidity was considered the reference category, and the first category was regarded as the reference category of independent variables. The female respondents were 1.3 times more likely to have single morbidity and 1.6 times more likely to have multimorbidity compared to male respondents. On the other hand, respondents from the urban areas were 1.2 times more likely to have single morbidity and 1.6 times more likely to have have multimorbidity than rural counterparts.
The age group was significantly associated with multimorbidity. The people in the age group of 80 years and above were 1.4 times more likely to have multimorbidity compared to the 60–64-year age group. In case of education, older adults with primary, secondary and higher education were 1.5 times more likely to have multimorbidity compared to illiterate older adults. The wealth index was significantly associated with multimorbidity; 1.1 times in poorer, 1.2 times in the middle, 1.3 times in richer and 1.5 times in richest more likely to have single morbidity and 1.3 times in poorer, 1.5 times in the middle, two times in richer and 2.6 times in richest more likely to have multimorbidity than poorest category. In case of the region, it was more likely to have single morbidity, 1.2 times in the north, 1.3 times in west and 1.4 times in south. And it was more likely to have multimorbidity, 1.2 times in central, 1.7 times in the east, 1.9 times in the north, 2.2 times in west and 2.9 times in south as compared to the north-east region. The people who reported using tobacco/smoke were 1.1 times more likely to have single morbidity than not users. Those who were living with spouse were 1.5 times more likely to have single morbidity than living alone.
Table 3: shows the prevalence of disease-specific multimorbidity by sociodemographic characteristics. Some diseases had high prevalence of comorbidity. Females had high prevalence of disease specific multimorbidity like-diabetes (86.3%), chronic lung disease (80.7%), arthritis (74%) than male. Others social group had high prevalence of disease-specific multimorbidity of cancer (89.9%), chronic heart disease (92.6%) and stroke (73.7%) than SC/ST and OBC groups. Disease specific multimorbidity was high in those living with children in case of diabetes (87.5%) and chronic lung disease (80.2%).
Table 4: shows the prevalence of disease specific multimorbidity in India and its major states. Multimorbidity was higher in chronic heart disease (91%) followed by cholesterol (89.2%) and was lower in angina (64.8%) followed by arthritis (70.5%) at national level. In terms of specific disease of hypertension, multimorbidity was high in Kerala (83.7%) followed by Karnataka (80.8%) and lowest in Haryana (49.4%) followed by Jharkhand (56.3%). In terms of specific disease of diabetes, multimorbidity was high in Jammu & Kashmir (89.5%%) followed by Karnataka (88.4%) and lowest in Chhattisgarh (64.3%). Cancer multimorbidity was high in Tamil Nadu, Madhya Pradesh, Gujrat and Delhi (100%) and lowest in Chhattisgarh (0%). The multimorbidity of chronic lung disease was high in Karnataka (91%) and the lowest in Chhattisgarh (59.27%). The multimorbidity of chronic heart disease was high in Karnataka (98.23%) and the lowest in Chhattisgarh (78.19%). Strike multimorbidity was high in Punjab (97.8%) and lowest in Tamil Nadu (41.22%). Arthritis multimorbidity was high in Kerala (88.5%) and lowest in Chhattisgarh (53%). Depression multimorbidity was high in Kerala (94.32%) and lowest in Delhi (54.63%). Cholesterol multimorbidity was high in Uttarakhand, Uttar Pradesh, Telangana, Madhya Pradesh, Jharkhand, Jammu & Kashmir, Delhi, Chhattisgarh & Andhra Pradesh (100%) and lowest in Karnataka (57.46%). Thyroid multimorbidity was high in Chhattisgarh (100%) and lowest in Madhya Pradesh (57.76%). Angina multimorbidity was high in Kerala (92.84%) and lowest in Jharkhand (40.29%).
The heat map shows the data value for each state and morbidity (Fig. 2a and b). Any patterns in the heat map may indicate an association between the state and morbidity. The colour band on the right side of the cluster map indicates information about the cluster map, such as dark orange showing the lowest disease specific multimorbidity and dark skyblue showing the highest disease specific multimorbidity among older adults in India. The height of dendrogram represent the distance between two cluster, higher the hight of dendrogram lower the similarity between the cluster and vise-versa. In our study, India and Bihar shows the same pattern of disease specific multimorbidity with euclidean distance (0.07) there after Odisha and Jharkhand show the second closet disease specific multimorbidity pattern with euclidean distance (0.09). Chronic lung disease and cancer, chronic lung disease and arthritis and hypertension and diabetes show the similar pattern of disease among different states in India with euclidean distance values (0.25, 0.34 and 0.35) respectively.
Discussion
Globally, multimorbidity is arguably the most significant health care challenge with its wide range of adverse consequences. Despite multimorbidity being extensively studied, only a few research has looked at the combinations or patterns of morbidity in LMICs [25]. The present Study assessed the prevalence and correlates of multimorbidity and disease-specific multimorbidity among older people in India using the LASI dataset. Present study showed that approximately one-third of older population had single morbidity, and another one-third of them had multimorbidity in India.
Prevalence of multimorbidity in this study varies with that of other countries; it may be due to variation in socioeconomics, age pyramid, reporting of morbidity cases and health care system. For instance, a previous study n Germany showed that 62% older people over the age of 65 years were having multimorbidity [26], similarly, 45% of multimorbidity were found among people age > 65 years in Kosovo [27], 55% among those age above 77 years in Sweden [28] A study in Brazil found a prevalence of 29% of multimorbidity among older adults [29] while another study in Ghana found that 38.8% of outpatients had multimorbidity [30].
Further studies conducted in India in the past one decade showed the varying prevalence of multimorbidity across the states. A study in South India found a prevalence of morbidity in one-third of the population [31], another study in Odisha found less than one third prevalence of multimorbidity, where women had one-third and men had one fourth percent of multimorbidity [32]. Another study in India depicted that overall, 32% of respondents were having multimorbidity, among them 30.6% were multimorbid and among them 21.3% were people age 60–69 years [33]. In a study based on the LASI pilot survey, the average multimorbidity was 9%, whereas single illness was 17.4% among older Indian adults. Kerala had the highest rate of multimorbidity (30%), followed by Punjab (22.4%) [20]. The current Study also revealed a significant variance in single morbidity and multimorbidity among Indian states and regions.
The most often detected chronic conditions were hypertension and arthritis and it was shown to be the most often occurring comorbidities in studies in LMICs [19, 20, 34]. Some leading morbidities among Indian population reported in previous studies include diabetes, chronic lung diseases, arthritis and hypertension [35]. A primary study conducted in rural Tamilnadu showed that the, cataract (57%) was very common morbidity followed by bone and joint disease (43.3%). Other morbidities were, hypertension (14%), heart disease (9%), diabetes (8.1%) and asthma (6%) among older persons in rural Tamilnadu. Another study showed that overall, 63% of older adults suffered from at-least one non-communicable disease and 30.7% of them had multimorbidity [21]. Most common combination of morbidities were, high blood pressure and arthritis (7.5%), cataract and arthritis (5.3%) and high blood pressure and diabetes (4.7%). In our study, highest prevalence of comorbidity was hypertension followed by angina, arthritis, diabetes, chronic lung disease, chronic heart disease, depression, stroke, cholesterol, thyroid and lowest cancer.
Furthermore, it is documented that multimorbidity becomes more common progressively with age [21, 36,37,38]. In our study, morbidity was higher in the age group of 75–79 years and slightly decreased in the age group of 80 years and above. Again, multimorbidity was higher in females (34.9%) than males (29.7%), which is similar to previous findings and may be attributed to lower healthcare use, poor socioeconomic status, living and working environments and adverse life events [39, 40], Further, the socioeconomic disparities in the prevalence of multimorbidity were observed in this study. As nations get wealthier, the adoption of risky health behaviours tends to shift from higher to lower socioeconomic categories [41, 42]. According to several cross-sectional studies, multimorbidity is more prevalent among older individuals with lower educational and income levels [4, 43,44,45]. However, in our study, multimorbidity was highly prevalent among those belonging to the richest wealth quintile and those who are residing in urban areas. This suggests that the affluence of disease still exists in Indian context and the pattern has not changed in the country yet. On the other hand, the prevalence of multimorbidity was less prevalent among older adults who engaged in moderate or vigorous physical activity than those who were physically active, suggesting the protective effect of healthy behaviour on multiple disease prevalence. Nonetheless, alcohol and tobacco use were not associated with multimorbidity in this study. This may be due to the nature of variables which capture only ever use, suggesting the need for future research.
However, our findings confirm that the factors such as alcohol and tobacco consumption increase the risk of burden of majority of the disease-specific multimorbidity. This is particularly higher in case of non-communicable diseases such as cancer, chronic lung disease, chronic heart disease and angina. These findings have important policy implications. Notably, government policies have aimed to promote healthier lifestyles among individuals, but with limited success. Therefore, policy makers and health care providers should design effective health-promotion programs, especially among socioeconomically advantaged groups, who are found to be at increased risk of disease-specific burden of multimorbidity in this study. Thus, strategies to reduce the risk of multimorbidity may include facilitating more space for physical exercises, restricting marketing of tobacco and alcohol to avoid unhealthy behaviors and making smoking/drinking cessation services more accessible to the population; and conducting large-scale education campaigns among community-dwelling older persons to encourage healthier lifestyles.
Finally, our findings revealed large regional variations in disease-specific multimorbidity. Also, some diseases, in particular, have a high prevalence of multimorbidity in some states, which means that having multimorbidity indicates the increased presence of a particular disease occurring with other diseases. Around 91 percent of older people with chronic heart disease had multimorbidity. In terms of cholesterol, older persons from Uttar Pradesh, Delhi, and Bihar had higher burden of cholesterol-specific multimorbidity, whereas older adults in Rajasthan had higher prevalence of multimorbidity with chronic heart disease [46]. Moreover, higher burden of disease-specific multimorbidity was observed in case of chronic heart disease, stroke, cholesterol and thyroid disorder than other diseases. Among these, burden of chronic heart disease was highest in the states of Karnataka and Kerala. This may indicate the higher prevalence of unhealthy lifestyle among older people in the southern states of India, which calls for special attention in terms of policy and programs. Disease-specific policies should also focus on regional variations and target the subpopulations from states with higher burden of disease-specific multimorbidity.
Limitations of the study
The present study has certain limitations. Due to the cross-sectional nature of the data used in our study, causation could not be established. Our study could only identify associations and longitudinal analyses may clarify the causal relationships among socioeconomic and demographic variables and multimorbidity. Also, our knowledge of the severity of morbidity and multimorbidity is constrained by the fact that the available statistics only provide information on prevalence and determinants. More importantly, the LASI did not include the institutionalized older adults who are expected to have more health problems and higher burden of multimorbidity than older adults in community-dwellings. Further, self-reported nature of several varriables including chronic conditions may lead to recall and reporting biases which might affect the current findings. The prevalence of diseases may be underestimated if some respondents are undiagnosed and may lead to biases, particularly if undiagnosed respondents are disproportionately of lower ocioeconomic status. Self-report of multimorbidity may also imply that some proportion of respondents who were diagnosed and treated with particular diseases may not have the disease at same time or at the time of survey.
Conclusion
In conclusion, our study based on multimorbidity among older adults in India, shows 32% multimorbidity and 30% single morbidity. Multimorbidity was high in women and in urban areas. Since multimorbidity can have serious cognitive and functional consequences with growing older population in developing nations such as India, one of the important implications of our findings is that researchers and policy-makers should collaborate to develop effective intervention strategies, and health-promotional programmes and to train the health care personnel to minimize the disease-specific burden of multimorbidity. The findings suggest that multimorbidity has a positive relationship with advancing age, and disease-specific burden of multimorbidity is higher among chronic heart patients. Comorbidity, especially among those who already have chronic heart disease, stroke, cholesterol or thyroid disorder can have severe consequences on physical functioning, therefore, disease-specific health management needs to be enhanced. By enhancing public care facilities and increasing investments in the public health sector, policy steps should be adopted to encourage treatment seeking among older Indian population. Further, by introducing a specific policy push, the emphasis should be on the demands of geriatric healthcare, especially among the cardiovascular patients in Southern states of India. All parties involved, including the government, community health workers, and civil society, must play a crucial role in achieving this.
Availability of data and materials
The LASI datasets used in our study can be downloaded from the Gateway to Global Aging Data. Data are anonymized and available by request from the Gateway. To access the public release data from the Gateway to Global Aging Data, you must first register and get a username and password at- https://g2aging.org/login&r=%5Eq%5E.
References
WHO. Aging and health: key fats. Geneva: WHO; 2018. https://www.who.int/ news-room/fact-sheets/detail/ageing-and-health. World Population Ageing 2015 (ST/ESA/SER.A/390).
Murray CJ, Barber RM, Foreman KJ, Ozgoren AA, Abd-Allah F, Abera SF, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;386(10009):2145–91.
United Nations, The World Population Prospects: The 2015 Revision. Department of Economic and Social Affairs, Population Division. New York: United Nations; 2015.
Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10(4):430–9.
Barik M, Panda SN, Tripathy SS, Sinha A, Ghosal S, Acharya AS, et al. Is multimorbidity associated with higher risk of falls among older adults in India? BMC Geriatr. 2022;22(1):1–8.
Puri P, Sinha A, Mahapatra P, Pati S. Multimorbidity among midlife women in India: well-being beyond reproductive age. BMC Womens Health. 2022;22(1):1–15.
Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009;7(4):357–63.
Le Reste JY, Nabbe P, Rivet C, Lygidakis C, Doerr C, Czachowski S, et al. The European general practice research network presents the translations of its comprehensive definition of multimorbidity in family medicine in ten European languages. PloS one. 2015;10(1):e0115796.
Arokiasamy P, Uttamacharya U, Jain K, Biritwum RB, Yawson AE, Wu F, et.at. The impact of multimorbidity on adult physical and mental health in low-and middle-income countries: what does the Study on global ageing and adult health (SAGE) reveal? BMC medicine. 2015;13(1):1–16.
Wei MY, Kawachi I, Okereke OI, Mukamal KJ. Diverse cumulative impact of chronic diseases on physical health–related quality of life: implications for a measure of multimorbidity. Am J Epidemiol. 2016;184(5):357–65.
van der Heide I, Snoeijs S, Melchiorre MG, Quattrini S, Boerma W, Schellevis F, Rijken M. Innovating care for people with multiple chronic conditions in Europe. Brussels: ICARE4EU. 2015.
Khan M, Malik MA, Akhtar SN, Yadav S, Patel R. Multimorbidity and its associated risk factors among older adults in India. BMC Public Health. 2022;22(1):1–8.
Stange KC. In this issue: challenges of managing multimorbidity. 2012.
Kadam UT, Croft PR, North Staffordshire GP Consortium Group. Clinical multimorbidity and physical function in older adults: a record and health status linkage study in general practice. Fam Pract. 2007;24(5):412–9.
Olivares DE, Chambi FR, Chañi EM, Craig WJ, Pacheco SO, Pacheco FJ. Risk factors for chronic diseases and multimorbidity in a primary care context of central Argentina: a web-based interactive and cross-sectional study. Int J Environ Res Public Health. 2017;14(3):251.
Low LL, Kwan YH, Ko MSM, Yeam CT, Lee VSY, Tan WB, Thumboo J. Epidemiologic characteristics of multimorbidity and sociodemographic factors associated with multimorbidity in a rapidly aging Asian country. JAMA Netw Open. 2019;2(11):e1915245–e1915245.
Vadrevu L, Kumar V, Kanjilal B. Rising challenge of multiple morbidities among the rural poor in India—a case of the Sundarbans in West Bengal. Int J Med Sci Public Health. 2016;5:343–50.
Chobe M, Chobe S, Dayama S, Singh A, Metri K, Basa JR, Raghuram N. Prevalence of Non-Communicable Diseases and Its Associated Factors Among Urban Elderly of Six Indian States. Cureus. 2022;14(10).
Banjare P, Pradhan J. Socioeconomic inequalities in the prevalence of multimorbidity among the rural elderly in Bargarh District of Odisha (India). PLoS ONE. 2014;9(6):e97832.
Arokiasamy P, Uttamacharya, & Jain, K. Multi-morbidity, functional limitations, and self-rated health among older adults in India: cross-sectional analysis of LASI pilot survey, 2010. SAGE Open. 2015;5(1):2158244015571640.
Mini GK, Thankappan KR. Pattern, correlates and implications of non-communicable disease multimorbidity among older adults in selected Indian states: a cross-sectional study. BMJ Open. 2017;7(3):e013529.
Chauhan S, Srivastava S, Kumar P, Patel R. Decomposing urban-rural differences in multimorbidity among older adults in India: a study based on LASI data. BMC Public Health. 2022;22(1):1–14.
International Institute for Population Sciences (IIPS), National Programme for Health Care of Elderly (NPHCE), MoHFW, Harvard T. H. Chan School of Public Health (HSPH) and the University of Southern California (USC) 2020. Longitudinal Ageing Study in India (LASI) Wave 1, 2017-18, India Report, International Institute for Population Sciences, Mumbai
Hosmer Jr DW, Lemeshow S, Sturdivant RX. Applied logistic regression (Vol. 398). New York: Wiley; 2013.
Prados-Torres A, Calderón-Larrañaga A, Hancco-Saavedra J, Poblador-Plou B, van den Akker M. Multimorbidity patterns: a systematic review. J Clin Epidemiol. 2014;67(3):254–66.
van den Bussche H, Schön G, Kolonko T, Hansen H, Wegscheider K, Glaeske G, Koller D. Patterns of ambulatory medical care utilization in elderly patients with special reference to chronic diseases and multimorbidity-results from a claims data based observational study in Germany. BMC Geriatr. 2011;11(1):1–10.
Jerliu N, Toçi E, Burazeri G, Ramadani N, Brand H. Prevalence and socioeconomic correlates of chronic morbidity among elderly people in Kosovo: a population-based survey. BMC Geriatr. 2013;13(1):1–9.
Marengoni A, Winblad B, Karp A, Fratiglioni L. Prevalence of chronic diseases and multimorbidity among the elderly population in Sweden. Am J Public Health. 2008;98(7):1198–200.
Nunes BP, Thumé E, Facchini LA. Multimorbidity in older adults: magnitude and challenges for the Brazilian health system. BMC Public Health. 2015;15(1):1–11.
Nimako BA, Baiden F, Sackey SO, Binka F. Multimorbidity of chronic diseases among adult patients presenting to an inner-city clinic in Ghana. Glob Health. 2013;9(1):1–7.
Bhojani U, Beerenahalli TS, Devadasan R, Munegowda CM, Devadasan N, Criel B, Kolsteren P. No longer diseases of the wealthy: prevalence and health-seeking for self-reported chronic conditions among urban poor in Southern India. BMC Health Serv Res. 2013;13(1):1–10.
Pati S, Sinha R, Panda M, Puri P, Pati S. Profile of multimorbidity in outpatients attending public healthcare settings: A descriptive cross-sectional study from Odisha, India. J Fam Med Prim Care. 2021;10(8):2900.
Pati S, Agrawal S, Swain S, Lee JT, Vellakkal S, Hussain MA, Millett C. Non communicable disease multimorbidity and associated health care utilization and expenditures in India: cross-sectional Study. BMC Health Serv Res. 2014;14(1):1–9.
Khanam MA, Streatfield PK, Kabir ZN, Qiu C, Cornelius C, Wahlin Å. Prevalence and patterns of multimorbidity among elderly people in rural Bangladesh: a cross-sectional study. J Health Popul Nutr. 2011;29(4):406.
Pati S, Swain S, Hussain MA, Van Den Akker M, Metsemakers J, Knottnerus JA, Salisbury C. Prevalence and outcomes of multimorbidity in South Asia: a systematic review. BMJ open. 2015;5(10):e007235.
Walker AE. Multiple chronic diseases and quality of life: patterns emerging from a large national sample Australia. Chronic Illn. 2007;3(3):202–18.
Salisbury C, Johnson L, Purdy S, Valderas JM, Montgomery AA. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2011;61(582):e12–21.
Business and Industry Advisory Committee. Meeting the Challenges of Ageing and Multiple Morbidities. OECD 50th Anniversary Conference on Health Reform, Paris, June. Fortin, M., Bravo, G., Hudon, C., Vanasse, A., & Lapointe, L. (2005). Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med. 2011;3(3):223–228.
Alimohammadian M, Majidi A, Yaseri M, Ahmadi B, Islami F, Derakhshan M, et.at. Multimorbidity as an important issue among women: results of a gender difference investigation in a large population-based cross-sectional study in West Asia. BMJ open. 2017;7(5):e013548.
Hosseinpoor AR, Bergen N, Kunst A, Harper S, Guthold R, Rekve D, et al. Socioeconomic inequalities in risk factors for non communicable diseases in low-income and middle-income countries: results from the World Health Survey. BMC public Health. 2012;12(1):1–13.
Blakely T, Hales S, Kieft C, Wilson N, Woodward A. The global distribution of risk factors by poverty level. Bull World Health Organ. 2005;83:118–26.
Schram MT, Frijters D, van de Lisdonk EH, Ploemacher J, de Craen A, J, de Waal MW. Et.al. Setting and registry characteristics affect the prevalence and nature of multimorbidity in the elderly. J Clin Epidemiol. 2008;61(11):1104–12.
Agborsangaya CB, Lau D, Lahtinen M, Cooke T, Johnson JA. Multimorbidity prevalence and patterns across socioeconomic determinants: a cross-sectional survey. BMC Public Health. 2012;12(1):1–8.
Kirchberger I, Meisinger C, Heier M, Zimmermann AK, Thorand B, Autenrieth CS, Döring A. Patterns of multimorbidity in the aged population. Results from the KORA-Age study. PloS one. 2012;7(1):e30556.
Gebregziabher M, Ward RC, Taber DJ, Walker RJ, Ozieh M, Dismuke CE, Et.al. Ethnic and geographic variations in multimorbidty: Evidence from three large cohorts. Soc SciMed. 2018;211:198–206.
Gupta R, Guptha S, Sharma KK, Gupta A, Deedwania P. Regional variations in cardiovascular risk factors in India: India heart watch. World J Cardiol. 2012;4(4):112.
Acknowledgements
Not applicable
Funding
Authors did not receive any funding to carry out this research.
Author information
Authors and Affiliations
Contributions
PP and HS conceptualized the study. PP is responsible for the analysis. PP, TM and HS contributed to the interpretation of the data, and critically revised all versions of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The data is freely available in the public domain and survey agencies that conducted the field survey for the data collection have collected prior consent from the respondent. It also guaranteed that the participants' privacy was protected and that informed consent was obtained from respondents during the survey. Therefore, prior ethical approval for using the datasets was not required.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Patel, P., Muhammad, T. & Sahoo, H. The burden of disease-specific multimorbidity among older adults in India and its states: evidence from LASI. BMC Geriatr 23, 53 (2023). https://doi.org/10.1186/s12877-023-03728-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-03728-1