Abstract
Background
There are several national and international criteria available for identifying potentially inappropriate medications (PIMs) for older people. The prevalence of PIM use may vary depending on the criteria used. The aim is to examine the prevalence of potentially inappropriate medication use in Finland according to the Meds75+ database, developed to support clinical decision-making in Finland, and to compare it with eight other PIM criteria.
Methods
This nationwide register study consisted of Finnish people aged 75 years or older (n = 497,663) who during 2017–2019 purchased at least one prescribed medicine considered as a PIM, based on any of the included criteria. The data on purchased prescription medicines was collected from the Prescription Centre of Finland.
Results
The annual prevalence of 10.7–57.0% was observed for PIM use depending on which criteria was used. The highest prevalence was detected with the Beers and lowest with the Laroche criteria. According to the Meds75+ database, annually every third person had used PIMs. Regardless of the applied criteria, the prevalence of PIM use decreased during the follow-up. The differences in the prevalence of medicine classes of PIMs explain the variance of the overall prevalence between the criteria, but they identify the most commonly used PIMs quite similarly.
Conclusion
PIM use is common among older people in Finland according to the national Meds75+ database, but the prevalence is dependent on the applied criteria. The results indicate that different PIM criteria emphasize different medicine classes, and clinicians should consider this issue when applying PIM criteria in their daily practice.
Similar content being viewed by others
Background
Inappropriate prescribing refers to the prescribing of a medication that significantly increases the risk of adverse drug events (ADEs) [1]. Potentially inappropriate medications (PIMs) are defined as medicines or medicine classes in which the risks of ADEs usually outweigh the clinical benefits and therefore these medicines should be avoided in most circumstances or for certain diseases or conditions among older people [2]. Use of PIMs has been associated with more than twofold increased odds of ADEs in people aged 65 years or older [3]. Furthermore, PIM use is associated with an increased risk of clinically important drug-drug interactions [4], hospitalizations [5] and consequently higher health care costs [6]. Despite the known risks, PIM use is common among the older population with a prevalence of 23% in Europe [7].
Several sets of criteria have been published to identify PIMs. For example, the first published criteria, the Beers criteria [2] from the United States, and two European criteria: the Laroche criteria [8] and the Screening Tool of Older Persons’ Potentially Inappropriate Prescriptions and Screening Tool to Alert to Right Treatment (STOPP/START) [9]. Later, PIM criteria have been nationally modified and published in many countries, including the Nordic countries [10,11,12,13]. However, criteria are not always applicable to other countries since PIM criteria development is country-specific with regard to prescribing practices and the available pharmaceutical market, leading to different PIM ratings. This raises concerns about their generalizability, reliability and feasibility in other settings.
Previously, several studies have compared different PIM criteria and analyzed prevalence of PIM use in various settings. For example, a prevalence range of 25–72% in PIM use has been reported when comparing the Beers criteria with STOPP criteria in studies conducted in nursing homes, hospitals and among community-dwelling older people aged 65 years or older [14,15,16]. Moreover, a previous nationwide register study [17] in the Swedish population aged 65 years or older compared PIMs according to five criteria and found a prevalence range of 16–-24%. Hence, it can be concluded that prevalence of PIMs varies depending on the applied criteria.
The Finnish Meds75+ database is a national database for PIM use developed to support clinical decision-making on the pharmacotherapy of people aged 75 years or over [13]. An earlier nationwide study [18] including all Finnish citizens aged 74 years or older found that the prevalence of reimbursed PIMs according to the Meds75+ database varied from 27 to 39% between Finnish hospital districts in 2011. However, the Meds75+ database has not been previously compared with other criteria.
Since the Meds75+ database and several criteria have been developed to be used in Europe, a comparison of the contents and the prevalence of PIMs is warranted. We hypothesized that different PIM criteria provide varying information about prevalence of PIM use. Therefore, our aim was to perform a cross-sectional study using nationwide register-based data to describe the prevalence of PIM use in Finland. The second aim was to provide comparing knowledge about the content of the Meds75+ database and eight other PIM criteria and to evaluate which differences in PIM rating explain the variation in prevalence.
Methods
Description of the Meds75+ database
The Meds75+ database is the national Finnish criteria used to identify PIMs and is maintained by the Finnish Medicines Agency Fimea [13]. The aim is to improve medication safety in primary health care and not only to classify medicines as inappropriate for persons aged 75 years or older but also to indicate medicines that are suitable or can be used with caution and is primarily intended for use by general practitioners. The database includes all drug substances or combinations used in primary health care and have at least 500 users aged 75 years or older annually. In addition, over-the-counter (OTC) medicines which are considered relevant for older persons are included. However, the database does not include substances used only in hospitals or in highly specialized care. Other PIM criteria, such as the Beers criteria, STOPP/START criteria, Laroche criteria and EU(7)-PIM list, have been used in the Meds75+ database development process [13], but the recommendations have been adjusted to the national treatment practices of Finland. The database places each drug substance in one of the following four categories: suitable for older persons (category A), present evidence or experience on use in older persons is vague or efficacy of the medicine is insufficient (B), suitable for older persons, with specific cautions (C), and avoid use in older persons (D). In addition, the database contains summarized information on the effects, dosing and most typical ADEs of the medicine. In this study, PIMs are defined according to category D. Since the database is continuously updated to consider the current prescribing practices and medicines on the Finnish market, the list of PIMs was formed on 2 July 2020.
Other PIM criteria included
We applied the following inclusion criteria when selecting other PIM criteria for this study: (1) intended for use in older people aged 65 years or older, (2) includes drug-specific statements about medicines that should be avoided by older people in most circumstances (explicit criteria), (3) developed in Nordic countries, Europe or Northern America, and (4) published in 2006 or later (latest version included). In addition, we applied the following exclusion criteria: (1) PIM statements that are related just to certain diseases or conditions and (2) the latest publication of criteria published in 2005 or before.
First we included the four PIM criteria applied in the Meds75+ database development process (the Beers criteria, STOPP/START criteria, Laroche criteria and EU(7)-PIM list). Furthermore, in order to focus on the Meds75+ database and prescribing guidelines in Northern Europe, we searched the literature and utilized reviews [19,20,21] to select criteria from other Nordic countries. Moreover, to be able to evaluate the classification discrepancies across Europe, we included the PRISCUS (Latin for “old and venerable”) list [22] since the preliminary EU(7)-PIM list also contained PIMs from the German criteria [23]. Altogether, a total of nine sets of PIM criteria were included and are described in Table 1.
The latest version of the Beers criteria [24] is divided into five sections, of which medications that are potentially inappropriate in most older adults were considered as PIMs in this study. Similarly, the following statement, from the nine sets of Swedish quality indicators for evaluation of older patients’ drug therapies (later the Swedish criteria) [12] were considered as PIMs: medicines that should be avoided unless there is a special reason for using them. The STOPP/START criteria [27] also include potential prescribing omissions in the START criteria, so in this study we only considered a list of PIMs in the STOPP criteria. Although, since STOPP criteria includes many statements considering PIM use in specific medical conditions, requiring clinical information, we applied the statements partially.
From the Norwegian General Practice (NORGEP) criteria [10], we used part A (regular use should be avoided) of the version updated in 2015 for assessing medication for nursing home residents (NORGEP-NH) [25], since it is based on the original NORGEP criteria and a comprehensive literature search. From the Danish Red-Yellow-Green list, drugs in the red category (drugs that should not be used in older people) were considered as PIMs. Although the Danish list was updated in 2016, the original edition was selected, since it has been published in English with ATC codes [26] and therefore is more accurate and leaves no room for interpretation.
Identifying potentially inappropriate medications
Drug-specific PIM statements were extracted from each of the nine criteria and entered into an Excel file. One author (JP) examined the selected criteria and created the summary table. If the criteria included a statement to avoid a medicine class, the statement was documented in the summary for medicines mentioned by name in other criteria. For example, the NORGEP-NH includes a statement about regular use of hypnotics. According to the Anatomical Therapeutic Chemical (ATC) classification system by the World Health Organization [28], the code for hypnotics and sedatives is N05C. Based on this international drug classification, the statement from NORGEP-NH was documented for drugs whose ATC code is N05C and those listed in other included criteria. Unclear classifications were discussed among the three authors (JP, JJ, EJ).
We did not consider the following kinds of PIM statements from the final table: (1) concurrent use of two or more drugs (e.g., warfarin combined with non-steroidal anti-inflammatory drugs (NSAIDs)), (2) PIMs and specific conditions (e.g., Angiotensin Receptor Blockers in patients with hyperpotassemia), (3) PIMs and restriction of treatment duration or dose, (4) PIMs with limited research evidence or experience among older people, and (5) anticholinergic medicines without a specific active substance. Not including a statement was related to the restrictions on the data. First, the statements requiring additional clinical information (e.g., diagnosis, renal insufficiency, dosage, treatment duration) were not applied since such details could not be captured from the national prescription register. Second, some of the included criteria (e.g., Meds75+ database, Beers criteria) contain a special category for medicines with specific caution (e.g. use with caution, present evidence or experience with use in older persons is vague). Overall, the comparison of criteria focused on identifying PIMs to avoid generally without considering additional clinical information. This research strategy collected a summary of 352 ATC codes considered as PIMs (see Additional file 1).
The summary was screened using both the Social Insurance Institution (SII) of Finland’s Medicinal Products Database and Finnish Medicines Agency’s FimeaWeb to exclude medicines not available in Finland. If the medicine was available on the market only in combination (e.g., codeine), the medicine was still included. In addition, if the medicine was available both as a single active substance and in combination (e.g., oxycodone), both ATC codes were included. Finally, after screening the summary, 172 ATC codes were considered as PIMs available on Finnish pharmaceutical market (see Additional file 1).
Data collection and statistical analysis
Since the Meds75+ database is intended to be used for older people aged 75 years or older this age limit was applied in the study population. In this retrospective cross-sectional study, the study population was drawn from the entire population of older people aged 75 years or older in Finland in 2017–2019. We obtained data on purchased prescription medicines, which reflects PIM use better than prescriptions only. The Prescription Centre of Finland is a national register held by the SII and contains all human medicine prescriptions and their medicine purchases delivered from pharmacies in Finland since 2017 [29, 30]. The database covers all Finnish citizens except persons living permanently in institutions (< 1% of persons aged ≥75 years) and medicines given in hospitals. The study cohort consisted of older people who had purchased at least one prescription medicine, reimbursed by National Health Insurance (tax-supported public social security coverage) or not, considered as a PIM (see Additional file 1) in 2017–2019 and were aged 75 years or over at the time of purchase. In order to calculate the total number of PIMs purchased by an individual, we used a pseudonymized identification number for every person.
Altogether the data consisted of 523,263 older person and their 14,488,277 medicine purchases from 1 January 2017 to 31 December 2019. To allow comparison between study years, the data was split into three cohorts, one for each year. After exclusion of prescription purchases with incorrect age criteria, missing gender, ATC code not included in the PIM summary table or invalid pharmaceutical form (e.g. topical estrogen), the final data used to assess the prevalence of PIMs in Finland consisted of 497,663 older people and their 11,685,648 medicine purchases.
The population characteristics were presented as mean values with standard deviations. The prevalence of PIM use was calculated based on census data obtained from Statistics Finland (mean population aged 75 years or older in 2017: N = 500,820.5; 2018: N = 506,884.5; and 2019: N = 518,276.0) [31]. The annual prevalence was calculated by dividing the number of older persons with at least one PIM purchase by the average population of each year. The prevalence of PIM use was presented as annual percentages per criteria. The number of PIMs per person was calculated as each individual ATC code regardless of the number of purchases. We also reported the most commonly used PIM classes and their prevalence per criteria during the three-year observation period. In addition, the most commonly used PIMs per criteria were presented. For numerical values, relevant descriptive statistics were presented (mean, standard deviation, median). The statistical analyses were performed using the IBM© SPSS© Statistics software, version 26.
Results
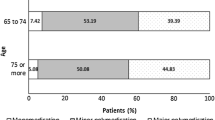
A total of 497,663 older people who had purchased altogether 168 different PIMs were included. The mean age of the population was 82.6 ± 5.7 years, and two thirds (61.8%) were female.
Prevalence of PIM use
We observed an annual prevalence of PIM use of 10.7–57.0% for Finnish older persons according to different criteria (Table 2). According to the Meds75+ database, the annual prevalence of PIM use was 30.4–33.6%. The Beers criteria and STOPP criteria resulted in higher prevalences (annually over 50%) than the other criteria (the third highest prevalence, with EU(7)PIM list, was 39.9% in 2017). Regardless of the applied criteria, the annual prevalence of PIM use decreased during the three-year period, from 14.2–57.0% in 2017 to 10.7–55.3% in 2019.
The number of PIMs per person varied between 1 and 17 according to the different criteria (Table 2). Depending on the applied criteria, proportion of 3.8–45.5% of older people with at least one PIM purchase used two or more PIMs during the observation period. The overlap between the Meds75+ database and eight criteria in detecting PIM users varied from 56.9 to 99.1%. The overlap was greatest between the Meds75+ database and the Swedish criteria, whereas only less than two third of PIM users according to the Beers criteria, STOPP criteria and the Red-Yellow-Green list were also identified by Meds75+ database.
Variation in PIM ratings
The most common medicine classes considered as PIMs were benzodiazepines (N05BA and N05CD), tricyclic antidepressants (N06AA) and drugs for urinary frequency and incontinence (G04BD). Considering individual drug substances, only amitriptyline, clomipramine and diazepam were considered as PIMs in all nine criteria. Most of the criteria identified also hydroxyzine (8/9), levomepromazine (8/9), nitrazepam (8/9), indomethacin (7/9), nortriptyline (7/9) solifenacin (7/9), tolterodine (7/9), and trimipramine (7/9).
Differences in the proportions of PIM users was observed in medicine classes (Table 3) and individual drug substances (see Additional file 2) when used different PIM criteria. For example, when the Beers criteria is applied, proton pump inhibitors (PPIs) were the most commonly used PIM class (46.4% of the total study population n = 497,663 with at least one PIM). When the STOPP criteria was applied the most commonly used PIM classes were loop diuretics (33.5%) and opioids (28.4%). These medicines were considered as PIMs only in one criterion, which led to higher prevalence when that criterion was applied. In case PPIs are not considered, the annual prevalences of PIM use according to the Beers criteria were as follows: 44.1% (2017), 42.7% (2018) and 40.8% (2019). According to STOPP criteria these prevalences were about 10 percentage points lower if loop diuretics and all opioids except codeine were not considered: 36.6% (2017), 35.4% (2018) and 34.0% (2019). Moreover, if these medicines are not considered, the most commonly used PIM class was found to be NSAIDs (30.1%) according to the NORGEP-NH and Red-Yellow-Green list.
Of individual drug substances, the most commonly used PIMs were furosemide, pantoprazole, and codeine. Included nine criteria rated the medicines quite similarly with regard to the most commonly used PIMs (Table 4). Opioids and NSAIDs were among the top three PIMs in most criteria.
Discussion
This is the first study describing and comparing nationwide prevalence of PIM use according to the Finnish Meds75+ database and eight different sets of PIM criteria. Our results indicate that the prevalence varied significantly (10.7–57.0%) between the different criteria among Finnish people aged 75 years or older during the three-year period. The highest prevalence of PIM use was detected with the Beers criteria and the lowest with the Laroche criteria. The annual prevalence detected with the Meds75+ database, one-third, was in the middle of the values obtained by other criteria. Also, the number of medications considered as PIMs and the overlap between the Meds75+ database and eight criteria varied clearly. Depending on the applied criteria, the proportion of people who used more than one PIM over the whole study period varied from 3.8 to 45.5%. However, the annual prevalence of PIMs decreased during the years 2017–2019 regardless of the applied criteria.
We hypothesized that different criteria used to evaluate PIMs provide varying information about their prevalence, and this is supported by our findings. The observation that the Beers and STOPP criteria detect higher PIM prevalence than other included European PIM criteria is consistent with earlier studies comparing more than four criteria [17, 32]. However, findings considering the variance of prevalence are mixed. A study comparing six criteria found a similar high variance, from 24% (NORGEP) to 63% (STOPP), among people aged 65 years or older in Taiwan [32]. On the other hand, a Swedish study detected PIM use by applying five criteria and found a smaller variance from 16.0% (NORGEP) to 24.1% (Beers) [17]. The mixed results might also demonstrate the fact that the criteria are not equally applicable since they are originally intended for use among different age groups. Furthermore, some of the criteria are older than others which may effect on sensitivity in detecting PIMs. These results support the finding from previous study [33] comparing EU(7)PIM and PRISCUS list, which concluded that differences between listed PIMs support regular updating of the PIM criteria.
According to the Meds75+ database, annually one third of Finnish older persons had used PIMs. A similar prevalence was also found in a study applying the Meds75+ database in a smaller population (n = 1000) with the same age limit [34], although that study determined the medications by interviews and included both prescription and OTC medicines. It should also be noted that the Meds75+ database is continuously updated, and the list of PIMs and prescribing practices have changed over time.
We found that annually over half of older persons used PIMs according to the Beers criteria. This prevalence is significantly higher compared to an earlier Finnish population-based register study which found a prevalence of 15% according to the Beers criteria [35]. The study population in that study also included Finnish people aged 65 years or older and the data consisted of only prescription PIMs reimbursed by National Health Insurance, which may explain the difference in prevalence compared to our results.
Our prevalences with the Meds75+ database and NORGEP-NH are consistent with the Norwegian cross-sectional study among home-dwelling people aged 70 years or older, according to the national NORGEP criteria [36]. On the other hand, we report higher prevalence with our national PIM criteria compared to the studies in the Swedish population with their national criteria (17–19%) [17, 37]. However, their prevalence is consistent with ours according to the Swedish criteria. In contrast with Norway and Sweden, we found a lower prevalence of PIM use with both the Meds75+ database and the Red-Yellow-Green list than a study conducted in the Danish population aged 65 years or older [38]. However, the Danish study also found that prevalence of PIM use decreased during the follow-up, which is consistent with our result.
The finding that annual PIM prevalence is decreasing is in concordance with two earlier Finnish studies. First, a register-based study reported that use of reimbursed PIMs decreased from 43 to 18% between 2000 and 2013 [39]. More recently, The Finnish Medicines Agency Fimea, who follows and compiles nationwide statistics about the quality of care of people aged 75 or older, reported that the decline had continued in 2017–2019, but still one fifth of older persons used PIMs, based on the Med75+ database [40]. The lower prevalence in these reports is most likely due to the restriction of PIMs to only prescription purchases reimbursed by National Health Insurance, whereas our data included also non-reimbursed prescription purchases. Moreover, the earlier study included also people aged 65–74 that may explain the higher prevalence at the beginning of the follow-up time compared to ours.
Based on our study, the differences in PIM prevalence are explained by the variances in prevalence of certain medicine classes. We found that more than one fifth of older persons had purchased a PPI, opioid, loop diuretic, NSAID or hypnotic, but the proportion of users of these medicine classes is dependent on the applied criteria. From this perspective, our results suggest that different criteria emphasize different medicine classes in their definition of PIMs. The high prevalences of PIM use detected with the Beers criteria and STOPP criteria is partially explained by the common use of PPIs, furosemide and opioids. If these medicines are not considered, the detected prevalence decreases almost to the same level as the Meds75+ database. Moreover, the Finnish Meds75+ database classifies PPIs and furosemide as suitable for older people and therefore these medicines are considered as a safe therapy option in Finland. Furthermore, the Beers criteria and STOPP criteria consider anxiolytics and antidepressants more comprehensively as PIMs compared to the other seven criteria, which also increases the prevalence according to these two PIM criteria.
Three medicines, amitriptyline, clomipramine and diazepam, were considered as PIMs in all criteria, which is consistent with findings from an earlier study [17]. Furthermore, we found that the nine criteria identify the most-used PIMs quite similarly. This is in contrast with results of an earlier study [32] which found that the top three PIMs varied significantly between the six criteria. However, they analyzed different criteria and had a small sample size (n = 193) which affects comparability. We detected codeine (Meds75+ database, Swedish criteria and NORGEP-NH), etoricoxib (EU(7)PIM list, PRISCUS list and Red-Yellow-Green list), ibuprofen (Beers criteria, NORGEP-NH and Red-Yellow-Green list), nitrofurantoin (Meds75+ database, Laroche criteria and PRISCUS list) and/or tramadol (Meds75+ database, EU(7)PIM list and Swedish criteria) as the most-used PIMs in three different criteria. This might be explained by the relation between the nine criteria, since the authors and experts developing and updating national criteria generally use PIM criteria from other countries.
Strengths and limitations
The present study has several strengths. Unlike earlier studies comparing PIM criteria, this study compiled all PIMs at population level regardless of, for example, comorbidities, and used nine different criteria, including the Finnish Meds75+ database. In addition, this is the first study comparing the content of the Meds75+ database to eight criteria in identifying PIMs. Furthermore, the very high coverage of the national prescription register makes it possible to obtain generalizable findings.
On the other hand, certain limitations should be noted. First, seven medicines were misinterpreted (i.e. interpreted as PIM only in certain clinical conditions or questionable PIM) from the EU(7)-PIM list and were not included in the data collection (see Additional file 1). Consequently, the actual prevalence of PIM use according the EU(7)-PIM list was underestimated. However, the effect of misinterpretation on the prevalence can be expected to be small based on the Finnish Statistics on Medicines published by the Finnish Medicines Agency Fimea and the SII [41].
Second, since different criteria rate PIMs at different levels, our comparison of nine criteria is limited. For example, medicines with anticholinergic burden have not been internationally defined but the Laroche criteria includes a statement to avoid concomitant use of anticholinergic drugs without specific drug substance. Although the Beers criteria, the Meds75+ database and the Swedish criteria consider individual drug substances with anticholinergic properties as PIMs, the Laroche statement was not considered for these drugs listed in other included criteria. The lower prevalence of PIM use detected with the Laroche criteria may be explained with the excluded anticholinergics.
Third, information on purchases rather than actual intake of medicines is a limitation. However, analysis of actual intake at nationwide scale is hardly possible. Furthermore, we could not take OTC medicines into account as the Prescription Centre does not register their use. As some PIMs are available also without prescription in Finland (e.g., acetylsalicylic acid), their actual use may be greater than we have observed. On long-term use, having a prescription makes the use cheaper so the significance of missing data about short-term OTCs is probably relatively limited.
Forth, we did not take into account those cases where PIM status of a medicine is limited to certain doses, indications, types of pharmaceutical form or duration of treatment. Although the Prescription Centre includes detailed information about deliveries (incl. For example the package size), dosage instructions are not recorded in such systematic way that would allow consideration of dosages or indications and collecting such information manually from the extensive data would have been unnecessarily challenging. For these reasons, the prevalence of PIM use may be undersized with the criteria where PIM status depends on these type of details related to the treatment: NORGEP-NH, STOPP, Red-Yellow-Green list, EU(7)PIM list and Laroche criteria.
Fifth, although the included criteria are intended for use in older persons, the age limit for this age group varies. Different age limits may affect which medications are considered as PIMs and thereby partly explain the variation in the observed prevalences. As the medicines that are considered as PIMs for older persons aged 65 or over should - quite obviously – be avoided in persons aged 75 years or over as well, all included criteria can be applied to our study population.
Conclusion
Our findings indicate that PIM use is common among older people in Finland according to the national Meds75+ database, but the prevalence varies significantly between the applied nine criteria. Furthermore, this study underlines the focus of the different criteria that clinicians should consider when applying PIM criteria in daily practice. Although we found that the nine criteria detect the most-used individual PIMs quite similarly, the differences in the prevalence of medicine classes explain the variation in overall prevalence. Differences in defining PIMs between criteria must be considered when studying use of medications in different areas and health care settings. Future research should focus on evaluating how medicine use is affected by the different criteria over time.
Availability of data and materials
The data that support the findings of this study are available from The Social Insurance Institution of Finland but restrictions apply to the availability of these data, which were used under license for this study, and so are not publicly available. Data are available from The Social Insurance Institution of Finland with the permission of The Finnish Social and Health Data Permit Authority Findata.
Abbreviations
- ADE:
-
Adverse drug event
- PIM:
-
Potentially inappropriate medication
- STOPP/START:
-
Screening Tool of Older Persons’ Potentially Inappropriate Prescriptions and Screening Tool to Alert to Right Treatment
- OTC:
-
Over-the-counter
- PRISCUS:
-
Latin for “old and venerable”
- Swedish criteria:
-
Swedish quality indicators for evaluation of older patients’ drug therapies
- NORGEP:
-
Norwegian General Practice
- NH:
-
Nursing home
- ATC:
-
Anatomical Therapeutic Chemical
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- SII:
-
Social Insurance Institution of Finland
- PPIs:
-
Proton pump inhibitors
- N05BA and N05CD:
-
World Health Organization’s Anatomical Therapeutic Chemical classification system for benzodiazepines
- N06AA:
-
World Health Organization’s Anatomical Therapeutic Chemical classification system for tricyclic antidepressants
- G04BD:
-
World Health Organization’s Anatomical Therapeutic Chemical classification system for drugs for urinary frequency and incontinence
References
O’Connor MN, Gallagher P, O’Mahony D. Inappropriate prescribing: criteria, detection and prevention. Drugs Aging. 2012. https://doi.org/10.2165/11632610-000000000-00000.
Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA division of geriatric medicine. Arch Intern Med. 1991;151(9):1825–32.
Hedna K, Hakkarainen KM, Gyllensten H, Jönsson AK, Petzold M, Hägg S. Potentially inappropriate prescribing and adverse drug reactions in the elderly: a population-based study. Eur J Clin Pharmacol. 2015. https://doi.org/10.1007/s00228-015-1950-8.
Marinovic I, Vrca VB, Samardzic I, Marusic S, Grgurevic I. Potentially inappropriate medications involved in drug-drug interactions at hospital discharge in Croatia. Int J Clin Pharm. 2021. https://doi.org/10.1007/s11096-020-01164-4.
Price SD, Holman CD, Sanfilippo FM, Emery JD. Association between potentially inappropriate medications from the Beers criteria and the risk of unplanned hospitalization in elderly patients. Ann Pharmacother. 2014. https://doi.org/10.1177/1060028013504904.
Sköldunger A, Fastbom J, Wimo A, Fratiglioni L, Johnell K. Impact of inappropriate drug use on hospitalizations, mortality, and costs in older persons and persons with dementia: findings from the SNAC study. Drugs Aging. 2015. https://doi.org/10.1007/s40266-015-0287-4.
Tommelein E, Mehuys E, Petrovic M, Somers A, Colin P, Boussery K. Potentially inappropriate prescribing in community-dwelling older people across Europe: a systematic literature review. Eur J Clin Pharmacol. 2015. https://doi.org/10.1007/s00228-015-1954-4.
Laroche ML, Charmes JP, Merle L. Potentially inappropriate medications in the elderly: a French consensus panel list. Eur J Clin Pharmacol. 2007. https://doi.org/10.1007/s00228-007-0324-2.
Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (screening tool of older Person's prescriptions) and START (screening tool to alert doctors to right treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008;46(2):72–83.
Rognstad S, Brekke M, Fetveit A, Spigset O, Wyller TB, Straand J. The Norwegian general practice (NORGEP) criteria for assessing potentially inappropriate prescriptions to elderly patients. A modified Delphi study. Scand J Prim Health Care. 2009. https://doi.org/10.1080/02813430902992215.
Danish Institute for Rational Pharmacotherapy. Rød-gul-grøn listen (red-yellow-green list). 2011.
The Swedish National Board of Health and Welfare (Socialstyrelsen). Indikatorer för god läkemedelsterapi hos äldre. 2017. https://www.socialstyrelsen.se/publikationer2017/2017-6-7 Accessed 5 Nov 2018.
Finnish Medicines Agency. Meds75+. 2021. https://www.fimea.fi/web/en/databases_and_registeries/medicines_information/database_of_medication_for_older_persons Accessed 14 Sep 2021.
Ubeda A, Ferrándiz L, Maicas N, Gomez C, Bonet M, Peris JE. Potentially inappropriate prescribing in institutionalised older patients in Spain: the STOPP-START criteria compared with the Beers criteria. Pharm Pract (Granada). 2012;10(2):83–91.
Li H, Pu S, Liu Q, Huang X, Kuang J, Chen L, et al. Potentially inappropriate medications in Chinese older adults: the beers criteria compared with the screening tool of older persons' prescriptions criteria. Geriatr Gerontol Int. 2017. https://doi.org/10.1111/ggi.12999.
Blanco-Reina E, Valdellós J, Aguilar-Cano L, García-Merino MR, Ocaña-Riola R, Ariza-Zafra G, et al. Beers criteria and STOPP v2 for detecting potentially inappropriate medication in community-dwelling older people: prevalence, profile, and risk factors. Eur J Clin Pharmacol. 2015;2019. https://doi.org/10.1007/s00228-019-02722-0.
Morin L, Fastbom J, Laroche ML, Johnell K. Potentially inappropriate drug use in older people: a nationwide comparison of different explicit criteria for population-based estimates. Br J Clin Pharmacol. 2015. https://doi.org/10.1111/bcp.12615.
Saastamoinen L, Verho J. Regional variation in potentially inappropriate medicine use in older adults. - a national register-based cross-sectional study on economic, health system-related and patient-related characteristics. Res Social Adm Pharm. 2021. https://doi.org/10.1016/j.sapharm.2020.08.018.
Dimitrow MS, Airaksinen MS, Kivelä SL, Lyles A, Leikola SN. Comparison of prescribing criteria to evaluate the appropriateness of drug treatment in individuals aged 65 and older: a systematic review. J Am Geriatr Soc. 2011. https://doi.org/10.1111/j.1532-5415.2011.03497.x.
Kaufmann C, Tremp R, Hersberger K, Lampert M. Inappropriate prescribing: a systematic overview of published assessment tools. Eur J Clin Pharmacol. 2014. https://doi.org/10.1007/s00228-013-1575-8.
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey G. Tools for assessment of the appropriateness of prescribing and association with patient-related outcomes: a systematic review. Drugs Aging. 2018. https://doi.org/10.1007/s40266-018-0516-8.
Holt S, Schmield S, Thürmann PA. Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arztebl Int. 2010;107(31–32):543–51.
Renom-Guiteras A, Meyer G, Thürmann PA. The EU(7)-PIM list: a list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur J Clin Pharmacol. 2015. https://doi.org/10.1007/s00228-015-1860-9.
American Geriatrics Society. American Geriatrics Society 2019 Updated AGS Beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019. https://doi.org/10.1111/jgs.15767.
Nyborg G, Straand J, Klovning A, Brekke M. The Norwegian general practice – nursing home criteria (NORGEP-NH) for potentially inappropriate medication use: a web-based Delphi study. Scand J Prim Health Care. 2015. https://doi.org/10.3109/02813432.2015.1041833.
Jensen LD, Andersen O, Hallin M, Petersen J. Potentially inappropriate medications related to weakness in older acute medical patients. Int J Clin Pharm. 2014. https://doi.org/10.1007/s11096-014-9940-y.
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015. https://doi.org/10.1093/ageing/afu145.
World Health Organization. ATC/DDD Index. 2020. https://www.whocc.no/atc_ddd_index/ Accessed 2 Jul 2020.
Furu K, Wettermark B, Andersen M, Martikainen JE, Almarsdottir AB, Sørensen HT. The Nordic countries as a cohort for Pharmacoepidemiological research. Basic Clin Pharmacol Toxicol. 2010. https://doi.org/10.1111/j.1742-7843.2009.00494.x.
The Social Insurance Institution of Finland. Prescriptions. 2020. https://www.kanta.fi/en/web/guest/professionals/prescription Accessed 14 Dec 2020.
Official Statistics of Finland. Population structure [e-publication]. ISSN=1797–5395. Helsinki: Statistics Finland; 2021. http://www.stat.fi/til/vaerak/index_en.html Accessed 13 Oct 2021
Chang CB, Chen JH, Wen CJ, Kuo HK, Lu IS, Chiu LS, et al. Potentially inappropriate medications in geriatric outpatients with polypharmacy: application of six sets of published explicit criteria. Br J Clin Pharmacol. 2011. https://doi.org/10.1111/j.1365-2125.2011.04010.x.
Krulichová IS, Selke GW, Thürmann PA. Trends and patterns in EU(7)-PIM prescribing to elderly patients in Germany. Eur J Clin Pharmacol. 2021. https://doi.org/10.1007/s00228-021-03148-3.
Bell JS, Ahonen J, Lavikainen P, Hartikainen S. Potentially inappropriate drug use among older persons in Finland: application of a new national categorization. Eur J Clin Pharmacol. 2013. https://doi.org/10.1007/s00228-012-1372-9.
Leikola S, Dimitrow M, Lyles A, Pitkälä K, Airaksinen M. Potentially inappropriate medication use among Finnish non-institutionalized people aged ≥65 years: a register-based, cross-sectional, national study. Drugs Aging. 2011. https://doi.org/10.2165/11586890-000000000-00000.
Nyborg G, Straand J, Brekke M. Inappropriate prescribing for the elderly--a modern epidemic? Eur J Clin Pharmacol. 2012. https://doi.org/10.1007/s00228-012-1223-8.
Johnell K, Fastbom J, Rosen M, Leimanis A. Inappropriate drug use in the elderly: a nationwide register-based study. Ann Pharmacother. 2007. https://doi.org/10.1345/aph.1K154.
Kristensen RU, Jensen-Dahm C, Gasse C, Waldemar G. Declining use of potentially inappropriate medication in people with dementia from 2000 to 2015: a repeated cross-sectional Nationwide register-based study. J Alzheimers Dis. 2021;79(4):1459–70.
Vartiainen AK, Hyttinen V, Jyrkkä J, Saastamoinen L, Valtonen H. Iäkkäät käyttävät vältettäviä lääkkeitä yleisesti. Suom Lääkäril. 2017;49:2899–906.
Jauhonen HM, Jyrkkä J. Monilääkitys ja lääkekustannukset kasvussa iäkkäillä. In: SIC! Drug Information from Fimea; 2020. https://sic.fimea.fi/arkisto/2020/3_2020/palstat-/monilaakitys-ja-laakekustannukset-kasvussa-iakkailla Accessed 2 Oct 2020.
The Social Insurance Institution of Finland, the Finnish Medicines Agency. Finnish Statistics on Medicines 2021. https://www.kela.fi/web/en/statistical-publications_finnish-statistics-on-medicines. Accessed 31 Aug 2021.
Acknowledgements
Not applicable.
Dual publication
A Policy Brief (abstract) considering this research was published as part of academic meeting of Finnish Research Network for Rational Pharmacotherapy 17 February 2022. The Policy Brief (word count 331) available (in Finnish only): https://www.fimea.fi/kehittaminen/tutkimus/rationaalisen-laakehoidon-tutkimusverkosto/policy-brief
Code availability
Not applicable.
Funding
This study was financially partly supported by the Competitive State Research Financing of the Expert Responsibility area of Tampere University Hospital (projects 96068 and 9AB016).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Johanna Jyrkkä was responsible of acquisition of data. Material preparation and data analysis were performed by Jasmin Paulamäki. The first draft of the manuscript was written by Jasmin Paulamäki, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
According to the Finnish legislation, retrospective register-based studies in which the subjects are not in contact / are not subject to intervention are not considered medical research (Medical Research Act 488/1999) and therefore ethical committee approval is not required. Informed consent was waived because the study utilized register data that can be used in scientific research. According to national legislation (including European Union General Data Protection Regulation 679/2016; Data Protection Act 1050/2018; Act on Electronic Prescriptions 61/2007; Act on the Secondary Use of Health and Social Data 552/2019) retrospectively collected health register data can be used for research with permission from the register owner. This institutional approval was obtained from the register owner Social Insurance Institution of Finland (Kela) (Dnro 96/522/2020) and no other administrative permission were required. All data obtained from the national prescription register was pseudonymized before submission to the authors, and the authors cannot convert the data back into identifiable form. This study was performed in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
Author Paulamäki, Author Jyrkkä and Author Hyttinen declare that they have no conflict of interest. Author Jämsen has received lecture fees (from lectures partly related to the present study) from medical companies (Chiesi, Lundbeck, Novartis, Nutricia, Orion Pharma) and professional organizations (Finnish Medical Society Duodecim, Pihlajalinna Ltd., Finnish Medical Association, Fioca Ltd). Authors Paulamäki, Jyrkkä and Jämsen are also members of the advisory board of the Meds75+ database.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Complete summary of PIMs, ignored statements and PIMs not available on the Finnish market.
Additional file 2.
Proportion of users of the most common medicine classes/substances among people using PIMs (total = 497,663).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Paulamäki, J., Jyrkkä, J., Hyttinen, V. et al. Prevalence of potentially inappropriate medication use in older population: comparison of the Finnish Meds75+ database with eight published criteria. BMC Geriatr 23, 139 (2023). https://doi.org/10.1186/s12877-022-03706-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03706-z