Abstract
Background
To synthesise the evidence for the effectiveness of inpatient rehabilitation treatment ingredients (versus any comparison) on functioning, quality of life, length of stay, discharge destination, and mortality among older adults with an unplanned hospital admission.
Methods
A systematic search of Cochrane Library, MEDLINE, Embase, PsychInfo, PEDro, BASE, and OpenGrey for published and unpublished systematic reviews of inpatient rehabilitation interventions for older adults following an unplanned admission to hospital from database inception to December 2020. Duplicate screening for eligibility, quality assessment, and data extraction including extraction of treatment components and their respective ingredients employing the Treatment Theory framework. Random effects meta-analyses were completed overall and by treatment ingredient. Statistical heterogeneity was assessed with the inconsistency-value (I2).
Results
Systematic reviews (n = 12) of moderate to low quality, including 44 non-overlapping relevant RCTs were included. When incorporated in a rehabilitation intervention, there was a large effect of endurance exercise, early intervention and shaping knowledge on walking endurance after the inpatient stay versus comparison. Early intervention, repeated practice activities, goals and planning, increased medical care and/or discharge planning increased the likelihood of discharge home versus comparison. The evidence for activities of daily living (ADL) was conflicting. Rehabilitation interventions were not effective for functional mobility, strength, or quality of life, or reduce length of stay or mortality. Therefore, we did not explore the potential role of treatment ingredients for these outcomes.
Conclusion
Benefits observed were often for subgroups of the older adult population e.g., endurance exercise was effective for endurance in older adults with chronic obstructive pulmonary disease, and early intervention was effective for endurance for those with hip fracture. Future research should determine whether the effectiveness of these treatment ingredients observed in subgroups, are generalisable to older adults more broadly. There is a need for more transparent reporting of intervention components and ingredients according to established frameworks to enable future synthesis and/or replication.
Trial registration
PROSPERO Registration CRD42018114323.
Similar content being viewed by others
Introduction
The world’s population is ageing, reflecting advances in economic and social development, public health, sanitation, and medicine [1]. Although people are living longer, multiple chronic and complex health issues increase with age [2]. This demographic trend, the changing health patterns of multimorbidity in old age contribute to fluctuating health service use and associated increased costs [3, 4]. A consequent increase in unplanned hospital admissions for older adults has the potential to lead to hospital associated deconditioning [5], with slower and poorer recovery without appropriate rehabilitation [6].
Rehabilitation is defined as a “set of measures aimed at individuals who have experienced or are likely to experience disability to assist them in achieving and maintaining optimal functioning (all body functions, activities and participation [7]) when interacting with their environments.” [8]. Treatment theory “refers to a class of specific theories that specify mechanisms by which ingredients of a treatment produce change in the treatment target, the aspect of function that is directly impacted by the treatment” [9,10,11,12]. Treatment theory conceptualises rehabilitation as a complex intervention made up of treatment components which address different targets; each treatment component e.g., skills and habits, is made up of more specific and measurable treatment ingredients, e.g., strength exercises or repeated practice activities (Fig. 1) [9,10,11,12]. Healthcare policies are shifting care away from the inpatient setting and into the community – either home or facility [13]. Inpatient rehabilitation may reduce the impact and complications of various health conditions and facilitate the earlier restoration of function, maximising potential for discharge home (and not to a facility) [14]. It is therefore essential to maximise the potential benefits from rehabilitation offered in this setting.
Rehabilitation as a complex intervention made up of treatment components addressing different targets; each treatment component is made up of more specific and measurable treatment ingredients [12]. ICF: International Classification of Functioning
There is a plethora of studies evidencing the effectiveness of inpatient rehabilitation for older adults admitted to hospital with an unplanned episode of injury or illness, summarised in systematic reviews and meta-analyses [15,16,17]. This rehabilitation often includes multiple treatment ingredients with uncertainty over which ingredient(s) account for the reported change in outcome [12]. This poses a challenge for clinicians when justifying the inclusion of a given ingredient in practice, and for researchers when determining which ingredient(s) to include in future studies of rehabilitation interventions [18].
It would be of value to both clinicians and researchers to determine which treatment ingredient(s) contribute to the effectiveness of rehabilitation [19]. We proposed to address this evidence gap through application of Treatment Theory in an overview review of rehabilitation treatment ingredients for older adults with unplanned hospital admission.
Aims and objectives
The aims of this overview review were to inform evidence-based inpatient rehabilitation for older adults following an unplanned hospital admission, and to identify gaps in the evidence to inform future research. More specifically, the primary objective was to synthesise the evidence for the effectiveness of inpatient rehabilitation treatment ingredients (versus any comparison) on functioning (body functions, activities) among older adults with an unplanned hospital admission. Secondary objectives included synthesizing the evidence for additional outcomes of quality of life, length of stay, discharge destination, and mortality.
Methods
We registered the protocol on the international prospective register of systematic reviews (PROSPERO: CRD42018114323). We reported this review in adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [20]. We did not require ethical approval as it used data from published systematic reviews and meta-analyses.
Eligibility criteria
Eligibility criteria are outlined in Table 1. Briefly, we included systematic reviews and meta-analyses of randomised controlled trials (RCTs) which compared the effectiveness of inpatient rehabilitation [21] to any comparator group on functioning (body functions, activities), quality of life, discharge destination, length of stay, and/or mortality after inpatient rehabilitation (and where available longest follow-up to one-year) among older adults with an unplanned hospital admission (Table 1). We applied no publication date, language, or geographical limits. We excluded reviews focusing exclusively on older adults post-stroke to avoid conclusions being dominated by the larger evidence base post-stroke.
Search methods
We developed structured search strategies, in consultation with a librarian using thesaurus terms for intervention, setting and study design for each database (e.g., EMTREE for EMBASE, MeSH for MEDLINE) and free text, targeting the “title” and “abstract” fields (Supplementary File 1). We searched from inception to December 10th 2020 for published and unpublished systematic reviews in the following electronic databases: Cochrane Library, MEDLINE, Embase, PsychInfo, PEDro, BASE, and OpenGrey. We also screened reference lists of eligible systematic reviews for additional reviews not identified through our search strategies. We exported references to Covidence for deduplication, screening, selection, and quality appraisal [22].
Screening and selection
We screened titles and abstracts and potentially eligible full text reviews in duplicate against eligibility criteria (KL, CK, SG, KS). A third researcher resolved any discrepancies. We quantified inter-rater reliability using Cohen’s Kappa statistic [23]. We avoided double-counting outcome data in our overview by primary RCT overlap with the creation of a citation matrix ordered first by publication date and then by lead author surname and excluded eligible reviews with no unique RCTs (retaining the most recent reviews) [24].
Quality appraisal
We assessed the methodological quality of each included review in duplicate using the Assessment of Multiple Systematic Reviews (AMSTAR 2) tool (KL, SH, SG, KS) [25]. AMSTAR 2 is a 16-item checklist which informs an overall qualitative rating on the confidence in the results of a review, based on weaknesses in critical domains [25]. Such domains include whether a protocol was registered, adequacy of literature search, exclusion criteria, and risk of bias. Four options were available when rating, ranging from critically low confidence to high confidence. A third researcher resolved any discrepancies.
Data extraction
We extracted data onto Microsoft Excel table templates defined a priori in duplicate (KL, EE, CK, SG, KS). A third researcher resolved any discrepancies. We contacted authors to supplement missing or incomplete data.
We extracted the following data items for the systematic reviews: review author, review year, population, intervention, comparators, outcome, number of studies eligible for the current overview, number of patients from eligibility studies. We extracted the following data items for eligible RCTs within the systematic reviews: RCT author, RCT year, country, sample size (intervention and comparator), characteristics of the population where available -age, gender, target group, and preadmission residence, comparison/s, interventions, outcomes and follow-up relevant to the current overview. For the interventions, we extracted three main treatment components and their more specific and measurable treatment ingredients specified by Treatment Theory [9,10,11,12]. Component 1: Organ Functions (example more specific treatment ingredient: strengthening exercise) [12]; Component 2: Skills and Habits (example more specific treatment ingredient: repeated practice of activities +/− increasing demands) [12]; and Component 3: Changing Behaviour (example more specific treatment ingredients: goals and planning, shaping knowledge) [26]. Where treatment ingredients did not fall under these three treatment components (e.g., increased medical care), we extracted them under Other Components. All treatment ingredients cited were assigned to a component in this review. For our outcomes, we extracted mean and standard deviation in each treatment arm for continuous outcome measures and proportions for categorical outcomes after inpatient rehabilitation and on longest follow-up (up to 1 year). We contacted all authors who presented data as medians, ranges, or 95% confidence intervals for means and standard deviations. If no response was received, we converted data presented as medians and ranges to means and standard deviations using methods as described by Hozo et al. [27]. We converted data presented as 95% confidence intervals to standard errors [28] and subsequently standard deviations (standard deviation = standard error x √sample size).
Data synthesis
All systematic reviews met the eligibility criteria for inclusion; however, 1) not all RCTs within reviews were relevant, and 2) there was considerable primary RCT overlap between reviews. Therefore, we re-analysed the data by performing random-effects meta-analyses within the subgroup of relevant RCTs for each outcome across the systematic reviews [29]. We estimated Hedges’ g or mean differences for continuous outcomes and log odds ratios for categorical outcomes. We interpreted effect sizes of 0.2 as small, 0.5 moderate, and 0.8 as large [28]. We completed sensitivity analyses with RCTs from reviews of low or critically low quality removed from the analyses.
We stratified meta-analyses which indicated the effectiveness of interventions on outcomes by individual treatment ingredients, e.g. endurance exercise [21]. For meta-analyses with at least ten RCTs, small study sample bias was assessed using Egger’s test for continuous outcomes and Peters test for categorical outcomes [28]. We assessed the potential for heterogeneity using I2 and followed the Cochrane convention of 0–40% heterogeneity as may not be important, 30–60% as moderate, 50–90% as substantial, and 75–100% as considerable heterogeneity [28]. Where at least ten RCTs were included in the meta-analysis, we also explored the potential for heterogeneity due to differences in characteristics of the RCTs (mean age, target group, continent of publication, and year of publication) with random-effects meta-regression [28] and stratified meta-analysis where there was a plausible characteristic which may explain the heterogeneity e.g., RCT geography on length of stay due to different organisation of care. All analyses were completed in Stata v16 [30]. We summarised RCT findings descriptively where meta-analysis was not possible.
Results
Selection
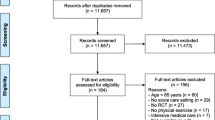
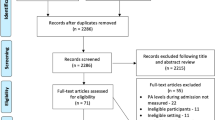
We included 12 systematic reviews in this overview review. Initial searches identified 2677 systematic reviews, of which 583 were duplicates. On the title and abstract screening, a further 1916 were excluded. Of the 178 reviews assessed at full text screening, 155 were ineligible for the following reasons: population (n = 104), intervention (n = 9), outcome (n = 5), study design (n = 17), setting (n = 21). Cohen’s Kappa statistic following full text review was 0.73 indicating substantial agreement between assessors. Following generation of a citation matrix ordered by publication date, we excluded a further 10 reviews [16, 31,32,33,34,35,36,37,38,39] which contained no RCTs not already included in a more recent review (Supplementary File 2) Fig. 2.
Quality
The results of the quality assessment are presented in Table 2. Overall, seven systematic reviews were assigned a moderate rating for overall confidence in review results (more than one non-critical weakness but no critical flaws) [15, 40, 42, 45, 47,48,49], four a low rating (one critical flaw – study selection not in duplication or failure to consider risk of bias for interpretation) [17, 41, 43, 46], and one a critically low rating (more than one critical flaw) [44]. Almost all included systematic reviews met the requirements for defining an appropriate research question (n = 12) [15, 17, 40,41,42,43,44,45,46,47,48,49], search strategy (n = 11) [15, 17, 40,41,42,43, 45,46,47,48,49], study selection (n = 11) [15, 17, 40,41,42,43,44,45, 47,48,49], risk of bias assessment (n = 11) [15, 17, 40,41,42,43, 45,46,47,48,49], explanation of heterogeneity in analyses (n = 9) [15, 17, 40,41,42, 45, 46, 48, 49], and declaring sources of conflicts of interest (n = 12) [15, 17, 40,41,42,43,44,45,46,47,48,49]. Most systematic reviews failed to explain their selection of the study designs for inclusion (n = 11) [15, 17, 40,41,42, 44,45,46,47,48,49], declare sources of funding for studies included in the review (n = 11) [15, 40,41,42,43,44,45,46,47,48,49] and/or carry out an adequate investigation of potential publication bias (n = 5) [40, 42, 43, 46, 47].
Characteristics
The 12 systematic reviews included 41 unique RCTs and 10,444 older adults with an unplanned hospital admission relevant to this overview (mean (min - max) sample size per RCT: 261 (12–1531)) (Table 3). The target population of systematic reviews included older adults admitted for a general medical reason (n = 5) [15, 17, 43, 45, 48], for any unplanned reason (n = 3) [41, 46, 49], with hip fracture (n = 2) [40, 47], orthopaedic trauma (n = 1) [44], or an exacerbation of chronic obstructive pulmonary disease (COPD) (n = 1) [42]. Outcomes captured by the systematic reviews included functional mobility, ADLs, walking endurance, walking speed, and/or lower limb strength (n = 11) [15, 17, 40,41,42,43,44,45,46, 48, 49]; quality of life (n = 4) [40, 42, 48, 49]; length of stay (n = 9) [15, 17, 40,41,42, 45,46,47,48]; discharge destination (n = 2) [41, 47]; and mortality (n = 7) [15, 17, 40, 41, 43, 48, 49].
Characteristics (as well as their treatment components and more specific and measurable ingredients) of the 44 RCTs included in the 12 systematic reviews are detailed in Supplementary Files 3 and 4. Examples of each treatment ingredient are specified in Table 4. For component 1 Organ Functions, treatment ingredients included: endurance exercise (n = 13), strengthening (n = 12), energy applied to soft tissue (n = 7), and/or breathing related exercises/training (n = 6). For component 2 Skills and Habits, treatment ingredients included: repeated practice activities (n = 15), functions (n = 8), and/or ‘exercise rehabilitation’ (n = 6). For component 3 Changing Behaviour, treatment ingredients included: shaping knowledge (n = 16), feedback and monitoring (n = 14), goals and planning (n = 11), antecedents (n = 12), natural consequences (n = 5), social support (n = 2), and/or comparison of behaviour (n = 1). For Other Components, treatment ingredients included: increased medical care for e.g., avoidance of complications and/or pain management (n = 14), early intervention (n = 12), team meetings and care planning (n = 11), discharge planning (n = 9), nutritional intervention (n = 8), home visits during inpatient stay (n = 5), and/or cognitive orientation exercise (n = 2).
The comparator was usual care for the majority of RCTs (n = 42, 95.5%) identified from the systematic reviews. Physiotherapy/occupational therapy was a core component of usual care for 21 RCTs (50.0%), provided following a physician referral for 5 RCTs (11.9%), not a component of usual care for 13 RCTs (30.9%), or not specified for 1 RCT (2.4%). Two RCTs (4.8%) included education and usual care (1 RCT with physiotherapy/occupational therapy, 1 RCT usual care not specified) as the comparator. The comparator was an alternative intervention - delayed ambulation or delayed weight bearing for 2 RCTs (4.6%).
Synthesis
Meta-analyses were completed for function (functional mobility, ADL, walking speed, walking endurance, lower limb strength), health-related quality of life, length of stay, discharge destination, and mortality (Table 5). Details for population, intervention treatment ingredients, comparator, outcome measurement, and follow-up for each RCT included in each meta-analysis are available alongside forest plots in Supplementary File 5. We noted no difference in effect estimates or confidence intervals for sensitivity analyses which excluded RCTs from reviews of low or critically low quality. If interventions favored the control group, this is specified in text alongside the results of meta-analyses. Forest plots for meta-analyses by treatment ingredient are available in Supplementary File 6. Meta-regression was used to explore heterogeneity in analyses for ADL, discharge home and length of stay. Outcomes which could not be included in meta-analyses due to absence of measure of central tendency or dispersion, sole study, and/or multiple measures for the same outcome are summarised in text and in Supplementary File 7.
Function
Walking endurance
Rehabilitation had a large effect on walking endurance versus comparison after inpatient stay (Total score: 6 RCTs including 307 participants; Hedges’ g = 1.50, 95% CI: 0.39, 2.60. I2 = 94.40; Change score: 3 RCTs including 139 participants; Log OR = 1.23, 95% CI: 0.68, 1.78. I2 = 54.96) supported by results of RCTs from one systematic review not included in the meta-analysis [42]. When included in a rehabilitation intervention, the treatment ingredients endurance exercise (Total score: 3 RCTs including 181 participants; Hedges’ g = 2.44, 95% CI: 0.49, 4.38. I2 = 95.56; Change score: 2 RCTs including 110 participants; Log OR = 0.98, 95% CI: 0.59, 1.37. I2 = 0.00) and shaping knowledge (2 RCTs including 152 participants; Hedges’ g = 1.51, 95% CI: 0.56, 2.46. I2 = 83.24) had a large effect, while early intervention had a moderate effect (2 RCTs including 100 participants; Hedges’ g = 0.51, 95% CI: 0.12, 0.91. I2 = 0.00) on walking endurance versus comparison after inpatient stay.
Walking speed
Rehabilitation had a small effect on walking speed versus comparison after inpatient stay (5 RCTs including 1175 participants; Hedges’ g = 0.17, 95% CI: 0.05, 0.28. I2 = 0.00). One systematic review reported on one RCT which noted no effect at follow-up [40]. When included in a rehabilitation intervention, the treatment ingredients strengthening exercise or repeated exercise rehabilitation did not increase walking speed.
Activities of daily living
Rehabilitation had a small effect on ADL versus comparison after inpatient stay (15 RCTs including 3929 participants; Hedges’ g = 0.21, 95% CI: 0.00, 0.42. I2 = 86.58). The effect was similar but non-significant for ADL change score (6 RCTs including 2779 participants; Log OR = 0.21, 95% CI: − 0.07, 0.49. I2 = 71.46). The effect was not sustained at 1–12 month follow-up (Total score: 5 RCTs including 895 participants; Hedges’ g = 0.04, 95% CI: − 0.31, 0.38. I2 = 82.69, 1 RCT favoured comparison; Change score: 2 RCTs including 973 participants; Log OR = 0.45, 95% CI: − 0.05, 0.96. I2 = 52.36). The absence of an effect was supported by results of RCTs from six systematic reviews not included in the meta-analyses [41,42,43, 45, 48, 49]. There was evidence of small study sample bias for the analysis of total ADL after inpatient rehabilitation (p = 0.01). For estimates of total ADL after inpatient stay, the total effect of rehabilitation interventions adjusted for age, target population, RCT geography, and publication year was not significant (p = 0.12) in meta-regression.
When included in a rehabilitation intervention, the treatment ingredient energy applied to soft tissue had a large effect versus comparison after inpatient stay (3 RCTs including 114 participants; Hedges’ g = 0.95, 95% CI: 0.23, 1.66. I2 = 70.20). There was no effect of endurance exercise, strengthening exercise, repeated practice activities, repeated exercise rehabilitation, goals and planning, feedback and monitoring, shaping knowledge, antecedents, increased medical care, nutritional intervention, or early intervention, on ADL versus comparison.
Other measures of function
Rehabilitation did not improve functional mobility or lower limb strength versus comparison after inpatient stay or functional mobility at follow-up evidenced by meta-analysis. Two systematic reviews identified RCTs reporting a between group difference in functional mobility when measured with the Physical Performance and Mobility Examination after inpatient rehabilitation [48] or the Short Physical Performance Battery at follow-up [41].
Discharge destination
Rehabilitation was effective at increasing the odds of living at home versus comparison after inpatient rehabilitation (11 RCTs including 3751 participants; Log OR = 0.47, 95% CI: 0.17, 0.76. I2 = 45.95) and at 3–12-month follow-up (2 RCTs including 676 participants; Log OR = 0.38, 95% CI: 0.03, 0.74. I2 = 0.00). When included in a rehabilitation intervention, the treatment ingredients repeated practice activities (6 RCTs including 2783 participants; Log OR = 0.49, 95% CI: 0.11, 0.87. I2 = 60.41), goals and planning (2 RCTs including 80 participants; Log OR = 0.83, 95% CI: 0.21, 1.45. I2 = 16.44), increased medical care (8 RCTs including 3451 participants; Log OR = 0.38, 95% CI: 0.04, 0.73. I2 = 53.78) early intervention (7 RCTs including 1279 participants; Log OR = 0.60, 95% CI: 0.20, 1.00. I2 = 27.45), and discharge planning (6 RCTs including 3236 participants; Log OR = 0.46, 95% CI: 0.09, 0.84. I2 = 62.41) increased the odds of living at home versus comparison after inpatient rehabilitation. When included in a rehabilitation intervention, the rehabilitation ingredients repeated exercise rehabilitation, antecedents, team meetings and care planning, and nutritional intervention had no effect on the odds of living at home after the period of inpatient rehabilitation. There was no evidence of small study sample bias. For total estimates after inpatient stay, the total effect of age, target population, RCT geography, and publication year was not significant (p = 0.14) in meta-regression suggesting these variables do not explain the observed heterogeneity. Subsequent meta-analysis was not carried out.
Quality of life
Rehabilitation did not increase health-related quality of life versus comparison after inpatient stay (Total score: 5 RCTs including 1583 participants; Hedges’ g = − 0.15, 95% CI: − 0.37, 0.07. I2 = 60.47; Change score: 2 RCTs including 78 participants; Log OR = − 0.40, 95% CI: − 0.84, 0.04. I2 = 0.00), or on 12-month follow-up (2 RCTs including 1150 participants; Hedges’ g = 0.01, 95% CI: − 0.11, 0.12. I2 = 0.00). Three systematic reviews reported on RCTs not incorporated in the meta-analysis which favoured rehabilitation intervention versus comparison after inpatient stay [42, 45] and reported conflicting evidence for follow-up [41, 42, 45].
Length of stay
Rehabilitation did not reduce the length of stay versus comparison after inpatient stay (29 RCTs including 6971 participants; mean difference = − 0.54, 95% CI: − 1.32, 0.23. I2 = 88.13, 3 RCTs favoured comparison); however, evidence was detected for small study sample bias (p < 0.001). For estimates of length of stay, the total effect of rehabilitation interventions adjusted for age, target population, RCT geography, and publication year was significant (p < 0.001) in meta-regression. A subsequent stratified meta-analysis by RCT geography was conducted. The absence of an effect of rehabilitation on length of stay persisted across regions with substantial heterogeneity for Australia (I2 = 86.26) and Europe (I2 = 76.47), and heterogeneity which may not be important for the United States of America (I2 = 18.10%).
Mortality
Rehabilitation did not reduce mortality among older adults with unplanned hospital admission versus comparison after inpatient rehabilitation (12 RCTs including 5619 participants; Hedges g = − 0.09, 95% CI: − 0.40, 0.23. I2 = 4.24, 1 RCT favoured comparison) or 1–12 month follow-up (13 RCTs including 4366 participants; Hedges’ g = − 0.12, 95% CI: − 0.28, 0.05. I2 = 0.00), further supported by an RCT from 1 systematic review not included in the meta-analysis [40]. No evidence was detected of small study sample bias.
Discussion
Main findings
We identified 12 systematic reviews of moderate to low quality which included 44 unique RCTs relevant to the current overview. When incorporated in a rehabilitation intervention, we report a large effect of the treatment ingredients endurance exercise (exclusively from RCTs of older adults with COPD), early intervention (predominantly from RCTs of older adults after hip fracture) and shaping knowledge (exclusively from RCTs of older adults with COPD) on walking endurance after the inpatient stay versus comparison. We also reported beneficial effects of early intervention, repeated practice activities, goals and planning, increased medical care and/or discharge planning on discharge home. The evidence for effectiveness of treatment ingredients that improve ADL was conflicting. Rehabilitation interventions were not found to be effective for functional mobility, strength, or quality of life, or reduce length of stay or mortality. Therefore, we did not explore the potential role of treatment ingredients for these outcomes.
Interpretation
Given ceaseless drives to decrease inpatient lengths of stay, it is important for clinicians to preferentially select treatment ingredients most likely to improve outcomes at discharge [13]. However, for effective inpatient rehabilitation interventions, previous systematic reviews highlighted a lack of sufficient data to determine the key features of successful interventions [15, 16]. We sought to supplement the existing evidence by exploring the role of individual treatment ingredients in the overall effectiveness of inpatient rehabilitation. We employed Treatment Theory [9,10,11,12] as a framework for the identification of treatment ingredients which may contribute to reported effectiveness. Our analyses identified a select few treatment ingredients for consideration by clinicians.
The treatment ingredient endurance exercise had a positive effect on walking endurance. This is important as objective quantitative data indicate adults over the age of 65 years take a median of just 468 steps per day during their inpatient stay (no difference by admitting reason or illness severity) [50]. Given the delay between discharge from the inpatient setting to initiation of community rehabilitation, it is important to optimise walking endurance early in rehabilitation [51, 52]. Three RCTs were included in the analysis of endurance exercise; all included patients with COPD exacerbations and these favoured the intervention group. The treatment ingredient was comprised of pedal ergometry daily with increased resistance [53], treadmill training twice daily with increasing duration (from 5 to 20 minutes) [54], or walking five times per day [55]. The largest individual effect sizes were noted for walking five times per day, followed by treadmill training twice daily, and then pedal ergometry (Supplementary File 6). A walking program does not require equipment and could be supported by members of the multidisciplinary team [56, 57] as well as formal and informal carers [49] during the inpatient stay. Where staffing levels are low and a walking programme could not be supported, pedal ergometry offers a low-cost alternative which could be completed at the bedside.
With bedrest, muscle strength is lost rapidly at a rate of 5% per day [5]. We found early intervention as a treatment ingredient to be effective at increasing endurance and the likelihood of a home discharge when incorporated into inpatient rehabilitation for older adults after an unplanned hospital admission. This is unsurprising given potential for rehabilitation to mitigate hospital-associated deconditioning [43] and prevent discharge to a higher level of care [58]. Most RCTs focused on older adults undergoing surgery for hip fracture (n = 7, 78%) with early intervention defined by mobilisation from bed within the first two days of surgery. This evidence has informed wide acceptance older adults with hip fracture should receive early mobilisation after surgery with early mobilisation a key performance indicator in national audits [59].
A discharge destination of home was more likely among participants who received interventions which incorporated treatment ingredients of goals and planning, repeated practice of activities, increased medical care, and/or discharge planning versus comparison. More specific detail for these treatment ingredients was limited. For example, repeated practice of activities often reflected ‘ADL training’ with no further detail related to the frequency, duration, or type of activities. One RCT specified transfers were practiced twice daily for 30 minutes [60]. Another indicated ADL training was completed twice daily for five days of the week but did not specify which activities were practiced [61].
Comparison with other studies
The findings of the current overview are consistent with those of the underlying systematic reviews which conclude that inpatient rehabilitation can improve functioning [15, 43, 48, 49] and the likelihood of discharge to home [15, 17, 48], but has no effect on mortality [17, 48] or length of stay [17, 46, 48] versus comparison (usual care for 95% of RCTs). This current overview does not support previous findings where inpatient rehabilitation led to improvements in quality of life [42, 45], or reductions in length of stay [47] or mortality [15]. This absence of an effect for the current overview may be due to the fact usual care comprised some form of rehabilitation in 29 of the 44 RCTs (2 additional not specified) which may attenuate the estimate of rehabilitation effectiveness between groups.
Limitations
There are several limitations to this overview review. First, we needed to make two protocol changes a) outcome data were extracted at ‘end of inpatient rehabilitation’, which was a change from our protocol which specified ‘on discharge’ due to lack of clarity in published data, and b) we excluded systematic reviews exclusively addressing post-stroke rehabilitation at full text selection due to their often impairment focus (e.g., upper limb motor deficit) that would not be potentially translatable to other admitting diagnoses. Second, where intervention detail was limited, we termed treatment ingredients such as repeated exercise rehabilitation where exercise rehabilitation was mentioned but not detailed, shaping knowledge where education was specified but not detailed, or increased medical care where examples of what ‘increased care’ may entail were provided but not explicitly measured. This may have led to an underestimation of more specific treatment ingredients. Third, we noted moderate to substantial heterogeneity for several outcomes overall and by treatment ingredient. It was not possible to complete meta-regression across all analyses due to the low number of RCTs [28]. For each analysis, we report the count of RCTs that favoured the comparison to guide the reader in their interpretation of uncertainty due to heterogeneity. Fourth, we attempted to reduce the number of analyses (and risk of multiplicity) by focusing on outcomes which changed following rehabilitation interventions [28]. Nonetheless, there is a risk some of the reported effects may be due to chance alone [28]. Fifth, we stratified meta-analyses by treatment ingredient to explore which treatment ingredients may be more or less effective. We were not able to determine whether potentially ineffective treatment ingredients become effective when combined with other treatment ingredients [10]. Sixth, we defined ‘functioning’ by body functions and activities and did not evaluate the effect of treatment ingredients on participation as an aspect of functioning [7]. Finally, an overview review only reports on data that have been published, systematically reviewed and/or meta-analysed and includes limitations of included RCTs [62].
Implications for clinical practice and research
The effect of endurance exercise on endurance was reflective of three RCTs of older adults with an unplanned admission due to an exacerbation of COPD while the findings from early intervention predominantly reflected older adults with hip fracture. These treatment ingredients should be prioritised for implementation for these patient groups. It may be reasonable to generalise the recommendations to similar groups of older adults with an unplanned admission to hospital. For example, early intervention may be generalised to other non-hip fragility fractures [63], and endurance exercise to patients admitted with exacerbations of other chronic lung diseases [64]. Whether the recommendations may be generalised to less similar groups require more consideration. For example, in the current overview no systematic reviews included RCTs explicitly focusing on older adults with heart failure. This is likely as most cardiac rehabilitation spans both hospital and community settings (and therefore would be excluded from the current overview). Endurance exercise is a key component of most cardiac rehabilitation programmes offered to older adults with heart failure [65]. However, the time at which an endurance programme begin relative to hospital admission is not clear. Given early intervention (mobilisation) is recommended for older adults admitted with an exacerbation of heart failure [66] a walking programme with a gradual increase in intensity from early post-admission likely reflects current clinical practice. Whether outcomes would vary for higher dosage and following the use of alternate equipment e.g., cycle ergometers requires additional research.
It was possible to assign treatment ingredients to inpatient rehabilitation interventions. However, for many, the interventions were poorly described limiting exploration of more specific treatment ingredients and/or the ingredient dose. Moreover, the description of usual care comparator groups was limited and those inclusive of rehabilitation could attenuate the between group comparisons for effectiveness. These are not new findings with several previous systematic reviews highlighting the challenges in synthesizing the evidence for rehabilitation interventions [15, 16]. This may have contributed to the observed heterogeneity for some analyses of the current overview. There is a need for more transparent reporting of rehabilitation interventions in line with established frameworks such as the template for intervention description and replication (TIDieR) [67]. A taxonomy of rehabilitation techniques similar to the taxonomy of behaviour change techniques is required for future analyses by individual treatment ingredients and interactions between ingredients [26].
Conclusion
The designation of treatment ingredients to interventions was challenging due to a paucity of detail specified by published interventions. Despite this, we reported the treatment ingredients early intervention and endurance exercise were effective at improving endurance, and early intervention, goals and planning, repeated practice of activities, increased medical care, and/or discharge planning effectively increased the likelihood of discharge to home for older adults following an unplanned admission to hospital. Benefits observed were often for subgroups of the older adult population e.g., endurance exercise was effective for endurance in older adults with COPD, and early intervention was effective for endurance for those with hip fracture. Future research should seek to determine whether the benefits observed from these treatment ingredients are generalisable to older adults more broadly. Further, there is a need for more transparent reporting of rehabilitation intervention treatment ingredients to enable future synthesis and/or replication. Finally, the challenge of making meaningful change during a short period of inpatient rehabilitation emphasizes the importance of comprehensive post-discharge rehabilitation.
Availability of data and materials
This overview review reflects a synthesis of previously published randomized controlled trials. All data generated or analysed during this study are included in this published article (and its supplementary files).
Abbreviations
- ADL:
-
Activities of daily living
- CI:
-
Confidence Interval
- OR:
-
Odds ratio
- ICF:
-
International classification of functioning
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- RCT:
-
Randomised controlled trial
- AMSTAR:
-
Assessment of Multiple Systematic Reviews
References
United Nations Department of economic and social affairs. World Population Ageing 2019. https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf
Office for National Statistics. Living longer: how our population is changing and why it matters. 2018. https://www.ons.gov.uk/releases/livinglongerhowourpopulationischangingandwhyitmatters
Terraneo M. Inequities in health care utilization by people aged 50+: evidence from 12 European countries. Soc Sci Med. 2015;126:154–63.
Kingsley DE. Aging and health care costs: narrative versus reality. Poverty Public Policy. 2015;7:3–21.
Harper CM, Lyles YM. Physiology and complications of bed rest. J Am Geriatr Soc. 1988;36(11):1047–54.
Hirshon JM, et al. Health systems and services: the role of acute care. Bull World Health Organ. 2013;91(5):386–8.
World Health Organisation. International classification of functioning, Disability and Health 2001.
World Health Organisation. World Report on Ageing and Health. 2016.
Whyte J, Barrett AM. Advancing the evidence base of rehabilitation treatments: a developmental approach. Arch Phys Med Rehabil. 2012;93(8 Suppl):S101–10.
Whyte J, Contributions of treatment theory and enablement theory to rehabilitation research and practice. Arch Phys Med Rehabil. 2014;95(1 Suppl):S17–23. e2.
Whyte J. Directions in brain injury research: from concept to clinical implementation. Neuropsychol Rehabil. 2009;19(6):807–23.
Hart T, et al. A theory-driven system for the specification of rehabilitation treatments. Arch Phys Med Rehabil. 2019;100(1):172–80.
National Health Service. Guide to reducing long hospital stays. 2018. https://www.england.nhs.uk/urgent-emergency-care/reducing-length-of-stay/
Connolly B, et al. Physical rehabilitation interventions for adult patients during critical illness: an overview of systematic reviews. Thorax. 2016;71(10):881–90.
Bachmann S, et al. Inpatient rehabilitation specifically designed for geriatric patients: systematic review and meta-analysis of randomised controlled trials. BMJ. 2010;340:c1718.
Chudyk AM, et al. Systematic review of hip fracture rehabilitation practices in the elderly. Arch Phys Med Rehabil. 2009;90(2):246–62.
de Morton NA, Keating JL, Jeffs K. Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev. 2007;1:CD005955.
Beswick AD, et al. Complex interventions to improve physical function and maintain independent living in elderly people: a systematic review and meta-analysis. Lancet. 2008;371(9614):725–35.
Ayis S, et al. Applying the impairment, activity limitation, and participation restriction constructs of the ICF model to osteoarthritis and low back pain trials: a reanalysis. J Rheumatol. 2010;37(9):1923–31.
Moher D, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Levack WMM, et al. One in 11 Cochrane reviews are on rehabilitation interventions, according to pragmatic inclusion criteria developed by Cochrane rehabilitation. Arch Phys Med Rehabil. 2019;100(8):1492–8.
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276–82.
Pieper D, et al. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67(4):368–75.
Shea BJ, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Michie S, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
Higgins JPT, T.J., Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). , Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook. 2021.
Pollock M, F.R., Becker L, Pieper D, Hartling L., chapter V: overviews of reviews., in Cochrane handbook for systematic reviews of interventions version 61 (updated September 2020). Cochrane, Editor 2020.
StataCorp. Stata statistical software: release 16. College Station, TX: StataCorp LLC; 2019.
Cameron ID, et al. Co-ordinated multidisciplinary approaches for inpatient rehabilitation of older patients with proximal femoral fractures. Cochrane Database Syst Rev. 2000;4:CD000106.
Crotty M, et al. Rehabilitation interventions for improving physical and psychosocial functioning after hip fracture in older people. Cochrane Database Syst Rev. 2010;1:CD007624.
Fox MT, et al. Effectiveness of acute geriatric unit care using acute care for elders components: a systematic review and meta-analysis. J Am Geriatr Soc. 2012;60(12):2237–45.
Handoll HH, et al. Multidisciplinary rehabilitation for older people with hip fractures. Cochrane Database Syst Rev. 2009;4:CD007125.
Hu Y, et al. Effect of early mobilization on the physical function of patients in intensive care unit: a Meta-analysis. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2019;31(4):458–63.
Puhan MA, et al. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;12:CD005305.
Talevski J, et al. Effect of clinical care pathways on quality of life and physical function after fragility fracture: a Meta-analysis. J Am Med Dir Assoc. 2019;20(7):926 e1–926 e11.
Thorne F, Baldwin C. Multimodal interventions including nutrition in the prevention and management of disease-related malnutrition in adults: a systematic review of randomised control trials. Clin Nutr. 2014;33(3):375–84.
Van Craen K, et al. The effectiveness of inpatient geriatric evaluation and management units: a systematic review and meta-analysis. J Am Geriatr Soc. 2010;58(1):83–92.
Handoll HH, Sherrington C, Mak JC. Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database Syst Rev. 2011;3:CD001704.
Heldmann P, et al. Early inpatient rehabilitation for acutely hospitalized older patients: a systematic review of outcome measures. BMC Geriatr. 2019;19(1):189.
Machado A, et al. Design of pulmonary rehabilitation programmes during acute exacerbations of COPD: a systematic review and network meta-analysis. Eur Respir Rev. 2020;29(158):1–13.
Martinez-Velilla N, et al. Physical activity and early rehabilitation in hospitalized elderly medical patients: systematic review of randomized clinical trials. J Nutr Health Aging. 2016;20(7):738–51.
Peck M, Holthaus A, Kingsbury K, Salsberry MG, Duggirala V, Mobility in acute Care for Geriatric Patients with orthopedic conditions: a review of recent literature. Curr Geriatrics Rep. 2020;9(4):300–10.
Peiris CL, et al. Additional physical therapy services reduce length of stay and improve health outcomes in people with acute and subacute conditions: an updated systematic review and Meta-analysis. Arch Phys Med Rehabil. 2018;99(11):2299–312.
Scrivener K, et al. After-hours or weekend rehabilitation improves outcomes and increases physical activity but does not affect length of stay: a systematic review. J Physiother. 2015;61(2):61–7.
Smith TO, et al. Enhanced rehabilitation and care models for adults with dementia following hip fracture surgery. Cochrane Database Syst Rev. 2020;2:CD010569.
Smith TO, et al. Interventions for reducing hospital-associated deconditioning: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2020;90:104176.
Yasmeen I, et al. The effect of caregiver-mediated mobility interventions in hospitalized patients on patient, caregiver, and health system outcomes: a systematic review. Arch Rehabil Res Clin Transl. 2020;2(3):100053.
Fisher SR, et al. Ambulatory activity of older adults hospitalized with acute medical illness. J Am Geriatr Soc. 2011;59(1):91–5.
Royal College of Physicians. Falls and fragility fracture audit Programme. Recovering after a hip fracture: helping people understand physiotherapy in the NHS. Physiotherapy ‘Hip Sprint’ audit report London 2017.
Harding KE, et al. Reducing waiting time for community rehabilitation services: a controlled before-and-after trial. Arch Phys Med Rehabil. 2013;94(1):23–31.
Torres-Sanchez I, et al. Effects of an exercise intervention in frail older patients with chronic obstructive pulmonary disease hospitalized due to an exacerbation: a randomized controlled trial. COPD. 2017;14(1):37–42.
He M, et al. Efficiency and safety of pulmonary rehabilitation in acute exacerbation of chronic obstructive pulmonary disease. Med Sci Monit. 2015;21:806–12.
Kirsten DK, et al. Exercise training improves recovery in patients with COPD after an acute exacerbation. Respir Med. 1998;92(10):1191–8.
King BJ, et al. Getting patients walking: a pilot study of mobilizing older adult patients via a nurse-driven intervention. J Am Geriatr Soc. 2016;64(10):2088–94.
Hastings SN, et al. Early mobility in the hospital: lessons learned from the STRIDE program. Geriatrics (Basel). 2018;3(4).
Fortinsky RH, et al. Effects of functional status changes before and during hospitalization on nursing home admission of older adults. J Gerontol A Biol Sci Med Sci. 1999;54(10):M521–6.
Royal College of Physicians. National hip Fracture Database annual report 2019. London: RCP; 2019. https://www.rcplondon.ac.uk/projects/outputs/national-hip-fracture-database-nhfd-annual-report-2019
Jones CT, L.A., MacGregor L, Brand CA, Tweddle N, Russell DM., A randomised controlled trial of an exercise intervention to reduce functional decline and health service utilisation in the hospitalised elderly. Australas J Ageing. 2006;25:126–133.
Naglie G, et al. Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial. CMAJ. 2002;167(1):25–32.
Fusar-Poli P, Radua J. Ten simple rules for conducting umbrella reviews. Evid Based Ment Health. 2018;21(3):95–100.
British Orthopaedic Association Standrad. The care of the older or frail orthopaedic trauma patient. 2019 https://www.boa.ac.uk/uploads/assets/a30f1f4c-210e-4ee2-98fd14a8a04093fe/boast-frail-and-older-care-final.pdf.
Tachi H, et al. Osimertinib-induced interstitial lung disease presenting as Eosinophilic pneumonia. J Thorac Oncol. 2017;12(8):e118–20.
Long L, et al. Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst Rev. 2019;1:CD003331.
Fleming LM, et al. Early ambulation among hospitalized heart failure patients is associated with reduced length of stay and 30-day readmissions. Circ Heart Fail. 2018;11(4):e004634.
Hoffmann TC, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687.
Acknowledgements
Thank you to Camilla Kristensen, Sofia Hemrage, and Esme Elsden who supported screening, quality appraisal and data extraction respectively.
Funding
This work was supported by a UKRI Future Leaders Fellowship [Grant Ref: MR/S032819/1].
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. In addition, KL, SG, KJS, GSdP, and SA contributed to the acquisition and the analysis of data. All authors contributed to the interpretation of the analysis. KL, SG and KJS drafted the manuscript. All authors critically revised the manuscript. All authors approved the final version for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
KS received a grant from UK Research & Innovation Future Leaders Fellowship to support this work. This funding provides salary support for KS, KL, and SG. KS also received funding from the National Institutes of Health Research (NIHR) and Chartered Society of Physiotherapy Charitable Trust for hip fracture health services research. CS, NEF, NW and EG receive funding from the National Institute for Health Research (NIHR). CS and NEF are NIHR Senior Investigators. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. CLG receives funding from Versus Arthritis (ref 22086). GSdP, SA, IDC, and FCM have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary File 1.
Search strategies. Search strategies for electronic databases of published and unpublished evidence.
Additional file 2: Supplementary File 2.
Citation matrix. Citation matrix detailing the identification of unique (non-overlapping) randomized controlled trials from systematic reviews included in this overview review.
Additional file 3: Supplementary File 3.
Characteristics of randomized controlled trials. Characteristics of eligible randomized controlled trials identified from systematic reviews included in this overview review.
Additional file 4: Supplementary File 4.
Treatment ingredients. Treatment ingredients employed by eligible randomized controlled trials identified from systematic reviews included in this overview review.
Additional file 5: Supplementary File 5.
Meta-analyses results. Results of meta-analyses (forest plot) of randomized controlled trials identified from systematic reviews included in this overview review for functioning, quality of life, length of stay, discharge destination and mortality. Each meta-analysis is accompanied by a table which describes the characteristics of each randomized controlled trial included in each meta-analysis.
Additional file 6: Supplementary File 6.
Treatment ingredient meta-analyses results. Results of meta-analyses (forest plot) of randomized controlled trials identified from systematic reviews included in this overview review by treatment ingredient.
Additional file 7: Supplementary File 7.
Narrative results. Results of randomized controlled trials identified from systematic reviews included in this overview review which were not incorporated into the meta-analyses and reasons why they were not incorporated.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lambe, K., Guerra, S., Salazar de Pablo, G. et al. Effect of inpatient rehabilitation treatment ingredients on functioning, quality of life, length of stay, discharge destination, and mortality among older adults with unplanned admission: an overview review. BMC Geriatr 22, 501 (2022). https://doi.org/10.1186/s12877-022-03169-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03169-2