Abstract
Background
Metabolic Syndrome (MetS) is a common health problem among older adults. Previous studies have revealed the relationship between sleep duration as well as global sleep status and MetS.
Objectives
This study aims to examine the association between the specific sleep characteristic and MetS as well as MetS components among community-dwelling old adults.
Methods
This cross-sectional study included 1499 community residents aged ≥ 60 years. Sleep characteristics were assessed using the Pittsburgh Sleep Quality Index (PSQI) and bed/rise time of the residents. Logistic regression analysis and multiple linear regression analysis were used to examine the associations between sleep characteristics and MetS as well as MetS components. A generalized additive model was built to assess the smooth relationship between triglyceride (TG) levels and sleep duration.
Results
Of the 1499 participants, 449 (30.0%) had MetS, and 443 (29.6%) had poor sleep quality. The rise time was found to be associated with MetS (> 6:00 vs. 5:00 ~ 6:00: adjusted OR (95%) = 1.77 (1.17–2.69), P = 0.007). For the MetS components, a U-shaped relationship was first revealed for sleep duration and TG levels (EDF = 1.85, P < 0.001). Furthermore, significant associations also included the associations of subjective sleep quality and daytime dysfunction with hypertension, the associations of sleep efficiency and rise time with hyperglycemia, the associations of rise time with TG levels, and the association of bedtime with waist circumference.
Conclusions
The different sleep characteristics were associated with different MetS components.
Similar content being viewed by others
Background
Metabolic syndrome (MetS) is a clustering of clinical syndromes with obesity, hyperglycemia (diabetes mellitus or impaired glucose regulation), dyslipidaemia (high serum triglyceride (TG) levels and/or low high-density lipoprotein cholesterol (HDL-C) levels) and hypertension. MetS is a common health problem among older adults, and its prevalence ranges from 24.5% to 30.5% among Chinese adults and ranges from 32.4% to 36.9% among older adults [1,2,3]. The pathogenic mechanisms of MetS are complex. Previous studies have shown that environmental factors and lifestyle factors play an important role [4]. Sleep as a modifiable lifestyle factor has been shown to be associated with MetS.
The prevalence of sleep disorder in China ranges from 47.2% to 49.9% for the population ≥ 60 years old [5, 6], and it often coexists with MetS in older population. Studies have shown that the Sleep curtailment affects human metabolism and endocrine function, and then affects the quality of life and health of older adults in the long term [7, 8]. Some studies have revealed the biological mechanism by which sleep contributes to the risk of MetS. Sleep disorders or short sleep duration can cause hypertension, overweight, obesity, type 2 diabetes, and dyslipidemia through affect sympathetic nerve activity [9], regulate leptin and ghrelin [10, 11], reduce insulin sensitivity, promote insulin resistance [12, 13], stimulate lipodieresis, increase plasma free fatty acid level [14]and other multiple biological mechanisms, all of which are risk factors for MetS. In the past few years, several studies have identified that sleep duration is associated with MetS [15,16,17,18,19] and MetS components such as waist circumference (WC), fasting plasma glucose (FPG) levels, TG levels, and HDL-C levels [20]. In addition, sleep characteristics based on Pittsburgh Sleep Quality Index (PSQI) were reported to be associated with MetS or MetS both in cross-sectional studies [21,22,23] and prospective study [24]. However, most studies only focused on individual sleep characteristic or global PSQI score. It is also worthwhile to observe which sleep characteristic has the best correlation with the specific MetS component. In addition, sleep characteristic profiles and their associations with MetS components among community-dwelling older adults have seldom been reported. Using a population-based cross-sectional study, the present study aimed to depict the sleep characteristics, including global PSQI quality, each of PSQI characteristics and rise/bed time, among older adults in China, and explore the correlation between these sleep characteristics and MetS components.
Methods
Participants and sampling
This population-based cross-sectional study was performed in Songjiang District, Shanghai, China, from May 1 2020 to December 31 2020. Participant recruitment was conducted using a multistage random sampling method. The samples of this study came from 15 blocks in Songjiang District. Neighborhoods with more than 200 residents aged ≥ 60 years were selected from 15 blocks. Among these selected neighborhoods, one neighborhood was randomly selected from each block and the list of home addresses was extracted. A total of 3534 permanent residents aged ≥ 60 years were selected and were invited to participate in the project. The neighborhood committee issued informed consent forms to these residents on the list. Informed consent forms stated that participants should have no diagnosed mental disorders and were physically able to conduct the survey. Participants came to the community health care center to participate in the investigation with signed informed consent forms, identity card and medical card. A total of 1646 participants aged ≥ 60 years came to participate in the investigation and none of the participants was found to have a medical record of mental disorders after a medical card was checked. Of the 1646 participants, 62 participants were missing sleep data, and 85 participants with a sleep efficiency greater than 1 which were considered as invalid data. Finally, 1499 participants were included in this study for analysis. Demographic information of the participants was collected via a face-to-face questionnaire survey, including age, sex, education level, marital status, depression, and lifestyles (drinking, smoking, sleep, physical activity, etc.).
This project was combined with the National Public Health Service Physical Examination Program for The Elderly. In the physical examination program, anthropometric indices, including WC, height and weight, were measured. Blood pressure (BP) was measured with a mercury sphygmomanometer. All participants provided venous blood samples after 12 h of overnight fasting. Fasting plasma glucose (FPG, hexokinase method), triglycerides (GPO-PAP), and high-density lipoprotein cholesterol (HDL-C, homogeneous enzyme immunoassay) were measured.
Measures and definitions
Metabolic syndrome
Metabolic syndrome (MetS) was defined according to the guidelines for the prevention and treatment of dyslipidemia in Chinese adults (Revised Edition 2016). Participants who met at least three of the following conditions were defined as having MetS: (1) WC ≥ 90 cm in men, or ≥ 85 cm in women; (2) Hyperglycemia: FPG level ≥ 6.1 mmol/L or Oral Glucose Tolerance Test (OGTT) 2 h plasma glucose level ≥ 7.8 mmol/L, and/or previously diagnosed diabetes that was under treatment; (3) Hypertension: BP ≥ 140/90 mmHg and/or diagnosed with hypertension that was under treatment; (4) HDL-C level < 1.04 mmol/L; and (5) TG level ≥ 1.70 mmol/L.
Sleep characteristics
Sleep characteristics were assessed using the Pittsburgh Sleep Quality Index (PSQI) and bed/rise time. The PSQI is a 19-item self-report questionnaire that assesses sleep quality and disturbances during the last month and generates seven component scores: subjective sleep quality, sleep latency (time spent before falling asleep), sleep duration (nocturnal), sleep efficiency (proportion of sleep duration to total time spent in bed), sleep disturbances, sleep drug use, and daytime dysfunction. The sum of the scores for these seven components forms a global PSQI score that ranges from 0 to 21, and a higher PSQI score indicates worse sleep quality. A global PSQI score greater than 5 was defined to differentiate poor sleep quality from good sleep quality. Each of the 7 sleep characteristics was analyzed on a 0–3 scale. Subjective sleep quality (0-very good sleep quality; 1—general sleep quality; 2—bad sleep quality; 3—very bad sleep quality) and sleep latency (0—≤ 15 min, 1—16 ~ 30 min, 2—31 ~ 60 min, 3—> 60 min) were assessed from 0–3 points. Sleep efficiency was divided into three groups (0—≥ 85%; 1—75% ~ 84%; 2—< 75%). Sleep duration was divided into three groups (0—6–8 h; 1—< 6 h; 2—> 8 h). Sleep drugs were divided into two groups (score = 0 was defined as no use; scores = 1, 2 and 3 were defined as use). Sleep disturbances were divided into three groups (score = 0 was defined as no; score = 1 was defined as mild; scores = 2/3 were defined as moderate-severe). Daytime dysfunction was divided into two groups (score = 0 was defined as no; scores = 1, 2 and 3 were defined as yes). Rise time was classified into four groups: < 5:00, 5:00 ~ 6:00, 6:01 ~ 7:00, and > 7:00, and bed time was classified into four groups: < 21:00, 21:00 ~ 22:00, 22:01 ~ 23:00, and > 23:00 [25].
Covariates
Data on age, sex, marital status (married and single) and education levels (illiterate, primary school and ≥ junior school) were collected from participants' self-reports. BMI was calculated as weight in kilograms divided by height in metres squared. Smoking status was defined by two questions: “Have you smoked 100 cigarettes so far?” and “Have you smoked in the past 30 days?” According to the answers to these two questions, smoking was divided into three categories. Those who had not smoked 100 cigarettes so far were defined as never smokers; those who had smoked 100 cigarettes so far and had not smoked in the past 30 days were defined as people who given up smoking; those who had smoked 100 cigarettes so far and had smoked in the last 30 days were defined as current smokers. Drinking status was categorized as drinking and never drinking. Physical activity (PA) was assessed by two questions: “During the last week, how many days did you perform moderate-intensity physical activities, such as playing badminton, walking fast, playing table tennis and square dancing? (None, 1–2 times, 3–4 times, 5–6 times, 7 times or more)” and “How much time did you spend doing physical activities each time you performed them? (< 20 min, 20–30 min, 30-40 min, 40–50 min, > 50 min)” [26], and the product of these two answers was used to calculate the time interval of PA in a week. Based on the American Heart Association's recommendation [27] and current recommendations for the practicing of physical activity [28], PA was categorized as inactive (PA < 150 min/week) and active (PA ≥ 150 min/week). Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9), which consists of 9 questions. The scores for each question range from 0 (not at all) to 1 (several days), 2 (more than half of the days), and 3 (nearly every day). The total score can range from 0–27 points. The participants were divided into five groups based on the total score (0–4: no depression, 5–9: mild depression, 10–14: moderate depression, 15–19: moderate to severe depression, and 20–27: major depression).
Statistical analysis
Sociodemographic and sleep characteristics of the participants were shown using descriptive statistical methods. Comparisons were performed using t tests for continuous variables between the MetS group and the non-MetS group and chi-square tests for categorical variables. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated using logistic regression model for the analysis of MetS’s association with the global sleep quality (poor sleep quality: PSQI score > 5, good sleep quality: PSQI score ≤ 5) and each PSQI characteristic. The associations of MetS components with global sleep quality or with each of 7 PSQI characteristics were furtherly analyzed. Multiple linear regression models were used for association between three continuous variables components of MetS (WC levels, TG levels and HDL-C levels) and sleep characteristics and multivariate logistic regression analysis were used for the association between hyperglycemia and hypertension (as a dichotomous variable according to the diagnostic criteria of metabolic syndrome) and sleep characteristics. Adjustments for age, sex, BMI, drinking status, smoking status, PA, and depression were made in all the multivariate analyses mentioned above. To examine nonlinear relationships between sleep duration and MetS/each MetS components, a generalized additive model (GAM) was built to explore their smooth relationships. Age, sex, BMI, smoking status, drinking status, PA and depression were applied to adjust the GAM. All analyses were performed using STATA software (version 16.0) and R (version 3.6.3), and a P < 0.05 was defined as statistically significant.
Results
Participants characteristics
The characteristics of participant are displayed in Table 1. The mean age of all 1499 participants was 72.39 ± 5.65 years (range 65–101 years), and the mean BMI was 24.08 ± 3.54 kg/m2. The majority of the participants were female (55.4%), illiterate (44.3%), married (82.4%), never drinkers (83.2%), never smokers (75.9%), physically inactive (55.8%), and not depressed (86.6%).
Of all the participants, 29.6% had poor sleep quality (PSQI score > 5), 14.5% had bad/very bad subjective sleep quality, 76.0% had mild/moderate-severe sleep disturbances and 34.6% had daytime dysfunction. The majority of older adults had normal sleep duration (6-8 h) (75.7%), went to bed at 21:00 ~ 22:00 PM (56.6%) and got up at 5:00 ~ 6:00 AM (76.5%). Of all participants, 30.0% had MetS. Participants with MetS were slightly, but statistically significantly younger (71.81 vs. 72.64, P = 0.008), and had higher BMI level (26.32 vs. 23.12, P < 0.001) and higher prevalence of female (64.1% vs. 51.7%, P < 0.001) than those without MetS. There were no differences in the distribution of global PSQI scores, any of PSQI characteristic, bed time and rise time between MetS group and non-MetS group.
Relationship between sleep characteristics and MetS
The results of logistic regression analysis on the associations between sleep characteristics and MetS after adjusting for age, sex, BMI, smoking status, drinking status, PA and depression are shown in Table 2. Older adults with rise time > 6:00 had higher odds of being MetS compared to those with rise time of 5:00 ~ 6:00 (univariate analysis: OR = 1.46, 95% CI 1.00–2.12, P = 0.048; multivariate analysis: OR = 1.77, 95% CI 1.17–2.69, P = 0.007). The global PSQI score and each PSQI characteristic had no significant association with MetS.
Sleep characteristic profiles and MetS spectrum
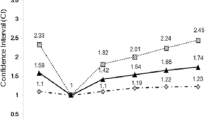
Figure 1 shows the significant associations between each PSQI characteristic and MetS component, including of significant associations of subjective sleep quality and daytime dysfunction with hypertension, the associations of sleep efficiency and rise time with hyperglycemia, the associations of sleep duration and rise time with TG levels, and the association of bed time with WC. Specifically, participants with general quality (OR = 1.45, 95% CI 1.10–1.90, P = 0.008) and bad subjective sleep quality (OR = 2.16, 95% CI 1.36–3.45, P = 0.001) had higher odds of being hypertension compared with those with very good subjective sleep quality (Fig. 2A). Participants undergoing daytime dysfunction have higher odds of being hypertension compared with those without daytime dysfunction. (OR = 1.36, 95% CI 1.02–1.80, P = 0.035, Fig. 2B). For the hyperglycemia, the chance of having an association with hyperglycemia was 1.40 times higher for the participants with a sleep efficiency of 75% ~ 84% than those with a sleep efficiency of ≥ 85% (OR = 1.40, 95% CI 1.05–1.85, P = 0.021, Fig. 2C), and participants with rise time > 6:00 also had higher odds of being hyperglycemia than those with rise time 5:00 ~ 6:00 (OR = 1.75, 95%CI 1.20–2.55, P = 0.003, Fig. 2D). With respect to the TG, participants with rise time > 6:00 had higher TG levels (β = 0.398, 95% 0.170–0.626, P = 0.001, Fig. 2E) than those with rise time of 5:00 ~ 6:00, and participants with rise time < 5:00 had lower TG levels (β = -0.198, 95% -0.380- -0.015, P = 0.034, Fig. 2E) than those with rise time of 5:00 ~ 6:00. In addition, participants with sleep duration of more than > 8 h had higher TG levels than those with sleep duration of 6 ~ 8 h hours (β = 0.358, 95% 0.162–0.555, P < 0.001, Fig. 2F). Moreover, participants with bed time > 22:00 have higher WC levels compared to those with bed time 21:00 ~ 22:00 (β = 1.923, 95% 0.281–3.565, P = 0.022, Fig. 2G).
Relationship between sleep characteristics and MetS components. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated using logistic regression model for sleep characteristics’ association with hypertension and hyperglycemia. The standardized regression coefficients (β) and 95% CI was estimated using multiple linear regression model for sleep characteristics’ association with WC levels, TG levels and HDL-C levels. The OR and β were adjusted for age, sex, BMI, smoking status, alcohol use status, physical activity and depression. P values were presented with asterisks: *P < 0.05, **P < 0.01
Specific description of significant associations between sleep characteristics and MetS components. Subjective sleep quality (A) and Daytime dysfunction (B) was associated with hypertension. Sleep efficiency (C) and rise time (D) was associated with hyperglycemia. Rise time (E) and sleep duration (F) was associated with triglyceride levels. (G) Bed time was associated with WC levels
The nonlinear relationship between sleep duration and TG levels was further probed by the generalized additive model. As shown in Fig. 3, a U-shaped association with a significant nonlinear fit between sleep duration and TG levels was found both in the univariable GAM (EDF = 1.81, P = 0.004) and in the multivariable GAM. (EDF = 1.85, P < 0.001).
Plots of estimated smoothing spline function of sleep duration with 95% confidence intervals for the generalized additive model when the response variable was triglyceride levels. (A) Model 1 shows the univariable smooth function of sleep duration (EDF = 1.81, P = 0.004). (B) Model 2 shows the multivariable smooth function of sleep duration, adjusted for age, sex, BMI, smoking status, alcohol use status, physical activity and depression (EDF = 1.85, P < 0.001)
Discussion
The present study demonstrated that several sleep characteristics were associated with metabolic syndrome (MetS) or the component of MetS in older Chinese adults, including poor subjective sleep quality, sleep insufficiency, daytime dysfunction, a sleep duration that was too long or too short, go to bed late and waking up late.
We first reported that older adults with rise time > 6:00 had higher odds of being MetS and hyperglycemia, and higher triglyceride (TG) levels, compared to those with rise time 5:00 ~ 6:00. In addition, we also found that older adults with bed time > 22:00 had higher waist circumference (WC) levels than those with bed time 21:00 ~ 22:00. These results indicated that sleep–wake cycle might influence the risk of MetS through regulating the glucose, WC and TG levels. We are rarely aware of any published study that has examined the association between the rise/bed time and MetS components. To our knowledge, only one study conducted among Iranian adults reported that waking earlier than 7:00 am was associated with MetS compared to waking later than 7:00 am in univariate analysis, but this association was not observed in multivariate analysis [22]. The sleep–wake cycle was reported to have a markedly modulatory effect on glucose tolerance and insulin secretion [29]. The sleep–wake cycle was also found to be linked to various processes of metabolism and sleep by affecting the circadian system [30]. Additionally, in our study, 96.6% older adults have bed time ≤ 22:00, indicating that waking up late means a longer sleep duration, and the association between long sleep duration and MetS and its components has been demonstrated [31].
Our results showed a strong U-shaped association between sleep duration and TG levels in older adults. A positive associations were previously reported between a long sleep duration and elevated TG levels [18, 20], as well as between a short sleep duration and elevated TG levels [32]. In addition, a U-shaped association between sleep duration and MetS was observed in a cross-sectional study among America populations [15], and both short sleep durations [33,34,35] and long sleep durations [16, 18, 36] were found to be associated with MetS [37]. Despite the study type, diagnostic criteria, risk classification, and sample characteristics of these studies, the association between sleep duration and MetS has been consistent. High TG levels has been confirmed as a risk factor for MetS [38], therefore, our findings indicated that sleep duration might influence the chance of being MetS partially through influencing the TG levels.
In our study, worse subjective sleep quality and daytime dysfunction were found to be associated with hypertension. A consistent positive association between poor subjective sleep quality and hypertension were previously reported in Chinese adults [39] and in Italian populations [40]. Several studies have suggested that poor sleep quality was associated with higher levels of diastolic blood pressure and/or systolic blood pressure [41,42,43]. For the association between daytime dysfunction and hypertension in older adults, the consistent result was also observed in Chinese adults [39]. However, the biological mechanisms of the association between these sleep characteristics and hypertension have not been elucidated. It has been reported that sleep may affect blood pressure by affecting sympathetic nerve activity to the vasculature and that abnormal sleeping may be involved in the pathogenesis of nondipping prehypertension and subsequently in hypertension disturbances [44].
We also found that sleep inefficiency was associated with hyperglycemia. In our study, hyperglycemia consists of fasting plasma glucose (FPG level) ≥ 6.1 mmol/L or Oral Glucose Tolerance Test (OGTT) 2 h plasma glucose level ≥ 7.8 mmol/L and/or previously diagnosed diabetes that was under treatment. In line with the result, a community-based cross-sectional study showed an inverse association between poor sleep efficiency and prevalence of diabetes in middle-aged and older adults [45]. Additionally, a study found that poor sleep efficiency was significantly associated with worse glycemic control among type 2 diabetic patients [46]. Some previously findings can provide the possible mechanism underlying the association between sleep inefficiency and hyperglycemia. Sleep inefficiency is a common quantitative indicator to evaluate insomnia [45, 47], and individuals with poor sleep efficiency are more likely to have poor sleep quality, which affects glucose regulation by changing levels of leptin [48, 49]. In addition, sleep inefficiency may induce diabetes risk factors by association with hypothalamic–pituitary–adrenal axis activity [50, 51]. Moreover, studies have indicated that poor sleep efficiency may cause reduced insulin sensitivity, impaired glucose tolerance, and decreased acute insulin resistance [7, 48].
For the analyses on association between the sleep efficiency and MetS as well as MetS components, we discard participants that have sleep efficiency > 1 due to possible self-reported error or participants' carelessness. Considering that their sleep may also be efficient, we included the participants whose sleep efficiency greater than 1 and classified them into group of sleep efficiency ≥ 85%. We also found that participants with a sleep efficiency of 75% ~ 84% have higher odds of being hyperglycemia compared to those with a sleep efficiency of ≥ 85% (OR = 1.39, 95% CI 1.05–1.89, P = 0.023, Supplementary Table S1).
Several limitations in this study should be acknowledged. First, this study is a cross-sectional study, and the ability to address the causal relationship between sleep and MetS is restricted. Therefore, this result should be further confirmed in a prospective cohort study. Second, this study only assessed older Chinese adults living in Shanghai, thus potentially limiting the generalizability of these results. Third, we evaluated sleep characteristics by self-report questionnaires, which may result in information bias. In addition, obstructive sleep apnoea, which can lead to poor sleep quality and sleep fragmentation, was not considered in this study. However, the PSQI scale includes snoring, which is a major symptom of obstructive sleep apnoea and can be considered as a risk indicator of sleep apnoea. Finally, in this survey-based study in a community population, we did not obtain accurate medication information for the older adults. However, the definition of the component of MetS includes the laboratory parameters and the medical histories of disease, such as diabetes and hypertension, which may reduce, to some extent, the impact of non-medication information on the results.
Conclusion
In summary, the rise time was an important sleep characteristic that may influence MetS for older adults. Poor subjective sleep quality, sleep insufficiency, daytime dysfunction, sleep duration that were too long or too short, and rise late were associated with different MetS components, here evidenced for adults aged 60 y and older. These findings indicated that different sleep characteristics were associate MetS through different pathways, and future longitudinal studies are necessary to confirm these results.
Availability of data and materials
The data that support the findings of this study are available from The Songjiang Center of Disease Prevention and Control, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the corresponding author Qianyi Xiao upon reasonable request and with permission of The Songjiang Center of Disease Prevention and Control.
Abbreviations
- PSQI:
-
Pittsburgh Sleep Quality Index
- MetS:
-
Metabolic Syndrome
- BP:
-
Blood pressure
- HDL-C:
-
High-density lipoprotein cholesterol
- TG:
-
Triglyceride
- WC:
-
Waist circumference
- FPG:
-
Fasting plasma glucose
- PA:
-
Physical Activity
- ORs:
-
Odds ratios
- CI:
-
Confidence Intervals
- BMI:
-
Body Mass Index
- GAM:
-
Generalized additive model
References
Li R, Li W, Lun Z, Zhang H, Sun Z, Kanu JS, Qiu S, Cheng Y, Liu Y. Prevalence of metabolic syndrome in Mainland China: a meta-analysis of published studies. BMC Public Health. 2016;16:296.
Yan HM, Zhang M, Zhang X, Xia YT, Shen T, Zhao ZP, Chen ZH, Huang ZJ, Wang LM. Study of epidemiological characteristics of metabolic syndrome and influencing factors in elderly people in China. Chinese Journal of Hypertension. 2019;27(11):1100.
Zuo H, Shi Z, Hu X, Wu M, Guo Z, Hussain A. Prevalence of metabolic syndrome and factors associated with its components in Chinese adults. Metab. 2009;58(8):1102–8.
Rochlani Y, Pothineni NV, Kovelamudi S, Mehta JL. Metabolic syndrome: pathophysiology, management, and modulation by natural compounds. Ther Adv Cardiovasc Dis. 2017;11(8):215–25.
Liu Y, Dong Y, Li X, Mao X, Peng G, Liu L. Meta-analysis of the prevalence of sleep disorder among Chinese elderly aged 60 years and over. Modern Prev Med. 2014;41(08):1442–1445+1449.
Sp D, Cx C. XJ H: Analysis of influencing factors of sleep disorder among the elderly in 22 provinces of China. Chin J Public Health. 2009;25(08):972–3.
Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354(9188):1435–9.
Borel AL. Sleep Apnea and Sleep Habits: Relationships with Metabolic Syndrome. Nutrients. 2019;11(11):2628.
Knutson KL, Van Cauter E, Rathouz PJ, Yan LL, Hulley SB, Liu K, Lauderdale DS. Association between sleep and blood pressure in midlife: the CARDIA sleep study. Arch Intern Med. 2009;169(11):1055–61.
Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141(11):846–50.
Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1(3):e62.
Broussard JL, Ehrmann DA, Van Cauter E, Tasali E, Brady MJ. Impaired insulin signaling in human adipocytes after experimental sleep restriction: a randomized, crossover study. Ann Intern Med. 2012;157(8):549–57.
Petersen KF, Oral EA, Dufour S, Befroy D, Ariyan C, Yu C, Cline GW, DePaoli AM, Taylor SI, Gorden P, et al. Leptin reverses insulin resistance and hepatic steatosis in patients with severe lipodystrophy. J Clin Invest. 2002;109(10):1345–50.
Hücking K, Hamilton-Wessler M, Ellmerer M, Bergman RN. Burst-like control of lipolysis by the sympathetic nervous system in vivo. J Clin Invest. 2003;111(2):257–64.
Smiley A, King D, Bidulescu A. The Association between Sleep Duration and Metabolic Syndrome: The NHANES 2013/2014. Nutrients. 2019;11(11):2582.
Hall MH, Muldoon MF, Jennings JR, Buysse DJ, Flory JD, Manuck SB. Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep. 2008;31(5):635–43.
Wu J, Xu G, Shen L, Zhang Y, Song L, Yang S, Yang H, Liang Y, Wu T, Wang Y. Daily sleep duration and risk of metabolic syndrome among middle-aged and older Chinese adults: cross-sectional evidence from the Dongfeng-Tongji cohort study. BMC Public Health. 2015;15:178.
Arora T, Jiang CQ, Thomas GN, Lam KB, Zhang WS, Cheng KK, Lam TH, Taheri S. Self-reported long total sleep duration is associated with metabolic syndrome: the Guangzhou Biobank Cohort Study. Diabetes Care. 2011;34(10):2317–9.
Itani O, Kaneita Y, Tokiya M, Jike M, Murata A, Nakagome S, Otsuka Y, Ohida T. Short sleep duration, shift work, and actual days taken off work are predictive life-style risk factors for new-onset metabolic syndrome: a seven-year cohort study of 40,000 male workers. Sleep Med. 2017;39:87–94.
Kim CE, Shin S, Lee HW, Lim J, Lee JK, Shin A, Kang D. Association between sleep duration and metabolic syndrome: a cross-sectional study. BMC Public Health. 2018;18(1):720.
Okubo N, Matsuzaka M, Takahashi I, Sawada K, Sato S, Akimoto N, Umeda T, Nakaji S. Relationship between self-reported sleep quality and metabolic syndrome in general population. BMC Public Health. 2014;14:562.
Zohal M, Ghorbani A, Esmailzadehha N, Ziaee A, Mohammadi Z. Association of sleep quality components and wake time with metabolic syndrome: The Qazvin Metabolic Diseases Study (QMDS). Iran Diabetes Metab Syndr. 2017;11(Suppl 1):S377-s380.
Hung HC, Yang YC, Ou HY, Wu JS, Lu FH, Chang CJ. The association between self-reported sleep quality and metabolic syndrome. PLoS ONE. 2013;8(1): e54304.
Bowman MA, Duggan KA, Brindle RC, Kline CE, Krafty RT, Thayer JF, Hall MH. Prospective associations among objectively and subjectively assessed sleep and the metabolic syndrome. Sleep Med. 2019;58:1–6.
Nikbakhtian S, Reed AB, Obika BD, Morelli D, Cunningham AC, Aral M, Plans D. Accelerometer-Derived Sleep Onset Timing and Cardiovascular Disease Incidence: A UK Biobank Cohort Study. European Heart Journal-Digital Health. 2021;00:1–9.
Ye B, Gao J, Fu H. Associations between lifestyle, physical and social environments and frailty among Chinese older people: a multilevel analysis. BMC Geriatr. 2018;18(1):314.
Lobelo F, Rohm Young D, Sallis R, Garber MD, Billinger SA, Duperly J, Hutber A, Pate RR, Thomas RJ, Widlansky ME, et al. Routine Assessment and Promotion of Physical Activity in Healthcare Settings: A Scientific Statement From the American Heart Association. Circulation. 2018;137(18):e495–522.
Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–34.
Huang W, Ramsey KM, Marcheva B, Bass J. Circadian rhythms, sleep, and metabolism. J Clin Invest. 2011;121(6):2133–41.
Copinschi G, Leproult R, Spiegel K. The important role of sleep in metabolism. Front Horm Res. 2014;42:59–72.
Fan L, Hao Z, Gao L, Qi M, Feng S, Zhou G. Non-linear relationship between sleep duration and metabolic syndrome: A population-based study. Medicine (Baltimore). 2020;99(2): e18753.
Chaput JP, McNeil J, Després JP, Bouchard C, Tremblay A. Short sleep duration as a risk factor for the development of the metabolic syndrome in adults. Prev Med. 2013;57(6):872–7.
Kobayashi D, Takahashi O, Deshpande GA, Shimbo T, Fukui T. Relation between metabolic syndrome and sleep duration in Japan: a large scale cross-sectional study. Intern Med. 2011;50(2):103–7.
Sabanayagam C, Zhang R, Shankar A. Markers of Sleep-Disordered Breathing and Metabolic Syndrome in a Multiethnic Sample of US Adults: Results from the National Health and Nutrition Examination Survey 2005–2008. Cardiol Res Pract. 2012;2012:630802.
Wu MC, Yang YC, Wu JS, Wang RH, Lu FH, Chang CJ. Short sleep duration associated with a higher prevalence of metabolic syndrome in an apparently healthy population. Prev Med. 2012;55(4):305–9.
Santos AC, Ebrahim S, Barros H. Alcohol intake, smoking, sleeping hours, physical activity and the metabolic syndrome. Prev Med. 2007;44(4):328–34.
Choi KM, Lee JS, Park HS, Baik SH, Choi DS, Kim SM. Relationship between sleep duration and the metabolic syndrome: Korean National Health and Nutrition Survey 2001. Int J Obes (Lond). 2008;32(7):1091–7.
O’Neill S, O’Driscoll L. Metabolic syndrome: a closer look at the growing epidemic and its associated pathologies. Obes Rev. 2015;16(1):1–12.
Lu K, Ding R, Tang Q, Chen J, Wang L, Wang C, Wu S, Hu D. Association between self-reported global sleep status and prevalence of hypertension in Chinese adults: data from the Kailuan community. Int J Environ Res Public Health. 2015;12(1):488–503.
Bruno RM, Palagini L, Gemignani A, Virdis A, Di Giulio A, Ghiadoni L, Riemann D, Taddei S. Poor sleep quality and resistant hypertension. Sleep Med. 2013;14(11):1157–63.
Liu RQ, Qian Z, Trevathan E, Chang JJ, Zelicoff A, Hao YT, Lin S, Dong GH. Poor sleep quality associated with high risk of hypertension and elevated blood pressure in China: results from a large population-based study. Hypertens Res. 2016;39(1):54–9.
Osonoi Y, Mita T, Osonoi T, Saito M, Tamasawa A, Nakayama S, Someya Y, Ishida H, Kanazawa A, Gosho M, et al. Poor sleep quality is associated with increased arterial stiffness in Japanese patients with type 2 diabetes mellitus. BMC Endocr Disord. 2015;15:29.
Wan Mahmood WA, Draman Yusoff MS, Behan LA, Di Perna A, Kyaw Tun T, McDermott J, Sreenan S. Association between Sleep Disruption and Levels of Lipids in Caucasians with Type 2 Diabetes. Int J Endocrinol. 2013;2013:341506.
Pepin JL, Borel AL, Tamisier R, Baguet JP, Levy P, Dauvilliers Y. Hypertension and sleep: overview of a tight relationship. Sleep Med Rev. 2014;18(6):509–19.
Yan B, Zhao B, Fan Y, Yang J, Zhu F, Chen Y, Ma X. The association between sleep efficiency and diabetes mellitus in community-dwelling individuals with or without sleep-disordered breathing. J Diabetes. 2020;12(3):215–23.
Bener A, Al-Hamaq A, Agan AF, Öztürk M, Ömer A. Sleeping disturbances and predictor risk factors among type 2 diabetic mellitus patients. Ann Afr Med. 2020;19(4):230–6.
Reed DL, Sacco WP. Measuring Sleep Efficiency: What Should the Denominator Be? J Clin Sleep Med. 2016;12(2):263–6.
Leproult R, Van Cauter E. Role of sleep and sleep loss in hormonal release and metabolism. Endocr Dev. 2010;17:11–21.
Kelesidis T, Kelesidis I, Chou S, Mantzoros CS. Narrative review: the role of leptin in human physiology: emerging clinical applications. Ann Intern Med. 2010;152(2):93–100.
Rosmond R, Björntorp P. The hypothalamic-pituitary-adrenal axis activity as a predictor of cardiovascular disease, type 2 diabetes and stroke. J Intern Med. 2000;247(2):188–97.
Nicolaides NC, Vgontzas AN, Kritikou I, Chrousos G: HPA Axis and Sleep. In: Endotext. Edited by Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, Dungan K, Grossman A, Hershman JM, Hofland J et al. South Dartmouth (MA): MDText.com, Inc; 2000–2022.
Acknowledgements
We gratefully thank all participants and the general practitioners for their cooperation.
Funding
This work was supported by grants from National Key Research and Development Program of China (Grant No. 2018YFC2002000&2018YFC2002001) and Healthy Shanghai action special project of Shanghai Municipal Commission (JKSHZX-2022-01). The funders had no role in the design, methods, participant recruitment, data collection, analysis, or preparation of the paper.
Author information
Authors and Affiliations
Contributions
Study conception and design: QX. Acquisition, analysis, or interpretation of data: LH, JG, XL, QW, YC, XC and HC. Statistical analysis: XL and QX. Manuscript drafting: XL. Review and comment to manuscript: QX and JG. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Department of Public Health in Fudan University, Shanghai, China (IRB#2019–04-0741). All participants or their legally acceptable representatives provided written informed consent. We confirm that all methods were performed in accordance with the guidelines and regulations.
Consent for publication
Not applicable.
Competing Interests
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1.The association between sleep efficiency and MetS and MetS compinents. (Included the participants whosesleep efficiency greater than 1 and classified them into group of sleep efficiency≥ 85%.).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, X., Huang, L., Wu, Q. et al. Sleep characteristic profiles and the correlation with spectrum of metabolic syndrome among older adult: a cross-sectional study. BMC Geriatr 22, 414 (2022). https://doi.org/10.1186/s12877-022-03074-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03074-8