Abstract
Background
Previous research showed association between frailty and an impaired autonomic nervous system; however, the direct effect of frailty on heart rate (HR) behavior during physical activity is unclear. The purpose of the current study was to determine the association between HR increase and decrease with frailty during a localized upper-extremity function (UEF) task to establish a multimodal frailty test.
Methods
Older adults aged 65 or older were recruited and performed the UEF task of rapid elbow flexion for 20 s with the right arm. Wearable gyroscopes were used to measure forearm and upper-arm motion, and electrocardiography were recorded using leads on the left chest. Using this setup, HR dynamics were measured, including time to peak HR, recovery time, percentage increase in HR during UEF, and percentage decrease in HR during recovery after UEF.
Results
Fifty-six eligible participants were recruited, including 12 non-frail (age = 76.92 ± 7.32 years), and 40 pre-frail (age = 80.53 ± 8.12 years), and four frail individuals (age = 88.25 ± 4.43 years). Analysis of variance models showed that the percentage increase in HR during UEF and percentage decrease in HR during recovery were both 47% smaller in pre-frail/frail older adults compared to non-frails (p < 0.01, effect size = 0.70 and 0.62 for increase and decrease percentages). Using logistic models with both UEF kinematics and HR parameters as independent variables, frailty was predicted with a sensitivity of 0.82 and specificity of 0.83.
Conclusion
Current findings showed evidence of strong association between HR dynamics and frailty. It is suggested that combining kinematics and HR data in a multimodal model may provide a promising objective tool for frailty assessment.
Similar content being viewed by others
Introduction
The concept of frailty is used to identify older adults with low physiological reserves, leading to vulnerability to illness, and increased risk of institutionalization and mortality [1, 2]. Muscle loss and weakness (sarcopenia and dynapenia) are the main symptoms of frailty, caused by inflammatory (elevated interleukin 6 (IL-6), C-reactive protein (CRP), tumor necrosis factor alpha (TNFα)), metabolic (deficiencies of various mitochondrial subunits), and hormonal derangements (cortisol and testosterone) that shift homeostasis from an anabolic to a catabolic state [3,4,5,6,7,8,9,10,11]. Previous research also showed association between frailty and an impaired autonomic nervous system (ANS) because of alterations in electrical conduction and action potential morphology [12, 13]. The presence of a compromised neurohormonal homeostasis associated with frailty as measured by ANS dysfunction is, in turn, associated with health complications and mortality [14,15,16,17].
Heart rate variability (HRV: variability in RR intervals) and HR complexity (entropy analysis) during resting have been used for assessing ANS dysfunction and proposed as a vital sign [18,19,20]. Although resting HRV provides information about abnormal ANS performance, it may not be directly associated with HR increase or recovery in response to physical activities, which show a natural decline with age [21]. Further, between-subject variability exists in resting HR/HRV data (e.g., due to breathing regulation and environmental factors [22,23,24]). In our previous research we measured HR dynamics defined as HR increase and recovery parameters during and after walking, and investigated the association between these parameters with frailty [25]. We observed that non-frail participants had significantly larger and faster increases in HR during walking, compared to pre-frail/frail older adults [25], more likely due to a lack of cardiovascular reserve and a compromised ANS in pre-frail/frail older adults [26,27,28,29,30,31,32]. Although these findings are promising, there are some limitations in assessing HR during walking, including motion artifacts due to whole body movement, lack of space in the clinical settings for performing gait test, and inability of some older adults to walk. Therefore, an alternative physical function testing for assessing HR dynamics was proposed in the current study to address these limitations.
Based on the previous evidence, the aim of the current study, was to establish and validate a platform for simultaneous assessment of motor and cardiac function to assess HR dynamics and predict frailty in community dwelling older adults. For the motor function we have previously validated an upper-extremity function (UEF) test, including rapid elbow flexion, to accurately detect systematic decrements in function, including slowness, weakness, inflexibility, and fatigue [33, 34]. We have validated the UEF motor test for discriminating between frailty groups, among both community dwelling older adults and bed-bound trauma patients, using the Fried frailty index and the short-version Rockwood questionnaire as comparators [35,36,37]. The hypotheses for the current work were: 1) HR dynamics due to UEF would be significantly associated with frailty; and 2) a combined model including both motor and HR parameters would more strongly be associated to frailty compared to models incorporating only one of these individual measures.
Methods
Participants and clinical measures
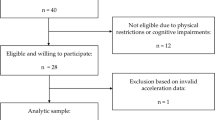
Older adults were recruited from the primary, secondary, and tertiary health care settings, community providers, assisted living facilities, retirement homes, and aging service organizations between October 2016 and March 2018. Inclusion criteria were: 1) being 65 years or older; and 2) the ability to walk a minimum distance of 9.14 m (30 ft) with or without an assistive device (for the frailty assessment). Exclusion criteria were: 1) severe motor disorders (Parkinson’s disease, multiple sclerosis, or recent stroke); 2) severe upper-extremity disorders (e.g., elbow bilateral fractures or rheumatoid arthritis); 3) cognitive impairment identified by a Mini-Mental State Examination (MMSE) score ≤ 23 [38]; 4) terminal illness (i.e., progressive disease where death within six months is expected as a consequence); 5) diseases/disorders that can directly influence HR (including arrhythmia and use of pacemaker); and 6) usage of β-blockers or similar medications that can influence HR. Written informed consent was obtained according to the principles expressed in the Declaration of Helsinki [39]. The study was approved by the University of Arizona Institutional Review Board.
Clinical measures collected included: 1) MMSE and Montreal Cognitive Assessment (MoCA) for cognition [38, 40]; 2) comorbidity based on Charlson Comorbidity Score (CCI) [41]; and 3) depression using Patient Health Questionnaire (PHQ-9) [42]. These measures were collected because they could potentially influence physical activity and the cardiovascular system performance, and accordingly were considered as adjusting variables in the statistical analysis.
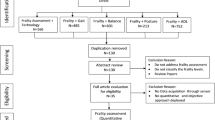
Frailty assessment
Frailty was assessed using the five-component Fried phenotype as an extensively validated and reliable tool [2]. This frailty test included: 1) self-reported unintentional weight loss of 4.54 kg (10 pounds) or more in the previous year; 2) weakness based on grip strength measurements from both left and right arms (adjusted with body mass index (BMI) and sex) and; 3) slowness based on the required time to walk 4.57 m or 15 ft (adjusted with height and sex); 4) self-reported exhaustion based on a short two-question version of Center for Epidemiological Studies Depression (CES-D) scale; and 5) self-reported low energy expenditure based on a short version of Minnesota Leisure Time Activity questionnaire [43]. Participants were categorized as non-frail if they met none of the criteria, pre-frail if they met one or two criteria, and frail if they met three or more criteria.
UEF test
Details of UEF validation and index development have been explained comprehensively within our previous work [35,36,37], and only crucial aspects of UEF regarding the measurement procedure and frailty category assessment were presented here. For UEF, while sitting on a chair, participants performed one trial of full elbow flexion and extension as fast as possible for 20 s using the right arm. Of note, we have shown that UEF results are similar on both sides [35]. Before the test, participants performed a short practice trial with their non-dominant arm to become familiar with the protocol. The protocol was explained to participants, and they were encouraged only once, before elbow flexion, to do the task as fast as possible. To assure consistency, exact same verbal instruction was used, and participants were not further encouraged during the task. Wearable motion sensors (triaxial gyroscope sensors, BioSensics LLC, Cambridge, MA, sampling frequency = 100 Hz) were used to measure forearm and upper-arm motion, and ultimately the elbow angular velocity.
The elbow angular velocity signals from the sensors were filtered to remove noise and drift (first-order high pass butter-worth filter with a cutoff of 2.5 Hz) [44]. Using a peak detection algorithm, maximums and minimums of the angular velocity signal, and subsequently, elbow flexion cycles were detected. Motor function outcomes were derived for each cycle and the average across the 20-s task was calculated. Function outcomes included slowness (speed of elbow flexion), flexibility (range of motion), weakness (strength of upper-extremity muscles), speed variability (motor accuracy), speed reduction (fatigue), and flexion number. For each of the above parameters a subscore was assigned based on previously determined ranges for the the frailty groups (based on the Fried frailty criteria). These subscores were determined previously based on parameter estimate values within multivariable ordinal logistic models, with the Fried frailty categories as the dependent variable and UEF parameters plus demographic information as independent variables [45]. The normalized UEF motor score (range: resilient = 0; extremely frail = 1) for a given participant was then calculated as the sum of subscores corresponding to performance results and demographic information (i.e., BMI score) [37]. The repeatability of UEF motor score was previously tested among a subsample of 14 hospitalized adults (age = 63 ± 12), while UEF was performed twice within (1.1 ± 1.1) days [46]. These findings suggested an excellent repeatability for the UEF motor score indicated by an intraclass correlation coefficient (ICC) of 0.84.
HR assessment
HR was measured using a wearable system with synchronized electrocardiogram (ECG) and accelerometer sensors (360° eMotion Faros, Mega Electronics, Kuopio, Finland; ECG sampling frequency = 1000 Hz and accelerometer sampling frequency = 100 Hz). One channel ECG was recorded using two electrodes. Electrodes were placed on the left chest, one on the upper mid-thorax, and the other one inferior to the left rib cage. Using the synchronized accelerometer data, the exact starting and endpoints of the UEF task were selected. Then a period of 5 s before and 10 s after the activity were selected, respectively, as baseline and recovery periods. To extract RR intervals, QRS peak detection was performed using the Pan-Tompkins algorithm [47], and detected peaks were manually inspected by two researchers (NT and ME).
Two types of HR measures were extracted, representing: 1) resting-state HR and HRV during baseline; and 2) HR dynamics including HR increase during UEF and HR recovery after UEF. HR baseline parameters included: 1) HR mean; 2) beat-to-beat (RR) interval mean; 3) RR CV: the coefficient of variation (standard deviation divided by mean) of RR intervals; and 4) RMSSD: root mean square of successive heartbeat interval differences. HR dynamics parameters explain the amount and timing of HR changes in response to UEF, which included: 1) time to peak HR: elapsed time to reach maximum HR during the task with reference to minimum baseline HR; 2) HR recovery time: elapsed time to reach minimum HR during the recovery with reference to maximum HR; 3) HR percent/absolute increase: percentage/absolute increase in HR during the task compared to minimum baseline HR; and 4) HR percent/absolute decrease: percent/absolute decrease in HR during the recovery compared to maximum HR during the task.
Statistical and power analysis
Analysis of variance (ANOVA) models were used to evaluate the differences in demographic parameters between frailty groups, except sex; chi-square (χ2) test was used to assess differences in sex categories among frailty groups. HR parameters were compared between frailty groups using ANOVA models; age, sex, and BMI were considered as covariates, and Cohen’s effect size (d) was estimated. Age, sex, and, BMI were selected as adjusting variables, since they have been previously associated with HR measures and frailty [37, 48,49,50]. ANOVA analyses for comparing HR parameters across frailty groups were repeated with clinical measures with significant association with frailty as covariates. In the next step of the analysis, HR and motor parameters, separately and combined, were used in multiple logistic regression models as independent variables to identify frailty status. A stepwise parameter selection based on Akaike information criterion (AIC) values was implemented to identify predictive independent variables. For each predicting model, the area under the curve (AUC) with 95% CI was calculated using receiver operator characteristics (ROC) curves. Power calculation was performed to detect differences in HR dynamic parameters between frailty groups for the sample size obtained for the current study using G*Power, ANOVA, Fixed-effect, one-way analysis [51].
Results
Participants and clinical measures
Fifty-six eligible participants were recruited, including 12 non-frail (age = 76.92 ± 7.32 years), 40 pre-frail (age = 80.53 ± 8.12 years), and four frail (age = 88.25 ± 4.42 years). None of the demographic information was significantly different between the three frailty groups (p > 0.10, Table 1). Among clinical measures, CCI comorbidity and PHQ-9 depression scores were significantly different between frailty groups (p < 0.03, Table 1).
UEF motor and HR parameters
UEF motor score was significantly different between the frailty categories; UEF motor score was 0.32 ± 0.18 on average for non-frail and 0.53 ± 0.23 for pre-frail/frail participants (p = 0.04, Table 2). For HR dynamic parameters, pre-frail/frail older adults showed almost half of the amount of HR increase during UEF, and HR decrease during the recovery compared to non-frail participants (p < 0.01, Table 2, Figs.1 and 2). The four parameters of HR increase during UEF and HR decrease during recovery were not significantly associated with any of the clinical measures including CCI comorbidity and PHQ-9 depression scores (p > 0.11). Further, the association between HR increase and decrease with frailty remained significant when CCI and PHQ-9 were added as covariates (p < 0.01). Time to peak and recovery of HR, however, were not significantly different between the frailty groups (p > 0.49, Table 2). Although trends of higher HR and smaller HRV for pre-frail/frail were observable, none of the baseline HR parameters were significantly different between the frailty groups (p > 0.23, Table 2).
For logistic model statistical analyses, the pre-frail and frail groups were merged due to the small number of included frail older adults in this study. Results from logistic models showed that percent increase and decrease in HR, as well as UEF motor score were all significantly associated with frailty (p < 0.01). Using previously developed UEF motor score in the logistic model, an area under curve (AUC) of receiver operating characteristic (ROC) of 0.78 was achieved. Combining both UEF HR dynamic (i.e., HR percent increase) and motor score, the AUC was improved to 0.87 (Table 3). Using this model, pre-frailty/frailty was predicted with a sensitivity and specificity of 0.82 and 0.83 (Table 3).
Discussion
HR dynamics and frailty
As hypothesized, significant associations were observed between frailty status and HR changes during the activity and afterwards during the recovery period. During physical activity, an increase in sympathetic outflow increases HR and stroke volume to match demand [52, 53]. During recovery from the physical activity, parasympathetic activity increases to reduce HR to baseline [54,55,56]. Lack of resilience in changing HR in pre-frail/frail older adults can be explained by both a compromised ANS performance or lack of cardiac reserve. Previous research provided evidence of ANS dysfunction with frailty. Focusing on resting state differences in HRV as an indicator of ANS performance, a smaller HRV has been observed among pre-frail and frail older adults compared to non-frails [57]. On the other hand, lack of cardiac reserve during resting, can move pre-frail/frail individuals to a more imbalanced (less homeostatic) and already stressed state, causing an inability to respond to additional stress such as a simple task of arm movement. In confirmation of this theory, although not significant, we observed trends of higher mean HR during resting among pre-frail and frail participants compared to non-frails (Table 3 and Fig. 2).
Only a few studies exist to assess HR dynamics during activity across frailty groups. Smaller changes in HR has been reported previously for lying-to-standing and seated step test [58, 59]. Also, in our previous research we observed that pre-frail/frail older adults had 46% smaller and 49% slower increase in HR during walking compared to pre-frail/frail older adults [46]. One noticeable difference between our previous and current findings is that time to peak HR during activity was significantly different in 15 ft walk test, while this parameter was not different in the current study. One possible explanation is that for pre-frail and frail older adults performing a walking test with a set distance takes longer than non-frails, which consequently may lead to a slower HR increase. This explanation needs to be further assessed by executing walking test with a set duration rather than distance. Nevertheless, based on current findings, assessing changes in HR magnitude, rather than timing of HR changes (both increase and recovery) may provide a more robust way of measuring HR dynamics.
Another important observation was that HR increase can characterize cardiac imbalance behavior, similar or even better than HR recovery. Most previous research has focused on HR recovery for disease diagnosis; studies showed prognostic value in measuring HR recovery one minute after cardiopulmonary exercise testing for heart failure prediction [17, 60]. Nevertheless, all these HR assessments were performed after the physical activity, since performing whole body exercise makes accurate HR assessment complex due to motion artifacts. In the implemented UEF approach, participants performed elbow flexion with the right arm while HR data measurement electrodes were placed on the left side. This ECG placement provided minimal motion artifact from the right-side arm movement to permit accurate dynamic HR assessment.
Combined HR and motor model
In confirmation of our hypothesis, current results suggest that combining HR and motor function in a single model can enhance frailty prediction in comparison to models involving each of these physiological systems individually. It is believed now that frailty is caused by loss of homeostasis not necessary in one domain, but multiple physiological systems. In other words, frailty is the result of a compromised dynamic interaction between several physiological systems, rather than one specific pathway [61]. Accordingly, the concept of frailty assessment across multiple physiological systems and their interactions has recently drawn more attention. Ghachem et al., for instance, assessed dysregulation of six physiological systems including oxygen transport, kidney/liver function, leukopoiesis, micronutrients, lipids, and electrolytes in association with frailty [62]. They have provided evidence that frailty is more strongly associated with the number of dysregulated systems, rather than the type of dysregulation [62]. In confirmation to previous research, current findings support the hypothesis that assessing multiple physiological systems would improve frailty assessment. Unlike previous work, our approach involved one testing, within which, both cardiac and motor performance were evaluated, to efficiently balance the accuracy and the burden of the testing process.
Limitation and future direction
Although current findings were promising, there are limitations that warrant future research. First, the sample of community dwelling older adults chosen for the current study was small and may not reflect condition of hospitalized older adults. Due to the small sample of participants, additional analyses were not performed, including assessment of interaction effect of frailty and HR on motor function performance. Further, in the current study the association between baseline HR and HR dynamic parameters were not reported. Since these results were similar to our previous work, we encourage readers to read previously reported findings regarding HR analysis during gait tests [46]. Also, although we validated HR dynamics outcomes for frailty assessment, their test-retest reliability should be investigated in future research.
One other limitation of the current study is the lack of long-term resting HR measurement. Although five seconds of rest before UEF would be enough for short-term HRV assessment, several other analyses related to regularity (complexity analysis) of HR data could not be accomplished here due to limited number of samples for nonlinear dynamic analysis. Previous studies demonstrated significant association between HR complexity and frailty [63,64,65], and therefore, it would be interesting to explore how the HR complexity during basal condition is related to HR dynamics in response to physical activity, especially across frailty groups. Further, older adult participants with arrhythmia and those who used β-blockers and pacemakers were excluded from the study. Therefore, effects of these disorders and medications on HR measures need to be studies in future. Lastly, none of the participants had identified frail in more than three criteria of the Fried phenotype. Therefore, our results may be limited in presenting too frail older adults. Further, validation using other frailty assessment tools and more importantly within longitudinal studies for predicting adverse outcomes is required in the future.
Conclusion and clinical implications
Current findings showed that HR changes due to physical activity was smaller among pre-frail and frail individuals during the activity and afterwards during the recovery period compared to non-frail older adults. We also showed that by combining HR and motor function we may improve frailty prediction compared to models incorporating each of these measures individually. The proposed multimodal HR and motor frailty assessment approach is objective and easy to perform. Due to its simplicity, compared to gait test, this test can be performed on hospitalized patients to predict therapy complications and identify patients with treatment-responsive frailty for directing appropriate care, with potential implications for older adults with heart diseases.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. The implemented code for HR data analysis will be available for research purposes. Please contact the corresponding author for request access to UEF codes.
References
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–62.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Ser A Biol Med Sci. 2001;56(3):M146–57.
Yao X, Li H, Leng SX. Inflammation and immune system alterations in frailty. Clin Geriatr Med. 2011;27(1):79–87.
Hubbard RE, O’Mahony MS, Savva GM, Calver BL, Woodhouse KW. Inflammation and frailty measures in older people. J Cell Mol Med. 2009;13(9b):3103–9.
Serviddio G, Romano AD, Greco A, Rollo T, Bellanti F, Altomare E, et al. Frailty syndrome is associated with altered circulating redox balance and increased markers of oxidative stress. Int J Immunopathol Pharmacol. 2009;22(3):819–27.
Schaap LA, Pluijm SM, Deeg DJ, Visser M. Inflammatory markers and loss of muscle mass (sarcopenia) and strength. Am J Med. 2006;119(6):526.e529–17.
Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB, et al. Relationship of interleukin-6 and tumor necrosis factor-α with muscle mass and muscle strength in elderly men and women: the health ABC study. J Gerontol Ser A Biol Med Sci. 2002;57(5):M326–32.
Cesari M, Penninx BW, Pahor M, Lauretani F, Corsi AM, Williams GR, et al. Inflammatory markers and physical performance in older persons: the InCHIANTI study. J Gerontol Ser A Biol Med Sci. 2004;59(3):M242–8.
Johar H, Emeny RT, Bidlingmaier M, Reincke M, Thorand B, Peters A, et al. Blunted diurnal cortisol pattern is associated with frailty: a cross-sectional study of 745 participants aged 65 to 90 years. J Clin Endocrinol Metab. 2014;99(3):E464–8.
O’Connell M, Tajar A, Roberts SA, Wu F. Do androgens play any role in the physical frailty of ageing men? Int J Androl. 2011;34(3):195–211.
López-Armada MJ, Riveiro-Naveira RR, Vaamonde-García C, Valcárcel-Ares MN. Mitochondrial dysfunction and the inflammatory response. Mitochondrion. 2013;13(2):106–18.
Varadhan R, Chaves PH, Lipsitz LA, Stein PK, Tian J, Windham BG, et al. Frailty and impaired cardiac autonomic control: new insights from principal components aggregation of traditional heart rate variability indices. J Gerontol Series A. 2009;64(6):682–7.
Moghtadaei M, Jansen HJ, Mackasey M, Rafferty SA, Bogachev O, Sapp JL, et al. The impacts of age and frailty on heart rate and sinoatrial node function. J Physiol. 2016;594(23):7105–26.
Adamson PB, Smith AL, Abraham WT, Kleckner KJ, Stadler RW, Shih A, et al. Continuous autonomic assessment in patients with symptomatic heart failure: prognostic value of heart rate variability measured by an implanted cardiac resynchronization device. Circulation. 2004;110(16):2389–94.
Scalvini S, Volterrani M, Zanelli E, Pagani M, Mazzuero G, Coats AJ, et al. Is heart rate variability a reliable method to assess autonomic modulation in left ventricular dysfunction and heart failure?: assessment of autonomic modulation with heart rate variability. Int J Cardiol. 1998;67(1):9–17.
De Jong MMJ, Randall DC. Heart rate variability analysis in the assessment of autonomic function in heart failure. J Cardiovasc Nurs. 2005;20(3):186–95.
Arena R, Guazzi M, Myers J, Peberdy MA. Prognostic value of heart rate recovery in patients with heart failure. Am Heart J. 2006;151(4):851.e857–13.
Morris JA, Norris PR. Role of reduced heart rate volatility in predicting death in trauma patients. Adv Surg. 2005;39:77–96.
Muller JE, Tofler G, Stone P. Circadian variation and triggers of onset of acute cardiovascular disease. Circulation. 1989;79(4):733–43.
Kleiger RE, Miller JP, Bigger JT Jr, Moss AJ. Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. Am J Cardiol. 1987;59(4):256–62.
Javorka M, Zila I, Balharek T, Javorka K. Heart rate recovery after exercise: relations to heart rate variability and complexity. Braz J Med Biol Res. 2002;35(8):991–1000.
Cipryan L, Litschmannova M. Intra-day and inter-day reliability of heart rate variability measurement. J Sports Sci. 2013;31(2):150–8.
Pinna GD, Maestri R, Torunski A, Danilowicz-Szymanowicz L, Szwoch M, La Rovere MT, et al. Heart rate variability measures: a fresh look at reliability. Clin Sci. 2007;113(3):131–40.
Taelman J, Vandeput S, Spaepen A, Van Huffel S. Influence of mental stress on heart rate and heart rate variability. In: In: 4th European conference of the international federation for medical and biological engineering: Springer; 2009. p. 1366–9.
Toosizadeh N, Ehsani H, Parthasarathy S, Carpenter B, Ruberto K, Mohler J, et al. Frailty and heart response to physical activity. Arch Gerontol Geriatr. 2021;93:104323.
Goldwater DS, Pinney SP. Frailty in advanced heart failure: a consequence of aging or a separate entity? Clinical medicine insights. Cardiology. 2015;9:CMC:S19698.
Anker S, Ponikowski P, Clark AL, Leyva F, Rauchhaus M, Kemp M, et al. Cytokines and neurohormones relating to body composition alterations in the wasting syndrome of chronic heart failure. Eur Heart J. 1999;20(9):683–93.
Levine B, Kalman J, Mayer L, Fillit HM, Packer M. Elevated circulating levels of tumor necrosis factor in severe chronic heart failure. N Engl J Med. 1990;323(4):236–41.
McMurray J, Abdullah I, Dargie HJ, Shapiro D. Increased concentrations of tumour necrosis factor in" cachectic" patients with severe chronic heart failure. Heart. 1991;66(5):356–8.
Anker SD, Clark AL, Kemp M, Salsbury C, Teixeira MM, Hellewell PG, et al. Tumor necrosis factor and steroid metabolism in chronic heart failure: possible relation to muscle wasting. J Am Coll Cardiol. 1997;30(4):997–1001.
von Haehling S, Doehner W, Anker SD. Nutrition, metabolism, and the complex pathophysiology of cachexia in chronic heart failure. Cardiovasc Res. 2007;73(2):298–309.
Uchmanowicz I, Łoboz-Rudnicka M, Szeląg P, Jankowska-Polańska B, Łoboz-Grudzień K. Frailty in heart failure. Curr Heart Fail Rep. 2014;11(3):266–73.
Ehsani H, Mohler MJ, Golden T, Toosizadeh N. Upper-extremity function prospectively predicts adverse discharge and all-cause COPD readmissions: a pilot study. Int J Chronic Obstruct Pulmo Dis. 2019;14:39.
Toosizadeh N, Berry C, Bime C, Najafi B, Kraft M, Mohler J. Assessing upper-extremity motion: an innovative method to quantify functional capacity in patients with chronic obstructive pulmonary disease. PLoS One. 2017;12(2):e0172766.
Toosizadeh N, Mohler J, Najafi B. Assessing upper extremity motion: an innovative method to identify frailty. J Am Geriatr Soc. 2015;63(6):1181–6.
Toosizadeh N, Joseph B, Heusser MR, Jokar TO, Mohler J, Phelan HA, et al. Assessing upper-extremity motion: an innovative, objective method to identify frailty in older bed-bound trauma patients. J Am Coll Surg. 2016;223(2):240–8.
Toosizadeh N, Wendel C, Hsu C-H, Zamrini E, Mohler J. Frailty assessment in older adults using upper-extremity function: index development. BMC Geriatr. 2017;17(1):1–7.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Association GAotWM: world medical association declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Coll Dentists. 2014;81(3):14–8.
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Thorofare: vol. 32: SLACK Incorporated; 2002. p. 509–15.
Fieo RA, Mortensen EL, Rantanen T, Avlund K. Improving a measure of mobility-related fatigue (the mobility-tiredness scale) by establishing item intensity. J Am Geriatr Soc. 2013;61(3):429–33.
Asghari M, Ehsani H, Cohen A, Tax T, Mohler J, Toosizadeh N. Nonlinear analysis of the movement variability structure can detect aging-related differences among cognitively healthy individuals. Hum Mov Sci. 2021;78:102807.
Sullivan LM, Massaro JM, D'Agostino RB Sr. Presentation of multivariate data for clinical use: the Framingham study risk score functions. Stat Med. 2004;23(10):1631–60.
Ruiz M, Peña M, Cohen A, Ehsani H, Joseph B, Fain M, et al. Physical and cognitive function assessment to predict postoperative outcomes of abdominal surgery. J Surg Res. 2021;267:495–505.
Pan J, Tompkins WJ. A real-time QRS detection algorithm. IEEE Trans Biomed Eng. 1985;3:230–6.
Anderson R, Jönsson P, Sandsten M. Effects of age, BMI, anxiety and stress on the parameters of a stochastic model for heart rate variability including respiratory information. Biosignals. 2018;4:17–25.
Gordon E, Peel N, Samanta M, Theou O, Howlett S, Hubbard R. Sex differences in frailty: a systematic review and meta-analysis. Exp Gerontol. 2017;89:30–40.
Hubbard RE, Lang IA, Llewellyn DJ, Rockwood K. Frailty, body mass index, and abdominal obesity in older people. J Gerontol Series A. 2010;65(4):377–81.
Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G* power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–60.
Evrengul H, Tanriverdi H, Kose S, Amasyali B, Kilic A, Celik T, et al. The relationship between heart rate recovery and heart rate variability in coronary artery disease. Ann Noninvasive Electrocardiol. 2006;11(2):154–62.
Shephard RJ: Exercise physiology: Toronto; Philadelphia: BC Decker; Saint Louis, Mo.: Sales and distribution … ; 1987.
Carter R III, Watenpaugh DE, Wasmund WL, Wasmund SL, Smith ML. Muscle pump and central command during recovery from exercise in humans. J Appl Physiol. 1999;87(4):1463–9.
Nishime EO, Cole CR, Blackstone EH, Pashkow FJ, Lauer MS. Heart rate recovery and treadmill exercise score as predictors of mortality in patients referred for exercise ECG. Jama. 2000;284(11):1392–8.
Savin WM, Davidson DM, Haskell WL. Autonomic contribution to heart rate recovery from exercise in humans. J Appl Physiol. 1982;53(6):1572–5.
Parvaneh S, Howe CL, Toosizadeh N, Honarvar B, Slepian MJ, Fain M, et al. Regulation of cardiac autonomic nervous system control across frailty statuses: a systematic review. Gerontology. 2016;62(1):3–15.
Romero-Ortuno R, Cogan L, O'Shea D, Lawlor BA, Kenny RA. Orthostatic haemodynamics may be impaired in frailty. Age Ageing. 2011;40(5):576–83.
Weiss CO, Hoenig HH, Varadhan R, Simonsick EM, Fried LP. Relationships of cardiac, pulmonary, and muscle reserves and frailty to exercise capacity in older women. J Gerontol Series A. 2010;65(3):287–94.
Maeder MT, Ammann P, Rickli H, Brunner-La Rocca HP. Impact of the exercise mode on heart rate recovery after maximal exercise. Eur J Appl Physiol. 2009;105(2):247–55.
Fried LP, Xue Q-L, Cappola AR, Ferrucci L, Chaves P, Varadhan R, et al. Nonlinear multisystem physiological dysregulation associated with frailty in older women: implications for etiology and treatment. J Gerontol Series A. 2009;64(10):1049–57.
Ghachem A, Fried LP, Legault V, Bandeen-Roche K, Presse N, Gaudreau P, et al. Evidence from two cohorts for the frailty syndrome as an emergent state of parallel dysregulation in multiple physiological systems. Biogerontology. 2021;22(1):63–79.
Chaves PH, Varadhan R, Lipsitz LA, Stein PK, Windham BG, Tian J, et al. Physiological complexity underlying heart rate dynamics and frailty status in community-dwelling older women. J Am Geriatr Soc. 2008;56(9):1698–703.
Katayama PL, Dias DPM, Silva LEV, Virtuoso-Junior JS, Marocolo M. Cardiac autonomic modulation in non-frail, pre-frail and frail elderly women: a pilot study. Aging Clin Exp Res. 2015;27(5):621–9.
Takahashi AC, Bonjorni LA, Buto MS, Vassimon-Barroso V, Minatel V, Rocha SM, et al. Short-term complexity of cardiovascular oscillations in frailty syndrome. In: In: 2014 8th conference of the European study group on cardiovascular oscillations (ESGCO): IEEE; 2014. p. 21–2.
Acknowledgements
Not applicable.
Funding
This project was supported by two awards from the National Institute of Aging (NIA/NIH - Phase 2B Arizona Frailty and Falls Cohort 2R42AG032748–04 and NIA/NIH - 1R21AG059202-01A1). The views represented in this work are solely the responsibility of the authors and do not represent the views of NIH.
Author information
Authors and Affiliations
Contributions
NT: concept, study design, subject recruitment, study management, data analysis and interpretation, statistical analysis, manuscript writing and editing, critical review of manuscript and approval of final manuscript. ME: data analysis, interpretation of findings, statistical analysis, manuscript writing and critical review of manuscript. HE: interpretation of findings, critical review of manuscript, and comments and approval of final manuscript. SP: interpretation of findings, critical review of manuscript, and comments and approval of final manuscript. MA: interpretation of findings, critical review of manuscript, comments and approval of final manuscript. NS: subject recruitment, study management, study design, interpretation of findings, critical review of manuscript and approval of final manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained according to the principles expressed in the Declaration of Helsinki. The study was approved by the University of Arizona Institutional Review Board (Protocol ID: 1412591150R002).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Toosizadeh, N., Eskandari, M., Ehsani, H. et al. Frailty assessment using a novel approach based on combined motor and cardiac functions: a pilot study. BMC Geriatr 22, 199 (2022). https://doi.org/10.1186/s12877-022-02849-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-02849-3